Abstract
Vitamin D deficiency is endemic in people living in the Gulf states. We performed a retrospective analysis of data gathered at the first attendance of 82,396 Emirati nationals to outpatient diabetes, endocrinology and general primary care services at two centres in the United Arab Emirates during 2012–2016. Our aim was to explore associations between vitamin D status and markers of cardiovascular and bone health. In the study population, 67.1% of men and 73.5% of women had serum 25(OH)D of less than 50 nmol/L, with the lowest levels being found in young adults. Among Emirati adults with type 2 diabetes, serum 25(OH)D < 50 nmol/L was associated with an increased risk of a coexisting adverse total cholesterol:HDL (TC:HDL) ratio (odds ratio 2.13 (1.60–2.84), p < 0.001). Correcting for age, sex, body mass index, HbA1c and statin therapy, an increase in 25(OH)D of 1 nmol/L was associated with a 0.01 unit reduction in TC:HDL in this population. In a subset of 1064 adult individuals, 25(OH)D < 25 nmol/L was associated with a reduction in DEXA-measured z-score of −0.29 (−0.44 to −0.15, p < 0.001) at the femoral neck and of −0.25(−0.45 to −0.05, p = 0.015) at L1–4, corrected for body mass index, compared with individuals with 25(OH)D ≥ 75 nmol/L. Our findings raise concerns regarding lifetime burden of cardiovascular disease and bone health for young Emiratis with vitamin D deficiency.
Similar content being viewed by others
Introduction
Incident UVB-spectrum sunlight available in the United Arab Emirates (UAE) is sufficient to permit adequate previtamin D3 synthesis throughout the year1. Despite this, deficiency of vitamin D is highly prevalent in the Arab Emirati population2. Although Emirati national dress covers the arms and legs, the face and hands are usually uncovered, and even brief daily exposure of 5% of body surface area to the sun should be sufficient to maintain vitamin D stores3. A culture of sun avoidance has been identified as an important factor predisposing to vitamin D deficiency in the UAE, particularly in young adult Emiratis who express the belief that exposure to sunlight is harmful to health4,5. The high prevalence of vitamin D deficiency reported in young adult Emiratis occurs despite a good understanding among local health professionals of its importance in maintaining bone health in children. Children born in the UAE are routinely prescribed supplementation with 400 international units of vitamin D3 per day until six months of age, but subsequent vitamin D supplementation is voluntary or through fortification of foods. Dietary vitamin D intake alone is, however, known to frequently be inadequate to meet requirements6,7.
Vitamin D deficiency is conventionally defined as a serum 25(OH)D concentration of <50 nmol/l (20 ng/ml), based on the levels at which bone-related symptoms become apparent, and insufficiency as a serum 25(OH)D of 50–75 nmol/l (20–30 ng/ml), determined by the level of vitamin D repletion sufficient for optimum bone health8,9. While severe vitamin D deficiency, defined as serum 25(OH)D < 25 nmol/L (10 ng/mL), is unequivocally linked with childhood rickets and adult osteomalacia10, the clinical impact of milder forms of deficiency and insufficiency, and the prevalence of true deficiency, are the subject of controversy11. Serum 25(OH)D level reflects vitamin D intake and total body vitamin D stores, and is therefore considered to be suitable and sufficient for clinical assessment of vitamin D status8,12.
A wide range of tissues express the vitamin D receptor and vitamin D-responsive elements are present in the promoter regions of over 2000 genes13,14. This has led to speculation that vitamin D status might affect other aspects of homeostasis and metabolism including neoplasia15, hypertension16, β-cell function17, insulin resistance18, and lipid profile19. Both Vitamin D deficiency20,21,22 and atherosclerotic heart disease23 have been reported to be of high prevalence in the Middle East. We hypothesised that vitamin D status and cardiovascular health are positively associated. We also speculated that vitamin D deficiency would be associated with poorer bone health in our population. We have therefore investigated the demographic associations of 25(OH)D sufficiency in the large population of Emirati individuals attending the ICLDC, with particular emphasis on the potential for interaction with other biochemical and metabolic parameters, bone health, and cardiovascular risk.
Methods
Study design and setting
The study was based at the two branches of Imperial College London Diabetes Centre (ICLDC), located in the cities of Abu Dhabi and Al Ain in the United Arab Emirates. ICLDC operates Diabetes, General Endocrinology and Primary Care clinics, with additional specialist clinics in Cardiology and Renal Medicine. Patients attend ICLDC from throughout the Emirates and are predominantly of Arab Emirati origin. Anonymized data from electronic patient records were analysed retrospectively.
Data acquisition and consent
Data were collected from electronic records of patients enrolled at Imperial College London Diabetes Centre (ICLDC). The study followed the ethical guidelines for retrospective studies, approved by the ICLDC Research Ethics Committee. Informed consent for use of clinical data in anonymised form was obtained from the patients at the time of enrolment. Investigations, including vitamin D status and lipid profile are requested as per clinical need and at discretion of the clinician taking care of individual patient. Every measurement of serum 25(OH)D determined in a patient attending ICLDC for the first time between 01/01/2010 and 30/12/2016 (inclusive) was included in the data set. Participants were assigned to subgroups by vitamin D sufficiency status based on serum 25(OH)D level. These groups were defined according to cut-offs commonly used in clinical practise, with severe deficiency of vitamin D defined as serum 25(OH)D < 25 nmol/l, deficiency as 25–49 nmol/L, insufficiency as 50–74 nmol/l and sufficiency as ≥75 nmol/l. Contemporaneous data regarding body mass index (BMI), date of birth, HbA1c, lipid profile, and the use of vitamin D supplementation or active forms of vitamin D were collected for each individual from their electronic record. Laboratory tests were performed using Elecsys Vitamin D total II kit for Cobas platform (Roche Diagnostics, Indianapolis, Indiana). Inter- and intra- assay variability were 10.7% and 4.6%, respectively.
Additionally, we identified electronic records for 5386 DEXA bone densitometry investigations performed using the Lunar Prodigy Advance system (GE Healthcare, Chicago, IL), between 2014-01-05 and 2016-12-29. Mean Z-scores for L1–L4 and femoral neck were acquired by hand for all individuals with recorded serum 25(OH)D < 25 nmol/L (n = 282). The remaining participants were stratified by 10-year age groups and a further 782 records were selected at random from within each group with the aim of obtaining records from equal numbers of individuals in each age range, where possible, giving a sample size of n = 1064.
Inclusion and exclusion criteria
All individuals of Emirati origin irrespective of the glucose tolerance status, who attended ICLDC for the first time between 2010-11-11 and 2016-12-31, and in whom serum 25(OH)D status was assessed, were included. Individuals diagnosed with secondary diabetes or monogenic diabetes were excluded from analysis because of the relatively tiny size of these groups. No limitation was placed on age or body habitus.
Statistical analysis
Data were processed using Microsoft Excel version 15.31 (Microsoft, Redmond) and graphing and statistical analysis were performed using the R Language for Statistical Computing version 3.4 (R Core Team, Vienna, Austria)24. Where parameters were skewed, they were log-transformed for inclusion in regression analyses. Correcting for multiple statistical tests and assuming a total of fifty tests would be performed, the threshold for significance was set at p = 0.001.
Results
25(OH)D status in the study population
The baseline characteristics of the 81598 participants overall and by categories of 25(OH)D are summarised in Table 1. The overall prevalence of serum 25(OH)D < 25 nmol/L was 28.8% (Males: 19.9%, Females: 34.2%). A further 42.2% (Males: 47.2%, Females: 39.2%) presented with serum 25(OH)D between 25 and 50 nmol/L. In total, 67.1% of Emirati men and 73.5% of Emirati women presented with serum 25(OH)D of <50 nmol/L. Vitamin D supplements were frequently prescribed, with 69.9% of patients already taking cholecalciferol or ergocalciferol equivalent to at least 400 international units per day at the first presentation. The relationships between serum 25(OH)D, age, and sex are illustrated in Fig. 1. Adjusting for the month in which sampling occurred, serum 25(OH)D decreased by 3.1 (3.1 to 3.2) nmol/L per year between infancy and age 18, while male sex was associated with a 6.4 (5.9 to 7.0) nmol/L higher serum 25(OH)D (all p < 0.001, adjusted R2 0.42; see Supplementary Table 1).
Adjusting for the effects of body mass index, sex, glycaemic status and month of sampling on serum 25(OH)D in Emirati adults aged ≥18 year, each one year of age was associated with an increase in serum 25(OH)D of 0.68 (0.67 to 0.7) nmol/L, while each 1 kg/m2 increase in body mass index was associated with a reduction in serum 25(OH)D of 0.35 (0.38 to 0.32) nmol/L. Male sex was associated with a 2.34 (1.94 to 2.73) nmol/L increase in serum 25(OH)D. The presence of a prediabetic state or type 2 diabetes were associated with reductions in 25(OH)D of 1.98 (1.5 to 1.98) nmol/L, and 1.85 (1.27 to 2.43) nmol/L, respectively, when compared with normal glucose tolerance (p < 0.001). Type 1 diabetes was not associated with a significant change in serum 25(OH)D. The overall model fit was poor, with the covariates together accounting for 13.2% of the variation seen in serum 25(OH)D (Supplementary Table 2).
25(OH)D status, PTH and bone profile in the study population
Serum parathyroid hormone (PTH), corrected calcium (Ca2+), phosphate (PO4) and alkaline phosphatase (ALP) were measured in a subset of the population aged >20 years; younger individuals were excluded due to the effects of growth on ALP and PO4. Median values for each parameter are presented in Table 2 along with the number of participants with available information. Kruskal-Wallis tests indicated significant differences in each parameter according to vitamin D status (p < 0.001 for each). Pairwise Mann-Whitney U tests with Bonferroni correction for multiple comparisons were performed to determine the significance of differences between groups. PTH was significantly lower in the individuals with serum 25(OH)D of ≥75 nmol/L than in each other group (all p < 0.001), while PTH was also significantly higher in each sufficiency group than the next higher group (25–49 nmol/L cf 50–74 nmol/L p < 0.001, <25 nmol/L cf 25–49 nmol/L p < 0.001).
Serum Ca2+ was significantly higher in Emirati adults with serum 25(OH)D ≥ 75 nmol/L (all p < 0.001, n = 52618,), while serum ALP was significantly lower (all p < 0.001, n = 24802,) than in each of the other vitamin D status groups. Serum phosphate was significantly higher in individuals with serum 25(OH)D ≥ 75 nmol/L than in individuals with serum 25(OH)D ≤ 49 nmol/L (p < 0.001, n = 52619).
DEXA Bone densitometry reports were examined in 1064 individuals, selected as described in the Methods section, and Z-scores based on Western values for age-matched bone mineral density were recorded for mean lumbar spine (L1–L4) and mean femoral neck, along with serum 25(OH)D at first presentation. In male participants (n = 268), mean Z-score for L1–4 was −0.33 ± 1.40 and mean Z-score for femoral neck was −0.24 ± 1.06, while in female participants (n = 796), mean Z-score for L1–4 was −0.51 ± 1.25 and mean Z-score for femoral neck was −0.19 ± 0.88. Z-score is a measure of the number of standard deviations from the age-adjusted mean and therefore, in a healthy population and with suitable reference values, it would be expected that mean Z-score would be 0.0 with standard deviation of 1.0. Correcting for the effect of body mass index using linear regression, serum 25(OH)D was significantly and positively associated with bone mineral density at the femoral neck, albeit with a small effect size. A 10 nmol/L increase in 25(OH)D was associated with an increase in Z score at the femoral neck of 0.01 (p < 0.001; Supplementary Table 3). This result should be interpreted with considerable caution since the models explained only 3% of the variability of z-score. Inclusion of log-transformed PTH in normocalcaemic individuals greatly improved model fit such that 8% of the variability of the Z-score at the femur was explained (Supplementary Table 4), with the significant limitations that, due to missing data, only 508 individuals were included, that 25(OH)D was not a significant predictor in this model, and that PTH reflects both vitamin D status and dietary calcium intake in normocalcaemic individuals.
25(OH)D status and cardiovascular risk profile in Emirati adults with type 2 diabetes
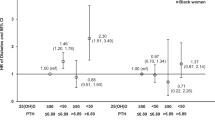
We examined the relationship between vitamin D status and lipid profile in 14559 participants with a diagnosis of type 2 diabetes. Serum 25(OH)D of <50 nmol/L is commonly considered to indicate vitamin D deficiency in routine clinical practice. The ratio of total cholesterol to HDL (TC:HDL) is considered a marker of metabolic health, with higher values denoting increased risk of cardiovascular disease. The median TC:HDL was 3.59 (2.93–4.51) in individuals with serum 25(OH)D < 50 nmol/L and 4.24 (3.39–5.3) in individuals with serum 25(OH)D > 50 nmol/L (p < 0.001). Median TC:HDL ratios, grouped by serum 25(OH)D level, are presented in Fig. 2.
Lipid status by 25(OH)D status in 14559 Emirati individuals with a diagnosis of type 2 diabetes. (1) Total cholesterol: high density lipoprotein (TC:HDL) ratio, four outlying values excluded, (2) Serum HDL (mmol/L), three outlying values excluded, (3) Serum LDL (mmol/L), (4) Log-transformed serum triglycerides (mmol/L). Tukey plots represent median, interquartile range, 25th percentile −1.5 * IQR and 75th percentile +1.5 * IQR. All differences between individual groups were highly significant, (p < 0.0001, multiple Mann-Whitney U tests with correction for multiple comparisons). Only pairwise comparisons between the ≥75 nmol/L group and each other group are included for clarity.
Per data from the Framingham Study25, TC:HDL < 3.4 in women or <3.5 in men is associated with a 50% reduction in cardiovascular risk, while TC:HDL ≥ 7.0 in women or ≥9.6 in men is associated with a two-fold increase in cardiovascular risk. The proportions of participants who had favourable or unfavourable lipid profiles are presented in Table 3, grouped by serum 25(OH)D level. Among participants with 25(OH)D < 50 nmol/L, 2448 (26.5%) had an favourable TC:HDL ratio, compared with 2574 (44.6%) in those with 25(OH)D ≥ 50 nmol/L. This difference in proportions was significant (p < 0.001, 2.23 (2.08–2.39), chi-square test). Conversely, individuals with 25(OH)D < 50 nmol/L were significantly more likely to have an unfavourable TC:HDL ratio than those serum 25(OH)D > 50 nmol/L (p < 0.001, OR 2.13 (1.60–2.84), chi-square test).
Correcting for the potential effects of body habitus, glycaemic control, sex, statin treatment, and age on the relationship between TC:HDL ratio and serum 25(OH)D in 14579 individuals with type 2 diabetes in linear regression, a serum 25(OH)D of less than 50 nmol/L was independently associated with an increase in TC:HDL ratio of 0.43 (95% CI 0.38–0.48) (p < 0.001; see Supplementary Table 5). Serum 25(OH)D was negatively associated with TC:HDL (10 nmol/L increase in 25(OH)D associated with a 0.1 unit reduction in TC:HDL, p < 0.001; see Table 4).
Discussion
The prevalence and patterns of vitamin D deficiency and insufficiency we found in Emirati nationals attending outpatient services were comparable with reports from the Middle East and North Africa (MENA) area. Between 30.7 and 61.8% of residents in the Lebanon, and 50–63% of residents of Jordan are reported to be deficient or insufficient in vitamin D20. 72.1% of a population of female students attending a high school in Iran were reported to have vitamin D deficiency21, while 81% of female students aged 12–15 attending a school in the Kingdom of Saudi Arabia were reported to have serum 25(OH)D of less than 25 nmol/L22. Only a limited number of studies have specifically investigated the prevalence of, and local factors associated with, vitamin D deficiency in the United Arab Emirates. One study conducted in Al Ain demonstrated hypovitaminosis D in 65.1% of a population of 143 adolescents, with vitamin D deficiency ≤ 50 nmol/l in 10% of boys and 28% of girls26. Vitamin D status was found to be paradoxically lower in summer than in winter in a population of 138 female university students in Abu Dhabi, attributed to high levels of sun avoidance and high outside temperatures; sun avoidance was independently negatively correlated with serum 25(OH)D levels4. 31.2% of children aged 8–14 attending an ambulatory clinic at Sheikh Khalifa Medical City in Abu Dhabi had serum 25(OH)D measured at <25 nmol/l27. In 141 indoor workers resident in the UAE, median 25(OH)D was reported as 22.4 nmol/l, with 63.2% being severely deficient and 29.1% deficient in vitamin D, and serum 25(OH)D was correlated with a 5-point scoring system rating sun-avoidant behaviours28. In the Emirati population we studied, 71.05% presented with serum 25(OH)D < 50nmol/l.
Our findings support the conclusion that, although the clinical impact of vitamin D insufficiency and moderate deficiency remains the source of some debate, serum 25(OH)D below 75 nmol/L is associated with small but statistically significant differences in serum parathyroid hormone, corrected calcium and alkaline phosphatase. In keeping with this finding, lower serum vitamin D was associated with a reduction in age-adjusted bone mineral density at femoral neck when corrected for body mass index. It remains possible that the coexisting clinical indications warranting investigation in the subset of individuals who underwent bone densitometry may have masked the impact of vitamin D status. Previous studies reports a lack of concordance between densitometry and vitamin D status in Hungarian men29 and American men of black or Hispanic origin30, although an association between bone mineral density at the hip and vitamin D status was found in a multinational cohort of postmenopausal women31. Comprehensive reference ranges for bone mineral density are not available for the Emirati population, and a PubMed search did not identify any studies specifically exploring the association between vitamin D status and bone mineral density in Arabic populations.
Our finding that low serum 25(OH)D is associated with a less favourable lipid profile is consistent with the previously published results of observational studies. In 107,811 American patients, 25(OH)D < 50 nmol/L was associated with lower HDL, higher LDL, higher total cholesterol and higher triglycerides32. Plasma 25(OH)D was positively associated with HDL in 237 children and adolescents living in the United States33. Low circulating 25(OH)D has been associated with an increased risk of myocardial infarction in men and with increased prevalence of cardiovascular disease in adult men and women34,35. Vitamin D supplementation has not, however, yet been demonstrated to provide beneficial effects on lipid profile and cardiovascular outcomes, although the randomized controlled trials performed to date have been relatively small and heterogeneous in their interventions and study populations36.
The relationship of 25(OH)D to age in our study population suggests that, although vitamin D supplementation for infants is effective, vitamin D status declines rapidly in childhood and young adulthood, especially young women. The most plausible explanation for this would appear to be sun avoidance in this population, while the increase in median 25(OH)D with age in older adults may be explained by differing attitudes to sun exposure and to incidental identification of vitamin D deficiency during treatment for other conditions. This raises two concerns for population health, which require further study. Firstly, adequate vitamin D status in pregnant women is important because of the associated risk of neonatal hypocalcaemia and tetany37, which is particularly prevalent in women with diabetes mellitus due to associated prematurity, hypomagnesemia and hyperparathyroidism38. Secondly, the association between vitamin D deficiency and an unfavourable lipid profile is cause for concern because of the possibility that young people who are vitamin D deficient could suffer from an increased risk of cardiovascular disease later in life. Diseases of the circulatory system are already the most common cause of death in Emirati nationals, accounting for 35% of deaths in 20152.
Owing to the retrospective nature of our study, there are certain limitations and potential sources of bias. Due to the extremely large size of the data set, it was necessary to choose a single attendance from several within the time period, and data regarding each individual’s diagnosis and treatment prior to attendance at ICLDC were not accessible electronically. The median age of participants was 43.7 years, which is older than the estimated overall median age of 30 years of the Emirati population. The included participants were patients attending a clinic rather than being randomly selected, which would increase the prevalence of coexisting illnesses, treatments, and other confounders. Due to the specialization of ICLDC, a large proportion of the sample consisted of people with type 2 diabetes; the International Diabetes Federation estimates the prevalence of diabetes mellitus in adults resident in the UAE at 14.6%, whereas 18.4% of the study population were diagnosed with type 2 diabetes, 1.4% with type 1 diabetes, 21.0% with impaired fasting glucose or impaired glucose tolerance and 59.2% with normal glucose tolerance. However, one strength of the study design is the large proportion of all Emirati individuals included; Health Authority Abu Dhabi (HAAD) estimated the total number of Emirati Nationals living in the UAE in 2014 at 524,0232, and consequently the data set presented here represents up to 15.6% of the entire population.
To conclude, Vitamin D deficiency is highly prevalent in Emirati nationals attending primary care services. The effects on biochemical parameters including lipid profile raise concerns regarding a possible effect on the future cardiovascular health of the United Arab Emirates. Longitudinal research regarding the effectiveness of vitamin D supplementation on lipid profile and cardiovascular risk in the Emirati population is needed.
References
Buckley, A. J., Hannoun, Z., Lessan, N., Holick, M. F. & Barakat, M. T. Environmental determinants of previtamin D synthesis in the United Arab Emirates. Dermato-Endocrinology 9, e1267079, https://doi.org/10.1080/19381980.2016.1267079 (2017).
AbuDhabi, H. A. o (2016).
Osmancevic, A. et al. Vitamin D production after UVB exposure–A comparison of exposed skin regions. Journal of Photochemistry and Photobiology B: Biology 143, 38–43 (2015).
Thomas, J., Alanouti, F., Campbell, C. & Ameri, S. A. Exploring sun avoidant attitudes and behaviors in the United Arab Emirates. Social Behavior and Personality: an international journal 38, 1111–1118 (2010).
Al Anouti, F. et al. Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates. Dermato-endocrinology 3, 235–239 (2011).
Hollis, B. W. Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D. The Journal of nutrition 135, 317–322 (2005).
Wacker, M. & Holick, M. F. Sunlight and Vitamin D: A global perspective for health. Dermato-endocrinology 5, 51–108 (2013).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. The. Journal of Clinical Endocrinology & Metabolism 96, 1911–1930 (2011).
Priemel, M. et al. Bone mineralization defects and vitamin D deficiency: Histomorphometric analysis of iliac crest bone biopsies and circulating 25‐hydroxyvitamin D in 675 patients. Journal of Bone and Mineral Research 25, 305–312 (2010).
Holick, M. F. The vitamin D deficiency pandemic: a forgotten hormone important for health. Public health reviews 32, 267 (2010).
Manson, J. E., Brannon, P. M., Rosen, C. J. & Taylor, C. L. Vitamin D deficiency—is there really a pandemic? New England Journal of Medicine 375, 1817–1820 (2016).
Carter, D. G. Accuracy of 25-hydroxyvitamin D assays: confronting the issues. Current drug targets 12, 19–28 (2011).
Hossein-Nezhad, A., Spira, A. & Holick, M. F. Influence of vitamin D status and vitamin D3 supplementation on genome wide expression of white blood cells: a randomized double-blind clinical trial. Plos one 8, e58725 (2013).
Neme, A., Seuter, S. & Carlberg, C. Selective regulation of biological processes by vitamin D based on the spatio-temporal cistrome of its receptor. Biochimica et Biophysica Acta (BBA)-Gene Regulatory Mechanisms 1860, 952–961 (2017).
Verlinden, L. et al. Action of 1, 25 (OH) 2D3 on the cell cycle genes, cyclin D1, p21 and p27 in MCF-7 cells. Molecular and cellular endocrinology 142, 57–65 (1998).
Forman, J. P. et al. Effect of Vitamin D Supplementation on Blood Pressure in BlacksNovelty and Significance. Hypertension 61, 779–785 (2013).
Mitri, J., Dawson-Hughes, B., Hu, F. B. & Pittas, A. G. Effects of vitamin D and calcium supplementation on pancreatic β cell function, insulin sensitivity, and glycemia in adults at high risk of diabetes: the Calcium and Vitamin D for Diabetes Mellitus (CaDDM) randomized controlled trial–. The American journal of clinical nutrition 94, 486–494 (2011).
Belenchia, A. M., Tosh, A. K., Hillman, L. S. & Peterson, C. A. Correcting vitamin D insufficiency improves insulin sensitivity in obese adolescents: a randomized controlled trial–. The American journal of clinical nutrition 97, 774–781 (2013).
Lupton, J. R. et al. Deficient serum 25-hydroxyvitamin D is associated with an atherogenic lipid profile: The Very Large Database of Lipids (VLDL-3) study. Journal of clinical lipidology 10, 72–81. e71 (2016).
Arabi, A., El Rassi, R. & Fuleihan, G. E.-H. Hypovitaminosis D in developing countries—prevalence, risk factors and outcomes. Nature Reviews Endocrinology 6, 550 (2010).
Moussavi, M., Heidarpour, R., Aminorroaya, A., Pournaghshband, Z. & Amini, M. Prevalence of vitamin D deficiency in Isfahani high school students in 2004. Hormone Research in Paediatrics 64, 144–148 (2005).
Siddiqui, A. M. & Kamfar, H. Z. Prevalence of vitamin D deficiency rickets in adolescent school girls in Western region, Saudi Arabia. Saudi medical journal 28, 441–444 (2007).
Raal, F. J. et al. Cardiovascular risk factor burden in Africa and the Middle East across country income categories: a post hoc analysis of the cross-sectional Africa Middle East Cardiovascular Epidemiological (ACE) study. Archives of Public Health 76, 15, https://doi.org/10.1186/s13690-018-0257-5 (2018).
Team, R. C. R A language and environment for statistical computing (2013).
Abbott, R. D., Wilson, P. W., Kannel, W. B. & Castelli, W. P. High density lipoprotein cholesterol, total cholesterol screening, and myocardial infarction. The Framingham Study. Arteriosclerosis, Thrombosis, and Vascular Biology 8, 207–211 (1988).
Muhairi, S. J. et al. Vitamin D deficiency among healthy adolescents in al ain, united arab emirates. BMC Public Health 13, 33 (2013).
Rajah, J., Haq, A. & Pettifor, J. M. Vitamin D and calcium status in urban children attending an ambulatory clinic service in the United Arab Emirates. Dermato-endocrinology 4, 39–43 (2012).
Al-Anouti, F. et al. Sun avoidance among indoor employees leading to vitamin D deficiency and depression in the United Arab Emirates. International Journal of Medicine and Medical Sciences 5, 503–509 (2013).
Bhattoa, H. et al. Prevalence and seasonal variation of hypovitaminosis D and its relationship to bone metabolism in healthy Hungarian men over 50 years of age: the HunMen Study. Osteoporosis International 24, 179–186 (2013).
Hannan, M. T. et al. Serum 25-hydroxyvitamin D and bone mineral density in a racially and ethnically diverse group of men. The Journal of Clinical Endocrinology & Metabolism 93, 40–46 (2008).
Lips, P. et al. A global study of vitamin D status and parathyroid function in postmenopausal women with osteoporosis: baseline data from the multiple outcomes of raloxifene evaluation clinical trial. The Journal of Clinical Endocrinology & Metabolism 86, 1212–1221 (2001).
Ponda, M. P., Huang, X. X., Odeh, M. A., Breslow, J. L. & Kaufman, H. W. Vitamin D may not improve lipid levels: a serial clinical laboratory data study. Circulation, CIRCULATIONAHA. 111, 077875 (2012).
Rajakumar, K. et al. Vitamin D status, adiposity, and lipids in black American and Caucasian children. The. Journal of Clinical Endocrinology & Metabolism 96, 1560–1567 (2011).
Giovannucci, E., Liu, Y., Hollis, B. W. & Rimm, E. B. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Archives of internal medicine 168, 1174–1180 (2008).
Kendrick, J., Targher, G., Smits, G. & Chonchol, M. 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis 205, 255–260 (2009).
Challoumas, D. Vitamin D supplementation and lipid profile: what does the best available evidence show? Atherosclerosis 235, 130–139 (2014).
Thomas, T. C., Smith, J. M., White, P. C. & Adhikari, S. Transient neonatal hypocalcemia: presentation and outcomes. Pediatrics 129, e1461–e1467 (2012).
Tsang, R. C. et al. Parathyroid function in infants of diabetic mothers. The Journal of pediatrics 86, 399–404 (1975).
Acknowledgements
The authors wish to acknowledge Prof. Munir Ahmad and Ms Amal Hussein for the input into the statistical aspects of the manuscript. This research was funded by Imperial College London Diabetes Centre, a Mubadala Company.
Author information
Authors and Affiliations
Contributions
A.J.B. collected data, performed the statistical analysis and wrote the manuscript. N.L. reviewed and contributed to the manuscript. M.F.H. reviewed and contributed to the manuscript. M.T.B. reviewed and contributed to the manuscript. A.J.B. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the analysis.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Buckley, A.J., Barakat, M.T., Holick, M.F. et al. Parameters of Bone and Cardiovascular Health Related to 25-Hydroxyvitamin D Status in Emirati Nationals attending Primary Care and Diabetes services: a retrospective cohort study. Sci Rep 9, 3835 (2019). https://doi.org/10.1038/s41598-019-40523-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-40523-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.