Abstract
Dysphagia is a side effect of nasopharyngeal carcinoma chemo-radiotherapy (CRT) which greatly influences the quality of life of the patients. We analyzed late dysphagia in 134 patients with nasopharyngeal cancer undergoing radical radiotherapy (RT), and correlated these findings with dose–volume histogram (DVH) parameters of the swallowing organs at risk (SWOARs). DVH parameters of SWOARs were correlated with late dysphagia, and with RTOG/EORTC scale score and the M. D. Anderson dysphagia inventory (MDADI) score. The mean dose (Dmean) to the superior and inferior constrictor muscles (SCM and ICM) and age were associated with grade 2 late dysphagia. Receiver operating characteristic (ROC) curves showed that the threshold values for grade 2 late dysphagia were: Dmean to SCM ≥ 67 Gy, partial volume receiving specified dose of 60 Gy (V60) of SCM ≥ 95%, Dmean to ICM ≥ 47 Gy, and V50 of ICM ≥ 23%. The areas under the ROC curve were 0.681 (p = 0.02), 0.677 (p = 0.002), 0.71 (p < 0.001) and 0.726 (p < 0.001) respectively. Our study demonstrates a significant relationship between late dysphagia and the radiation doses delivered to the SCM and ICM. Our findings suggest that physicians should be cautious in reducing the RT dose to SWOARs in order to avoid severe dysphagia. Further prospective trials are necessary to recommend this as part of routine clinical practice.
Similar content being viewed by others
Introduction
Nasopharyngeal carcinoma (NPC) is a common malignancy in Southern China, especially in Guangdong and Guangxi provinces1,2. Radiotherapy is the primary treatment strategy for non-disseminated NPC due to its unique anatomical position and radio-sensitivity. In recent years, intensity-modulated radiation therapy (IMRT), which is characterized by high conformity and the benefit of sparing the organs at risk (OARs), has been used for NPC treatment. Compared to conventional radiotherapy, IMRT reduces the incidence of several complications such as oral mucositis, xerostomia and temporal lobe injury, and improves patients’ quality of life (QOL)3. Late dysphagia has however emerged as a common side effect of NPC radiotherapy4,5.
Normal swallowing is a complex process involving several muscles and cranial nerves. Late dysphagia is associated with swallowing-related structures, tumor, and treatment6,7. However, the IMRT dose tolerances of the swallowing-related structures are poorly characterized. Furthermore, much of the existing data is based on the experiences of the 2D-CRT era, and concrete clinical evidence regarding IMRT is lacking8. Therefore, it is necessary to further study the radio-tolerance of SWOARs in NPC patients receiving IMRT.
We retrospectively reviewed the clinical and dosimetric data of a cohort of NPC patients who developed late dysphagia after IMRT, and performed dose-volume outcome analysis to determine the effect of different doses on swallowing-related structures. The aim was to evaluate the potential relationship between the planned dose–volume parameters and the observed incidence of late dysphagia in these patients. After a re-contouring of the SWOARs according to recently published guidelines, we determined the dose tolerated by the SWOARs that achieved the highest uncomplicated tumor control.
Materials and Methods
Patient population
A total of 158 patients with NPC who received IMRT at the First Affiliated Hospital of Guangxi Medical University from March 2013 to April 2014 were initially enrolled. The inclusion criteria were 1) treatment with curative IMRT at a dose delivered to the gross tumor volume (PGTVnx) of at least 66 Gy either alone or in combination with concomitant chemotherapy, 2) the availability of treatment plan record with DVH parameters, and 3) willingness to complete the stipulated questionnaires. The exclusion criteria were: 1) persistent/recurrent tumor, 2) distant metastasis, 3) previous radiotherapy for another head and neck tumor or with palliative intent, 4) Any RTOG/EORTC grade swallowing dysfunction before treatment and tumor invasion in oropharynx and hypopharynx, and 5) hoarseness, nasal regurgitation, lingual deviation and atrophy, coughing while drinking, unclear enunciation etc. The newly diagnosed NPC patients who suffered from dysphagia before treatment were still excluded so as to ensure that the observed dysphagia was only induced by radiation-related SWOARs dysfunction but not by lower cranial neuropathy. Based on these criteria, 24 patients were excluded: 3 were lost during the follow-up, 15 underwent a second treatment (re-irradiation and/or chemotherapy) due to either distant metastasis (n = 9) or loco-regional relapse (n = 6), and 6 were excluded because they had swallowing dysfunction before treatment. The remaining 134 patients received the questionnaires and provided informed consent. All methods were in accordance with the relevant guidelines and regulations, and were approved by the Ethical Review Committee of the First Affiliated Hospital of Guangxi Medical University. All clinical information of the participants is available and can be accessed.
Outline of swallowing structures
Based on published studies9,10,11,12, the SWOARs comprise of the following five muscles: the superior constrictor muscle (SCM), middle constrictor muscle (MCM) and inferior constrictor muscle (ICM) which are part of the pharyngeal constrictor muscle (PCM), the cricopharyngeus muscle (CPM), and the esophagus inlet muscle (EIM). The SCM, MCM and ICM form the posterior and lateral pharyngeal walls. The SCM extends from the caudal tip of the pterygoid plate to the lower edge of second cervical vertebra, MCM extends from the upper edge of third cervical vertebra to the lower edge of the hyoid bone, and ICM extends from below the lower edge of the hyoid bone to the lower edge of the arytenoid cartilage. CPM extended from below the lower edge of the arytenoid cartilage to the lower edge of the cricoid cartilage, and EIM consisted of the 1 cm of the muscular compartment of the esophagus inlet. Anatomical borders of each SWOAR are indicated in Table 1, and further delineated in Fig. 1.
Assessment of dysphagia
All patients were followed-up to assess late dysphagia using the RTOG/EORTC scale13. Patient-reported clinical swallowing function was also assessed by the M.D. Anderson dysphagia inventory (MDADI) scoring, which consists of 20 questions with global, emotional, functional and physical subscales. In the MDADI questionnaire, a higher score is equated to a better quality of life and less swallowing trouble14.
Statistical analyses
Age, duration of follow up and dosimetric variables (Dmean and Vn) were analyzed. Data conforming to normal distribution were compared using t-test, and data with non-normal distribution using the Wilcoxon Rank-Sum test. The χ2 or Fisher’s test were used to compare the grade 0-1 and grade 2 late dysphagia groups.
The clinical and dosimetric variables were assessed in the univariate analysis, and were incorporated into a binary logistic regression model to assess their independent contribution. Prior to the multivariate analysis, a correlation matrix was produced to identify those potential prognostic factors with high correlations, in particular between the DVH parameters. Based on Pearson correlation coefficients P ≥ 0.70 or variance inflation factor (VIF) ≥ 10 between the candidate prognostic factors, only one variable was selected and incorporated into the model to avoid multicollinearity, which may have negatively affected the generality of the model. The dosimetric variables that resulted from the independent factors of multivariate analysis and their corresponding significant DVH parameters in the univariate analysis were used for receiver operating characteristic (ROC) curve analysis, in order to calculate their threshold values of late dysphagia and assess their diagnostic capability. The dosimetric variables, which showed a correlation in the univariate analysis, were subjected to principal component analysis (PCA). Pearson correlation coefficients (r) were used to analyze the association between MDADI results and all demographic parameters, dosimetric variables and the degree of dysphagia (RTOG/EORTC scale).
Statistical analysis was performed using the STATISTICA 22.0 software. A p-value of ≤ 0.05 was considered statistically significant. The figures were generated using GRAPHPAD 5.0.
Results
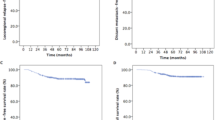
Patents characteristics and late toxicity
Table 2 summarized the clinical characteristics of 134 patients diagnosed with NPC. The median age of the patients was 44 years (range 18–71 years). During the median follow-up of 34 months (range 25–44 months), 71 patients (53%) were reportedly suffering from late dysphagia. Late dysphagia, according to the RTOG/EORTC scale, was scored as grade (G) 0 in 63 (47%) patients, G1 in 37 (28%) patients and G2 in 34 patients (25%). No cases of G3-4 toxicity were found. We then divided the patients into Group 1 (grade 0–1) and Group 2 (grade 2) based on the severity scores of dysphagia, and found that age and gender were related to the grade level of late dysphagia in the univariate analysis (p < 0.05).
Association between the dosimetric parameters of SWOARs and late dysphagia
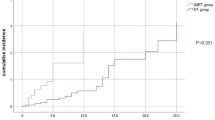
The correlation between Dmean, V50, and V60 to the affected constrictor muscles and the severity of the late dysphagia is shown in Table 3. The respective Dmean to the PCM, SCM, MCM and ICM were each associated with G2 late dysphagia (p ≤ 0.001). Similarly, the respective V60 of the SCM and MCM, and V50 of the MCM and ICM were correlated with G2 late dysphagia (p ≤ 0.01). Multivariate analysis by forward elimination of insignificant explanatory variables was performed to adjust for various factors. Due to the high correlation between the Dmean and the V50/V60 of the constrictor muscles (Pearson coefficient > 0.8, p < 0.001), we used the Dmeans to SCM and ICM for multivariate analysis, with age and gender as co-variants. Multivariate analysis showed that age (OR 1.050, 95%CI 1.005–1.098, p = 0.031), Dmean to SCM (OR 1.170, 95%CI 1.018–1.344, p = 0.027) and Dmean to ICM (OR 1.251, 95%CI 1.074–1.457, p = 0.004) were the independent predictors (Table 4). Finally, we evaluated the dose tolerance of the grade 2 late dysphagia using ROC curves in terms of the above significant independent variables. Due to the strong correlation between the V50/V60 and Dmean, V50 of ICM and V60 of SCM were also evaluated using ROC curve analysis. The significant dosimetric parameters and cut-off points of the ROC curve analysis are shown in Table 5. Dmean to SCM ≥ 67 Gy, Dmean to ICM ≥ 47 Gy, V60 of SCM ≥ 95% and V50 of ICM ≥ 23% were the threshold values of grade 2 late dysphagia (Supplementary Figures 1–4). The areas under the ROC curves, as showed in Fig. 2, were 0.681 for Dmean to SCM (sensitivity 0.647, specificity 0.65, p = 0.002) and 0.71 for Dmean to ICM (sensitivity 0.676, specificity 0.67, p < 0.001). In the same way, the areas under the ROC curves were 0.677 for V60 of SCM (sensitivity 0.735, specificity 0.6, p = 0.002) and 0.726 for V50 of ICM (sensitivity 0.765, specificity 0.63, p < 0.001). In the principal component analysis, KMO and Bartlett tests showed correlations between the included variables (p < 0.001). The scree plot suggested three principle components as the optimal number which could explain 75.3% of the variation. Subsequently, a rotating element matrix was used to identify the dosimetric variables that had different attributes (Table 6). Dmean to ICM, V50 of ICM and V60 of ICM had the most distinguishable contributions to the first principal component. Furthermore, the reliability and validity were examined by MDADI as showed in Table 7. The CPM and EIM were non-significant factors in relation to the grade 2 late dysphagia.
Discussion
Although IMRT with concomitant chemotherapy for NPC has a high rate of local control, radiation-induced late dysphagia is usually debilitating to patients. Furthermore, late dysphagia in NPC patients treated with IMRT is poorly understood. It is essential to know the dose tolerance for dysphagia in order to predict the safety of treatment plans. The aim of this retrospective study was to improve the understanding of late dysphagia and thus optimize IMRT for NPC.
The effect of the radiation dose and volume on the healthy tissues is a major concern in radiotherapy. Patterson et al. evaluated the swallowing function of 18 NPC patients using a patient-reported oral function score with fiberoptic endoscopic examination; 5 patients suffered from moderate late dysphagia but no severe cases were observed4. Another study by Xu et al. showed that 50% of NPC patients treated with IMRT had swallowing dysfunction15. Our results, which are consistent with the previous studies, showed that 53% of the patients experienced late dysphagia and grade 2 late dysphagia occurred in 25% of the patients. Therefore, treatment-related late toxicity may worsen patients’ quality of life.
Some recent studies have assessed the relationship between the dose-volume parameters of swallowing structures and late dysphagia in patients undergoing treatment for head and neck tumors9,16,17. Deantonio et al. reported that >50 Gy Dmean to SCM and MCM correlated with grade 2–3 late dysphagia, and Dmean to MCM is the only significant predictor of late grade dysphagia18. In the prospective study of Feng et al., patients with adequate aspiration received >60 Gy Dmean to PCM19. Furthermore, studies have also analyzed the incidence of late dysphagia relative to tumor location. The primary tumor site in the larynx, hypopharynx and posterior pharyngeal wall was associated with long-term dysphagia20,21,22. However, very few studies have been conducted on late dysphagia in NPC patients who received IMRT, and did not reveal any significant association between late dysphagia and dose-volume effect. A study found that the SCM, MCM and ICM easily tolerated radiation doses in patients with a small tumor volume, but had a lower tolerance in case of larger tumors23. Our results demonstrated that the doses delivered to the SCM and ICM were independent factors predicting G2 late dysphagia. Consequently, we found that the Dmean to SCM ≥ 67 Gy, V60 of SCM ≥ 95%, Dmean to ICM ≥ 47 Gy and V50 of ICM ≥ 23% were the threshold doses of G2 late dysphagia in NPC patients treated with IMRT. A study evaluated the anatomical changes in the PCM after chemo-radiotherapy of head and neck cancer and their dose-effect relationships using MRI7. The MRI signals and the muscle thickness changed significantly as the dose increased, suggesting that the underlying causes of SWOARs dysfunction are inflammation and edema. On the other hand, Truong et al. reported that late dysphagia was related to radiation-induced free radical damage to the SWOARs and subsequent development of PCM fibrosis, with stricture formation and loss of muscle pliability24. They also found that oxidative stress and microvascular injury to the endothelium correlated with progressive changes in the blood. Therefore, tumor location and radiation dose to the SWOARs are significant factors in late dysphagia. Levendag et al. found significant relationships between the Dmean > 50 Gy to the SCM and MCM and severe dysphagia complaints10. Christianen et al. also showed that late dysphagia correlated with Dmean > 60 Gy to SCM or MCM25. Based on the results of these two studies, the SCM and MCM likely have a major role in late dysphagia, while ICM may not influence swallowing symptoms. In contrast, Dirix et al. indicated that a Dmean > 50 Gy to the MCM and ICM significantly correlated with late dysphagia. Nevertheless, our results showed that the dose delivered to ICM also had a crucial impact on late dysphagia, as did between the dose and SCM, whereas the dose delivered to MCM had no impact.
IMRT is widely used for patients with NPC, and delivers a high radiation dose to tumors while maintaining a safe dose for normal tissues surrounding the tumor. This technique also exhibits excellent tumor coverage. Compared to three-dimensional conformational radiation therapy, IMRT in head and neck reduces adverse effects such as dysphagia and thus improves quality of life (QOL)26,27. Currently, despite expert recommendations to spare a portion of the SWOARs in order to reduce dysphagia, the dose constraint to PCM is unclear26,28. Studies have shown different results, possibly due to methodological differences and the ambiguous contouring of the SWOARs. Limiting the radiation dose to the crucial SWOARs is expected to decrease the incidence and severity of radiation-induced dysphagia with IMRT. A study used the new technique of swallowing sparing IMRT (SW-IMRT), and reduced the doses to the SWOARs based on the following criteria listed in order of priority: (1) minimizing the mean dose to the SCM, (2) minimizing the mean dose to the MCM, (3) minimizing the mean dose to the supraglottic larynx, and (4) minimizing the proportion of the EIM receiving ≥60 Gy (EIM V60). Compared to the standard IMRT (ST-IMRT), SW-IMRT reduced the mean dose to the various SWOARs, along with a 9% mean reduction (3%-20%) in predicted physician-rated RTOG/EORTC grade 2–4 swallowing dysfunction27.
The results of our study must be viewed cautiously because of several limitations. Due to the retrospective approach, we used the previously described dose tolerance in clinical practice in a prospective manner till they were validated. The second limitation is regarding the method of delineation of the swallowing structures that, although performed by an experienced radiation oncologist, are not fully standardized and could thus result in a bias. Other limitations are the small sample size, lack of anatomical examinations such as endoscopy, MRI, and barium meal test.
Conclusion
We found a significant relationship between late dysphagia and the radiation dose delivered to superior and inferior pharyngeal constrictor muscles during radiotherapy of NPC. The Dmean to SCM ≥ 67 Gy, V60 of SCM ≥ 95%, Dmean to ICM ≥ 47 Gy, and V50 of ICM ≥ 23% correlated with grade 2 late dysphagia. The optimal modality to assess late dysphagia and the most appropriate dose limits of constrictor muscles are still open issues and should be further investigated. A prospective study is needed to validate the findings of the present study, and to determine whether the dosimetric benefits of this treatment strategy translate into better clinical outcomes.
References
Yu, M. C. & Yuan, J. M. Epidemiology of nasopharyngeal carcinoma. Seminars in cancer biology 12, 421–429 (2002).
Chua, M. L., Wee, J. T., Hui, E. P. & Chan, A. T. Nasopharyngeal carcinoma. Lancet (London, England) 387, 1012–1024, https://doi.org/10.1016/s0140-6736(15)00055-0 (2016).
Lai, S. Z. et al. How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? International journal of radiation oncology, biology, physics 80, 661–668, https://doi.org/10.1016/j.ijrobp.2010.03.024 (2011).
Patterson, M. et al. Functional swallowing outcomes in nasopharyngeal cancer treated with IMRT at 6 to 42 months post-radiotherapy. Dysphagia 29, 663–670, https://doi.org/10.1007/s00455-014-9559-0 (2014).
Chang, Y. C. et al. A 2-year follow-up of swallowing function after radiation therapy in patients with nasopharyngeal carcinoma. Archives of physical medicine and rehabilitation 92, 1814–1819, https://doi.org/10.1016/j.apmr.2011.06.008 (2011).
Logemann, J. A. et al. Swallowing disorders in the first year after radiation and chemoradiation. Head & neck 30, 148–158, https://doi.org/10.1002/hed.20672 (2008).
Popovtzer, A., Cao, Y., Feng, F. Y. & Eisbruch, A. Anatomical changes in the pharyngeal constrictors after chemo-irradiation of head and neck cancer and their dose-effect relationships: MRI-based study. Radiotherapy and oncology: journal of the European Society for Therapeutic Radiology and Oncology 93, 510–515, https://doi.org/10.1016/j.radonc.2009.05.013 (2009).
Emami, B. et al. Tolerance of normal tissue to therapeutic irradiation. International journal of radiation oncology, biology, physics 21, 109–122 (1991).
Christianen, M. E. et al. Predictive modelling for swallowing dysfunction after primary (chemo)radiation: results of a prospective observational study. Radiotherapy and oncology: journal of the European Society for Therapeutic Radiology and Oncology 105, 107–114, https://doi.org/10.1016/j.radonc.2011.08.009 (2012).
Levendag, P. C. et al. Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiation therapy dose to the superior and middle constrictor muscle: a dose-effect relationship. Radiotherapy and oncology: journal of the European Society for Therapeutic Radiology and Oncology 85, 64–73, https://doi.org/10.1016/j.radonc.2007.07.009 (2007).
Rancati, T. et al. Radiation dose-volume effects in the larynx and pharynx. International journal of radiation oncology, biology, physics 76, S64–69, https://doi.org/10.1016/j.ijrobp.2009.03.079 (2010).
Mazzola, R. et al. Dose-volume-related dysphagia after constrictor muscles definition in head and neck cancer intensity-modulated radiation treatment. The British journal of radiology 87, 20140543, https://doi.org/10.1259/bjr.20140543 (2014).
Cox, J. D., Stetz, J. & Pajak, T. F. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). International journal of radiation oncology, biology, physics 31, 1341–1346, https://doi.org/10.1016/0360-3016(95)00060-c (1995).
Zhang, L. J. et al. Psychometric Properties of the Chinese Version of the M.D. Anderson Dysphagia Inventory for Head and Neck Cancer Patients. Cancer nursing 40, E9–e16, https://doi.org/10.1097/ncc.0000000000000397 (2017).
Xu, L. et al. Prospective study of swallowing function protection with intensity modulated radiation therapy in nasopharyngeal carcinoma. Chinese Journal of Cancer Prevention and Treatment 22, 1695–1699 (2015).
Gensheimer, M. F., Nyflot, M., Laramore, G. E., Liao, J. J. & Parvathaneni, U. Contribution of submandibular gland and swallowing structure sparing to post-radiation therapy PEG dependence in oropharynx cancer patients treated with split-neck IMRT technique. Radiation oncology (London, England) 11, 151, https://doi.org/10.1186/s13014-016-0726-3 (2016).
Dornfeld, K. et al. Radiation doses to structures within and adjacent to the larynx are correlated with long-term diet- and speech-related quality of life. International journal of radiation oncology, biology, physics 68, 750–757, https://doi.org/10.1016/j.ijrobp.2007.01.047 (2007).
Deantonio, L., Masini, L., Brambilla, M., Pia, F. & Krengli, M. Dysphagia after definitive radiotherapy for head and neck cancer. Correlation of dose-volume parameters of the pharyngeal constrictor muscles. Strahlentherapie und Onkologie: Organ der Deutschen Rontgengesellschaft… [et al] 189, 230–236, https://doi.org/10.1007/s00066-012-0288-8 (2013).
Feng, F. Y. et al. Intensity-modulated radiotherapy of head and neck cancer aiming to reduce dysphagia: early dose-effect relationships for the swallowing structures. International journal of radiation oncology, biology, physics 68, 1289–1298, https://doi.org/10.1016/j.ijrobp.2007.02.049 (2007).
Caudell, J. J. et al. Factors associated with long-term dysphagia after definitive radiotherapy for locally advanced head-and-neck cancer. International journal of radiation oncology, biology, physics 73, 410–415, https://doi.org/10.1016/j.ijrobp.2008.04.048 (2009).
Teguh, D. N. et al. Treatment techniques and site considerations regarding dysphagia-related quality of life in cancer of the oropharynx and nasopharynx. International journal of radiation oncology, biology, physics 72, 1119–1127, https://doi.org/10.1016/j.ijrobp.2008.02.061 (2008).
Dirix, P., Abbeel, S., Vanstraelen, B., Hermans, R. & Nuyts, S. Dysphagia after chemoradiotherapy for head-and-neck squamous cell carcinoma: dose-effect relationships for the swallowing structures. International journal of radiation oncology, biology, physics 75, 385–392, https://doi.org/10.1016/j.ijrobp.2008.11.041 (2009).
Yao, J. J. et al. A prospective study on radiation doses to organs at risk (OARs) during intensity-modulated radiotherapy for nasopharyngeal carcinoma patients. Oncotarget 7, 21742–21752, https://doi.org/10.18632/oncotarget.7826 (2016).
Truong, M. T. et al. Correlating computed tomography perfusion changes in the pharyngeal constrictor muscles during head-and-neck radiotherapy to dysphagia outcome. International journal of radiation oncology, biology, physics 82, e119–127, https://doi.org/10.1016/j.ijrobp.2011.04.058 (2012).
Christianen, M. E., Langendijk, J. A., Westerlaan, H. E., van de Water, T. A. & Bijl, H. P. Delineation of organs at risk involved in swallowing for radiotherapy treatment planning. Radiotherapy and oncology: journal of the European Society for Therapeutic Radiology and Oncology 101, 394–402, https://doi.org/10.1016/j.radonc.2011.05.015 (2011).
Roe, J. W. et al. Swallowing outcomes following Intensity Modulated Radiation Therapy (IMRT) for head & neck cancer - a systematic review. Oral oncology 46, 727–733, https://doi.org/10.1016/j.oraloncology.2010.07.012 (2010).
van der Laan, H. P., Christianen, M. E., Bijl, H. P., Schilstra, C. & Langendijk, J. A. The potential benefit of swallowing sparing intensity modulated radiotherapy to reduce swallowing dysfunction: an in silico planning comparative study. Radiotherapy and oncology: journal of the European Society for Therapeutic Radiology and Oncology 103, 76–81, https://doi.org/10.1016/j.radonc.2011.11.001 (2012).
Eisbruch, A. et al. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? International journal of radiation oncology, biology, physics 60, 1425–1439, https://doi.org/10.1016/j.ijrobp.2004.05.050 (2004).
Acknowledgements
This study was sponsored by the Young and Middle-aged Teachers’ Basic Ability Improvement Project of Guangxi (No.2018KY0134), the Youth Science Foundation of Guangxi Medical University (No.GXMUYSF201505), and Guangxi Science and Technology Program Project (GK AD17129017, GK AD17195042 and GK AD17129013). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Yong Zhang and Rensheng Wang designed this study. Yiru Wang and Tong Wu collected data and followed the patients. Chenhui Huang and Xiaobi Tang performed the data analyses. Li Jiang, Chenhui Huang and Yixiu Gan wrote the paper. Rensheng Wang and Yong Zhang inspected the manuscript critically and took part in the revision of manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, L., Huang, C., Gan, Y. et al. Radiation-induced late dysphagia after intensity-modulated radiotherapy in nasopharyngeal carcinoma patients: a dose-volume effect analysis. Sci Rep 8, 16396 (2018). https://doi.org/10.1038/s41598-018-34803-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-34803-y
Keywords
This article is cited by
-
Longitudinal functional outcomes and late effects of radiation following treatment of nasopharyngeal carcinoma: secondary analysis of a prospective cohort study
Journal of Otolaryngology - Head & Neck Surgery (2022)
-
Organs-at-risk dose constraints in head and neck intensity-modulated radiation therapy using a dataset from a multi-institutional clinical trial (JCOG1015A1)
Radiation Oncology (2022)
-
The Relationships Between Radiation Dosage and Long-term Swallowing Kinematics and Timing in Nasopharyngeal Carcinoma Survivors
Dysphagia (2022)
-
Proton pencil-beam scanning radiotherapy in the treatment of nasopharyngeal cancer: dosimetric parameters and 2-year results
European Archives of Oto-Rhino-Laryngology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.