Abstract
Evidence from recent animal studies suggest that minocycline, a broad-spectrum antibiotic capable of regulating immune processes, may possess antidepressant properties. These studies, however, have yet to be comprehensively reviewed. Accordingly, this systematic review and meta-analysis summarizes the extant literature examining the effect of minocycline on depressive-like behavior in rodent models. PubMed, PsycINFO, and Web of Science databases were systematically searched for articles that met prespecified inclusion and exclusion criteria, and standardized mean differences (SMDs) were calculated for each continuous measure of depressive-like behavior. The overall effect of minocycline on depressive-like behavior was estimated using robust variance estimation meta-analysis. Separate subgroup analyses were conducted on diseased vs healthy animal models, different rodent species, and immobility-based vs anhedonia-based measures of depressive-like behavior. A total of 22 preclinical studies (816 animals) were included. Overall, minocycline reduced depressive-like behavior in rodents (SMD = −1.07, 95% CI −1.41–−0.74, p < 0.001). Subgroup analyses revealed that minocycline reduced depressive-like behavior in diseased, but not healthy, animal models. Finally, minocycline was found to reduce both immobility-based and anhedonia-based outcomes. These findings suggest that minocycline may be an effective treatment of core depressive symptoms, and that further investigation of minocycline treatment for clinically relevant depression in humans is warranted.
Similar content being viewed by others
Introduction
Major depressive disorder is a debilitating form of mental illness that affects approximately 1 in 20 people worldwide1,2. The disorder is estimated to cost the United States over $200 billion per year in medical services and workplace-related losses3. Significantly, depression accounts for 7.5% of all years lived with disability worldwide—the greatest disability burden of any single disease2. It is also a significant source of mortality via depression-linked suicide, as well as through its association with ischemic heart disease4.
Antidepressant medications are often employed as the primary treatment for depressive illness. A recent comprehensive meta-analysis found 21 different antidepressants to be significantly more efficacious than placebo5, but the magnitude of this effect was rather modest for nearly all the drugs evaluated. Simply put, many depressed patients do not respond adequately to conventional antidepressant therapy6,7,8, and even those who do will typically face a high risk of relapse following acute treatment6,9,10. Such findings highlight the continued need for development of novel efficacious depression interventions.
Minocycline, a second-generation antibiotic with pronounced inhibitory effects on the brain’s microglia, may represent one such innovative approach. A growing body of evidence suggests that minocycline beneficially targets several pathways of relevance to the pathophysiology of depression. For instance, inflammation is strongly associated with depression11,12, and pro-inflammatory medications carry the potential to induce depressive symptoms in humans13,14. Preliminary evidence also suggests that some anti-inflammatory drugs may have antidepressant effects comparable to those of conventional pharmacological treatments15. Microglia are the primary immune cells within the central nervous system that mediate neuroinflammation16, and minocycline is capable of reducing inflammation both by directly suppressing microglia activation and by indirectly inhibiting microglia-induced inflammatory processes17. In doing so, minocycline also indirectly acts upon key monoaminergic systems implicated in depressive symptomatology, including the modulation of neurochemical cascades involving serotonin, dopamine, and norepinephrine11, as well as promotion of serotonin synthesis by reducing activation of the kynurenine pathway17. Finally, minocycline protects against oxidative stress and neuronal damage, two other harmful processes implicated in pathogenesis and maintenance of depression17,18.
Preliminary evidence also suggests that minocycline may have psychotropic effects in humans. The addition of minocycline to treatment with atypical antipsychotics has been shown to reduce negative symptoms, such blunted affect and anhedonia, in individuals with early-stage schizophrenia19,20. Additionally, an open-label study by Miyaoka et al.21 reported that minocycline, in combination with antidepressants, reduced depressive symptoms in individuals with psychotic depression. Only a few placebo-controlled clinical trials, however, have investigated minocycline as a treatment for depression in humans. Although a recent meta-analysis of three randomized controlled trials22 found support for an antidepressant effect of minocycline, it is premature to draw any substantive conclusions in light of the limited evidence available.
Despite the paucity of published clinical trials, there does exist a much larger preclinical (animal) literature regarding the antidepressant potential of minocycline. However, to the best of our knowledge, these preclinical studies have not yet been comprehensively reviewed. Accordingly, the purpose of this study is to summarize and quantify existing preclinical studies of the effect of minocycline on depressive behaviors by means of a systematic review and meta-analysis.
Results
Study selection and characteristics
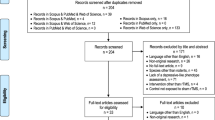
Twenty-two studies23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44 with 39 independent experimental groups and 816 rodent subjects were included in the meta-analysis (Fig. 1 and Table 1). Eleven studies used rats as experimental subjects and 11 others used mice. Twenty-five of the 39 experimental groups were identified as clinical models of disease, meaning that the animals were exposed to experimental manipulation in addition to their assigned treatment with either minocycline or placebo. Examples of experimental manipulation included chronic stress25,30,37,39,40,41, induced sickness25,27,28,29,43, olfactory bulbectomy-induced depression24,34, and induced type-1 diabetes23.
In total, 17 studies assessed immobility-based depressive-like behavior with either the forced swim test or the tail-suspension test, while seven studies assessed anhedonia-based depressive-like behavior with the sucrose preference test (and five studies used both immobility-based and anhedonia-based measures). Two studies assessed olfactory bulbectomy-induced hyperactivity with the open field test, proposed to be a measure of depressive-like behavior in this specific rodent model24,34. Finally, one study assessed social avoidance.
Doses of minocycline ranged from 10–160 mg/kg and the duration of treatment ranged from a single administration to 42 consecutive days. Minocycline was most commonly administered by either intraperitoneal injection or through drinking water.
Bias assessment
Risk of bias assessment for the included studies can be viewed in Table 2. Almost no study provided sufficient detail regarding selection, performance, or detection bias. Poor reporting of experimental and statistical methods is a recognized problem in animal research that negatively affects the validity and reproducibility of published findings45. More detail was generally provided regarding attrition, reporting, and other forms of potential bias. Over half of the included studies had a low risk of attrition and other bias, while all included studies had a low risk of reporting bias. One study had a high risk of detection bias41, and five studies had a high risk of other bias29,30,34,38,42. A separate sensitivity analysis revealed that removal of these studies did not substantively impact our final results. Overall, however, the risk of bias for each individual study is unclear, which suggests that the observed treatment effects may be overestimated46,47.
Minocycline efficacy
Combining standardized mean differences (SMDs) for the 39 included experimental groups revealed a pooled SMD of −1.07 (95% CI −1.41–−0.74, p < 0.001; Fig. 2). Minocycline administration, compared to placebo, significantly reduced depressive-like behavior in rodents. This effect was not significantly moderated in meta-regressions by either sample size (β = −0.001, 95% CI: −0.06–0.05, p = 0.961), treatment duration (β = 0.01, 95% CI: −0.01–0.04, p = 0.375), or treatment dose (β = −0.02, 95% CI: −0.03–0.003, p = 0.091).
Meta-analysis of studies investigating the antidepressant effect of minocycline in rodents. SMD = Standardized mean difference; CI = Confidence interval. An aggregate SMD is displayed for each experimental group. A measure-specific forest plot can be viewed in Supplementary Fig. S1.
Subgroup analyses revealed that minocycline administration significantly reduced depressive-like behavior only among diseased animals (SMD = −1.6, 95% CI: −1.93 –−1.26, p < 0.001); it had no significant impact among healthy animals, i.e., those naïve to experimental manipulation (SMD = −0.21, 95% CI: −0.55–0.14, p = 0.221). Minocycline also significantly reduced depressive-like behavior in both rats (SMD = −1.22, 95% CI: −1.71 –−0.72, p < 0.001) and mice (SMD = −0.97, 95% CI: −1.44 –−0.49, p < 0.001). Separate analyses revealed that minocycline significantly reduced both immobility-based (SMD = −1.17, 95% CI: −1.56 –−0.77, p < 0.001) and anhedonia-based (SMD = −0.78, 95% CI: −1.28 –−0.27, p = 0.005) outcomes. An exploratory meta-regression indicated that both minocycline pretreatment and acute treatment in diseased animals resulted in a significant reduction in depressive-like behavior compared to healthy animals (β = −0.91, 95% CI: −1.51 –−0.32, p = 0.005 and β = −1.64, 95% CI: −2.15 – −1.12, p < 0.001, respectively). Additionally, treatment following disease induction was associated with a significantly greater antidepressant effect than that of pretreatment (β = −0.72, 95% CI: −1.35 –−0.09, p = 0.027).
Publication bias and heterogeneity
Visual inspection of a funnel plot (Fig. 3) revealed the presence of potential asymmetry, which was further supported by the use of an Egger test (t = −5.92, df = 69, p < 0.001). Together, these findings suggest that publication bias may be present in the included data, resulting in the omission of non-significant or opposing findings in the final analyses. There was also high heterogeneity across the 39 experimental groups (I2 = 75.7%), indicating a great deal of inconsistency across studies. High heterogeneity and funnel plot asymmetry, which have been previously identified as a significant problem among meta-analyses of animal research, weaken the generalizability of overall findings48. Inclusion of study characteristics, such as sample size, treatment differences, and subject species/strain as moderating variables failed to reduce heterogeneity. However, separate analysis of diseased and healthy animals did reduce heterogeneity to moderate levels (I2 = 61.6% and I2 = 55.7%, respectively), supporting recent proposals that the use of consistent and well-validated experimental models may aid in the translation of preclinical research findings49.
Discussion
This systematic review and meta-analysis included 22 preclinical studies, which encompassed a total of 39 independent experimental groups and 816 rodents. Minocycline administration significantly decreased depressive-like behavior among study animals in our primary analysis, with a robust pooled standardized mean difference (SMD) of −1.07 in comparison with placebo. Moreover, 19 of the 22 included studies reported a statistically significant minocycline effect on at least one salient outcome measure.
Notably, however, minocycline only evidenced significant antidepressant effects among animals that were already experimentally stressed or diseased before they faced the depression assessment protocol—typically another acutely stressful procedure such as forced swimming or prolonged tail suspension. The drug had no significant impact upon animals that entered the challenging depression paradigm in an otherwise healthy state. This striking between-group contrast may perhaps best be explained by critical differences in depression symptom severity among the healthy and diseased rodents, as the induced disease states among study animals—chronic stress30,37,39, provoked inflammation or sickness25,27,29, and olfactory bulbectomy24,34—are all associated with an increase in depressive-like behavior23,24,25,27,37,50,51. In other words, it is possible that minocycline only exerts significant antidepressant effects in the presence of elevated levels of depressive symptomatology. This conjecture is congruent with the finding that conventional antidepressants outperform placebo most consistently in more severe cases of depression52,53. Accordingly, future clinical trials might be advised to attend carefully to baseline depression severity among study patients, and perhaps to focus the investigation of minocycline effects upon the severe and very severe depression subtypes.
In our secondary analyses, minocycline reduced depressive-like behavior in diseased animals regardless of whether the drug was administered as a pretreatment—prior to depressogenic challenge—or as an acute treatment of existing symptomatology. Such a finding has clear parallels in the clinical literature. Although antidepressants are most commonly prescribed to treat active depressive episodes54, they also seem to protect against the onset of iatrogenic (treatment-induced) depression in humans. For example, prophylactic antidepressant use reduces the risk of depression among patients receiving depressogenic interferon-α treatment55. Additionally, patients administered an antidepressant prior to surgery or radiation therapy for cancer may become less likely to develop depression during treatment56. Because minocycline pretreatment likewise protects against disease-induced depressive-like behavior in rodents, it will be valuable to see future investigation of its prophylactic value in humans, especially for medically-induced depression in clinical settings. On the other hand, we did find that the therapeutic effect of minocycline was largest when administered following disease induction, which raises the possibility that the drug might be most useful as a treatment for existing depressive symptoms.
It is also worth noting that minocycline improved performance on both immobility- and anhedonia-based measures of depressive-like behavior in study analyses. Immobility measures, such as the forced swim test and the tail suspension test, are widely used to screen potential antidepressants, and they are considered to represent negative affectivity50,51,57, although there is still some debate over the extent to which immobility challenge behaviors reflect a true depressive phenotype58,59. The sucrose preference test, on the other hand, is used to assess anhedonic behaviors59. Negative mood and anhedonia are fundamental features of depression; in fact, the current classification of major depressive disorder effectively requires at least one of these two symptoms to be present for diagnosis60. Anhedonia and dysphoria also both contribute substantially to psychosocial impairment in depression61, rendering them particularly important targets for antidepressant therapy. Inasmuch as minocycline may address both symptom domains, it may have potentially far-reaching clinical utility.
The observed antidepressant-like effects of minocycline may derive in part from the drug’s established anti-inflammatory properties, including its ability to inhibit microglia-induced inflammatory processes in the brain. In our analysis, five of six studies found that minocycline had a meaningful effect on depressive-like behavior after the experimental induction of an inflammatory state25,27,28,29,43,44. Minocycline was also observed either to alter microglia function, including glial gene expression, or to reduce biomarkers of inflammation in 10 studies24,27,28,29,34,37,39,40,42,43. Finally, one reviewed study found that minocycline decreased depressive-like behavior while simultaneously altering the composition of the gut microbiota41—symbiotic microorganisms that play a key role in regulating immune processes62—thereby highlighting another possible route by which minocycline could target inflammation.
One important interpretive caveat for the present work is the fact that the risk of bias for each reviewed study is unclear—a pervasive, well-documented limitation of much preclinical research63. Insufficient detail was provided for seven of the 10 domains enumerated in the influential SYRCLE risk-of-bias tool64, thereby raising concerns that observed results may be affected by biases related specifically to inadequate randomization, allocation concealment, and blinding procedures. Such biases can lead to an overestimation of treatment effects46,47, which can in turn hamper translational research efforts. In fact, only an estimated 10% of investigational drugs that begin clinical testing obtain final approval, and those that reach later phases of clinical trials frequently fail due to lack of efficacy65. Reducing bias in preclinical trials can help to decrease such attrition by facilitating more accurate predictions of clinical efficacy49, which may in turn decrease the financial and human burden associated with failed clinical trials. Future investigations of minocycline, accordingly, should take care to properly implement and report procedures to reduce selection, performance, and detection bias.
A major barrier facing the use of minocycline in clinical settings is acquired resistance. Similar to other forms of antibiotic, minocycline usage is linked to the development of resistant bacterial strains66. It is possible that such resistance might diminish the antidepressive efficacy of minocycline, even if not used in an antibacterial capacity. Likewise, it may be useful to investigate the degree to which adjuvant medications designed to combat acquired resistance, such as loperamide67, potentiate the effects of minocycline in depressed patients.
One important limitation of the present analysis concerns the high level of methodological heterogeneity present in the reviewed studies. Subject characteristics, animal models, treatment dose, and administration period differed significantly across studies. Because high heterogeneity reduces the predictive validity of meta-analyses48,68, the present results should be interpreted with appropriate caution. A major source of this heterogeneity was simply the methodological variability across studies, as the mere separation of healthy and diseased animals for analytic purposes led to a substantial reduction in statistical heterogeneity.
Another limitation of the present work is the fact that sample sizes of included studies typically ranged between 10 to 30 animals. Such small sample sizes, common in preclinical studies, can negatively affect both the reliability and validity of study outcomes69. They can also lead to publication bias, which our analyses suggest may be present in the minocycline preclinical literature; if so, it could further weaken the generalizability of study results69. Also, although 39 experimental groups—a reasonably large number for meta-analytic purposes—were included in the overall analysis, the number was roughly halved for our two key subgroup analyses (diseased vs. healthy animals and immobility vs. anhedonia measures). Because subgroup analysis can result in substantially reduced statistical power70, this study may not have been adequately powered to detect all statistically significant subgroup effects. Finally, our search strategy, limited to the inclusion of only mice and rat subjects and English-language articles, may have introduced bias71.
In conclusion, minocycline was observed to significantly reduce depressive-like behavior on both immobility- and anhedonia-based measures. These findings support the desirability of additional clinical trials to investigate the antidepressant potential of this antibiotic among humans. Because minocycline had no effect on depressive-like behavior in healthy animals, it may prove optimal for future research to focus principally upon the treatment of clinically significant depression, as opposed to prophylaxis among healthy individuals. Finally, the anti-inflammatory effects of minocycline should be more extensively investigated as a promising candidate mechanism of antidepressant action.
Methods
We adhered to CAMARADES guidelines for conducting systematic reviews and meta-analyses of animal studies72. The study protocol was not preregistered and can be viewed at https://doi.org/10.17504/protocols.io.vege3bw.
Criteria
Studies were deemed eligible if they met the following inclusion criteria: 1) study subjects were either rats or mice; 2) minocycline was experimentally administered; 3) depressive-like behavior was a primary or secondary study outcome.
Studies were omitted from review if they met one or more of the following exclusion criteria: 1) there was no matched control group; 2) the experimental subjects did not directly receive the administration of minocycline (e.g., the treatment was administered to the subjects’ mothers); 3) descriptive outcome data (means, standard deviations, and sample sizes) were not available for the measured depressive-like behavior; 4) the full text of the article was not available in English. Conference abstracts were omitted due to lack of necessary information.
Search strategy
Potential studies were identified by searching PubMed, PsycINFO, and Web of Science databases, from the earliest record of the databases to September 2017. Search terms included minocycline OR probiotic AND depressive-like (the exemplar PubMed search strategy can be found in the Supplementary Information). All studies were screened and evaluated in a standardized manner by two independent reviewers (DR and EC). First, the title and abstract for each search result were reviewed to identify potential studies, after which full-texts were evaluated to determine study inclusion. Disagreements between reviewers were resolved by discussion, with final decisions made by consensus. The flow chart of study selection can be viewed in Fig. 1.
Data collection
Data collection was conducted using a custom form based on CAMARADES guidelines72. Extracted data included subject information (e.g., rodent species and strain, age, experimental status), intervention type (e.g., minocycline dose and duration), and outcome data (e.g., outcome measure, sample sizes, means and variances). Different measures of depressive-like behavior were assumed to be equivalent. If depressive-like behavior was measured at multiple time points throughout the study, the final measurement of the interventional period was selected as the included data. Data presented only in graphical format were extracted using WebPlotDigitizer graph digitization software73, a program recommended for use in systematic reviews74. Potential study bias was evaluated using SYRCLE’s risk-of-bias tool64. All data and risk-of-bias evaluations were extracted by two independent reviewers (DR and EC), and disagreements during this process were resolved by discussion. Finally, 11 authors were contacted and asked to provide additional study details and data. Two authors responded and these studies were included in the final study selection. Extracted study characteristics can be viewed in Table 1.
Statistical analyses
The meta-analyses were performed with R 3.4.4 software75. All analyses were pre-specified unless otherwise stated. A standardized mean difference (SMD; also known as Hedges’ g) between minocycline-treated and matched control groups was calculated for all continuous measures of depressive-like behavior. A standard normal distribution was used to calculate confidence intervals for each SMD. Sample size, treatment duration, and treatment dose were assed as moderating variables in individual meta-regressions—study-level variables, rather than aggregated patient-level data, were chosen as moderators to avoid potential ecological bias76. Separate subgroup analyses were conducted on diseased (those receiving additional experimental manipulations prior to outcome measurement, such as induced sickness, chronic stress, etc.) and healthy animals (those receiving only minocycline or placebo intervention prior to outcome measurement), as well as mouse and rat samples. An exploratory meta-regression was conducted to compare minocycline effects, respectively, among healthy animals, diseased animals given the drug prior to disease induction (pretreatment), and diseased animals given minocycline after disease induction (treatment). Results from immobility-based (i.e. forced swim test and tail suspension test) and anhedonia-based (i.e. sucrose preference test) measures of depressive-like behavior were also analyzed in separate analyses. Multiple rodent subgroups within a single study (e.g., different rodent strains or experimental conditions) were included as independent SMDs, provided that each treatment group had a separate, matched control group. Whenever multiple treatment groups were compared against the same control group, an SMD was calculated from the combined results of the different treatment groups77.
If multiple measures of depressive-like behavior were available for a single treatment group, then a separate SMD was calculated for each outcome. Summary SMDs were calculated using robust variance estimation (RVE) meta-analyses, a form of random-effects meta-analysis shown to address dependency between SMDs measured in the same sample78. In RVE meta-analysis, multiple outcomes from a single study are included as separate SMDs and share a single study weight. SMDs were weighted by their precision (i.e., inverse variance). Between-study heterogeneity was evaluated using the I2 statistic, with values of I2 more than 25%, 50%, and 75% selected to reflect low, moderate, and high heterogeneity, respectively79. Potential publication bias was assessed for using funnel plot asymmetry and an Egger test80.
Data Availability
All data analyzed during this study are included in this article and its Supplementary Information files.
References
Ferrari, A. J. et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol. Med. 43, 471–481, https://doi.org/10.1017/s0033291712001511 (2013).
World Health Organization. Depression and other common mental disorders: Global health estimates (2017).
Greenberg, P. E., Fournier, A. A., Sisitsky, T., Pike, C. T. & Kessler, R. C. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J. Clin. Psychiatry 76, 155–162, https://doi.org/10.4088/JCP.14m09298 (2015).
Ferrari, A. J. et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 10, e1001547, https://doi.org/10.1371/journal.pmed.1001547 (2013).
Cipriani, A. et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. https://doi.org/10.1016/s0140-6736(17)32802-7 (2018).
Rush, A. J. et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am. J. Psychiatry 163, 1905–1917, https://doi.org/10.1176/ajp.2006.163.11.1905 (2006).
Souery, D. et al. Clinical factors associated with treatment resistance in major depressive disorder: results from a European multicenter study. J. Clin. Psychiatry 68, 1062–1070 (2007).
Sung, S. C. et al. The impact of chronic depression on acute and long-term outcomes in a randomized trial comparing selective serotonin reuptake inhibitor monotherapy versus each of 2 different antidepressant medication combinations. J. Clin. Psychiatry 73, 967–976, https://doi.org/10.4088/JCP.11m07043 (2012).
Kennedy, N., Abbott, R. & Paykel, E. S. Remission and recurrence of depression in the maintenance era: long-term outcome in a Cambridge cohort. Psychol. Med. 33, 827–838 (2003).
Kuyken, W. et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet 386, 63–73, https://doi.org/10.1016/s0140-6736(14)62222-4 (2015).
Slavich, G. M. & Irwin, M. R. From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychol. Bull. 140, 774–815, https://doi.org/10.1037/a0035302 (2014).
Kiecolt-Glaser, J. K., Derry, H. M. & Fagundes, C. P. Inflammation: depression fans the flames and feasts on the heat. Am. J. Psychiatry 172, 1075–1091, https://doi.org/10.1176/appi.ajp.2015.15020152 (2015).
Capuron, L. & Miller, A. H. Cytokines and psychopathology: Lessons from interferon-alpha. Biol. Psychiatry 56, 819–824, https://doi.org/10.1016/j.biopsych.2004.02.009 (2004).
Raison, C. L., Capuron, L. & Miller, A. H. Cytokines sing the blues: Inflammation and the pathogenesis of depression. Trends Immunol. 27, 24–31, https://doi.org/10.1016/j.it.2005.11.006 (2006).
Köhler, O. et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry 71, 1381–1391, https://doi.org/10.1001/jamapsychiatry.2014.1611 (2014).
Brites, D. & Fernandes, A. Neuroinflammation and Depression: Microglia Activation, Extracellular Microvesicles and microRNA Dysregulation. Front. Cell. Neurosci. 9, 476, https://doi.org/10.3389/fncel.2015.00476 (2015).
Soczynska, J. K. et al. Novel therapeutic targets in depression: Minocycline as a candidate treatment. Behav. Brain. Res. 235, 302–317, https://doi.org/10.1016/j.bbr.2012.07.026 (2012).
Michels, M. et al. The role of microglia activation in the development of sepsis-induced long-term cognitive impairment. Brain. Behav. Immun. 43, 54–59, https://doi.org/10.1016/j.bbi.2014.07.002 (2015).
Liu, F. et al. Minocycline supplementation for treatment of negative symptoms in early-phase schizophrenia: A double blind, randomized, controlled trial. Schizophr. Res. 153, 169–176, https://doi.org/10.1016/j.schres.2014.01.011 (2014).
Levkovitz, Y. et al. A double-blind, randomized study of minocycline for the treatment of negative and cognitive symptoms in early-phase schizophrenia. J. Clin. Psychiatry. 71, 138–149, https://doi.org/10.4088/JCP.08m04666yel (2010).
Miyaoka, T. et al. Minocycline as adjunctive therapy for patients with unipolar psychotic depression: An open-label study. Prog. Neuropsychopharmacol. Biol. Psychiatry 37, 222–226, https://doi.org/10.1016/j.pnpbp.2012.02.002 (2012).
Rosenblat, J. D. & McIntyre, R. S. Efficacy and tolerability of minocycline for depression: A systematic review and meta-analysis of clinical trials. J. Affect. Disord. 227, 219–225, https://doi.org/10.1016/j.jad.2017.10.042 (2018).
Amorim, D. et al. Minocycline reduces mechanical allodynia and depressive-like behaviour in type-1 diabetes mellitus in the rat. Behav. Brain. Res. 327, 1–10, https://doi.org/10.1016/j.bbr.2017.03.003 (2017).
Burke, N. N., Kerr, D. M., Moriarty, O., Finn, D. P. & Roche, M. Minocycline modulates neuropathic pain behaviour and cortical M1-M2 microglial gene expression in a rat model of depression. Brain. Behav. Immun. 42, 147–156, https://doi.org/10.1016/j.bbi.2014.06.015 (2014).
Chijiwa, T., Oka, T., Lkhagvasuren, B., Yoshihara, K. & Sudo, N. Prior chronic stress induces persistent polyI:C-induced allodynia and depressive-like behavior in rats: Possible involvement of glucocorticoids and microglia. Physiol. Behav. 147, 264–273, https://doi.org/10.1016/j.physbeh.2015.04.050 (2015).
Deak, T. et al. Behavioral responses during the forced swim test are not affected by anti-inflammatory agents or acute illness induced by lipopolysaccharide. Behav. Brain Res. 160, 125–134, https://doi.org/10.1016/j.bbr.2004.11.024 (2005).
Henry, C. J. et al. Minocycline attenuates lipopolysaccharide (LPS)-induced neuroinflammation, sickness behavior, and anhedonia. J. Neuroinflammation 5, https://doi.org/10.1186/1742-2094-5-15 (2008).
Mahmoud, M. E., Fereig, R. & Nishikawa, Y. Involvement of Host Defense Mechanisms against Toxoplasma gondii Infection in Anhedonic and Despair-Like Behaviors in Mice. Infect. Immun. 85, https://doi.org/10.1128/iai.00007-17 (2017).
Majidi, J., Kosari-Nasab, M. & Salari, A.-A. Developmental minocycline treatment reverses the effects of neonatal immune activation on anxiety- and depression-like behaviors, hippocampal inflammation, and HPA axis activity in adult mice. Brain Res. Bull. 120, 1–13, https://doi.org/10.1016/j.brainresbull.2015.10.009 (2016).
McKim, D. B. et al. Neuroinflammatory Dynamics Underlie Memory Impairments after Repeated Social Defeat. J. Neurosci. 36, 2590–2604, https://doi.org/10.1523/jneurosci.2394-15.2016 (2016).
Molina-Hernández, M., Tellez-Alcántara, N. P., Párez-García, J., Olivera-Lopez, J. I. & Jaramillo-Jaimes, M. T. Antidepressant-like actions of minocycline combined with several glutamate antagonists. Prog. Neuropsychopharmacol. Biol. Psychiatry 32, 380–386, https://doi.org/10.1016/j.pnpbp.2007.09.004 (2008).
Molina-Hernandez, M., Tellez-Alcantara, N. P., Perez-Garcia, J., Olivera-Lopez, J. I. & Jaramillo-Jaimes, M. T. Desipramine or glutamate antagonists synergized the antidepressant-like actions of intra-nucleus accumbens infusions of minocycline in male Wistar rats. Prog. Neuropsychopharmacol. Biol. Psychiatry 32, 1660–1666, https://doi.org/10.1016/j.pnpbp.2008.06.010 (2008).
Nagpal, K., Singh, S. K. & Mishra, D. Evaluation of safety and efficacy of brain targeted chitosan nanoparticles of minocycline. Int. J. Biol. Macromol. 59, 20–28, https://doi.org/10.1016/j.ijbiomac.2013.04.011 (2013).
Rinwa, P. & Kumar, A. Quercetin suppress microglial neuroinflammatory response and induce antidepressent-like effect in olfactory bulbectomized rats. Neuroscience 255, 86–98, https://doi.org/10.1016/j.neuroscience.2013.09.044 (2013).
Saravi, S. S., Mousavi, S. E., Saravi, S. S. & Dehpour, A. R. Minocycline Attenuates Depressive-Like Behaviour Induced by Rat Model of Testicular Torsion: Involvement of Nitric Oxide Pathway. Basic Clin. Pharmacol. Toxicol. 118, 249–258, https://doi.org/10.1111/bcpt.12489 (2016).
Saravi, S. S. et al. On the effect of minocycline on the depressive-like behavior of mice repeatedly exposed to malathion: interaction between nitric oxide and cholinergic system. Metab. Brain Dis. 31, 549–561, https://doi.org/10.1007/s11011-015-9764-z (2016).
Singh, B., Mourya, A., Sah, S. P. & Kumar, A. Protective effect of losartan and ramipril against stress induced insulin resistance and related complications: Anti-inflammatory mechanisms. Eur. J. Pharmacol. 801, 54–61, https://doi.org/10.1016/j.ejphar.2017.02.050 (2017).
Singh, T. & Goel, R. K. Adjuvant indoleamine 2,3-dioxygenase enzyme inhibition for comprehensive management of epilepsy and comorbid depression. Eur. J. Pharmacol. 784, 111–120, https://doi.org/10.1016/j.ejphar.2016.05.019 (2016).
Tong, L. et al. Microglia Loss Contributes to the Development of Major Depression Induced by Different Types of Chronic Stresses. Neurochem. Res. https://doi.org/10.1007/s11064-017-2270-4 (2017).
Wang, H. T. et al. Early-Life Social Isolation-Induced Depressive-Like Behavior in Rats Results in Microglial Activation and Neuronal Histone Methylation that Are Mitigated by Minocycline. Neurotox. Res. 31, 505–520, https://doi.org/10.1007/s12640-016-9696-3 (2017).
Wong, M. L. et al. Inflammasome signaling affects anxiety- and depressive-like behavior and gut microbiome composition. Mol. Psychiatry 21, 797–805, https://doi.org/10.1038/mp.2016.46 (2016).
Xu, N. et al. Spared Nerve Injury Increases the Expression of Microglia M1 Markers in the Prefrontal Cortex of Rats and Provokes Depression-Like Behaviors. Front. Neurosci. 11, https://doi.org/10.3389/fnins.2017.00209 (2017).
Zheng, L. S., Kaneko, N. & Sawamoto, K. Minocycline treatment ameliorates interferon-alpha- induced neurogenic defects and depression-like behaviors in mice. Front. Cell. Neurosci 9, 5, https://doi.org/10.3389/fncel.2015.00005 (2015).
Zheng, X. et al. Peripheral immunomodulation with ginsenoside Rg1 ameliorates neuroinflammation-induced behavioral deficits in rats. Neuroscience 256, 210–222, https://doi.org/10.1016/j.neuroscience.2013.10.023 (2014).
Kilkenny, C. et al. Survey of the quality of experimental design, statistical analysis and reporting of research using animals. PLoS One 4, e7824, https://doi.org/10.1371/journal.pone.0007824 (2009).
Crossley, N. A. et al. Empirical evidence of bias in the design of experimental stroke studies: A metaepidemiologic approach. Stroke 39, 929–934, https://doi.org/10.1161/strokeaha.107.498725 (2008).
Bebarta, V., Luyten, D. & Heard, K. Emergency medicine animal research: Does use of randomization and blinding affect the results? Acad. Emerg. Med. 10, 684–687 (2003).
Moja, L. et al. Flaws in animal studies exploring statins and impact on meta-analysis. Eur. J. Clin. Invest. 44, 597–612, https://doi.org/10.1111/eci.12264 (2014).
Denayer, T., Stöhr, T. & Van Roy, M. Animal models in translational medicine: Validation and prediction. New Horiz. Transl. Med. 2, 5–11, https://doi.org/10.1016/j.nhtm.2014.08.001 (2014).
Krishnan, V. & Nestler, E. J. Animal models of depression: molecular perspectives. Curr. Top. Behav. Neurosci. 7, 121–147, https://doi.org/10.1007/7854_2010_108 (2011).
Yan, H. C., Cao, X., Das, M., Zhu, X. H. & Gao, T. M. Behavioral animal models of depression. Neurosci. Bull. 26, 327–337, https://doi.org/10.1007/s12264-010-0323-7 (2010).
Kirsch, I. et al. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med. 5, e45, https://doi.org/10.1371/journal.pmed.0050045 (2008).
Fournier, J. C. et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA 303, 47–53, https://doi.org/10.1001/jama.2009.1943 (2010).
American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder - third edition. Available from https://www.psychiatry.org/psychiatrists/practice/clinical-practice-guidelines (2010).
Jiang, H. Y. et al. Specific serotonin reuptake inhibitors prevent interferon-alpha-induced depression in patients with hepatitis C: a meta-analysis. Clin. Gastroenterol. Hepatol. 12, 1452–1460, e1453, https://doi.org/10.1016/j.cgh.2013.04.035 (2014).
Lydiatt, W. M., Bessette, D., Schmid, K. K., Sayles, H. & Burke, W. J. Prevention of depression with escitalopram in patients undergoing treatment for head and neck cancer: randomized, double-blind, placebo-controlled clinical trial. JAMA Otolaryngol. Head Neck Surg. 139, 678–686, https://doi.org/10.1001/jamaoto.2013.3371 (2013).
Slattery, D. A. & Cryan, J. F. Using the rat forced swim test to assess antidepressant-like activity in rodents. Nat. Protoc. 7, 1009–1014, https://doi.org/10.1038/nprot.2012.044 (2012).
Molendijk, M. L. & de Kloet, E. R. Immobility in the forced swim test is adaptive and does not reflect depression. Psychoneuroendocrinology 62, 389–391, https://doi.org/10.1016/j.psyneuen.2015.08.028 (2015).
Nestler, E. J. & Hyman, S. E. Animal models of neuropsychiatric disorders. Nat. Neurosci. 13, 1161–1169, https://doi.org/10.1038/nn.2647 (2010).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edn, (American Psychiatric Publishing 2013).
Fried, E. I. & Nesse, R. M. The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS One 9, e90311, https://doi.org/10.1371/journal.pone.0090311 (2014).
Carabotti, M., Scirocco, A., Maselli, M. A. & Severi, C. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 28, 203–209 (2015).
Macleod, M. R. et al. Risk of Bias in Reports of In Vivo Research: A Focus for Improvement. PLoS Biol. 13, e1002273, https://doi.org/10.1371/journal.pbio.1002273 (2015).
Hooijmans, C. R. et al. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 14, 43, https://doi.org/10.1186/1471-2288-14-43 (2014).
Hay, M., Thomas, D. W., Craighead, J. L., Economides, C. & Rosenthal, J. Clinical development success rates for investigational drugs. Nat. Biotechnol. 32, 40–51, https://doi.org/10.1038/nbt.2786 (2014).
Ochsendorf, F. Minocycline in acne vulgaris: benefits and risks. Am. J. Clin. Dermatol. 11, 327–341, https://doi.org/10.2165/11319280-000000000-00000 (2010).
Worthington, R. J. & Melander, C. Combination approaches to combat multidrug-resistant bacteria. Trends Biotechnol. 31, 177–184, https://doi.org/10.1016/j.tibtech.2012.12.006 (2013).
Melsen, W. G., Bootsma, M. C., Rovers, M. M. & Bonten, M. J. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin. Microbiol. Infect. 20, 123–129, https://doi.org/10.1111/1469-0691.12494 (2014).
Button, K. S. et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat. Rev. Neurosci. 14, 365–376, https://doi.org/10.1038/nrn3475 (2013).
Borenstein, M. & Higgins, J. P. Meta-analysis and subgroups. Prev. Sci. 14, 134–143, https://doi.org/10.1007/s11121-013-0377-7 (2013).
Jüni, P., Holenstein, F., Sterne, J., Bartlett, C. & Egger, M. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int. J. Epidemiol. 31, 115–123 (2002).
Vesterinen, H. M. et al. Meta-analysis of data from animal studies: a practical guide. J. Neurosci. Methods 221, 92–102, https://doi.org/10.1016/j.jneumeth.2013.09.010 (2014).
Rohatgi, A. WebPlotDigitizer http://arohatgi.info/WebPlotDigitizer (2017).
Tsafnat, G. et al. Systematic review automation technologies. Syst. Rev. 3, 74, https://doi.org/10.1186/2046-4053-3-74 (2014).
R Core Team. R: A language and environment for statistical computing. (R Foundation for Statistical Computing, Vienna, Austria 2016).
Reade, M. C., Delaney, A., Bailey, M. J. & Angus, D. C. Bench-to-bedside review: avoiding pitfalls in critical care meta-analysis–funnel plots, risk estimates, types of heterogeneity, baseline risk and the ecologic fallacy. Crit. Care 12, 220, https://doi.org/10.1186/cc6941 (2008).
Cochrane Handbook for Systematic Reviews of Interventions (eds J. P. T. Higgins & S. Green). Version 5.1.0. Available from http://handbook.cochrane.org (The Cochrane Collaboration 2011).
Tipton, E. Small sample adjustments for robust variance estimation with meta-regression. Psychol. Methods 20, 375–393, https://doi.org/10.1037/met0000011 (2015).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Bmj 327, 557–560, https://doi.org/10.1136/bmj.327.7414.557 (2003).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. Bmj 315, 629–634 (1997).
Acknowledgements
This manuscript was supported by grant number R25GM62232 from the National Institute of General Medical Science (NIGMS), a component of the National Institutes of Health (NIH). This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
E.C. and S.I. conceived of the review and analysis. E.C. and D.R. performed the literature review and collected data. D.R. analyzed the results. All authors contributed to the drafting and revision of this manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reis, D.J., Casteen, E.J. & Ilardi, S.S. The antidepressant impact of minocycline in rodents: A systematic review and meta-analysis. Sci Rep 9, 261 (2019). https://doi.org/10.1038/s41598-018-36507-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-36507-9
This article is cited by
-
Regulation of synaptic connectivity in schizophrenia spectrum by mutual neuron-microglia interaction
Communications Biology (2023)
-
Microglia and their LAG3 checkpoint underlie the antidepressant and neurogenesis-enhancing effects of electroconvulsive stimulation
Molecular Psychiatry (2022)
-
The antidepressant and anxiolytic effects of cannabinoids in chronic unpredictable stress: a preclinical systematic review and meta-analysis
Translational Psychiatry (2022)
-
Beyond the lesion site: minocycline augments inflammation and anxiety-like behavior following SCI in rats through action on the gut microbiota
Journal of Neuroinflammation (2021)
-
Anti-inflammatory IL-10 administration rescues depression-associated learning and memory deficits in mice
Journal of Neuroinflammation (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.