Abstract
Comprehensive genomic sequencing (CGS) enables us to detect numerous genetic alterations in a single assay. We aimed to identify molecular markers for predicting prognosis and conversion surgery in Stage IV colorectal cancer (CRC) using CGS. One-hundred eleven patients with Stage IV CRC who underwent primary tumor resection were analyzed. We retrospectively investigated genetic alterations using CGS of a 415-gene panel. Clinicopathological variables and genetic alterations were analyzed to identify independent prognostic factors of overall survival (OS). Forty-five of 111 patients had R0 resection; of these, 11 patients underwent conversion surgery. Univariate and multivariate analyses identified histopathological grade 3, R0 resection, BRAF V600E mutation, and SRC mutation as independent prognostic factors for OS (P = 0.041, P = 0.013, P = 0.005, and P = 0.023, respectively). BRAF V600E and SRC mutations were mutually exclusive, and SRC mutation was significantly associated with left-sided tumor and liver metastasis compared to BRAF V600E mutation (P = 0.016 and P = 0.025, respectively). Eleven of the 74 initially unresectable patients underwent conversion surgery for R0 resection, yet none harbored BRAF V600E or SRC mutations. BRAF V600E and SRC mutations are important molecular markers which can predict prognosis and conversion surgery in Stage IV CRC.
Similar content being viewed by others
Introduction
Worldwide, colorectal cancer (CRC) was responsible for an estimated 1.4 million new cases and 694,000 deaths in 2012, and ranks as third most frequent cancer in men (after lung and prostate), and second in women (after breast)1. Despite widespread early detection screening for CRC, approximately 25% of patients with CRC are found to have distant metastases at time of diagnosis2,3. The American Joint Committee on Cancer (AJCC) defines Stage IV CRC as any tumor with an M stage of M1a, M1b, or M1c, which describes a tumor that has spread to distant organs, nodes or the peritoneum2. Stage IV CRC however, is a highly diverse disease, and as such, a more precise stratification of patients is required. Incorporation of non-anatomic factors beyond TNM would provide a more accurate and probabilistic individualized outcome prediction for precision medicine4,5.
In the past few years, there has been an explosion in the understanding of molecular markers. KRAS, NRAS, and BRAF are important components of the MEK/ERK pathway, which controls cell proliferation and survival in CRC. Activating somatic mutations at KRAS, NRAS, and BRAF, which predict poor response to anti-EGFR therapy6,7, are detected in up to 40%, 7%, and 10% patients with CRC, respectively2,3,8. Among them, BRAF V600E mutations are associated with a worse prognosis9, and are recognized as a non-anatomic poor prognostic factor in CRC2. The AJCC 8th edition states that these non-anatomic factors are important to consider when making treatment decisions2.
R0 resection, a microscopically margin-negative resection where no gross or microscopic tumor remains, has been the most effective surgical treatment strategy in stage IV CRC3,10. For patients with oligometastatic disease contained to a single or a few organs, long-term survival or even cure can be attained in 20–50% patients following R0 resection of both primary and metastatic lesions10. Furthermore, there is the benefit of conversion surgery, where systemic therapy in patients with initially unresectable distant metastasis provides the prospect of R0 resection3,11,12. However, to date, predictive molecular markers for conversion surgery is not known.
SRC is a member of a superfamily of membrane-associated non-receptor protein tyrosine kinases13. These proteins are activated by a number of receptors, such as platelet-derived growth factors, epidermal growth factor, and fibroblast growth factor; and regulate a cascade of downstream targets to affect proliferation, adhesion, differentiation, and migration14. In CRC, a few reports have demonstrated that overexpression of SRC is associated with distant metastasis14,15,16 and drug resistance17,18; however, to date, the clinicopathological characteristics and clinical significance has not been fully elucidated.
Comprehensive genomic sequencing (CGS) is an emerging technology that can detect numerous genetic mutations and copy number alterations in a single assay. By utilizing CGS technology, projects such as The Cancer Genome Atlas (TCGA) have profiled genomic changes in many cancers including CRC8. Similarly, we have previously generated a genomic overview of Japanese CRC patients using a 415-gene CGS panel19,20,21, and speculated that CGS can detect clinically important genetic alterations of Stage IV CRC. We aimed to identify molecular markers for predicting prognosis and conversion surgery in Stage IV CRC using CGS.
Materials and Methods
Patients
This retrospective analysis was performed in accordance with the Helsinki Declaration, and the Ethics Committee of the School of Medicine, Niigata University, approved the study protocol. All methods were performed in accordance with the relevant guidelines and regulations, and written informed consent was obtained from all patients. A total of 111 patients diagnosed with stage IV CRC (AJCC, 7th edition)22 who underwent a primary tumor resection between 2009 and 2015 at the Niigata University Medical and Dental Hospital or Niigata Cancer Center Hospital were randomly selected, and enrolled. Patients with familial adenomatous polyposis or inflammatory bowel disease were excluded. Of the 111 patients, metastasis to the liver, lung, peritoneum, and other sites at initial assessment were identified in 88, 34, 22, and 23 patients, respectively. Thirty-seven and 74 patients were diagnosed with resectable and unresectable metastatic disease, respectively, at initial assessment (Fig. 1A). Resectability of metastatic disease was determined by colorectal and hepatobiliary surgeons of each of the two hospitals using computed tomography and/or magnetic resonance imaging.
Residual tumor status and conversion surgery
Patients were classified according to residual tumor status. Patients who achieved R0 resection of both the primary lesion and distant metastasis were classified as “R0”, while patients for whom R0 resection could not be achieved were classified as “R2”. Conversion surgery was defined as R0 resection after systemic therapy for initially unresectable distant metastasis3,11,12.
CGS analysis of primary tumors
As we previously reported, CGS of primary tumor was performed as follows19,20,21. Tumor content was evaluated by an independent pathologist for each sample using hematoxylin and eosin-stained slides to ensure >50% tumor content. Where applicable, unstained slides were macro-dissected to enrich for tumor content, and DNA was extracted using a BioStic FFPE Tissue DNA Isolation Kit (Mo Bio Laboratories, Inc., Carlsbad, CA). All sample preparations, CGS, and analytics were performed in a CLIA/CAP-accredited laboratory (KEW Inc., Cambridge, MA). DNA fragment (50–150 ng) libraries were prepared and enriched for the CancerPlex 415-gene panel (KEW Inc.)19,20,21. Sequencing was performed on Illumina MiSeq and NextSeq platforms with an average 500X sequencing depth. Genomic data were then processed through a proprietary bioinformatics platform and knowledgebase to identify multiple classes of genomic abnormalities, including single nucleotide substitutions, small insertions/deletions, copy number variations, and translocations. Single nucleotide variant (SNV) and insertion or deletion (indel) calling were only performed in genomic regions intended to be captured by the assay (region of interest). We set a standard threshold of 10% allelic fraction for calling SNVs and indels to focus on primary truncal driver mutations and avoid subclonal events. Copy number variants were called for exons as well as globally. We segmented regions using a Fused-Lasso method and exported results to a VCF file. The threshold for gain was >2.5 fold, and for loss was <0.5 fold. Variants were filtered or flagged according to technical quality (e.g. coverage, allelic fraction, number of supporting reads), presence in previously characterized normal samples, or presence/absence in the following databases: dbSNP, ExAC, COSMIC, ClinVar, and KEW. SNVs and indels in VCF format were annotated using SnpEff and the output was adapted according to HGVS recommendations. Tumors were tested for the presence of microsatellite instability (MSI) based on an extended loci panel. In addition to the Bethesda panel, a collection of 950 regions consisting of tandem repeats of one, two, or three nucleotides of minimum length of 10 bases were examined. The number of indels within the regions of interest was calculated, and tumors were classified as MSI-high (MSI-H) or microsatellite stable (MSS).
Prognostic factors
To identify factors influencing overall survival (OS) after surgery, genetic alterations (identified using the 415 gene panel) and 15 clinicopathological variables (Table 1) were tested in all 111 patients. In this study, genetic alterations that occurred at a frequency of more than 5% were evaluated for their prognostic impact in univariate and multivariate analyses of 5-year OS. Regarding BRAF mutation, we separately evaluated BRAF V600E and non-V600E.
Genetic alterations in EGFR pathway
To investigate the association between efficacy of anti-EGFR therapy and genetic alterations in EGFR pathway, genetic alterations of TK receptors (ERBB2, MET, EGFR, FGFR1, and PDGFRA), MEK/ERK pathway (KRAS, NRAS, HRAS, BRAF, and MAPK2K1), and PI3K pathway (PTEN and PIK3CA) were analyzed using CGS of the 415-gene panel. We defined patients who had no alterations in any of the 12 genes as “all wild-type”; theoretically, these patients should respond to anti-EGFR therapy23,24.
Statistical analysis
Statistical analyses were performed with IBM SPSS Statistics 22 (IBM Japan, Inc., Tokyo, Japan). Five-year OS rates were estimated using the Kaplan-Meier method. The log-rank test was used to assess for significant differences between subgroups by univariate analysis. To investigate independent prognostic factors for OS, factors with a P-value of less than 0.05 in univariate analyses were entered into a multivariate analysis. The Cox proportional hazards regression model was used to identify factors that were independently associated with OS after surgery. Pearson’s chi-squared test or Fisher’s exact test was used to evaluate the associations between clinicopathological characteristics and genetic alterations evaluated using CGS. P-values less than 0.05 were considered statistically significant.
Results
Genetic alterations detected with CGS
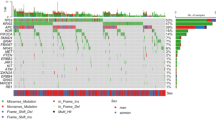
CGS of the 415-gene panel successfully detected genetic alterations in all 111 patients, and identified 31 genes altered at a frequency of more than 5% (Fig. 1B). Of the 31 genes, APC was the most frequently altered gene, in 92 of 111 patients (83%), followed by TP53 (77%), PTEN (36%), and KRAS (35%). Two of 111 patients (2%) were MSI-H.
Association between Metastatic sites and genetic alterations
Of the 111 patients, metastasis to the liver, lung, peritoneum, and distant lymph nodes at initial assessment were identified in 88, 34, 22, and 21 patients, respectively (Supplementary Table 1). Metastasectomy was performed for 49 of 111 patients. Among the 49 patients, simultaneous metastasectomy was performed for 23 patients, and metachronous metastasectomy was performed for 26 patients. Typically, chemotherapy was administered according to the guidelines3,7,25,26. Median number of lines before resection of metastasis was 1 line (range: 1–4 lines). In 31 genes altered at a frequency of more than 5%, liver metastasis was significantly associated with BRAF wild-type (P = 0.026); lung metastasis was significantly associated with APC wild-type (P = 0.030); peritoneal metastasis was not significantly associated with any genetic alterations; distant lymph node metastasis was significantly associated with ATM mutant-type and TP53 mutant-type (P = 0.010 and P = 0.024, respectively).
Factors influencing OS after primary tumor resection
Of 111 patients, 81 patients were died of cancer while 4 patients were died of other causes. The OS rate after primary tumor resection in 111 patients was 84.6% at one year, 40.8% at three years, and 11.6% at five years. Forty-five of the 111 patients had R0 resection at both primary and metastatic sites (Fig. 1A). Of these, 11 patients had undergone conversion surgery after systemic chemotherapy (Fig. 1A). Univariate analyses revealed that histopathological grade 3, N1, 2 category, BRAF V600E mutation (Fig. 2A, Supplementary Fig. 1A), and SRC mutation (Fig. 2B, Supplementary Fig. 1B) were associated with worse OS (Table 1) and R0 resection was associated with better OS (Table 1). Regarding BRAF non-V600E mutations, OS rate of six patients with BRAF non-V600E mutations showed no significant difference compared to BRAF wild-type (Fig. 2A). Multivariate analysis identified histopathological grade 3, R0 resection, BRAF V600E mutation, and SRC mutation as independent prognostic factors for OS (P = 0.041, P = 0.013, P = 0.005, and P = 0.023, respectively; Table 1).
Stratification by BRAF V600E and SRC mutation status in Stage IV CRC
BRAF mutations were identified in 13 patients (seven with V600E and six with a non-V600E mutation), and an SRC mutation was identified in 14 patients (13 with amplification and one with deletion). BRAF V600E and SRC mutations were mutually exclusive. Stratification of the 111 patients according to BRAF V600E and SRC mutation status found patients wild-type for both having significantly better OS (P < 0.001; Fig. 3) (Supplementary Figs 2 and 3). In terms of clinicopathological characteristics, SRC mutation was significantly associated with left-sided tumor and liver metastasis compared to BRAF V600E mutation (P = 0.016 and P = 0.025, respectively; Table 2).
Comparison of genetic alterations between initially resectable and initially unresectable groups
Thirty-seven and 74 patients were diagnosed as initially resectable and initially unresectable, respectively (Fig. 1A). No significant differences were observed between the two groups in genetic alterations altered at frequency of more than 10%.
Genetic alterations of initially resectable group
Of 37 patients who were diagnosed as initially resectable metastatic disease, three patients did not undergo R0 resection because of progressive disease after preoperative chemotherapy; ARID1A and ATM mutations were significantly associated with progressive disease (P = 0.026 and P = 0.042, respectively), however, no significant differences were observed in the other genetic alterations at frequency of more than 10%. Regarding MSI status, one of the three patients who showed progressive disease after preoperative chemotherapy had MSI-H tumor.
Comparison of genetic alterations between conversion and non-conversion groups in initially unresectable patients
Of 74 patients who were diagnosed as initially unresectable metastatic disease, 11 patients underwent conversion surgery (Fig. 1A, Table 3) and had significantly better OS than R2 patients (P = 0.004; Fig. 4A). Regarding the association between metastatic sites and conversion surgery, 8 of 29 patients (28%) with liver-limited disease received conversion surgery, while only 3 of 45 patients (7%) with the other initially unresectable metastases received conversion surgery. BRAF or SRC mutations were completely absent in the 11 R0 patients that underwent conversion surgery compared with 20 of the 63 R2 patients harboring a mutation in one of these genes (P = 0.023; Fig. 4B), however, no significant differences were observed in the other genetic alterations at frequency of more than 10%.
Genetic alterations in EGFR pathway and response to anti-EGFR therapy
In this cohort, 8 of 74 patients with initially unresectable metastatic disease received anti-EGFR therapy with cytotoxic agents (Fig. 1A). CGS revealed that 5 patients were “all wild-type” in EGFR pathway and theoretically should respond to anti-EGFR therapy. Three of the 5 patients (60%) showed significant response to anti-EGFR therapy: 1 patient showed complete response and alive with no evidence of disease, and 2 patients received conversion surgery after anti-EGFR therapy (Fig. 5A,B). Conversely, no patients with “mutant-type” showed complete response to anti-EGFR therapy or received conversion surgery.
Response to anti-EGFR therapy for patients with initially unresectable metastatic disease. Waterfall plot for 8 patients with initially unresectable disease after anti-EGFR therapy (A). Representative case of an “all wild-type” patient who received conversion surgery after anti-EGFR therapy. Arrows show liver metastases at base line. Arrowheads show liver metastases at best response to anti-EGFR therapy (B).
Discussion
The present study had three main findings. First, BRAF V600E and SRC mutations were identified as independent prognostic factors for OS. Second, BRAF V600E and SRC mutations were mutually exclusive, and patients with Stage IV CRC were stratified according to BRAF V600E and SRC mutation status. Third, only patients with wild-type for both BRAF V600E and SRC mutations underwent R0 conversion surgery. These results imply that BRAF V600E and SRC mutations are important molecular markers in Stage IV CRC.
CGS can detect numerous important genetic alterations in many solid cancers8. Genetic alterations in the MEK/ERK pathway, such as in KRAS, NRAS, and BRAF V600E, are benchmarks used to determine treatment strategies for patients with metastatic CRC. National Comprehensive Cancer Network (NCCN) guidelines state that all patients with metastatic CRC should have tumor tissue genotyped for KRAS, NRAS, and BRAF V600E mutations, and any patient with a known KRAS or NRAS mutation should not be treated with anti-EGFR therapy such as cetuximab and panitumumab7. AJCC 8th edition states KRAS, NRAS, and BRAF V600E mutations are poor prognostic factors in CRC (level II evidence)2. In the present analysis, we identified BRAF V600E and SRC mutations as independent prognostic factors for OS, which may have the potential to stratify Stage IV CRC and predict conversion surgery after systemic therapy. We suggest CGS be utilized in clinical practice to facilitate precision medicine.
CGS allows the simultaneous detection of BRAF V600E mutations as well as BRAF non-V600E mutations in a single assay. BRAF V600E mutation occurs at approximately 5 to 10%, and is one of the important molecular subtypes of CRC2,3,7. On the other hand, BRAF non-V600E mutations occur at approximately 1 to 5%, and show different clinicopathological characteristics, such as left-sided tumor and better prognosis, than BRAF V600E mutation27,28,29,30. Hence, we separately evaluated BRAF V600E and non-V600E mutations in this analysis.
To the best of our knowledge, this is the first report of clinical significance of SRC mutation in CRC using CGS. Previous reports demonstrated that activating mutation of SRC was found in 12% of CRC patients31,32, and indicated that SRC mutation is associated with distant metastasis and drug resistance in CRC14,15,16,17,18. In this analysis, we reported that 14 of 111 patients (13%) had SRC mutation, which was significantly associated with left-sided tumor and liver metastasis compared to BRAF V600E mutation. Multivariate analysis revealed that SRC mutations were independent prognostic factors on OS in Stage IV CRC. Moreover, BRAF V600E and SRC mutations were mutually exclusive. Taken together, we consider that SRC mutation might be an important molecular subtype in CRC.
Although this analysis found patients with BRAF V600E or SRC mutations had a poorer prognosis and seem poor candidates for conversion surgery, BRAF V600E and SRC mutations are regarded as druggable. In melanoma, the BRAF V600E mutation is the target of the BRAF-mutant inhibitor vemurafenib33. However, BRAF V600E mutant CRCs are not sensitive to BRAF-mutant inhibitors due to the feedback reaction of EGFR34. As such, clinical trials are planned for metastatic CRC using combinations of BRAF-mutant inhibitors, MEK and EGFR inhibition35,36. SRC activity is considered to play a key role in CRC development and metastasis, and there are several trials using SRC inhibitors such as dasatinib37,38. Thus, targeting BRAF V600E and SRC may represent a future treatment strategy for Stage IV CRC, which has the possibility to improve OS and rate of conversion surgery in these dismal molecular subtypes.
Emerging CGS technologies enable the detection of numerous genetic mutations in a single assay, and we can now analyze the clinical significance regarding not only “single mutation” such as BRAF V600E and SRC, but also various combinations of genetic alterations using CGS. Recently, clinical impact of “double mutation” has been reported in patients with CRC. Yamashita et al. reported that double mutation of APC and PIK3CA was associated with response to preoperative chemotherapy and poor survival for colorectal liver metastasis39. Chun et al. reported that double mutation of RAS and TP53 was associated with shorter OS after hepatectomy for colorectal liver metasstasis40. Chow et al. reported that double mutation of KRAS and TP53 was associated with lymph node metastasis in Stage II/III rectal cancer patients who received chemoradiotherapy followed by total mesorectal excision41. Although we did not find clinical significance of these double mutations (APC and PIK3CA, RAS and TP53, KRAS and TP53) in our cohort, we consider that, not only “single mutation”, but also “double mutation” might be an important concept in the era of precision medicine.
To achieve conversion surgery for initially unresectable patients, a regimen leading to high response rates and/or a large tumor size reduction is recommended, and a cytotoxic doublet plus an anti-EGFR antibody is applied for patients with RAS wild-type disease3. Although RAS mutations are established biomarkers of efficacy to anti-EGFR therapy, anti-EGFR therapy is not effective for all patients with a RAS wild-type tumor. Genetic alterations in TK receptors, the RAS pathway (other than KRAS and NRAS mutations), and the PI3K pathway are other possible mechanisms of resistance to anti-EGFR therapy25,26. In the present analysis, we defined patients who had no alterations in any of the 12 genes as “all wild-type”, and demonstrated that “all wild-type” in the EGFR pathway might be a predictor for significant response to anti-EGFR therapy and subsequent conversion surgery. Thus, we consider that, in addition to BRAF and SRC mutations, genetic alterations in EGFR pathway are also important for precision medicine of Stage IV CRC.
This analysis has several limitations. First, it was a retrospective analysis performed at two institutions and included a relatively small number of patients. Second, this analysis included patients who underwent various systemic therapies with or without targeted therapy. Third, this analysis did not include the patients who did not undergo primary tumor resection. Fourth, this analysis did not include patients whose treatment was tailored based upon their tumor’s individual genetic alterations. As we are now in the era of precision medicine, future analyses need to assess the value of CGS in patients whose treatment has been tailored to their tumor’s genetic alterations.
In conclusion, BRAF V600E and SRC mutations are important molecular markers which can predict prognosis and conversion surgery in Stage IV CRC.
References
World Health Organization. GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012, http://globocan.iarc.fr/Pages/fact_sheets_population.aspx (2012).
Amin, M. B. et al. AJCC Cancer Staging Manual. 8th edition (Springer, 2017).
Van Cutsem, E. et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 27, 1386–1422, https://doi.org/10.1093/annonc/mdw235 (2016).
Kattan, M. W. et al. American Joint Committee on Cancer acceptance criteria for inclusion of risk models for individualized prognosis in the practice of precision medicine. CA Cancer J Clin. 66, 370–374, https://doi.org/10.3322/caac.21339 (2016).
Asare, E. A., Washington, M. K., Gress, D. M., Gershenwald, G. E. & Greene, F. L. Improving the quality of cancer staging. CA Cancer J Clin. 65, 261–263, https://doi.org/10.3322/caac.21284 (2015).
Allegra, C. J. et al. American Society of Clinical Oncology provisional clinical opinion: testing for KRAS gene mutations in patients with metastatic colorectal carcinoma to predict response to anti-epidermal growth factor receptor monoclonal antibody therapy. J Clin Oncol. 27, 2091–2096, https://doi.org/10.1200/JCO.2009.21.9170 (2009).
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology-rectal cancer (version 1. 2018), https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf (2018).
Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 487, 330–337, https://doi.org/10.1038/nature11252 (2012).
Gavin, P. G. et al. Mutation profiling and microsatellite instability in stage II and III colon cancer: an assessment of their prognostic and oxaliplatin predictive value. Clin Cancer Res. 18, 6531–6541, https://doi.org/10.1158/1078-0432.CCR-12-0605 (2012).
Weiser, M. R., Jarnagin, W. R. & Saltz, L. B. Colorectal cancer patients with oligometastatic liver disease: what is the optimal approach? Oncology (Williston Park). 27, 1074–1078 (2013).
Adam, R. et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 240, 644–657 (2004).
Okuno, M. et al. Does response rate of chemotherapy with molecular target agents correlate with the conversion rate and survival in patients with unresectable colorectal liver metastases?: A systematic review. Eur J Surg Oncol. 43, 1003–1012, https://doi.org/10.1016/j.ejso.2016.08.019 (2017).
Yeatman, T. J. A renaissance for SRC. Nat Rev Cancer. 4, 470–480 (2004).
Chen, J., Elfiky, A., Han, M., Chen, C. & Saif, M. W. The role of Src in colon cancer and its therapeutic implications. Clin Colorectal Cancer. 13, 5–13, https://doi.org/10.1016/j.clcc.2013.10.003 (2014).
Termuhlen, P. M., Curley, S. A., Talamonti, M. S., Saboorian, M. H. & Gallick, G. E. Site-specific differences in pp60c-src activity in human colorectal metastases. J Surg Res. 54, 293–298 (1993).
Aligayer, H. et al. Activation of Src kinase in primary colorectal carcinoma: an indicator of poor clinical prognosis. Cancer. 94, 344–351 (2002).
Griffiths, G. J. et al. Expression of kinase-defective mutants of c-Src in human metastatic colon cancer cells decreases Bcl-xL and increases oxaliplatin- and Fas-induced apoptosis. J Biol Chem. 279, 46113–46121 (2004).
Kopetz, S. et al. Synergistic activity of the SRC family kinase inhibitor dasatinib and oxaliplatin in colon carcinoma cells is mediated by oxidative stress. Cancer Res. 69, 3842–3849, https://doi.org/10.1158/0008-5472.CAN-08-2246 (2009).
Nagahashi, M. et al. Genomic landscape of colorectal cancer in Japan: clinical implications of comprehensive genomic sequencing for precision medicine. Genome Med. 8, 136, https://doi.org/10.1186/s13073-016-0387-8 (2016).
Shimada, Y. et al. Utility of comprehensive genomic sequencing for detecting HER2-positive colorectal cancer. Hum Pathol. 66, 1–9, https://doi.org/10.1016/j.humpath.2017.02.004 (2017).
Shimada, Y. et al. Comprehensive genomic sequencing detects important genetic differences between right-sided and left-sided colorectal cancer. Oncotarget. 8, 93567–93579, https://doi.org/10.18632/oncotarget.20510 (2017).
Edge, S. B. et al. AJCC Cancer Staging Manual. 7th edition (Springer, 2010).
Bertotti, A. et al. The genomic landscape of response to EGFR blockade in colorectal cancer. Nature. 526, 263–267, https://doi.org/10.1038/nature14969 (2015).
Bertotti, A. et al. A molecularly annotated platform of patient-derived xenografts (“xenopatients”) identifies HER2 as an effective therapeutic target in cetuximab-resistant colorectal cancer. Cancer Discov. 1, 508–523, https://doi.org/10.1158/2159-8290.CD-11-0109 (2011).
Watanabe, T. et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 23, 1–34, https://doi.org/10.1007/s10147-017-1101-6 (2018).
Japanese Society for Cancer of the Colon and Rectum. Japanese classification of colorectal carcinoma. 2nd English ed. (Kanehara & Co, 2009).
Cremolini, C. et al. BRAF codons 594 and 596 mutations identify a new molecular subtype of metastatic colorectal cancer at favorable prognosis. Ann Oncol. 26, 2092–2097, https://doi.org/10.1093/annonc/mdv290 (2015).
Jones, J. C. et al. (Non-V600) BRAF Mutations Define a Clinically Distinct Molecular Subtype of Metastatic Colorectal Cancer. J Clin Oncol. 35, 2624–2630, https://doi.org/10.1200/JCO.2016.71.4394 (2017).
Shinozaki, E. et al. Clinical significance of BRAF non-V600E mutations on the therapeutic effects of anti-EGFR monoclonal antibody treatment in patients with pretreated metastatic colorectal cancer: the Biomarker Research for anti-EGFR monoclonal Antibodies by Comprehensive Cancer genomics (BREAC) study. Br J Cancer. 117, 1450–1458, https://doi.org/10.1038/bjc.2017.308 (2017).
Shimada, Y. et al. Clinical significance of BRAF non-V600E mutations in colorectal cancer: A retrospective study of two institutions. J Surg Res. 232, 72–81, https://doi.org/10.1016/j.jss.2018.06.020 (2018).
Irby, R. B. et al. Activating SRC mutation in a subset of advanced human colon cancers. Nat Genet. 21, 187–190 (1999).
Irby, R. B. & Yeatman, T. J. Role of Src expression and activation in human cancer. Oncogene. 19, 5636–5642 (2000).
Sosman, J. A. et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med. 366, 707–714, https://doi.org/10.1056/NEJMoa1112302 (2012).
Prahallad, A. et al. Unresponsiveness of colon cancer to BRAF(V600E) inhibition through feedback activation of EGFR. Nature. 483, 100–103, https://doi.org/10.1038/nature10868 (2012).
Corcoran, R. B. et al. Combined BRAF and MEK Inhibition With Dabrafenib and Trametinib in BRAF V600-Mutant Colorectal Cancer. J Clin Oncol. 33, 4023–4031, https://doi.org/10.1200/JCO.2015.63.2471 (2015).
Hyman, D. M. et al. Vemurafenib in Multiple Nonmelanoma Cancers with BRAF V600 Mutations. N Engl J Med. 373, 726–736, https://doi.org/10.1056/NEJMoa1502309 (2015).
Kopetz, S. et al. Src activity is modulated by oxaliplatin and correlates with outcomes after hepatectomy for metastatic colorectal cancer. BMC Cancer. 14, 660, https://doi.org/10.1186/1471-2407-14-660 (2014).
Parseghian, C. M. et al. Dual Inhibition of EGFR and c-Src by Cetuximab and Dasatinib Combined with FOLFOX Chemotherapy in Patients with Metastatic Colorectal Cancer. Clin Cancer Res. 23, 4146–4154, https://doi.org/10.1158/1078-0432.CCR-16-3138 (2017).
Yamashita, S. et al. APC and PIK3CA Mutational Cooperativity Predicts Pathologic Response and Survival in Patients Undergoing Resection for Colorectal Liver Metastases. Ann Surg., https://doi.org/10.1097/SLA.0000000000002245 (2017).
Chun, Y. S. et al. Deleterious Effect of RAS and Evolutionary High-risk TP53 Double Mutation in Colorectal Liver Metastases. Ann Surg., https://doi.org/10.1097/SLA.0000000000002450 (2017).
Chow, O. S. et al. KRAS and Combined KRAS/TP53 Mutations in Locally Advanced Rectal Cancer are Independently Associated with Decreased Response to Neoadjuvant Therapy. Ann Surg Oncol. 23, 2548–2555, https://doi.org/10.1245/s10434-016-5205-4 (2016).
Acknowledgements
This project was supported by Denka Co., Ltd. Tokyo, Japan and, in part, by JSPS KAKENHI Grant Number JP18K08612 and JP17K10624.
Author information
Authors and Affiliations
Contributions
Y.S. and T.W. provided substantial contributions to the design and interpretation of data, drafting of article, and final approval of article and agreed to be accountable for all aspects of the work. Y.M., M.N., H.I., Y.T., Y.H., T.A., M.N., J.S., H.K., Y.T., Y.L., S.O. and K.T. provided substantial contributions to the conception and design of study, critically revised the work, final approval of article, and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shimada, Y., Muneoka, Y., Nagahashi, M. et al. BRAF V600E and SRC mutations as molecular markers for predicting prognosis and conversion surgery in Stage IV colorectal cancer. Sci Rep 9, 2466 (2019). https://doi.org/10.1038/s41598-019-39328-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39328-6
This article is cited by
-
Oncological evaluation in the perioperative period using cfDNA with BRAF V600E mutation in patients with colorectal cancer
Scientific Reports (2021)
-
Histopathological characteristics and artificial intelligence for predicting tumor mutational burden-high colorectal cancer
Journal of Gastroenterology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.