Abstract
This study was performed to evaluate the prevalence and risk factors of dry eye disease (DED) among paramedical workers at a university hospital in Korea. This cross-sectional study included 566 paramedical workers at a university hospital in Korea. Dry eye symptoms were assessed using a 9-item questionnaire, and DED was defined as having 1 or more dry eye symptoms often or all the time. A survey including demographic data and potential risk factors of DED was also performed. Psychological stress was measured using stress VAS and perceived stress scale 4 (PSS-4) questionnaires. Of the 566 paramedical workers, 232 (35 male and 197 female) completed the survey. Prevalence of DED was 42.7% (99/232). Univariate analysis revealed that female sex (P < 0.001), prolonged computer use (P = 0.003) and higher stress VAS (P < 0.001) and PSS-4 (P = 0.009) scores had significant association with DED. In multivariate analysis, DED had significant association with female sex (P = 0.003) and stress VAS (P = 0.013) after adjustment for sex, duration of computer use and stress VAS, and had significant association with female sex (P = 0.003) and durations of computer use (P = 0.029) after adjustment for sex, duration of computer use and PSS-4 score. In conclusion, DED was prevalent among paramedical workers in Korea. Its risk increased among females and workers with increased psychological stress. Prolonged use of computer was possibly associated with DED.
Similar content being viewed by others
Introduction
Dry eye disease (DED) is one of the most common diseases with a prevalence of 10–30% worldwide1,2. It has emerged as a major public health problem because the condition poses considerable amount of economic burden both to affected individual and society3,4. The symptoms of DED, such as, ocular discomfort, pain, grittiness, redness, dryness, foreign body sensation and visual disturbance can interfere with daily activities including reading, driving, using computer and watching TV5,6; thus, the disease can result in serious impairment of quality of life4,5,6.
DED is a multifactorial disease that is characterized by discrepancy between dry eye symptoms and ocular surface signs, which renders the diagnosis and management of the disease difficult2,7,8,9. Previous studies suggested that subjective dry eye symptoms can be influenced by individual pain perception or psychosomatic conditions including depression, anxiety and stress10,11. Increased use of video terminal display (VDT) is also shown be associated with the risk of DED6,12.
A large number of studies have been conducted to evaluate the nature of DED. However, there are only few data about the characteristics of DED in healthcare personnel13,14. Hospital workers are exposed to work requiring great concentration and large amount of VDT work in relatively less humidified environment in ward or operation room, which may increase the risk of developing the dry eye symptoms. However, to the best of our knowledge, there has been no report on nature of DED in hospital workers in Korea.
Therefore, in the present study, we evaluated the prevalence and risk factors of DED among paramedical workers at a university hospital in Korea.
Patients and Methods
Study Design and Population
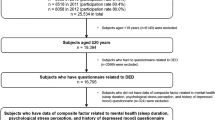
This is a cross-sectional study that included 566 paramedical workers including nurse and medical technicians at Kangwon National University Hospital in Korea.
Only workers who fully understood the nature of the survey and agreed to participate were included. Exclusion criteria included active ocular surface inflammation, such as, infectious keratitis, infectious or allergic conjunctivitis, glaucoma, connective tissue disorders, history of ocular trauma, history of ocular surgery other than refractive surgery, systemic vasculitis.
Every participant was contacted by trained interviewers and requested to fill out a survey that comprises three categories of questions, as follows: (1) questions regarding dry eye symptoms, (2) questions about demographic data and potential risk factors of DED and (3) questions regarding psychological stress.
First, a Dry Eye Questionnaire (DEQ) was administered. The DEQ, which consisted of 9 questions pertaining to dry eye symptoms, was generated by modifying dry eye symptom questions suggested in the literature (Table 1)8,9,10. Each participant was asked to indicate whether each of the 9 symptoms related to DED was experienced rarely, sometimes, often, or all the time. The diagnosis of DED was made when a participant reported to have 1 or more symptoms often or all the time during the past 2 weeks.
The dry eye visual analog scale (VAS) and ocular surface disease index (OSDI) questionnaires were also administered for the quantification of the dry eye symptoms, according to the literature13,15,16,17. The VAS questionnaire comprised three questions, each of which had an answer scale from 0 (no symptom) to 10 (the worst symptom imaginable), for pain, dryness and foreign-body sensation, respectively; thus, the total VAS score ranged from 0 to 3016,18. The OSDI questionnaire consisted of 12 questions related to dry eye symptoms that each subject experienced during one week prior to the interview13,15,16,17. The OSDI was expressed as a sum score of 0–100, according to the literature13,15,16,17.
Second, the participants also filled in the questionnaire regarding demographic data, such as, age by decades and sex, potential risk factors of DED including contact lens (CL) use, history of refractive surgery, hours of computer use, hours of paper work, sleep duration and personal habits including alcohol consumption. Age of each participant was collected by decade as per the recommendation from the IRB to prevent disclosure of identification of the participants.
Third, psychological stress was evaluated using the Perceived Stress Scale 4 (PSS-4) questionnaire and stress VAS, according to the literature19,20,21,22. PSS-4 questionnaire consisted of 4 questions pertaining to perceived psychological stress (Table 2), and used to quantify the perceived stress between the score of 0 to 16, with higher scores reflected an increased perceived psychological stress22. Stress VAS score was also used for the measurement of psychological stress, with an answer scale from 0 (no stress) to 10 (extreme stress that can be imagined)19,20,21.
Statistical analysis
SPSS software for Windows version 18.0 (SPSS, Inc, Chicago, Illinois) was used for the statistical analyses. The prevalence of DED was calculated with a 95% confidence interval (CI). The association between DED and potential risk factors was determined with univariate analysis using Pearson’s chi-square test for categorical variables and Student’s t-test for quantitative variables. Multivariate analysis using logistic regression analysis was also performed for the evaluation of the risk factors of DED. P-value < 0.05 was considered statistically significant.
Ethics Statement
This study was approved by the institutional review board (IRB) of the Kangwon National University Hospital and was conformed to the tenets of the Declaration of Helsinki. Informed consent was obtained from all the participants.
Results
Prevalence of DED
Of a total of 566 paramedical workers, 232 co-operated with the interview and completed the survey, of whom 35 (15.1%) were male and 197 (84.9%) were female. Prevalence of DED was 42.7% (99/232; 95% CI, 36.6% – 48.7%). Subjects with DED (DED group) showed significantly higher VAS and OSDI score compared to those without DED (non-DED group) (P < 0.001 for both) (Table 3).
Risk factors for DED
Univariate analysis showed that female sex (P < 0.001), prolonged computer use (P = 0.003) and higher stress VAS (P < 0.001) and PSS-4 (P = 0.009) scores were associated with increased risk of DED. The prevalence of DED was significantly higher in female (47.7%, 94/197) compared to male (14.3%, 5/35) participants (P < 0.001). Workers in DED group showed significantly longer duration of computer use(7.9 ± 2.0 hr vs. 7.0 ± 2.8 hr, P = 0.003). Both stress VAS (6.7 ± 2.2 vs. 5.6 ± 2.7, P < 0.001) and PSS-4 (7.9 ± 2.3 vs. 7.0 ± 2.4, P = 0.009) scores were also significantly higher in the DED group compared to non-DED group. However, age, CL wear, history of refractive surgery, hours of paper work, sleep duration, alcohol consumption did not show significant association with (Table 4).
Table 5 shows the results of multivariate logistic regression analyses using various models. After adjustment for sex, duration of computer use and stress VAS score, female sex (odds ratio [OR], 4.53; 95% CI, 1.65–12.42; P = 0.003) and stress VAS score (OR, 1.17; 95% CI, 1.03–1.32; P = 0.013) had significant association with DED (Model 1). After adjustment for sex, duration of computer use and PSS-4 score, female sex (OR, 4.57; 95% CI, 1.67–12.48; P = 0.003) and computer use (OR, 1.15; 95% CI, 1.01–1.30; P = 0.029) were significant associated to DED (Model 2).
Stress VAS score showed significant correlation with both OSDI (P < 0.001, r2 = 0.10) and dry eye VAS (P < 0.001, r2 = 0.16). PSS-4 score also had significant correlation with both OSDI (P < 0.001, r2 = 0.04) and dry eye VAS (P < 0.002, r2 = 0.02) score.
Discussion
In this study, we evaluated the prevalence and risk factors of DED among paramedical workers at a hospital in Korea. The diagnosis of DED was made based on the presence of dry eye symptoms included in the DEQ2. Symptom-based definition of DED has been used in the researches of DED worldwide, especially in large population-based studies1,2,6,23,24,25, which might be due to the following reasons: (1) there is no gold standard test of the diagnosis of DED yet24,25, (2) Lack of correlation between signs and symptoms of DED has been reported24,25,26,27, (3) Relief of dry eye symptoms is the main goal of treatment for DED2,28, and (4) DEQs were proven to have substantial repeatability6,24,25,29. In this study, both OSDI and dry eye VAS were significantly higher in DED group, suggesting the reliability of the DEQ (Table 2).
The present study revealed high prevalence of DED in paramedical workers (42.7%). Prior studies reported the higher prevalence of DED in Asian countries, especially in elderly population1,2,30. A study on Japanese elderly population over 60 years reported that the prevalence of DED was 73.5%30. Its prevalence in a Korean and Chinese population >65 years was 33.2% and 23.5%, respectively1,2. Meanwhile, studies have indicated that DED might be also prevalent in younger age group6,13,23,31. Studies on Japanese population reported that the prevalence of DED was over 20% in adolescents and high school students23,31. Another Japanese study revealed that the prevalence of DED in young and middle-aged office workers was 27.3% in male and 48.0% in female participants6. A study on university students in Ghana also reported a high prevalence of symptom-based DED of 44.3%32. These findings suggest that DED may be prevalent in younger population, particularly in office workers and students.
A recent study demonstrated high DED prevalence of 56% in surgical residents with a mean age of 27.8 years old, and suggested that working inside the operating room, in which the ventilation environment is closed and precise procedures with great concentration are performed, might increase the risk of DED13. These findings, along with our results, suggest that hospital worker might have increased risk of DED13. The environmental characteristics of hospital, such as, low indoor humidity, reduced indoor air flow and exposure to volatile organics might make individuals more prone to develop DED33,34. Makateb et al.35 revealed that night-time working were associated with decreased tear film stability and worsening of dry eye symptoms. Thus, it can be postulated that frequent night-shift in hospital workers may increase the risk of DED. There findings suggest that improvement of hospital environment and reduction in night shift work could lower the risk of DED in paramedical workers. Further studies are needed to evaluate the nature and risk factors of DED in paramedical workers.
The results showed that stress VAS was associated with an increased risk of DED. PSS-4 score also had significant association with DED in univariate analysis, although no significant association was found in multivariate analysis. These findings suggest a close relationship between psychologic stress and DED. Although the association between DED and psychiatric conditions including depression and post-traumatic stress disorder have been reported by several studies10,36,37, there has been only few studies regarding the association between psychological stress and DED, probably due to the difficulty in the measurement of the psychological stress. We measured the psychologic stress among the paramedical workers using the stress VAS because it was proven to be a simple, suitable and efficient tool for the assessment of psycholgical stress by occupational physicians20,21. We also used PSS-4 because it was also shown to be a reliable tool in quantification of perceived psychological stress22. Na et al.11 also demonstrated that DED was associated with an increased risk of severe psychological stress, depression and anxiety in Korean women11. These findings, along with our results. suggest that psychological stress may be associated with an increased risk of DED. Therefore, it can be postulated that management of psychological stress can reduce the risk of DED in hospital workers. Although the pathophysiology underlying the association between psychological stress and DED is still ulcer, several mechanisms can be postulated, as follows: (1) Psychological stress may affect pain perception, and make individuals with increased stress more prone to feel dry eye symptoms. Geva et al.38 revealed that acute stress can reduce the ability to modulate pain. Cohen et al.39 also suggested that psychological stress can increase pain by inducing elevation of cortisol level. (2) Psychological stress can increase systemic inflammatory activity by promoting production of inflammatory cytokines40, which lead to increased risk of developing various diseases, including DED41,42. (3) Perceived stress was shown to be associated with of somatization43. Thus, somatization induced by psychological stress can aggravate dry eye symptoms. (4) Psychological stress can result in depression40, which is a well-known risk factor for DED10,36,37. (5) There is a possibility that the effect of Korean culture, such as, pressure for high achievement, vigorous competition for jobs and promotion and emotional stress from co-workers and customers might also play a role. We believe further studies including larger population are necessary to evauate the pathophysiology underlying the association between the two conditions.
This study showed that female sex was associated with DED, which is in agreement with the results of the previous studies1,2,6,12. Vehof et al.44 revealed that women showed higher dry eye symptom scores than men and increased discrepancy between dry eye signs and symptoms. Schaumberg et al.45 demonstrated that women tended to experience more severe and frequent DED symptoms than men, and also complained a greater influence of DED on daily activities. A recent study by Na et al.46 also reported that menstrual irregularity had an association with DED. These findings suggest that sex hormones might affect ocular surface environment through their effects on corneal sensitivity, conjunctival goblet cells, lacrimal glands and Meibomian glands1,2. Japanese studies revealed increased prevalence of DED in female sex in Japanese high school students and young office workers6,23. Our results also showed high prevalence of DED in young female paramedical workers, indicating that sex hormones might play a role in DED in young women as well as older ones. However, the reason for increased risk of DED in the female population is still unclear, and therefore further studies are warranted.
The results also suggest that long duration of computer use was possibly associated with an increased risk of DED, which is in consistent with the results of the prior studies that prolonged use of video display terminal (VDT) was associated with DED6,12. Kawashima et al.47 revealed that 60% of the workers using VDT had DED, which might cause a significant impairment of the productivity of the workers48. Prolonged VDT use may be associated with decreased blinking rates and increased tear evaporation, which can lead to tear film instability and hyperosmolarity, and eventually short break-up time type DED6,48. Moreover, blue light emission from VDTs can suppress the synthesis of melatonin, particularly in young population31. Decrease in melatonin level might lead to disruption of sleep cycle, which can aggravate dry eye symptoms49.
The present study has limitations as follows: (1) Data of only 232 participants from only one hospital were included in this study, which is substantially small number to represent the population of paramedical workers in Korea. However, we still believe this study can provide significant information regarding the characteristics of DED in paramedical workers, particularly because it revealed an association between DED and psychological stress. We also believe further studies including larger population group in multiple hospitals are needed to evaluate the characteristics of DED in paramedical workers. (2) Pathophysiology underlying the association between stress and DED is still unclear, and the correlation analysis could not show causative relationship, which necessitate further studies. (3) Diagnosis of DED was made only based on the presence of dry eye symptoms, and examination for dry eye signs was never performed. However, symptom-based approach using DEQs was proven to be highly reliable for identification of DED29. A number of previous studies were successfully conducted using the symptom-based definition of DED using DEQs1,2,6,23,24,25,28. Nevertheless, we still believe that ophthalmologic examination should be incorporated into study protocols for elucidation of the nature of DED in further studies with larger population.
In conclusion, this study showed that DED may be prevalent in paramedical workers in Korea. Psychological stress measured using VAS had significant association with a risk of DED. Female sex was also associated with an increased risk of DED, and prolonged computer use was also possibly associated with DED.
Data Availability
All the data supporting the conclusions of this article is included in the present article.
References
Lin, P. Y. et al. Prevalence of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 110, 1096–101 (2003).
Han, S. B. et al. Prevalence of dry eye disease in an elderly Korean population. Arch Ophthalmol 129, 633–8 (2011).
Amparo, F., Schaumberg, D. A. & Dana, R. Comparison of Two Questionnaires for Dry Eye Symptom Assessment: The Ocular Surface Disease Index and the Symptom Assessment in Dry Eye. Ophthalmology 122, 1498–503 (2015).
Miljanovic, B., Dana, R., Sullivan, D. A. & Schaumberg, D. A. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol 143, 409–15 (2007).
Miljanovic, B. et al. Relation between dietary n-3 and n-6 fatty acids and clinically diagnosed dry eye syndrome in women. Am J Clin Nutr 82, 887–93 (2005).
Uchino, M. et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology 115, 1982–8 (2008).
Baudouin, C. et al. Clinical impact of inflammation in dry eye disease: proceedings of the ODISSEY group meeting. Acta Ophthalmol 96, 111–119 (2017).
Han, S. B., Yang, H. K., Hyon, J. Y. & Wee, W. R. Association of dry eye disease with psychiatric or neurological disorders in elderly patients. Clin Interv Aging 12, 785–92 (2017).
Vehof, J., Kozareva, D., Hysi, P. G. & Hammond, C. J. Prevalence and risk factors of dry eye disease in a British female cohort. Br J Ophthalmol 98, 1712–7 (2014).
Kim, K. W. et al. Association between depression and dry eye disease in an elderly population. Invest Ophthalmol Vis Sci 52, 7954–8 (2011).
Na, K. S. et al. Depression, Stress, Quality of Life, and Dry Eye Disease in Korean Women: A Population-Based Study. Cornea 34, 733–8 (2015).
Uchino, M. et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol 156, 759–66 (2013).
Castellanos-Gonzalez J. A. et al. Prevalence of dry eye syndrome in residents of surgical specialties. 2016; 16: 108.
Smedbold, H. T., Ahlen, C., Norback, D. & Hilt, B. Sign of eye irritation in female hospital workers and the indoor environment. Indoor Air 11, 223–31 (2001).
Vitale, S., Goodman, L. A., Reed, G. F. & Smith, J. A. Comparison of the NEI-VFQ and OSDI questionnaires in patients with Sjogren’s syndrome-related dry eye. Health Qual Life Outcomes 2, 44 (2004).
Han, S. B., Yang, H. K., Hyon, J. Y. & Hwang, J. M. Children with dry eye type conditions may report less severe symptoms than adult patients. Graefes Arch Clin Exp Ophthalmol 251, 791–6 (2013).
Schiffman, R. M. et al. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol 118, 615–21 (2000).
Han, S. B. et al. Reduced corneal sensitivity in patients with primary Sjogren’s syndrome. Acta Ophthalmol 88, e277–8 (2010).
Lesage, F. X., Berjot, S. & Deschamps, F. Clinical stress assessment using a visual analogue scale. Occupational Medicine-Oxford 62, 600–5 (2012).
Lesage, F. X. & Berjot, S. Validity of occupational stress assessment using a visual analogue scale. Occupational Medicine-Oxford 61, 434–6 (2011).
Dutheil, F. et al. At-risk and intervention thresholds of occupational stress using a visual analogue scale. Plos One 12, e0178948 (2017).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J Health Soc Behav 24, 385–96 (1983).
Uchino, M. et al. Japan Ministry of Health study on prevalence of dry eye disease among Japanese high school students. Am J Ophthalmol 146, 925–9 (2008).
The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop Ocul Surf 2007;5:93–107 (2007).
Nichols, K. K., Nichols, J. J. & Mitchell, G. L. The lack of association between signs and symptoms in patients with dry eye disease. Cornea 23, 762–70 (2004).
Schein, O. D. et al. Prevalence of dry eye among the elderly. Am J Ophthalmol 124, 723–8 (1997).
Vehof, J., Sillevis Smitt-Kamminga, N., Nibourg, S. A. & Hammond, C. J. Predictors of Discordance between Symptoms and Signs in Dry Eye Disease. Ophthalmology 124, 280–6 (2017).
Lin, P. Y. et al. Association between symptoms and signs of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Invest Ophthalmol Vis Sci 46, 1593–8 (2005).
Gulati, A. et al. Validation and repeatability of a short questionnaire for dry eye syndrome. Am J Ophthalmol 142, 125–31 (2006).
Uchino, M. et al. The features of dry eye disease in a Japanese elderly population. Optom Vis Sci 83, 797–802 (2006).
Ayaki, M. et al. Gender differences in adolescent dry eye disease: a health problem in girls. Int J Ophthalmol 11, 301–7 (2018).
Asiedu, K., Kyei, S., Boampong, F. & Ocansey, S. Symptomatic Dry Eye and Its Associated Factors: A Study of University Undergraduate Students in Ghana. Eye Contact Lens 43, 262–6 (2017).
Lu CY et al. Personal, Psychosocial and Environmental Factors Related to Sick Building Syndrome in Official Employees of Taiwan. Int J Environ Res Public Health;15 (2017)
Lopez-Miguel, A. et al. Dry eye exacerbation in patients exposed to desiccating stress under controlled environmental conditions. Am J Ophthalmol 157, 788–98 e2 (2014).
Makateb, A. & Torabifard, H. Dry eye signs and symptoms in night-time workers. J Curr Ophthalmol 29, 270–3 (2017).
Fernandez, C. A. et al. Dry eye syndrome, posttraumatic stress disorder, and depression in an older male veteran population. Invest Ophthalmol Vis Sci 54, 3666–72 (2013).
Galor, A. et al. Prevalence and risk factors of dry eye syndrome in a United States veterans affairs population. Am J Ophthalmol 152, 377–84 (2011).
Geva, N., Pruessner, J. & Defrin, R. Acute psychosocial stress reduces pain modulation capabilities in healthy men. Pain 155, 2418–25 (2014).
Cohen, S. et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci USA 109, 5995–9 (2012).
Slavich, G. M. & Irwin, M. R. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull 140, 774–815 (2014).
Shields, G. S. et al. Better cognitive control of emotional information is associated with reduced pro-inflammatory cytokine reactivity to emotional stress. Stress 19, 63–8 (2016).
Research in dry eye: report of the Research Subcommittee of the International Dry Eye WorkShop Ocul Surf 2007;5:179–93 (2007).
Burton, T., Farley, D. & Rhea, A. Stress-induced somatization in spouses of deployed and nondeployed servicemen. J Am Acad Nurse Pract 21, 332–9 (2009).
Vehof, J., Sillevis Smitt-Kamminga, N., Nibourg, S. A. & Hammond, C. J. Sex differences in clinical characteristics of dry eye disease. Ocul Surf 16, 242–8 (2018).
Schaumberg, D. A. et al. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS One 8, e76121 (2013).
Song, J. Y. et al. Association Between Menstrual Irregularity and Dry Eye Disease: A Population-Based Study. Cornea 35, 193–8 (2016).
Kawashima, M. et al. Screening of dry eye disease in visual display terminal workers during occupational health examinations: The Moriguchi study. J Occup Health 57, 253–8 (2015).
Uchino, M. et al. Dry eye disease and work productivity loss in visual display users: the Osaka study. Am J Ophthalmol 157, 294–300 (2014).
Ayaki, M. et al. Sleep and mood disorders in dry eye disease and allied irritating ocular diseases. Sci Rep 6, 22480 (2016).
Acknowledgements
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant No. NRF-2017R1D1A1B03029983).
Author information
Authors and Affiliations
Contributions
(1) Substantial contributions to the conception (J.Y.H.; S.B.H.) or design (J.Y.H.;H.K.Y.; S.B.H.) of the work, or the acquisition (H.K.Y.; S.B.H.), analysis (J.Y.H.; H.K.Y.) or interpretation (J.Y.H.; S.B.H.) of data. (2) Drafting the work (J.Y.H.; H.K.Y.) or revising it critically (S.B.H.). (3) Final approval for submission (J.Y.H.; H.K.Y.; S.B.H.).
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hyon, J., Yang, H. & Han, S. Association between Dry Eye Disease and Psychological Stress among Paramedical Workers in Korea. Sci Rep 9, 3783 (2019). https://doi.org/10.1038/s41598-019-40539-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-40539-0
This article is cited by
-
Association of self-reported psychiatric and systemic risk factors in dry eye disease in adult Korean population
Eye (2024)
-
Prevalence of dry eye disease among Chinese high school students during the COVID-19 outbreak
BMC Ophthalmology (2022)
-
Role of neuroticism and perceived stress on quality of life among patients with dry eye disease
Scientific Reports (2022)
-
Diagnostic ability of maximum blink interval together with Japanese version of Ocular Surface Disease Index score for dry eye disease
Scientific Reports (2020)
-
Eyelid Disorders in Ophthalmology Practice: Results from a Large International Epidemiological Study in Eleven Countries
Ophthalmology and Therapy (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.