Abstract
Renal denervation (RDN) is one of the most frequently used invasive methods for the treatment of arterial hypertension. However, recent randomized sham-controlled studies raised concern about the efficacy and predictability of response. We retrospectively analyzed outcomes of patients, who underwent RDN in our hypertension center between November 2010 and April 2014 and report here outcomes twelve months after procedure based on 24-hours ambulatory blood pressure monitoring. We defined ten-mm Hg decrease in office systolic blood pressure (SBP) as a cut-off for response and looked for possible predictors of this response using binary multiple regression analysis. 42 patients were included. Their mean age was 59.6 ± 9.2 years and 24% were female. Baseline office SBP and diastolic blood pressure (DBP) were 164.1 ± 20.3 and 91.8 ± 12.4 mm Hg respectively. Mean 24 h-SBP significantly decreased from 149.8 ± 13.3 mm Hg to 141.2 ± 14.6 mm Hg. Mean 24 h-DBP significantly decreased from 83.3 ± 11.7 mm Hg to 78.8 ± 11.2 mm Hg. A higher level of mean 24 h-DBP and office DBP was shown to be predictive for response in office BP and a higher level of mean 24 h-DBP for response in 24 h-SBP and 24 h-DBP. Further properly designed randomized trials are warranted to confirm this finding as well as further investigate the role of diabetes mellitus and arterial stiffness in RDN.
Similar content being viewed by others
Introduction
Arterial hypertension has a major disease burden. Percutaneous renal denervation (RDN) has been shown to effectively reduce blood pressure (BP) in different previous trials1,2,3. However, reported responses vary from large falls in BP to unchanged or small increase in BP even within a given study population4. This suggests, that specific patient characteristics may predict the response to RDN. Establishing such predictors is very important for clinicians since significant fall in BP after RDN could cause more morbidity due to hypotension, whereas poor response would not be expected to reduce cardiovascular events, which is the primary purpose of BP reduction. The randomized and sham-controlled SIMPLICITY-HTN 3 trial could not show any benefit of RDN compared to sham-group with optimal medical treatment5 and raised doubt about the effectiveness of RDN, though reliable data support the “proof of concept” of RDN6,7. Recently published sham-controlled Spyral HTN ON-MED and OFF-MED studies demonstrated clinically relevant fall in 24-hours ambulatory systolic BP (SBP) with 7.4 mm Hg after six months in the ON-MED trial and 5.5 mm Hg after three months in the OFF-MED trial8,9. In the sham-controlled, prospective, double-blind Radiance-HTN solo trial, where an intravascular applied ultrasound was used for renal artery nerve ablation, 24-h-SBP reduction of 5 mm Hg was observed10. Both studies showed a clear tendency for the effectiveness of the RDN procedure. However, the magnitude of response was unpredictable with some over-responder and only about 70–80% presenting with any BP reduction after RDN.
In the light of current data, identification of the predictors for response to RDN seems to be crucial in order to select the patients appropriately. The response should be evaluated according to change in mean 24 h-SBP and diastolic BP (DBP) obtained with ambulatory blood pressure monitoring (ABPM), due to known shortcomings of office BP11. Based on ABPM readings, more data are needed from a “real-world setting” dealing with reliable predictors of the response to RDN. In this retrospective analysis, we sought to identify such baseline parameters in a cohort of patients with refractory hypertension, who underwent RDN in our centre. We considered changes in 24 h-BP measured with ABPM in order to avoid shortcomings related to office BP-based assessment of treatment effect.
Results
In total, 81 patients underwent RDN in our nephrology and hypertensiology department at Charité University Berlin, Campus Benjamin Franklin between November 2010 and April 2014. Complete demographic, clinical and procedure-related data and follow-up data including the course of BP values assessed with ambulatory blood pressure monitoring over 24 hours (24 h-ABPM) was available for 42 subjects, who were included in our retrospective analysis. According to the chosen response definition, twenty-one patients showed BP-response after RDN. Mean patient age, BMI, kidney function, amount of albuminuria, office SBP and DBP, heart rate and the number of antihypertensive medications at baseline and after twelve months did not differ significantly in both groups. In the responder group, the mean 24 h-SBP and -DBP at baseline were significantly higher compared to the non-responder group. In the non-responder group the number of patients with diabetes was significantly higher than in the responder group. Details of demographics and clinical data of the whole collective, responder and non-responder group are presented in Table 1.
During RDN 9.9 ± 3.6 ablations were performed. As shown in Table 2 there was no statistically significant difference in procedure-related parameters such as the diameter of renal arteries, the distance between the origin of the renal artery and the last ablation point, the number of ablation points, or the anatomy of renal arteries.
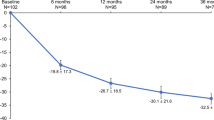
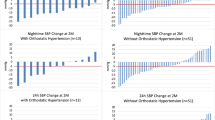
We observed a significant decline in mean 24 h-SBP and 24 h-DBP in the whole group and the responder group twelve months after RDN. Non-responder did not show any significant change in 24 h-SBP and 24 h-DBP. Details for whole group, responder and non-responder are shown in Table 3. Individual changes in 24-h mean SBP and DBP from baseline to twelve months are presented in Fig. 1. 24 h-SBP and -DBP mean changes at two days, one month, three months, six months, nine months and twelve months after RDN are shown in Fig. 2.
In the univariate analysis significantly different parameters between responder and non-responder group (see Table 1) and age, sex, BMI, baseline office SBP and DBP, eGFR, heart rate, and ISH were inputted in a binary logistic regression. For prediction of response to RDN the odds ratio of baseline office DBP and 24 h-ABPM DBP was 1.2 [95% CI 1.0 to 1.5; p = 0.045] and 1.5 [95% CI 1.1 to 1.9; p = 0.007] respectively; the odds ratio of baseline 24 h-ABPM SBP and diabetes mellitus were 1.01 [95% CI 0.9 to 1.1, non-significant] and 2.9 [95% CI 0.3 to 26.2, non-significant] (Fig. 3). We also performed multiple linear regression analysis for change in mean 24 h-SBP and 24 h-DBP including the same independent variables as in the analysis of predictive effect based on defined response cut-off (>10 mm Hg change in office SBP). In this analysis, baseline mean 24 h-DBP predicted significantly decrease in mean 24 h-SBP (p = 0.003) and mean 24 h-DBP (p = 0.001) after RDN.
Impact of diabetes mellitus, baseline 24 h mean systolic blood pressure (SBP) and baseline 24 h mean diastolic blood pressure (DBP) on the response to renal denervation assessed with binary logistic regression analysis. X-axis represents odds ratio with logarithmic (log10) scale; *statistically significant with p = 0.007; #statistically significant with p = 0.045. Variables entered in multivariate analysis: baseline office SBP and DBP, baseline mean 24 h-SBP and mean 24 h-DBP, diabetes, isolated systolic hypertension, baseline heart rate, age, sex, body-mass-index, estimated glomerular filtration rate.
The particular analysis of diabetic patients showed significantly higher baseline mean 24 h-SBP (154.3 ± 13.7 vs. 145 ± 11.5 mm Hg, p = 0.001) and mean 24 h-DBP (88.9 ± 10.0 vs. 77.6 ± 10.6 mm Hg, p = 00.1) compared to non-diabetics. Both mean 24 h-SBP and 24 h-DBP did not change significantly twelve months after RDN in diabetic patients (Fig. 4). Prevalence of isolated systolic hypertension was 33% in non-diabetics and 67% in diabetic patients (p = 0.06).
Discussion
In this study, we performed a retrospective analysis regarding the BP-lowering effect of RDN-procedure in our center. We saw a clinically relevant reduction in 24 h mean SBP (8.6 mm Hg) and mean DBP (4.5 mm Hg). Observed amount of BP-reduction is comparable with the findings of recent randomized sham-controlled trials, which were explicitly designed to eradicate known limitations of RDN trials8,9,10. In addition to the inclusion of the sham procedure and assessment of BP-lowering effect based on results of ABPM, investigators also performed RDN in subjects without any antihypertensive medication (OFF MED approach) to assess the real effect of RDN on BP. Furthermore, in the case of electrical RDN, the ablation procedure was performed with the latest generation multielectrode catheter and generator8,9. Acknowledging the sophisticated trial design and improvements in ablation techniques, our patients had similar BP response after RDN compared to patients from above mentioned modern RDN-trials. This circumstance underlines the reliability of our data. Worth mentioning, baseline 24 h-DBP in SPYRAL HTN-ON and -OFF MED trials was substantially higher than in our analysis.
We choose to dichotomize the BP-response after RDN and set the cut-off by ≥10 mm Hg fall in office SBP as already done in previous studies12,13. We observed a statistically significant independent impact of baseline office DBP and mean 24 h-DBP on response to RDN using multiple binary regression analysis. Significant predictive effect of mean baseline 24-h DBP also remained, when the BP-lowering effect was assessed as a continuous variable using multiple linear regression analysis.
Virtually all previously published RDN studies identified baseline BP as the major primary determinant of BP response after RDN: Symplicity HTN-1 Investigators reported the issue for office BP response already in the initially published results14. Randomized sham-controlled SIMPLICITY HTN 3 trial confirmed these findings. Various registry analyses including experiences from different countries also found baseline BP as a major predictor of BP-lowering effect after RDN and confirmed data coming from proof-of-concept studies and randomized trials by the evidence from real-life setting15,16,17,18,19,20,21. Noteworthy, baseline SBP predicted lowering effect in SBP and baseline DBP predicted lowering effect in DBP in all previously mentioned studies. In contrast, we observed baseline office DBP and 24 h-DBP being predictors for the fall in SBP (office and 24 h-ABPM). To our knowledge, this finding has not been reported yet and thus extends available evidence. A possible biological explanation could be that higher DBP might reflect arterial vessels without severe and irreversible wall damage. Profound arteriosclerosis leads to increased arterial stiffness, higher pulse wave velocity (PWV), lower DBP and increased prevalence of isolated systolic hypertension (ISH)22. In this case, sympathetic overdrive is probably not a dominant driving mechanism of refractory arterial hypertension and thus associated with impaired response to RDN. Growing evidence supports this hypothesis that patients with advanced arterial stiffness and thus severe arterial wall damage as indicated by increased PWV23, aortic calcifications24 or ISH16,25 showed attenuated BP response after RDN.
One of the major causes of arteriosclerosis is diabetes mellitus. However, the impact of diabetes mellitus on BP response failed the statistical significance in multiple regression analysis, though it has shown a statistically significant negative impact on the BP response after RDN in univariate analysis among our patients. Further analysis of the subgroups with and without diabetes mellitus revealed that the former had significantly higher mean baseline SBP and DBP in ABPM, which could attenuate the effect of diabetes mellitus in the statistical analysis. Furthermore, patients with diabetes had also numerically more ISH compared to the group without diabetes. Lower baseline DBP and higher prevalence of ISH in non-responders and diabetic patients could be an expression of increased arterial stiffness and thus poorer response to RDN in our collective.
One of the strengths of our analysis is that the response to RDN was assessed with office BP measurements and ABPM, though patients were classified as responder or non-responder according to the amount of office SBP change. However, grouping in responder and non-responder according to office BP response reflected the response of 24-h ambulatory SBP and DBP in our analysis very well. As already shown, office BP might have some potential confounding characteristics such as “regression to the mean” phenomenon and white coat hypertension, which significantly influence the amount of BP change over time8. These phenomena could be in part eliminated by ABPM11.
We acknowledge several limitations of our analysis. Our findings were obtained from a single centre and analysed in a retrospective fashion. Thus, looking for potential predictors of response to RDN our findings reflect associations and can only generate a possible hypothesis, which should then be tested in appropriately designed prospective studies. Relatively small number of the included patients and open non-blinded design of the analysis might not be able to cover the abundance of confounding factors in RDN as we have learned from previous studies. Keeping the potentially higher risk of confounding in mind, our results show a similar response to RDN compared to recent second-generation sham-controlled randomized studies8,9,10.
Testing patient compliance was not a part of clinical routine during the follow up after the RDN in our collective. Thus, confounding of the BP-lowering effect of RDN by varying medication intake cannot be ruled out. It is a common problem of all RDN studies or analyses, which included patients on antihypertensive medications without compliance testing as an inclusion criterion or as a part of follow up. We cannot distinguish the true resistant hypertensive patients from the patients who are incompliant to their antihypertensive drugs. Among the non-responders in our study collective, the BP increased over time. A possible explanation of this finding could be the higher amount of incompliant patients, who took their medication in preparation to RDN and shortly after and then reduced or stopped it.
The cut-off margin for responder was defined for office BP based on previous studies18. Study findings could thus not be generally translated to response in ABPM and other cut-offs for a definition of responder vs. non-responder to RDN. Hence, we additionally looked for response predictors for change in mean 24 h-SBP and mean 24 h-DBP in ABPM and could demonstrate that higher baseline 24-DBP, but not baseline office DBP, significantly predicted a higher decrease of mean 24 h-SBP and 24 h-DBP 12 months after RDN. In our analysis, we showed the trend for diabetes mellitus to be a predictor for negative RDN response, which failed to remain statistically significant in the multiple logistic regression. This could be due to a relatively small study collective and further prospective studies directly approaching this issue with more patients are needed.
Recently released new guidelines on the management of hypertension by European Society of Hypertension and European Society of Cardiology do not recommend to use RDN in the clinical routine as hypertension treatment method anymore. One of the concerns leading to this recommendation was insufficient data about the suitable subpopulation of hypertensive patients and lack of predictors for RDN response26.
The primary conclusion and clinical implication from our study are that DBP, measured in office and with ABPM, seems to be a predictor of response to RDN. Given that lower DBP could be a reflection of increased arterial stiffness and more advanced arterial wall damage, our data add to the available evidence pointing to impaired response to RDN in patients with increased arterial stiffness. Further properly designed randomized trials are warranted to confirm this finding as well as further investigate the role of diabetes mellitus and arterial stiffness in RDN.
Methods
This retrospective analysis was performed according to the Declaration of Helsinki and written informed consent was obtained from all patients included. The local ethics committee (ethics committee of Charité Medical University Berlin, Germany) approved the study. There is no restriction on the availability of additional materials or information, which can be any time obtained by sending a query to the corresponding author via email.
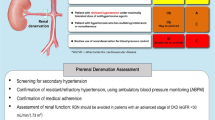
Patients were considered to have resistant hypertension, when the mean of three measurements of office systolic blood pressure was >140 mm Hg and/or of office DBP >90 mm Hg respectively and the mean SBP >130 mm Hg and mean DBP >80 mm Hg with 24 hours ambulatory blood pressure monitoring. 81 patients with resistant hypertension underwent RDN between November 2010 and April 2014. All of them were treated with at least three antihypertensive drugs including a diuretic at maximally tolerated dosages before performing the RDN. Common secondary causes of hypertension such as sleep apnea syndrome, hemodynamic significant renal artery stenosis, hyperaldosteronism, hypercortisolism, abnormality of thyroid function and pheochromocytoma were excluded prior to RDN.
Further exclusion criteria were pregnancy, age below 18 years, implanted peacemaker or intracardiac defibrillators, severe cardiac valve abnormalities and renal artery diameter <4 mm or length of renal artery <20 mm. Renal artery anatomy was checked before intervention by either CT-angiography or MR-angiography.
For RDN, the Symplicity RDN Catheter System (Medtronic Inc., Minneapolis, Minnesota, USA) was used via the right femoral approach. RDN procedure was performed in both renal arteries during the same session with a minimum of five ablation points in each renal artery. The RDN procedure was performed under general anesthesia. We defined the bilateral presence of single renal artery without any anatomical abnormalities as “standard anatomy”; any other case was defined as “non-standard” anatomy.
Routine clinical follow-up visits were performed after two days, one month, three months, six months, nine months, and twelve months. During each visit routine blood tests including assessment of kidney function and albuminuria were taken, information about current medication was collected and office blood pressure measurement, as well as ABPM were performed. ABPM was performed using Spacelabs 90207-2 device (Spacelab Healthcare, Snoqualmie, WA 98065 US). The interval between 0600 to 2200 was defined as daytime (readings every 20 minutes) and the interval between 2200 and 0600 was defined as night-time (readings every 30 minutes). The cuff was placed on the non-dominant upper arm and patients were instructed to keep their arm calm during the measurement. 42 patients with complete data for ABPM readings at baseline and after 12 months were included in this retrospective analysis.
Whenever a reduction in office SBP achieved ≥10 mm Hg after twelve months compared to baseline, the patient was considered to be a responder to RDN.
Isolated systolic hypertension was defined as the presence of SBP >140 mm Hg with simultaneously DBP ≤90 mm Hg detected with office measurements or with ABPM.
Statistical Analysis
Continuous variables are expressed as mean with standard deviation. Presence of normal distribution was assessed with the Kolmogorov Smirnov test. In case of normal distribution, we used the t-test for comparison. In case of non-normal distribution, we used the Mann-Whitney-U test for comparison.
Discrete parameters are expressed as the number of patients and percentages. The differences were compared using χ2-test.
A multiple binary logistic regression analysis with stepwise forward inclusion model was applied to determine the predictors of RDN response after twelve months.
The level of significance used for all tests was a two-sided p-value of 0.05.
Change history
22 August 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper
References
Symplicity, H. T. N. I. et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 376, 1903–1909, https://doi.org/10.1016/S0140-6736(10)62039-9 (2010).
Lambert, T. et al. Individual-patient visit-by-visit office and ambulatory blood pressure measurements over 24 months in patients undergoing renal denervation for hypertension. Int J Cardiol 181, 96–101, https://doi.org/10.1016/j.ijcard.2014.12.001 (2015).
Rosa, J. et al. Role of Adding Spironolactone and Renal Denervation in True Resistant Hypertension: One-Year Outcomes of Randomized PRAGUE-15 Study. Hypertension 67, 397–403, https://doi.org/10.1161/HYPERTENSIONAHA.115.06526 (2016).
Fink, G. D. & Phelps, J. T. Can we predict the blood pressure response to renal denervation? Auton Neurosci 204, 112–118, https://doi.org/10.1016/j.autneu.2016.07.011 (2017).
Bhatt, D. L. et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 370, 1393–1401, https://doi.org/10.1056/NEJMoa1402670 (2014).
Krum, H. et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 373, 1275–1281, https://doi.org/10.1016/S0140-6736(09)60566-3 (2009).
Hoobler, S. W. et al. The effects of splanchnicectomy on the blood pressure in hypertension; a controlled study. Circulation 4, 173–183 (1951).
Kandzari, D. E. et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet, https://doi.org/10.1016/S0140-6736(18)30951-6 (2018).
Townsend, R. R. et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet 390, 2160–2170, https://doi.org/10.1016/S0140-6736(17)32281-X (2017).
Azizi, M. et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet, https://doi.org/10.1016/S0140-6736(18)31082-1 (2018).
Howard, J. P., Nowbar, A. N. & Francis, D. P. Size of blood pressure reduction from renal denervation: insights from meta-analysis of antihypertensive drug trials of 4,121 patients with focus on trial design: the CONVERGE report. Heart 99, 1579–1587, https://doi.org/10.1136/heartjnl-2013-304238 (2013).
Ott, C. et al. Renal denervation in moderate treatment-resistant hypertension. J Am Coll Cardiol 62, 1880–1886, https://doi.org/10.1016/j.jacc.2013.06.023 (2013).
Esler, M. D. et al. Renal sympathetic denervation for treatment of drug-resistant hypertension: one-year results from the Symplicity HTN-2 randomized, controlled trial. Circulation 126, 2976–2982, https://doi.org/10.1161/CIRCULATIONAHA.112.130880 (2012).
Symplicity, H. T. N. I. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 57, 911–917, https://doi.org/10.1161/HYPERTENSIONAHA.110.163014 (2011).
Vogel, B. et al. Renal sympathetic denervation therapy in the real world: results from the Heidelberg registry. Clin Res Cardiol 103, 117–124, https://doi.org/10.1007/s00392-013-0627-5 (2014).
Ewen, S. et al. Reduced effect of percutaneous renal denervation on blood pressure in patients with isolated systolic hypertension. Hypertension 65, 193–199, https://doi.org/10.1161/HYPERTENSIONAHA.114.04336 (2015).
Id, D. et al. Predictors of blood pressure response: Obesity is associated with a less pronounced treatment response after renal denervation. Catheter Cardiovasc Interv 87, E30–38, https://doi.org/10.1002/ccd.26068 (2016).
Rohla, M. et al. Predictors of response to renal denervation for resistant arterial hypertension: a single center experience. J Hypertens 34, 123–129, https://doi.org/10.1097/HJH.0000000000000764 (2016).
Persu, A. et al. Hyperresponders vs. nonresponder patients after renal denervation: do they differ? J Hypertens 32, 2422–2427; discussion 2427, https://doi.org/10.1097/HJH.0000000000000347 (2014).
Volz, S. et al. Renal sympathetic denervation in Sweden: a report from the Swedish registry for renal denervation. J Hypertens 36, 151–158, https://doi.org/10.1097/HJH.0000000000001517 (2018).
Tsioufis, C. et al. Blood pressure response to catheter-based renal sympathetic denervation in severe resistant hypertension: data from the Greek Renal Denervation Registry. Clin Res Cardiol 106, 322–330, https://doi.org/10.1007/s00392-016-1056-z (2017).
Tolle, M., Reshetnik, A., Schuchardt, M., Hohne, M. & van der Giet, M. Arteriosclerosis and vascular calcification: causes, clinical assessment and therapy. Eur J Clin Invest 45, 976–985, https://doi.org/10.1111/eci.12493 (2015).
Fengler, K. et al. Predictors for profound blood pressure response in patients undergoing renal sympathetic denervation. J Hypertens 36, 1578–1584, https://doi.org/10.1097/HJH.0000000000001739 (2018).
Courand, P. Y. et al. Abdominal Aortic Calcifications Influences the Systemic and Renal Hemodynamic Response to Renal Denervation in the DENERHTN (Renal Denervation for Hypertension) Trial. J Am Heart Assoc 6, https://doi.org/10.1161/JAHA.117.007062 (2017).
Mahfoud, F. et al. Reduced blood pressure-lowering effect of catheter-based renal denervation in patients with isolated systolic hypertension: data from SYMPLICITY HTN-3 and the Global SYMPLICITY Registry. Eur Heart J 38, 93–100, https://doi.org/10.1093/eurheartj/ehw325 (2017).
Williams, B., Mancia G. ESC-ESH Guidelines for the Management of Arterial Hypertension. Eur Heart J, in press (2018).
Author information
Authors and Affiliations
Contributions
Dr. Alexander Reshetnik: conception of study design, analysis and interpretation of data, drafting the article. Dr. Christopher Gohlisch: writing the article; acquisition of data. Dr. Christian Scheurig-Münkler: acquisition of data; interpretation of data, providing intellectual content of critical importance to the work described; final approval of the version to be published. Dr. Maximilian De Bucourt: interpretation of data; providing intellectual content of critical importance to the work described; final approval of the version to be published. Prof. Dr. Walter Zidek: providing intellectual content of critical importance to the work described; final approval of the version to be published. Dr. Markus Tölle: providing intellectual content of critical importance to the work described; final approval of the version to be published. Prof. Dr. Markus van der Giet: conception of study design, interpretation of data; revising the article.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reshetnik, A., Gohlisch, C., Scheurig-Münkler, C. et al. Predictors for success in renal denervation–a single centre retrospective analysis. Sci Rep 8, 15505 (2018). https://doi.org/10.1038/s41598-018-33783-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33783-3
Keywords
This article is cited by
-
The position of renal denervation in treatment of hypertension: an expert consensus statement
Netherlands Heart Journal (2023)
-
Haben interventionelle Hochdruckverfahren eine Zukunft?
CardioVasc (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.