Abstract
Congenital heart disease (CHD) often requires surgical intervention, and is sometimes associated with life-threatening post-operative complications. We have investigated some factors of the innate immune system involved in the initiation or regulation of complement lectin pathway activation (MASP-1, MASP-2 MASP-3, MAp19, MAp44, ficolin-3) and related them to complications and prognosis in 190 pediatric patients undergoing CHD repair with the use of cardiopulmonary bypass (CPB). Patients with MAp44 levels ≤1.81 µg/ml more frequently experienced low cardiac output syndrome (LCOS), renal insufficiency, systemic inflammatory response syndrome (SIRS) and multiorgan dysfunction (MODS). Low MASP-3 (≤5.18 µg/ml) and high MASP-1 (≥11.7 µg/ml) levels were often associated with fatal outcome. Low ficolin-3 concentrations (≤10.1 µg/ml) were more common among patients experiencing SIRS and MODS than in those without complications. However, patients suffering from SIRS and MODS with low ficolin-3 had a much better prognosis (91% survival vs. 37% among other patients; p = 0.007). A discriminating value of 12.7 µg/ml ficolin-3 yielded 8% vs. 60% mortality (p = 0.001). Our data extend the knowledge concerning involvement of proteins of the lectin pathway in development of post-CPB complications. The potential prognostic value of low preoperative MAp44 and high preoperative ficolin-3 seems promising and warrants independent confirmation.
Similar content being viewed by others
Introduction
Congenital heart disease (CHD) is a leading cause of infant mortality1. Its incidence differs among various populations, but generally, it is estimated as 10–12/1000 live births, corresponding to approx. 1.3 million cases worldwide yearly2. Some less severe defects may be consistent with relatively good health and a normal life, but others require surgery (approx. 25%) or other interventions during the first year of life. Some patients suffer from life-threatening post-operative complications, prolonging intensive care unit stay and increasing costs of the therapy3. Patients may be affected by hospital-acquired infections, low cardiac output syndrome (LCOS) and systemic inflammatory response syndrome (SIRS) which may further lead to multiple organ dysfunction syndrome (MODS). The inflammation occurring after cardiac surgery and cardio-pulmonary bypass (CPB) involves multiple cellular and humoral pathways, among which the complement system plays a central role4. Three major complement activation pathways have been described: the classical (CP), the alternative (AP) and the lectin pathway (LP). The last is activated by specific pattern-recognition molecules (PRMs), i.e., ficolins and some collectins, complexed with enzymes belonging to the MASP (mannose-binding lectin serine protease) family. The involvement of the mannose-binding lectin (MBL)-dependent lectin pathway activation in the inflammatory response following CPB has been documented by us previously5,6. Therefore we decided to investigate the significance of particular MASPs and related non-enzymatic (regulatory) proteins. Furthermore, we investigated ficolin-3 (H-ficolin) as the most abundant lectin pathway-associated PRM.
Serine proteases (MASP-1, MASP-2, MASP-3) and non-enzymatic MAp44 (also termed MAP-1) and MAp19 (or sMAP) are in turn complexed with ficolins/collectins, enabling an initiation of complement activation, its regulation and/or cross-talk with other cascades like coagulation system. MASP-1, MASP-3 and MAp44 are products of alternative splicing of RNA of the MASP1/3 gene whereas MASP-2 and MAp19 are splice variants of RNA of the MASP2 gene7,8. PRM-MASP complexes are considered important players of the first-line antimicrobial innate immune defense. Beside microbial structures, their activation can be triggered by apoptotic cells, necrotic debris or other aberrant self-structures9. Auto-activated MASP-1 is responsible for MASP-2 activation as well as for cleaving of C4-bound complement component C210. MASP-2 activates C4 and C4-bound C211. A substrate for the MASP-3 protease is profactor D, which leads to generation of factor D, an enzyme involved in the initiation of the alternative pathway of complement12,13. On the other hand, MASP-3 has also been suggested to hinder the LP cascade7,14. Similar inhibitory activity was proposed also for MAp4415. Although MAp19 was thought to be a LP regulatory factor as well, its biological significance remains to be clarified, since in physiological conditions it did not influence C4 cleavage product deposition16. MASP-1 and MASP-2 may contribute to thrombogenesis from their ability to cleave fibrinogen, factor XIII, prothrombin and thrombin activatable fibrinolysis inhibitor (TAFI)17,18,19.
Factors influencing MASP/MAp and ficolin-3 synthesis are still unknown, however major surgery was associated with a drop in ficolin-3, MASP-1, -2, -3 and MAp44 concentrations within 12–48 h20,21,22,23. However, in contrast to MASP-3, a marked increase of MASP-1 and MAp44 within 4–20 post-operative days was observed, suggesting they could be acute phase proteins20,21. Furthermore, MASP-2 was suggested to be an acute-phase reactant based on data from patients with acute pancreatitis24.
Here we report an investigation of pre-operative serum MASP-1, MASP-2, MASP-3, MAp44, MAp19 and ficolin-3, concentrations and their possible influence on the incidence of post-operative complications in infants and children operated on because of congenital heart disease. As our study has strictly been focused on the understanding of involvement of complement lectin pathway in complications after CHD repair, we have not recruited healthy controls.
Material and Methods
Patients
One hundred and ninety patients (77 girls and 113 boys), aged from 3 months to 17 years (mean: 3 years and 4 months), undergoing primary cardiac surgery for the reason of CHD, with the use of CPB were recruited. Seventy-nine patients (aged from 3 to 12 months) were defined as infants while 111 were defined as older children. There were no differences in male/female ratio between age groups.
The types of CHDs diagnosed as well as other clinical and demographic data are listed in Table 1. Basic Aristotle Score (BAS) was used for evaluation of surgical procedure complexity, potential for mortality and morbidity as well as technical difficulty25. Exclusion criteria were: need for pre-operative mechanical ventilation, pre-operative infection or organ dysfunction, and death during surgery. The post-operative course was observed and documented until hospital discharge. Patients were screened for symptoms of post-operative complications (infection, SIRS, LCOS, organ dysfunctions), essentially as described previously5,6.
Cardiovascular status was assessed using the vasoactive inotropic score (VIS)26. SIRS was diagnosed according to Goldstein et al.27, and multiorgan dysfunction (MODS) when dysfunction of at least two organs was observed. Low cardiac output syndrome (LCOS) was defined according to clinical criteria including: tachycardia, poor peripheral perfusion, hypotension, need for introducing new inotropic agent or increase doses twice, oliguria, cardiac arrest, elevated lactates. Hepatic dysfunction was defined as prothrombin time at least 2x normal and ALT > 100 IU/l; renal insufficiency was defined as the need for renal replacement therapy. The approval of the Bioethical Committee of the Polish Mother’s Memorial Hospital Research Institute and written informed parental consent were obtained. This work conforms to the provisions of the Declaration of Helsinki.
Clinical material
Serum samples were obtained from blood taken in the operating room just before cardiac surgery into tubes without anticoagulant5,6 and then kept at 4 °C for 30 min for clotting, centrifugated, distributed to Eppendorf tubes and stored at −80 °C.
Determination of ficolin-3 and MASP family proteins serum concentrations
Serum levels of the MASP family proteins were determined using assays described elsewhere: for MASP-128, MASP-229, MASP-320, MAp4420 and MAp1916. Ficolin-3 concentrations were measured by ELISA as described previously30 with later modification29. For some analyses, cut-off values out of interquartile range (IQR; lower or higher) were chosen arbitrarily. They are presented in Table S1.
Statistical analysis
The Shapiro-Wilk test was used to determine normality. As the distribution of pre-operative levels of tested proteins was not normal (see below), the medians were compared using the Mann-Whitney U-test. The frequencies of low or high protein concentrations, as well as post-operative complications were compared by χ2 test or χ2 test with Yates correction (depending on expected value) and in smaller groups (n < 40) by two-sided Fischer’s exact test. Correlations were determined by Spearman’s test. P values < 0.05 were considered statistically significant.
Results
Basic clinical data
The types of CHDs diagnosed as well as other clinical and demographic data are listed in Table 1. The most common procedures were: bidirectional Glenn, Fontan operation, Ross operation, correction of tetralogy of Fallot, ventricular septal defect (VSD) repair, atrial septal defect repair, atrioventricular canal (CAV) defect repair. Mean CPB time was 85.9 minutes (±42.4) and mean aorta cross-clamping time was 42.9 min (±27.2).
The Basic Aristotle Score, reflecting surgery technical difficulties and the risk of complications, was significantly higher in the older children (p < 0.0001). They also more often required pharmacological cardiovascular support (VIS) after surgery (p = 0.0002) and were more frequently diagnosed with post-operative renal insufficiency [OR = 3.81, 95% CI (1.06–13.6), p = 0.029] or liver failure [OR = 2.88, 95% CI (1.11–7.47), p = 0.025] in comparison to infants and they needed markedly longer stays in hospital (p = 0.009).
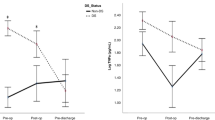
Pre-operative concentrations of lectin pathway-associated proteins in infants and older children
The pre-operative serum concentrations of MASP-1, MASP-2, MASP-3, MAp44, MAp19 and ficolin-3 were estimated in both groups of patients (Fig. 1). MASP-1 and MAp44 were slightly but significantly higher in infants while the opposite was true for MASP-3. Consistently with this, MASP-3 correlated positively while MASP-1 and MAp44 – inversely, with age. Serum MAp44 significantly correlated with the majority of other proteins tested (except for MASP-2), and most strongly with MASP-1 (Table S2).
Serum MAp44 and MASP-3 concentrations correlated inversely with surgical complexity (BAS) in older children, whereas Map44, MASP-3 and MAp19 correlated inversely with the need for pharmacological cardiovascular support (VIS) (Table 2).
Pre-operative concentrations of lectin pathway-related proteins and post-operative complications
To analyze the possible associations of pre-operative concentrations of lectin pathway factors with post-operative complications, data from patients with such events as fever, infections, SIRS, SIRS accompanied with MODS, LCOS, liver failure, renal insufficiency, and those without complications were compared. Furthermore, the results from survivors and non-survivors were analyzed. No significant differences in patient’s age or BAS were noted between the subgroups being compared (not shown). On the other hand, median VIS was significantly higher in patients suffering from each of those post-operative complications, in comparison with the reference group (p < 0.0001). Moreover, as expected, the stay at ICU and in the hospital in general, was significantly longer in patients with post-operative complications (not shown).
MASP-1, MASP-2 and MASP-3
Median MASP-1, MASP-2 and MASP-3 concentrations in patients with no complications were 7.5 µg/ml, 0.25 µg/ml and 6.2 µg/ml, respectively (Table 3). MASP-3 levels were significantly lower in patients who died as a result of post-operative complications in comparison with survivors (5.4 μg/ml vs. 6.3 μg/ml, p = 0.027). Moreover, patients with low MASP-3 (<5.18 µg/ml) had generally a worse prognosis than those with higher values [22.2% vs. 7.2% deaths (OR = 3.67, 95% CI, 1.04–12.9)].
Additionally, children with the highest levels of MASP-1 (≥90th percentile, 11.68 µg/ml), had a much lower rate of survival compared with individuals with lower MASP-1 concentrations. No such relationship was found in the case of MASP-2 (data not shown).
MAp44 and MAp19
Median pre-operative concentrations of MAp44 and MAp19 among patients who did not suffer from post-operative complications were 2.33 µg/ml and 0.36 µg/ml, respectively (Table 3). In the case of MAp44, the median was significantly lower in patients experiencing post-operative LCOS, SIRS and/or organ dysfunctions whereas lower MAp19 was associated with patients with fever (Table 3). Furthermore, for older children, lower MAp19 levels were associated with SIRS, (accompanied or not with multiorgan dysfunction), single organ dysfunctions and LCOS (not shown).
These relationships were confirmed by analysis of low serum concentrations of MAp44 and MAp19 (Table 4). The patients with low MAp44 more frequently experienced post-operative LCOS, renal insufficiency, SIRS and SIRS + MODS. Low MAp19 concentrations were markedly more common among patients with fever.
Ficolin-3
Median pre-operative ficolin-3 concentration did not differ significantly between the group of patients who were discharged from the hospital with no post-operative complications and any group experiencing any of the complications analyzed (Table 3).
However, low ficolin-3 was more common among patients suffering from SIRS + MODS (p = 0.027, Table 4). Yet within this (SIRS + MODS) subgroup, those who died had significantly higher pre-operative ficolin-3 levels than survivors [medians: 14.8 µg/ml (n = 11) vs. 8.4 µg/ml (n = 16); p = 0.03]. Indeed, patients who developed SIRS and MODS with ficolin-3 levels ≤ 25th percentile had generally a much better prognosis [91% survival vs. 37%; OR = 16.7; 95% CI (1.7–164.9); p = 0.007]. Conversely, an adverse effect was observed for patients with ficolin-3 ≥75th percentile compared with those <75th percentile: 20% vs. 82% survival [OR = 0.05; 95% CI (0.007–0.39); p = 0.003]. These findings prompted us to perform a ROC analysis, to find the best discriminating value in relation to survival. The best fit was found to be 12.7 µg/ml (AUC = 0.75; sensitivity 90.9%; specificity 75%). Using this value, it was calculated once again that low ficolin-3 concentrations are associated with lower mortality in patients who developed SIRS and MODS [92% survival compared with 29% among patients with ficolin-3 above 12.7 µg/ml; OR = 30.0; 95% CI (2.9–313.7); p = 0.001].
The 12.7 µg/ml cut-off also has prognostic value when any post-operative complication co-exists [survival: 94% vs. 73% when compared with patients without any post-operative complications; OR = 5.9 95% CI (1.2–28.4); p = 0.02], but not for the patient cohort in total (96% vs. 88% survival; p = 0.11).
Discussion
Post-bypass systemic inflammatory response and other complications are still a problem in cardiac surgery. The incidence of post by-pass SIRS in pediatric patients is estimated to be between 8.9 and 30.5%31,32. It often has a fatal outcome and is associated with organ injury, longer ICU and total hospital stays. Complement activation has been considered one of the key mechanisms responsible for the development of post-CPB inflammatory response. In the last 2 decades, the significance of the lectin pathway has been taken into account. Our previous reports evidenced MBL-dependent LP activation during cardiac surgery using cardiopulmonary bypass and the contribution of this phenomenon to the development of post-operative SIRS. We observed also that MBL2 genotypes and MBL pre-operative serum levels correlate with the risk of various post-bypass complications5,6. Furthermore, we found deposition of MBL and ficolins as well as deposition of C4 activation products on the surface of polyurethane tubing routinely used for CPB33. Here we reported data concerning other lectin pathway-associated proteins: MASP-1 (crucial for the initiation of the cascade), MASP-2 (responsible for C4 cleavage) as well as MASP-3, non-proteolytic MAp44 and MAp19 (as regulatory factors) as well as ficolin-3 (the most abundant LP-related PRM). It should be also stressed that afore-mentioned MASP cross-talk with alternative pathway activation and/or coagulation cascade/kinin system might contribute to amplification of some adverse effects.
The high expression of MAp44 mRNA in the heart and its significance for cardiac development provokes particular attention14,34,35. Our data demonstrated that individuals with low pre-operative MAp44 more frequently suffered from such post-operative complications as SIRS, MODS, LCOS or kidney failure. For MAp19, similar associations were found in children older than 1 year but not in infants. That suggests MAp44 (and MAp19 in older patients) acts to prevent injury from excessive complement activation and thus from systemic inflammation in response to major surgery. Those findings correspond to some extent with significant inverse correlations of MAp44 and MAp19 with such parameters of disease severity as VIS or BAS in older children (Table 2). Therefore, deficient individuals may be at a higher risk of development of afore-mentioned complications and non-enzymatic members of the MASP family might be considered as their potential biomarkers. Generally, results reported here confirmed our previous conclusion that LP activation contributes to development of post-operative SIRS5,6. As no association of MASP-2 concentration with postoperative complications or outcome was found, the key role of pattern-recognition molecules (collectins, ficolins) and/or regulatory factors (MAp44, MAp19, MASP-3) or its direct activator (MASP-1, see below) may be supposed. It should be stressed that MASP-2 levels are apparently less variable compared with other tested proteins (as well as MBL5,6) therefore even relatively low concentration may be sufficient for as active lectin pathway as allowed by the level of associated PRM and/or other MASP family members. That conclusion is additionally supported by previously published evidence that low activity of MBL-MASP-2 complexes (strongly correlating with MBL concentration and MBL-MASP-1 activity) offer protection against LCOS, SIRS, renal insufficiency and multi-organ failure5,6. Furthermore, pre-operative MASP-2 levels did not correlate significantly with MBL-MASP-2 activities (not shown).
According to the afore-mentioned report6, low pre-operative serum activity of MBL-MASP-1 complex protected patients from post-operative fever and SIRS but were associated with a higher risk of hospital infections. Our current evaluation of total serum MASP-1 concentration has not shown simply corresponding associations. However, children with the highest levels of MASP-1 (≥11.68 μg/ml, corresponding to the 90th percentile) had a poorer survival rate than those with lower MASP-1. It might be speculated that when a patient experiences severe complications (especially SIRS + MODS), high concentration of this protease (as in the case pattern-recognition molecule, ficolin-3) contributes to the amplification of adverse effects of activation of complement, coagulation and kinin systems. Therefore, high pre-operative levels of both factors involved in the initiation of the LP cascade might enhance the risk of life-threatening events. In parallel, relatively high MAp44 concentrations in some patients (due to significant correlation with MASP-1) seem not to be enough to be protective. In contrast, low MASP-3, another product of the MASP1/3 gene possibly involved in regulation of complement activation, was associated with high mortality. Previously, low MASP-3 on admission of pediatric patients to intensive care unit was associated with new hospital infections and prolonged stay at the ward36. We have not found such an influence of that enzyme in the case of patients suffering from CHD, although its concentration correlated reversely with VIS (Table 2).
Earlier, Frauenknecht et al.37 found plasma MASP-1 concentrations higher and MASP-2 lower in patients with myocardial infarction (MI) than in healthy controls. MASP-3 and MAp44 did not differ significantly37. Next, Holt et al.38 reported significantly higher plasma MAp44, MASP-1, and MASP-3 concentrations in MI, although no association with short-term outcome was observed. However, low MAp44 level predicted higher risk of death in renal transplant recipients while neither MASP-3 nor MAp19 concentrations were associated with patients’ survival39.
Ficolin-3-dependent lectin pathway activation during CPB was originally reported by Hein et al.40. Earlier, Xuan et al.41 reported lower ficolin-3 concentrations in newborns with tetralogy of Fallot (TOF) and ventricular septum defect (VSD) than in healthy controls. The lack of age-matched control group of children without CHD in our study makes similar comparison impossible. It has to be emphasized that aim of our study (which was investigation of associations of selected proteins with post-operative complications but not CHD itself) did not assume comparisons with healthy controls. On the other hand, we observed relatively higher ficolin-3 concentrations in TOF and VSD patients than in other types of CHD (not shown). Our most important findings concerning that protein are perhaps an association of its low pre-operative serum concentration with the development of SIRS and MODS and, secondly, its potential predictive value. It is not obvious why lower levels of a factor involved in complement activation contribute to excessive inflammatory response finally resulting in multiorgan failure. Although low ficolin-3 accompanied by high C3a level was associated with chronic heart failure42, that cannot be directly related to our results. It has been suggested that altered self-structures in the failing heart may bind ficolin-3, leading to its lowered plasma levels and induction of complement activation42. On the other hand, according to our data, in patients who developed SIRS followed by MODS, lower pre-operative serum ficolin-3 concentration seems to be beneficial. After further, possibly independent investigation, that protein might be considered as prognostic factor in the cases of severe complications after CPB. Our results (although from a relatively small number of pediatric patients) suggest that a suitable cut-off level would be 12.7 μg/ml. Previously, high ficolin-3 (as well as MASP-2) levels in plasma were suggested to predict a fatal outcome after severe traumatic brain injury43,44. Previously, ficolin-3 has been considered an anti-microbial agent45, however we did not observe a significant difference between its median concentrations in patients who developed post-operative infections and those who did not. That might support our earlier hypothesis that the crucial role of that factor may be in controlling normal (commensal) flora rather than protection from obligatory pathogens (including agents of hospital infections).
Although concentrations of ficolin-3 and MASP family proteins (with an exception for MASP-3) have been reported to differ between males and females28,46 no such differences were seen in our pediatric patients (not shown). It may be speculated that such differences become evident during adolescence.
To summarize, our data add considerably to the knowledge concerning involvement of complement activation via the lectin pathway in development of post-CPB complications. Possible interaction with other endogenous cascades, make the problem more complicated and data difficult to interpret, but create additional questions to be answered. Of immediate interest are our findings of (i) low preoperative MAp44 and various post-operative complications and (ii) high preoperative ficolin-3 and increased mortality. These promising prognostic associations warrant independent confirmation, perhaps by a large multi-centre study.
References
Yang, Q. et al. Racial differences in infant mortality attributable to birth defects in the United States, 1989–2002. Birth Defects Res A Clin Mol Teratol. 76, 706–713 (2006).
Hoffman, J. The global burden of congenital heart disease. Cardiovasc J Afr. 24, 141–145 (2013).
Greco, G. et al. Costs associated with health care-associated infections in cardiac surgery. J Am Coll Cardiol. 65, 15–23 (2015).
Stahl, G. L., Shernan, S. K., Smith, P. K. & Levy, J. H. Complement activation and cardiac surgery: a novel target for improving outcomes. Anesth Analg. 115, 759–771 (2012).
Pagowska-Klimek, I. et al. Activation of the lectin pathway of complement by cardiopulmonary bypass contributes to the development of systemic inflammatory response syndrome after pediatric cardiac surgery. Clin Exp Immunol. 184, 257–263 (2016).
Pagowska-Klimek, I. et al. Mannose-binding lectin (MBL) insufficiency protects against the development of systemic inflammatory response after pediatric cardiac surgery. Immunobiology. 221, 175–181 (2016).
Dahl, M. R. et al. MASP-3 and its association with distinct complexes of the mannan-binding lectin complement activation pathway. Immunity. 15, 127–135 (2001).
Stover, C. M. et al. Two constituents of the initiation complex of the mannan-binding lectin activation pathway of complement are encoded by a single structural gene. J Immunol. 162, 3481–3490 (1999).
Dobo, J. et al. Multiple roles of complement MASP-1 at the interface of innate immune response and coagulation. Mol Immunol. 61, 69–78 (2014).
Kjaer, T. R., Thiel, S. & Andersen, G. R. Toward a structure-based comprehension of the lectin pathway of complement. Mol Immunol. 56, 413–422 (2013).
Rossi, V. et al. Substrate specificities of recombinant mannan-binding lectin-associated serine proteases-1 and -2. J Biol Chem. 276, 40880–40887 (2001).
Dobo, J., Pal, G., Cervenak, L. & Gal, P. The emerging roles of mannose-binding lectin-associated serine proteases (MASPs) in the lectin pathway of complement and beyond. Immunol Rev. 274, 98–111 (2016).
Pihl, R. et al. Analysis of Factor D Isoforms in Malpuech-Michels-Mingarelli-Carnevale Patients Highlights the Role of MASP-3 as a Maturase in the Alternative Pathway of Complement. J Immunol (2017).
Skjoedt, M. O. et al. A novel mannose-binding lectin/ficolin-associated protein is highly expressed in heart and skeletal muscle tissues and inhibits complement activation. J Biol Chem. 285, 8234–8243 (2010).
Degn, S. E., Jensen, L., Olszowski, T., Jensenius, J. C. & Thiel, S. Co-complexes of MASP-1 and MASP-2 associated with the soluble pattern-recognition molecules drive lectin pathway activation in a manner inhibitable by MAp44. J Immunol. 191, 1334–1345 (2013).
Degn, S. E. et al. MAp19, the alternative splice product of the MASP2 gene. J Immunol Methods. 373, 89–101 (2011).
Hajela, K. et al. The biological functions of MBL-associated serine proteases (MASPs). Immunobiology. 205, 467–475 (2002).
Krarup, A., Wallis, R., Presanis, J. S., Gal, P. & Sim, R. B. Simultaneous activation of complement and coagulation by MBL-associated serine protease 2. PLoS One. 2, e623 (2007).
Hess, K. et al. Effects of MASP-1 of the complement system on activation of coagulation factors and plasma clot formation. PLoS One. 7, e35690 (2012).
Degn, S. E. et al. Biological variations of MASP-3 and MAp44, two splice products of the MASP1 gene involved in regulation of the complement system. J Immunol Methods. 361, 37–50 (2010).
Thiel, S. et al. Mannan-binding lectin (MBL)-associated serine protease-1 (MASP-1), a serine protease associated with humoral pattern-recognition molecules: normal and acute-phase levels in serum and stoichiometry of lectin pathway components. Clin Exp Immunol. 169, 38–48 (2012).
Szala, A. et al. Ficolin-2 and ficolin-3 in women with malignant and benign ovarian tumours. Cancer Immunol Immunother. 62, 1411–1419 (2013).
Larsen, J. B. et al. The lectin pathway and coagulation in lung cancer patients undergoing lobectomy - A randomised controlled trial. Thromb Res. 163, 92–99 (2018).
Novovic, S. et al. Mannan-binding lectin and mannan-binding lectin-associated serine protease 2 in acute pancreatitis. Pancreas. 40, 1097–1102 (2011).
Lacour-Gayet, F. et al. The Aristotle score for congenital heart surgery. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 7, 185–191 (2004).
Gaies, M. G. et al. Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med. 11, 234–238 (2010).
Goldstein, B., Giroir, B. & Randolph, A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 6, 2–8 (2005).
Troldborg, A. et al. Lectin complement pathway proteins in healthy individuals. Clin Exp Immunol. 188, 138–147 (2017).
Świerzko, A. S. et al. Components of the lectin pathway of complement activation in paediatric patients of intensive care units. Immunobiology. 221, 657–669 (2016).
Michalski, M. et al. H-ficolin (ficolin-3) concentrations and FCN3 gene polymorphism in neonates. Immunobiology. 217, 730–737 (2012).
Soares, L. C., Ribas, D., Spring, R., Silva, J. M. & Miyague, N. I. Clinical profile of systemic inflammatory response after pediatric cardiac surgery with cardiopulmonary bypass. Arq Bras Cardiol. 94, 127–133 (2010).
Guvener, M., Korun, O. & Demirturk, O. S. Risk factors for systemic inflammatory response after congenital cardiac surgery. J Card Surg. 30, 92–96 (2015).
Eppa, L. et al. Deposition of mannose-binding lectin and ficolins and activation of the lectin pathway of complement on the surface of polyurethane tubing used for cardiopulmonary bypass. J Biomed Mater Res B Appl Biomater. 106, 1202–1208 (2018).
Degn, S. E. et al. MAp44, a human protein associated with pattern recognition molecules of the complement system and regulating the lectin pathway of complement activation. J Immunol. 183, 7371–7378 (2009).
Mortensen, S. A. et al. Endogenous Natural Complement Inhibitor Regulates Cardiac Development. J Immunol. 198, 3118–3126 (2017).
Ingels, C. et al. Lectin pathway of complement activation and relation with clinical complications in critically ill children. Pediatr Res. 75, 99–108 (2014).
Frauenknecht, V. et al. Plasma levels of mannan-binding lectin (MBL)-associated serine proteases (MASPs) and MBL-associated protein in cardio- and cerebrovascular diseases. Clin Exp Immunol. 173, 112–120 (2013).
Holt, C. B. et al. Association between endogenous complement inhibitor and myocardial salvage in patients with myocardial infarction. Eur Heart J Acute Cardiovasc Care. 3, 3–9 (2014).
Smedbraten, J. et al. Low level of MAp44, an inhibitor of the lectin complement pathway, and long-term graft and patient survival; a cohort study of 382 kidney recipients. BMC Nephrol. 17, 148 (2016).
Hein, E. et al. Heparin-coated cardiopulmonary bypass circuits selectively deplete the pattern recognition molecule ficolin-2 of the lectin complement pathway in vivo. Clin Exp Immunol. 179, 294–299 (2015).
Xuan, C. et al. Proteomic study reveals plasma protein changes in congenital heart diseases. Ann Thorac Surg. 97, 1414–1419 (2014).
Prohaszka, Z. et al. Association of ficolin-3 with severity and outcome of chronic heart failure. PLoS One. 8, e60976 (2013).
Pan, J. W. et al. Low serum ficolin-3 levels are associated with severity and poor outcome in traumatic brain injury. J Neuroinflammation. 12, 226 (2015).
Osthoff, M., Walder, B., Delhumeau, C., Trendelenburg, M. & Turck, N. Association of Lectin Pathway Protein Levels and Genetic Variants Early after Injury with Outcomes after Severe Traumatic Brain Injury: A Prospective Cohort Study. J Neurotrauma. 34, 2560–2566 (2017).
Michalski, M. et al. Ficolin-3 activity towards the opportunistic pathogen, Hafnia alvei. Immunobiology. 220, 117–123 (2015).
Gaya da Costa M. et al. Age and sex-associated changes of complement activity and complement levels in a healthy Caucasian population. Front Immunol. 9, 2664, https://doi.org/10.3389/fimmu.2018.02664.
Acknowledgements
MM was the recipient of fellowship for PhD students from the National Science Centre (Poland), 2015/16/T/NZ6/00412, https://www.ncn.gov.pl/?language = en. This study was partially supported by the National Science Centre, grant no. UMO2011/03/B/NZ6/00052. We acknowledge the Danish Council for Independent Research, Medical Sciences and the Lundbeck Foundation for financial support. The authors thank Prof. Jolanta Łukasiewicz (Ludwik Hirszfeld Institute of Immunology and Experimental Therapy, Polish Academy of Sciences, Wrocław, Poland) for providing coating antigen for ficolin-3 ELISA and Dr David C. Kilpatrick for critical reading of the manuscript and helpful discussion.
Author information
Authors and Affiliations
Contributions
M.M., A.S.Ś. and M.C. designed the study and performed majority of experimental work; M.M. wrote the draft manuscript; I.P.K. was responsible for patient’s qualification; S.T., A.G.H. and J.C.J. contributed to study design, data interpretation, manuscript preparation and co-edited it to prepare its final version. All authors read and approved manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Michalski, M., Pągowska-Klimek, I., Thiel, S. et al. Factors involved in initiation and regulation of complement lectin pathway influence postoperative outcome after pediatric cardiac surgery involving cardiopulmonary bypass. Sci Rep 9, 2930 (2019). https://doi.org/10.1038/s41598-019-39742-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39742-w
This article is cited by
-
Associations of ficolins and mannose-binding lectin with acute myeloid leukaemia in adults
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.



