Abstract
Highly active antiretroviral therapy (HAART) causes a rapid increase of CD4 + T cells counts during the first 3–6 months of treatment and may enhance the development of opportunistic infections (OIs). However, the short- and long-term effects of HAART exposure on the development of incident OIs has not been extensively studied. This nationwide longitudinal study followed up a total of 26,258 people living with HIV/AIDS (PLWHA) to ascertain the short- and long-term effects of HAART on incident OIs. During 150,196 person-years of follow-up, 6,413 (24.4%) PLWHA had new onset of OIs. After adjusting for demographics, comorbidities, and AIDS status, PLWHA who received HAART were more likely to develop OIs than those who did not receive HAART. Considering the short- and long-term effects of HAART on the development of OIs, HAART was found to be a risk factor for developing OIs during the first 90 days of treatment, but a protective factor against OIs after 180 days of HAART use. The risk for the development of active OIs significantly decreased as the duration of HAART increased (P < 0.001). Our study suggests that HAART is a risk factor for developing OIs in the short term, but is a protective factor in the long term.
Similar content being viewed by others
Introduction
Acquired immunodeficiency syndrome (AIDS) is a deadly infectious disease caused by the human immunodeficiency virus (HIV). By December 2016, 36.7 million people in the world were living with HIV/AIDS, and more than 35 million having died of the disease1.
HIV infection causes the depletion of CD4+ T cells and may increase the risk for opportunistic infections (OIs). OIs have been reported as the major driver of HIV-associated morbidity and mortality, even in the era of highly active antiretroviral therapy (HAART)2,3. Since early diagnosis and treatment of OIs could significantly reduce the associated mortality4, it is imperative to identify populations at high risk for OIs among PLWHA.
HAART significantly improves survival in PLWHA. Antiretroviral drugs cause a swift increase of CD4+ T lymphocytes during the early phase of treatment. Since immunopathologic host responses to microorganism are central to the clinical presentation of infectious disease, several observational studies found that OIs in PLWHA could develop shortly after HAART initiation5,6. However, few longitudinal studies investigated the short- and long-term effects of HAART on incident OIs, and their results were inconsistent. Two studies found that HAART could significantly increase the risk for incident candidiasis or Mycobacterium avium complex infection during the first 60 and 90 days of HAART use, respectively5,7; however, a US-based study showed that HAART was not significantly associated with a risk for incident tuberculosis (TB) during the first 180 days of HAART8. Furthermore, two previous studies revealed that PLWHA who received HAART for more than 90 or 180 days were at lower risk for TB7,8, Mycobacterium avium complex infection7, cryptococcosis7, candidiasis7, or cytomegalovirus (CMV) infection7. However, another study identified no protective effect against candidiasis development in PLWHA after 60 days of HAART5.
Identification of risk factors for the development of OIs in PLWHA may help in their prevention and management. We therefore conducted a nationwide longitudinal study to evaluate the short- and long-term effects of HAART on incident OIs among PLWHA in Taiwan.
Methods
Data source
In this retrospective longitudinal study, the Taiwan Centers for Disease Control (CDC) HIV Surveillance Database was accessed to identify all reported cases of HIV infection from 2000 to 2014. These reported HIV cases had either a positive HIV-1 polymerase chain reaction or Western blot. In Taiwan, it is mandatory to report all new HIV-infected cases to the Taiwan CDC within 24 hours of diagnosis, and since 1997, free-of-charge HAART has been offered to all HIV-infected individuals9. The Taiwan CDC HIV Surveillance Database can only be accessed at the Collaboration Center of Health Information Application, Department of Health, Taiwan, after obtaining approval from the National Health Research Institutes (KMUHIRB-20140073). Patient identification codes in the Taiwan CDC HIV Surveillance Database are scrambled and de-identified before being accessed by the researchers. This study was approved by the institutional review board of Kaohsiung Medical University. The informed consents for study participants were waived in this report. All methods in this study were performed in accordance with relevant guidelines and regulations.
Study subjects
HIV-infected individuals (age ≥ 15 years) were identified from Taiwan CDC HIV Surveillance Database from 2000 to 201410. These individuals were followed up until a diagnosis of OI was made, December 31, 2014, or death. Death cases were confirmed by the Taiwan death certificate database.
Outcome variable
The National Health Insurance Research Database in Taiwan was linked to the Taiwan CDC HIV database. Newly diagnosed OIs included disseminated Mycobacterium avium complex infection (International Classification of Diseases, Ninth Revision [ICD-9] code 0312), CMV infection (ICD-9-CM code 078.5), Pneumocystis jirovecii pneumonia (ICD-9-CM code 1363), cryptococcal meningitis (ICD-9-CM code 3210), candidiasis (ICD-9-CM code 112), Penicillium marneffei infection (ICD-9-CM code 1179), and toxoplasma encephalitis (ICD-9-CM code 130). A person was considered to have a new onset of OIs only if the condition occurred in an inpatient setting or if it was recorded in three or more outpatient visits11. New onset of tuberculosis was identified by using the Taiwan CDC tuberculosis surveillance database, as medical professionals need to report new cases of turberculosis to Taiwan CDC within 7 days of diagnosis by law.
Main explanatory variable
HAART was the the main explanatory variable. PLWHA who received HAART were defined as those receiving anti-retroviral drugs before the onset of new OIs. Because of rapid increase of CD4 + T lymphocytes during the first 3–6 months of HAART initiation12, the short-term effects of HAART on the development of OIs was defined as the risk of OIs within 90 and between 90 and 180 days of treatment8. The long-term effect of HAART was defined as the risk after 180 days of HAART use8.
Other explanatory variables
Sociodemographic variables analyzed included urbanization (urban or rural) and income level. The average monthly income of the insured individual was categorized as: low (≤19 200 New Taiwan Dollars [NTD]), intermediate (19 201 NTD to <40 000 NTD), or high (≥40 000 NTD). The comorbidities investigated included chronic kidney disease (ICD-9 code 580–587), diabetes (ICD-9 code 250), hypertension (ICD-9 code 401–405), congestive heart failure (ICD-9 code 428.0), cerebral vascular disease (ICD-9 code 430–437), cancer (ICD-9 code 140–208), and chronic obstructive pulmonary disease (ICD-9 codes 491, 492, and 496).
AIDS status was defined as the presence of any of the AIDS-defining conditions or a CD4+ lymphocyte count <200 cells/mm3 13.
Statistical analysis
The incidence density (ID) for each OI was calculated in this cohort of PLWHA. To calculate the ID for each OI, PLWHA were excluded if they had received a diagnostic code for the OI before the study period. Moreover, this study evaluated the ID in PLWHA not receiving HAART, those receiving HAART within 90 days, between 90 and 180 days, and after 180 days of treatment. The follow-up years in different phases of treatment were calculated independently in each OI. The ID of each OI was calculated by dividing the number of observed cases by the total person-years at risk for that OI.
Time-dependent Cox proportional hazards models were used to determine the association between HAART and each OI. In these models, death was considered as a competing risk event14, and HAART and AIDS status were regarded as time-dependent variables15. The short- and long-term effects of HAART on the development of incident OIs were evaluated. Adjusted HRs (AHRs) with 95% CIs were calculated to indicate the direction and strength of associations.
The robustness of the association between HAART and incident OIs was determined by sensitivity analysis, including only subjects with recorded CD4+ count or viral load at the time of HIV diagnosis. Statistical analysis was performed with SAS 9.4 (SAS Institute, Cary, NC).
Results
Participant selection
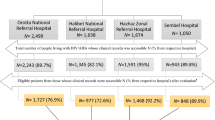
During the period from January 1, 2000 through December 31, 2014, 26 838 HIV-infected individuals were reported to Taiwan CDC. After excluding those younger than 15 years (n = 72) and those with incomplete data (n = 508), the remaining 26 258 PLWHA were included in the analysis (Fig. S1). The overall mean (SD) age was 32.3 (10.2) years; 93.9% of the subjects were male; and 73.4% of the subjects received HAART (Table 1). Compared with PLWHA who did not receive HAART, PLWHA who received HAART had a significantly higher proportion of AIDS status, diabetes, CKD, HTN, COPD, and cancer.
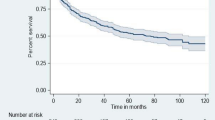
Incidence of OIs in PLWHA
During the study follow-up period, 6413 (24.4%) PLWHA developed OIs. Of these OIs, Pneumocystis jirovecii pneumonia had the highest ID (n = 2978; ID = 21.63/1000 person-years), followed by candidiasis (n = 2658; ID = 19.80/1000 person-years) and CMV infection (n = 893; ID = 6.09/1000 person-years; Table 2).
Association between HAART and incident OIs
After adjusting for demographics, comorbidities, and AIDS status, the time-dependent Cox proportional hazards model showed that PLWHA who received HAART were more likely to develop OIs than those who did not receive HAART, such as tuberculosis (AHR 1.88; 95% CI 1.44–2.44), disseminated Mycobacterium avium complex infection (AHR 11.7; 95% CI 5.39–25.5), CMV infection (AHR 7.42; 95% CI 5.65–9.74), Pneumocystis jirovecii pneumonia (AHR 3.41; 95% CI 2.94–3.94), cryptococcal meningitis (AHR 5.13; 95% CI 3.26–8.09), candidiasis (AHR 2.14; 95% CI 1.86–2.46), penicillium marneffei infection (AHR 2.97; 95% CI 1.79–4.93), and toxoplasma encephalitis (AHR 2.84; 95% CI 1.31–6.13; Table 3).
Short- and long-term effects of HAART on incident OIs
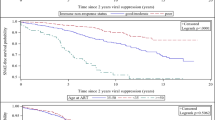
The time-dependent Cox proportional hazards model found that PLWHA who received HAART within the first 90 days of treatment were at higher risk of OIs, including TB (AHR 6.92; 95% CI 5.28–9.08), disseminated Mycobacterium avium complex infection (AHR 29.4; 95% CI 14.5–59.7), CMV infection (AHR 13.30; 95% CI 10.30–17.1), Pneumocystis jirovecii pneumonia (AHR 7.78; 95% CI 6.88–8.79), cryptococcal meningitis (AHR 8.67; 95% CI 5.64–13.30), candidiasis (AHR 5.59; 95% CI 4.91–6.37), Penicillium marneffei infection (AHR 6.86; 95% CI 4.14–11.4), and toxoplasma encephalitis (AHR 6.63; 95% CI 2.81–15.6) (Table 4). Moreover, PLWHA who received HAART between 90 and 180 days of treatment had higher risk of incident disseminated Mycobacterium avium complex infection (AHR 10.40; 95% CI 4.58–23.7) and CMV infection (AHR 3.54; 95% CI 2.42–5.18). However, when PLWHA received HAART for more than 180 days, they were at lower risk for OIs, including TB (AHR 0.49; 95% CI 0.37–0.64), disseminated Mycobacterium avium complex infection (AHR 2.17; 95% CI 1.03–4.58), CMV infection (AHR 0.69; 95% CI 0.51–0.93), Pneumocystis jirovecii pneumonia (AHR 0.26; 95% CI 0.23–0.31), cryptococcal meningitis (AHR 0.52; 95% CI 0.31–0.87), and candidiasis (AHR 0.32; 95% CI 0.28–0.37). The risk for the development of active OIs decreased as the duration of HAART increased (P < 0.001).
Sensitivity analysis for the association between HAART and incident OIs
A total of 6413 PLWHA with CD4+ counts or viral load data at the time of HIV diagnosis were included in the sensitivity analysis. After adjusting for demographics, comorbidities, AIDS status, CD4+ count, and viral load, HAART was found to be significantly associated with a higher risk of incident OIs, except toxoplasma encephalitis (Supplementary Table 1). Considering the short- and long-term effects of HAART on the development of OIs, PLWHA who received HAART within the first 90 days of treatment were at higher risk of OIs, including tuberculosis, disseminated Mycobacterium avium complex infection, CMV infection, Pneumocystis jirovecii pneumonia, cryptococcal meningitis, candidiasis, and Penicillium marneffei infection (Supplementary Table 2). Moreover, PLWHA who received HAART between 90 and 180 days of treatment had higher risks of incident tuberculosis, disseminated Mycobacterium avium complex infection, and CMV infection. However, when PLWHA received HAART for more than 180 days, they were at a lower risk of Pneumocystis jirovecii pneumonia and candidiasis. As the duration of HAART increased, the risk of developing active OIs decreased (P < 0.001).
Discussion
This longitudinal study showed that PLWHA who received HAART were more likely to develop OIs than those who did not. Considering the short- and long-term effects of HAART on the development of OIs, HAART was found to be a risk factor for the development of OIs during the first 90 days of HAART, but a protective factor after 180 days of HAART. The risk of incident OIs significantly decreased with increasing duration of HAART.
Previous studies reported that PLWHA could develop OIs soon after starting HAART5,6. However, only a few studies investigated the short- and long-term effects of HAART on the development of OIs and reported inconsistent results. A US-based study showed that HAART was not significantly associated with the development of tuberculosis within the first 180 days of treatment (AHR 0.65; 95% CI 0.28–1.51), but was significantly associated with a lower risk of the development of tuberculosis after 180 days of HAART use (AHR 0.29; 95% CI 0.16–0.53)8. A French hospital-based study followed up 1647 HIV-infected patients and found that HAART significantly increased the risk for incident candidiasis within the first 2 months of treatment (AHR 2.6; 95% CI 1.2–5.5) but was not significantly associated with the development of candidiasis after 2 months of HAART use (AHR 0.8; 95% CI 0.3–2.4)5. Another HIV-CAUSAL Collaboration cohort study found that HAART was a risk factor for Mycobacterium avium complex infection during the first 90 days of treatment, but was a protective factor against tuberculosis, Mycobacterium avium complex infection, cryptococcosis, candidiasis, and CMV infection after 90 days of HAART use7. The present study showed that PLWHA receiving HAART were more likely to develop OIs than those not receiving HAART. While considering the short term and long term effects of HAART on OIs, HAART was found to be a risk factor for the development of OIs during the first 90 days of treatment, but a protective factor after 180 days of treatment. Since the mortality rate was high in PLWHA with OIs16, HIV-infected individuals who receive HAART should be followed up carefully for the development of OIs, particularly during the early phase of HAART use.
Biphasic recovery of CD4+ T lymphocyte counts may explain the short-term risk but long-term protection effects of HAART on the development of OIs. When HIV-infected individuals received HAART, the combination antiretroviral drugs cause two stages of CD4+ T lymphocyte recovery, including the rapid increase in CD4+ T cells (CD4 + 5RO+) during the first 3–6 months of HAART treatment and a slow increase in CD4+ T cells (CD4 + 5RA+, CD62L+) after 6 months of HAART use12,17. A prior in vitro study demonstrated that the CD4+ T lymphocyte count increased 3.5-fold after 3–6 months of HAART and then slowly increased to 4-fold after 2 years of HAART use12. The fast increase in CD4+ T lymphocytes following HAART treatment could result in rapid immune restoration. Because OIs often present with an insidious onset in immunodeficient PLWHA17, this fast increase in the number of CD4+ T lymphocytes could speed up the development of active OIs by enhancing the immune response to subclinical OIs5,18. The slow increase in CD4+ T cells in PLWHA receiving HAART for more than 6 months could lead to a long-term protection against OIs. Since CD4+ T-cell-mediated immunity plays an essential role in protecting against OIs19, and the stabilized T cell immunity could provide long-term protection against OIs development in PLWHA receiving HAART for more than 6 months.
This cohort study has several strengths. First, this nationwide study included all HIV-infected subjects with an HIV diagnosis based on a positive HIV-1 polymerase chain reaction or Western blot, which supported the validity of these findings. Second, because all medical costs of PLWHA are covered under the National Health Insurance Program in Taiwan, this cohort study could trace all HIV-infected individuals with referral bias being minimized. Third, unlike previous studies that did not account for changes in HAART exposure during the study period8, in this study, HAART was considered a time-dependent variable in order to determine the exact effect of HAART exposure on the development of active OIs20. Finally, because the rate of the competing risk of death was high among HIV-infected individuals in this study (12.4%), this report used competing risk analysis to determine the precise association of HAART with incident OIs21.
This study also has some limitations. First, because it is not mandatory to report CD4+ counts and viral loads to the Taiwan CDC when reporting new HIV cases, only 6413 (24.4%) cases had these data at the time of HIV diagnosis. The sensitivity analysis showed that PLWHA who received HAART for <90 days were more likely to develop OIs, but were less likely to develop OIs after 180 days of HAART use, after adjusting for comorbidities, CD4+ counts, and viral loads. As the duration of HAART increased, the risk for the development of active OIs significantly decreased. Second, the diagnosis of OIs in this study may be less accurate than diagnoses made in a prospective clinical setting because it was based on administrative claims data recorded by hospitals or physicians Nonetheless, there is no reason to suspect that the validity of claims data would differ on the basis of the patients’ HIV status. This non-differential misclassification of outcome would cause a bias toward a null association. Finally, the generalizability of our findings to other non-Asian ethnic groups needs further verification because most of our subjects were Taiwanese. Nevertheless, our findings may have important clinical implications for improving medical care in PLWHA.
In summary, this nationwide population-based cohort study showed that PLWHA receiving HAART were more likely to develop OIs than those not receiving HAART. HAART was found to be a risk factor for the development of OIs in the short term (during the first 90 days of treatment), but a protective factor in the long run (after 180 days of treatment). Since OIs remain the major driver of HIV-associated morbidity and mortality, our study suggests that PLWHA who received HAART should be monitored carefully for the development of OIs, particularly during the early phase of HAART.
References
World Health Organization Report on the global HIV/AIDS Epidemic. http://www.who.int/hiv/en/ accessed 10 December 2017 (2016).
Manosuthi, W. et al. Incidence and risk factors of major opportunistic infections after initiation of antiretroviral therapy among advanced HIV-infected patients in a resource-limited setting. J Infect 55, 464–469 (2007).
Ghate, M. et al. Incidence of common opportunistic infections in HIV-infected individuals in Pune, India: analysis by stages of immunosuppression represented by CD4 counts. Int J Infect Dis 13, e1–8 (2009).
Zanoni, B. C. & Gandhi, R. T. Update on opportunistic infections in the era of effective antiretroviral therapy. Infect Dis Clin North Am 28, 501–518 (2014).
Nacher, M. et al. Increased incidence of mucosal candidiasis after HAART initiation: a benign form of immune reconstitution disease? AIDS 21, 2534–2536 (2007).
Girardi, E. et al. Incidence of Tuberculosis among HIV-infected patients receiving highly active antiretroviral therapy in Europe and North America. Clin Infect Dis 41, 1772–1782 (2005).
Opportunistic infections and AIDS malignancies early after initiating combination antiretroviral therapy in high-income countries. AIDS 28, 2461–2473 (2014).
Pettit, A. C. et al. Timing of Antiretroviral Treatment, Immunovirologic Status, and TB Risk: Implications for Testing and Treatment. J Acquir Immune Defic Syndr 72, 572–578 (2016).
Chen, Y. M. & Kuo, S. H. HIV-1 in Taiwan. Lancet 369, 623–625 (2007).
Frisch, M., Biggar, R. J., Engels, E. A. & Goedert, J. J. Association of cancer with AIDS-related immunosuppression in adults. Jama 285, 1736–1745 (2001).
Yen, Y. F. et al. Association of pulmonary tuberculosis and ethambutol with incident depressive disorder: a nationwide, population-based cohort study. J Clin Psychiatry 76, e505–511 (2015).
Notermans, D. W. et al. Immune reconstitution after 2 years of successful potent antiretroviral therapy in previously untreated human immunodeficiency virus type 1-infected adults. J Infect Dis 180, 1050–1056 (1999).
Schneider, E. et al. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years–United States, 2008. MMWR Recomm Rep 57, 1–12 (2008).
Jason, P. F. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 94, 496–509 (1999).
Anderson, A. M., Fountain, J. A., Green, S. B., Bloom, S. A. & Palmore, M. P. Human immunodeficiency virus-associated cytomegalovirus infection with multiple small vessel cerebral infarcts in the setting of early immune reconstitution. J Neurovirol 16, 179–184 (2010).
Djawe, K. et al. Mortality Risk After AIDS-Defining Opportunistic Illness Among HIV-Infected Persons–San Francisco, 1981-2012. J Infect Dis 212, 1366–1375 (2015).
Mtei, L. et al. High rates of clinical and subclinical tuberculosis among HIV-infected ambulatory subjects in Tanzania. Clin Infect Dis 40, 1500–1507 (2005).
Breen, R. A., Smith, C. J., Cropley, I., Johnson, M. A. & Lipman, M. C. Does immune reconstitution syndrome promote active tuberculosis in patients receiving highly active antiretroviral therapy? AIDS 19, 1201–1206 (2005).
Okoye, A. A. & Picker, L. J. CD4(+) T-cell depletion in HIV infection: mechanisms of immunological failure. Immunol Rev 254, 54–64 (2013).
Collett D. Modelling survival data in medical research, 2nd ed., Chapman & Hall (2003).
Southern, D. A. et al. Kaplan-Meier methods yielded misleading results in competing risk scenarios. J Clin Epidemiol 59, 1110–1114 (2006).
Acknowledgements
This study was supported by a grant from Kaohsiung Medical University Research Foundation (105KMUOR05). The authors thank Yun Lee, Peng-Chien Kuo, and Yu-An Lin for their help in analyzing the data.
Author information
Authors and Affiliations
Contributions
Y.F.Y. substantially contributed to the conception and design of the study, data interpretation and the drafting of the manuscript. P.H.C. and M.C. contributed to the conception and design of the study. I.A.J. participated in developing the idea into a concept. C.Y.L. and S.I.L. participated in collecting data. Y.M.C. applied for and received the project grants. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41598_2019_39665_MOESM1_ESM.docx
Figure S1. Process of enrollment and follow-up among patients with HIV, 2000-2014. PLWHA = people living with HIV/AIDS; HIV = human immunodeficiency virus; OIs = opportunistic infections.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yen, YF., Chen, M., Jen, IA. et al. Short- and Long-term Risks of Highly Active Antiretroviral Treatment with Incident Opportunistic Infections among People Living with HIV/AIDS. Sci Rep 9, 3476 (2019). https://doi.org/10.1038/s41598-019-39665-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39665-6
This article is cited by
-
The association between fear of progression and medical coping strategies among people living with HIV: a cross-sectional study
BMC Public Health (2024)
-
Spectrum and mortality of opportunistic infections among HIV/AIDS patients in southwestern China
European Journal of Clinical Microbiology & Infectious Diseases (2023)
-
Identifying subtypes of HIV/AIDS-related symptoms in China using latent profile analysis and symptom networks
Scientific Reports (2022)
-
Different Trends of Distinct Time Points of AIDS Events Following HIV Diagnosis in Various At-risk Populations: A Retrospective Nationwide Cohort Study in Taiwan
Infectious Diseases and Therapy (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.