Abstract
There are no data on the effects of fingolimod, an immunomodulatory drug used in treatment of multiple sclerosis (MS), on circulating tight-junction (TJ) protein levels as well as on peripheral blood mononuclear cells (PBMC) migration. Serum TJ protein [occludin (OCLN), claudin-5 (CLN-5) and zonula occludens-1 (ZO-1)] levels, sphingosine-1 phosphate 1 (S1P1) receptor expression on circulating leukocyte populations as well as in vitro PBMC migration were longitudinally assessed in 20 MS patients under 12-months fingolimod treatment and correlated with clinical and magnetic resonance imaging (MRI) parameters. After 12 months of treatment, a significant reduction of mean relapse rate as well as number of active lesions at MRI was found. TJ protein levels significantly decreased and were associated with reduction of S1P1 expression as well as of PBMC in vitro migratory activity. A significant correlation of CLN-5/OCLN ratio with new T2 MRI lesions and a significant inverse correlation of CLN-5/ZO-1 ratio with disability scores were found. These findings support possible in vivo effects of fingolimod on the blood-brain barrier (BBB) functional activity as well as on peripheral cell trafficking that could result in avoiding passage of circulating autoreactive cells into brain parenchyma. Circulating TJ protein levels and respective ratios could be further studied as a novel candidate biomarker of BBB functional status to be monitored in course of fingolimod as well as of other immunomodulatory treatments in MS.
Similar content being viewed by others
Introduction
In multiple sclerosis (MS), the expansion of activated and autoreactive lymphocyte clones adhering to blood-brain barrier (BBB) endothelium and subsequently migrating into the brain parenchyma is thought to be a fundamental step of cascade of events leading to inflammatory damage to myelin and axons1. Interendothelial tight junction (TJ) proteins such as occludin (OCLN), claudin-5 (CLN-5) as well as zonula occludens-1 (ZO-1), contribute to maintenance of the blood-brain barrier (BBB) anatomical and functional integrity2 and are subjected to shedding and release becoming detectable in biological fluids such as serum and thus representing a possible in vivo marker of BBB functional integrity as recently found in ischemic stroke3. Fingolimod (FTY720) phosphate, approved for treatment of highly active relapsing-remitting (RR) MS, acts as a functional antagonist of the sphingosine 1-phosphate (S1P) receptor subtypes and its binding to S1P1, mainly expressed on the lymphocyte surface, results in inhibition of lymphocyte leakage from lymph nodes thus determining a reversible redistribution of pathogenic lymphocytes as well as reducing their recirculation into the central nervous system (CNS)4. Moreover, in rat experimental autoimmune encephalomyelitis (EAE), experimental evidence of additional effects of FTY720 on BBB repair through reduction of adhesion molecule expression as well as downregulation of other endothelial barrier gene transcripts (ICAM-1, MMP-9, P-selectin, TIMP-1, VCAM-1) has been achieved5. Furthermore, pretreatment of immortalized human brain endothelial cultures with FTY720 prevented BBB alterations induced by MS sera6. Conversely, targeting endothelial S1P1 with FTY720 in a mouse model caused changes in subcellular location of TJ proteins and led to transient BBB opening7. However, to date, there is lack of data on the possible effects of FTY720 on serum TJ protein levels in MS patients as potential in vivo surrogate marker of BBB repair as well as on peripheral blood mononuclear cells (PBMC) migration. To address these issues, we longitudinally evaluated TJ protein levels in serum of MS patients under FTY720 treatment, measured the S1P1 receptor expression on circulating leukocyte and lymphocyte populations as well as assessed in vitro PBMC migration. We also correlated these findings with clinical and magnetic resonance imaging (MRI) parameters.
Results
Clinical and MRI features
Clinical and demographic characteristics of the patients and normal healthy subjects (NHS) as well as previous disease modifying therapies (DMT) are summarized in Table 1. After 12-months treatment, mean relapse rate (RR) of the patient cohort in the last year prior to treatment significantly decreased by 96% (p < 0.0001). Out of 20 patients, one had a clinical relapse at 9 months of therapy. There was a slight but not significant reduction of disability score by 11% (p = 0.17) (Table 2). No evidence of disease activity (NEDA) at12 months of treatment, as defined in methods, was observed in 13 of 20 (65%) patients. At the end of follow-up, there was a not significant reduction by 53% of mean new T2 weighted lesions (p = 0.34) at MRI. Conversely, a significant reduction by 80% of T1 gadolinium enhancing (GAD+) lesions was observed (p = 0.001) (Table 2).
Serum TJ proteins levels
All three proteins levels were found to be significantly reduced at 6 months as well as after 12-months treatment. This reduction was substantially similar for all three proteins. In particular, serum OCLN decreased by 47.4% and 70,5% after 6 and 12 months of therapy, respectively (p < 0.0001) (Fig. 1A). Serum CLN-5 significantly decreased by 54.8% and 73.6%, respectively (p < 0.0001) (Fig. 1B) and ZO-1 by 53.5% and 74.5%, respectively (p < 0.0001) (Fig. 1C). However, for all three proteins, the levels at 12 months treatment were significantly higher than those of NHS. There was no significant correlation between single TJ protein levels and clinical parameters such as relapse rate and disability score assessed by EDSS at baseline as well as at 12 months. No significant correlation between single TJ protein levels and neuroimaging parameters at MRI such as new T2 weighted lesions and T1 GAD+ lesions was observed. (Supplementary Table S1). However, when calculating CLN-5/OCLN and CLN-5/ZO-1 ratios, we found a significant correlation of CLN-5/OCLN ratio at baseline with the number of new T2 weighted MRI lesions both at baseline (r = 0.56; p = 0.0095) (Fig. 2A) and at 12- months treatment (r = 0.50; p = 0.023) (Fig. 2B). Conversely, there was a high statistical trend towards a negative correlation (r = −0.40; p = 0.056) and a significant inverse correlation (r = −0.46; p = 0.037), of CLN-5/ZO-1 ratio at baseline with EDSS at baseline and at 12- months treatment, respectively (Fig. 2C,D).
Serum tight junction protein levels in multiple sclerosis (MS) patients (n = 20) during treatment with fingolimod and in normal healthy subjects (NHS) (n = 25): occludin (OCLN) (A), claudin-5 (CLN-5) (B), zonula occludens (ZO-1) (C). T0 = baseline time prior to treatment; T6 = at 6 months of treatment; T12 = at 12 months of treatment. The results are shown as scatter plots with mean ± SD. ANOVA and Tukey post test were used.
Correlations of serum tight junction protein ratios with clinical and MRI parameters. Correlation of CLN-5/OCLN ratio with new T2 weighted lesions at MRI at T0 (A) and at T12 (B). Correlation of CLN-5/ZO-1 ratio with EDSS at T0 (C) and at T12 (D). T0 = baseline time prior to treatment; T12 = at 12 months of treatment. CLN-5 = claudin-5; OCLN = occludin; ZO-1 = zonula occludens-1. EDSS = expanded disability status scale. Spearman correlation coefficient was calculated.
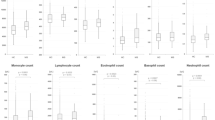
Expression of S1P1 in PBMC
Representative flow cytometry analysis of S1P1 receptor in leukocyte populations from MS and NHS is shown in Fig. 3. In MS patients, a significantly reduced expression of S1P1 by 30% and 61% was observed in CD4+ cells at 6 and 12 months, respectively (p = 0.0001) (Fig. 4A). A similar extent of reduction by 24% and 52% was observed in CD8+ cells (p = 0.0001) (Fig. 4B). In both subpopulations, S1P1 expression extent after 12 months of therapy, reached that of NHS. In CD19+ cells, the reduction was 11% and 28%, respectively (p = 0.019) (Fig. 4C) whilst in CD14+ cells, the S1P1 expression was unchanged at 6 months but significantly decreased by 29% at 12 months (p = 0.0001) (Fig. 4D). However, in both CD19+ and CD14+ cells, treatment reduced the receptor expression to values similar to those of NHS.
Representative flow cytometry analysis of S1P1 receptor in CD4+, CD8+, CD19+ and CD14+ cells at baseline (T0) and at 12 months of treatment (T12) from one MS patient (A,B) and from one normal healthy subject (NHS) (C). Grey dot line: isotype control; black line: specific anti-cell marker monoclonal antibody.
Expression of sphingosine-1 phosphate1 receptor (S1P1) in CD4+ (A), CD8+ (B), CD19+ (C) and CD14+ cells (D) from multiple sclerosis (MS) patients (n = 20) during treatment with fingolimod and from normal healthy subjects (NHS) (n = 10). SFI = specific fluorescence index; T0 = baseline time prior to treatment; T6 = at 6 months of treatment; T12 = at 12 months of treatment. The results are shown as scatter plots with mean ± SD. ANOVA and Tukey post test were used.
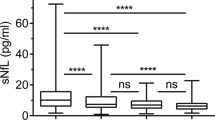
Chemotaxis assay
A very significant reduction of PBMC migration rate by 39.5% and 68% was observed at 6 and 12 months, respectively (p < 0.0001) (Fig. 5A). To test whether the effect on migration was specifically due to FTY720 therapy, we assayed PBMCs from NHS (n = 12) or MS patients (n = 20) at baseline after a 24-hour in vitro exposure to FTY720 and observed a migration rate similar to that of MS patients at 12 months therapy (Fig. 5B). There was no correlation between the extent of S1P1 expression in CD4+ (r = 0.03; p = 0.89) and CD8+ cells (r = −0.16; p = 0.48) and PBMC migration rate indicating no direct role of lymphocyte S1P1 expression on the peripheral cell migration.
In vitro migratory activity of peripheral blood mononuclear cells (PBMC) from multiple sclerosis (MS) patients (n = 20) during treatment with fingolimod and from normal healthy subjects (NHS) (n = 12) (A). In vitro migratory activity of PBMC from multiple sclerosis (MS) patients prior to start fingolimod treatment and from normal healthy subjects (NHS) prior to and after in vitro exposure to fingolimod (B). MI = migration index; T0 = baseline time prior to treatment; T6 = at 6 months of treatment; T12 = at 12 months of treatment; S1P = sphingosine 1-phosphate; MS T0 FTY720+ = PBMC from MS patients at baseline time exposed to fingolimod; NHS T0 FTY720+ = PBMC from NHS after in vitro exposure to fingolimod. S1P+ FTY720 = assays performed with S1P at bottom of the chemotaxis chamber in the presence of FTY720. The results are shown as scatter plots with mean ± SD.
Discussion
In this study, we demonstrated that treatment with fingolimod is associated with significant reduction of circulating TJ proteins levels contributing to the architecture of BBB. BBB changes constitute one of the pathological hallmarks in MS8 and are associated with TJ proteins alterations. In MS brains, changes in ZO-1 and OCLN were found in both active lesions and normal-appearing white matter (NAWM)9 and ZO-1 was also found altered in inactive chronic lesions10. These findings suggest that damage to TJ proteins concurs to cause subtle alterations of the BBB architecture even in areas where the inflammatory process should be exhausted as well as in areas far from active or chronic lesions such as NAWM supporting the concept that BBB function is profoundly compromised in MS and with difficulty normalizes11. Moreover, there is experimental evidence that serum from active MS patients reduces the expression of OCLN and VE-cadherin in endothelial cultures suggesting that circulating proinflammatory factors such as cytokines, metalloproteinases as well as reactive oxygen radicals contribute to TJ protein changes and subsequent endothelium alterations12. These pathological findings parallel the MS real clinical life where often GAD+ lesions at MRI, thought a surrogate marker of BBB alteration13, were also detected during clinical stability stages independently of occurrence of new clinical relapses14,15. Despite the lack of any correlation between single TJ protein levels and number of GAD+ lesions, we, however, detected the highest TJ protein levels at baseline, in patients showing at least one GAD+ lesion or experiencing a clinical relapse at a time close to blood collection and thus being in active disease, consisting with the association of TJ proteins alterations with BBB leakage. However, considering that the average duration of contrast enhancement at a MRI lesion was found to be around 3 weeks16 and the different time of blood collection respect to MRI in our cohort, we can’t rule out that TJ protein levels could be lower than those detected and thus may be underpowered to allow to reach significant values at the correlation analysis. Of interest is the significant correlation of CLN-5/OCLN ratio with new T2 weighted lesions at MRI suggesting a common pathway underlying the release of both TJ proteins into the peripheral blood and related to brain inflammatory lesion formation as indicated by detection of new T2 lesions. It has been demonstrated that, at the cerebral microvessels, CLN-5 and OCLN are assembled into oligomers contributing to selective inhibition of the paracellular transport as well as to endothelial cell polarity fundamental for maintaining BBB integrity17. Moreover, the significant inverse correlation between CLN-5 /ZO-1 ratio and EDSS suggests that increased release of ZO-1 reduces this ratio and is associated with the complex process underlying the disability accrual. This hypothesis is supported by ZO-1 location at the brain endothelial cell cytoplasm binding both to the occludin-CLN-5 complex and to cytoskeleton proteins18. It is likely that the cascade of events causing TJ protein release leads to disassembly of cytoskeleton proteins such as actin thus resulting in BBB breakdown associated with diffuse inflammation and nervous tissue damage and causing MS disability11,19.
In our study, the lowest TJ protein levels were detected after 12-months treatment showing a significant decrease of GAD+ lesions and thus supporting an in vivo effect of fingolimod on BBB functional activity and likely on repair of BBB damage due to neuroinflammation. However, these levels, although reduced, tended to be higher than NHS supporting the persistence of subtle BBB alterations in clinically stable MS patients, even though we can’t rule out that an extension of longitudinal measurement over 12-months treatment could show further level reduction.
Of interest are the findings on the S1P1 expression in different leukocyte populations never, to the best of our knowledge, investigated in MS patients. It is demonstrated that reduction of S1P1 receptor expression by fingolimod is due to its internalization20 and subsequent degradation21. In our study, the extent of expression reduction differed between lymphocyte subsets and B cells as well as monocytes, respectively, likely reflecting possible differences in the effects of fingolimod on circulating immunocompetent cells rather than fluctuations of single cell populations counts22. Indeed, several distinct modulatory effects on B cell subsets and related cytokine phenotype23 as well as on monocytes24 were recently found in MS patients under fingolimod treatment. Unique are the findings on PBMC migration suggesting that circulating PBMC not entrapped in lymph nodes by fingolimod, are subjected to changes in the complex pathway of adhesion molecules and cell surface receptors involved in cell adhesion to and passage across BBB endothelium. Experimental evidence of an effect of fingolimod on these molecules has been achieved in EAE where reduction and downregulation of a number of endothelial adhesion molecule transcripts has been shown5. In addition, a significant reduction in CXCL13 levels, a chemokine involved in leukocyte cell trafficking, has recently been found in cerebrospinal fluid from MS patients under treatment with fingolimod supporting a modulatory role of this drug in the cell migration25. Recently, any insights into the possible underlying mechanisms of fingolimod effects on BBB cell migration have been provided in an animal experimental model by Zhao et al. demonstrating that FTY720 blocks in vivo leukocyte recruitment into the brain parenchyma by inhibition of brain endothelium activation through reduction of phosphorylation of a number of signaling molecules such as serine/threonine-specific protein kinases, STAT6 and NFkB26. In our study, the demonstration of a direct effect of fingolimod on cell migration was provided by the finding that PBMC from NHS as well as MS patients prior to starting treatment, display a significant reduction of migratory activity up to the extent detected in MS patients at 12-months treatment, after in vitro exposure to this molecule. Although we were not able to find any correlation between S1P1 expression and extent of migration rate, the overlapping of migration index of fingolimod-treated cells with that of untreated cells, suggests however a link of this receptor subtype with migration pathway that remains to be elucidated. A possible limitation of these findings comes from the characteristics of the chemotaxis assay lacking in an endothelial cell monolayer more representative of the BBB architecture in vivo and thus not allowing to achieve direct data on BBB transmigration.
In conclusion, our study provides novel data on possible in vivo effects of fingolimod on BBB functional activity and repair during neuroinflammation and extends its effect on peripheral blood cell trafficking speculating on a possible reduction of migratory activity of circulating immunocompetent cells across BBB and likely avoiding passage of circulating autoreactive cells into brain parenchyma. Further studies are however needed to confirm this hypothesis. All biomarkers of BBB alteration in MS, investigated to date, resulted poorly sensitive when correlated with the number of GAD+ lesions27. It is therefore reasonable in searching for new BBB investigating tools, to take into account other quantitative MRI parameters than number of GAD+ lesions such as volume of gadolinium enhancement even though different patterns of in vivo BBB alteration should be considered in MS28. However, circulating TJ proteins levels and respective ratios could be further studied as a novel candidate biomarker of BBB functional status to be monitored in course of fingolimod as well as of other immunomodulatory treatments in MS patients.
Materials and Methods
Patients
This is an observational prospective study. Twenty RRMS patients (6 male and 14 female subjects)29 were recruited. Twenty-five sex- and age-matched NHS, blood donors at the Blood Transfusion Centre of the Siena University Medical School and giving informed consent, were included as control group. All patients signed informed consent and the study was conducted according to the Declaration of Helsinki and approved by the Ethics Committee of the Medical School of University of Siena. All patients started second-line therapy with FTY720 (0.5 mg/die) according to the criteria approved by Agenzia Italiana del Farmaco (AIFA) including the failure of a first-line therapy or occurrence of highly active MS as demonstrated by at least two clinical relapses in the last year with at least one GAD+ lesions or increase in number of T2 weighted lesions at MRI30. Number of relapses in the last year prior to enrollment in the study as well as sustained disability score by EDSS31 at the enrollment time and after 12 months of treatment were assessed. Relapses were defined as occurrence of new clinical neurological signs or symptoms not associated with fever. Brain MRI at 1.5 Tesla with and without gadolinium infusion was performed according to the standard procedures for clinical follow-up at baseline time and after 12 months of treatment and number of new T2 weighted and T1 GAD+ lesions was estimated. In addition, NEDA at 12 months defined as a composite consisting of absence of relapses, no sustained EDSS score progression, and no new or enlarging T2 or T1 GAD+ lesions at MRI was assessed.
Blood collection and PBMC separation
PBMC were isolated by standard density gradient centrifugation procedures on Ficoll-Hypaque from buffy coat preparations of NHS obtained on the same day by Transfusion Centre, as well as from MS patients. In MS subjects, blood sample was drawn at baseline time after a wash out of the first-line therapy ranging from three to four weeks and at 6 and 12 months of FTY720 therapy. In NHS, serum sample was obtained by Transfusion Centre on the same day as blood donation.
ELISA assay for the assessment of serum levels of claudin, occludin and zonula occludens
Serum TJ proteins (CLN-5, OCLN and ZO-1) were measured by sandwich ELISA using commercial monoclonal and polyclonal antibody pairs, as briefly described. After washing with 0.05 Tween-20 in PBS at pH 7.4 and incubating for 2 hours at room temperature with blocking buffer (3% BSA in PBS at pH 7.4) to block unspecific binding sites, microplates, pre-coated with mouse anti human OCLN monoclonal antibody (mAb) (clone E-5, Santa Cruz, Dallas, TX, USA) or anti human CLN-5 mAb (clone A-12, Santa Cruz) or anti-human ZO-1 mAb (clone 61357, Abcam, Cambridge, UK) (all 5 μg/ml in carbonate buffer pH 9.6) overnight at 4 °C, were overlaid with recombinant OCLN (Abnova, Taiwan), CLN-5 (Abnova) e ZO-1 (Genway Biotech, CA, USA) to generate a reference standard curve (ranging between 0,156 and 10 ng/ml) as well as with MS and NHS sera (1:400 in PBS pH 7,4 - 0,5% BSA) for 2 hours at room temperature (Supplementary Fig. S1). Serum dilution was chosen from an ELISA curve previously obtained from 4 human serum samples (Supplementary Fig. S2). After washing, microplates were incubated for 2 h at room temperature with either polyclonal goat anti-ZO-1 antibody (2.5 μg/ml, Santa Cruz) or rabbit anti-CLN-5 (2,5 μg/ml, Santa Cruz), or peroxidase (POD) conjugated mouse anti-OCLN mAb (clone: OC-3F10, 1 μg/ml, Zymed-Thermo Fisher Scientific,Whaltam, MA, USA). After washing, affinity- purified POD conjugated anti-goat and rabbit IgG (1:10000, all from Calbiochem - Novabiochem, San Diego, CA, USA.) were added in microplates exposed to anti-ZO-1 and anti-CLN-5 mAbs as a secondary antibody for 1 h at room temperature. After washing, 0.1% o-phenylendiamine in 0.05 M citrate buffer at pH 4.5–0.002% H2O2 was added for 10 min at room temperature in dark. The color reaction was stopped with 1 M H2SO4 and measured with a photometer at 490 nm wavelength. The assay specificity for each TJ protein was tested in a competitive ELISA with recombinant standard proteins and bovine serum albumin as other unrelated protein (Supplementary Fig, S3). Inter-assay coefficient variability (CV) was 2.39%, 3.50% and 3.40% for OCLN, CLN-5 and ZO-1, respectively. Intra-assay CV was 2.60%, 3.99% and 2.48% for OCLN, CLN-5 and ZO-1, respectively.
Expression of the S1P1 receptor in circulating immunocompetent cells by flow cytometry
The differential expression of S1P1 receptor was measured with flow cytometry in leukocyte populations (T cells, B cells and monocytes) by using mAbs capable of recognizing specific cell markers (CD4+, CD8+, CD19+ and CD14+, respectively) conjugated with different fluorochromes. In particular, 1 × 106 PBMC in PBS pH 7.4 from each patient or NHS, were labelled with allophycocyanin (APC) -anti-human CD4 (clone: OKT4, 0.6 μg/ml), peridinin-chlorophyll-protein-cyanine5.5 (PerCP-Cy5.5) anti-human CD8 (clone: RPA-T8, 2.5 μg/ml), APC-anti-human CD19 (clone: HIB19, 1.25 μg/ml) and PerCP-Cy5.5-anti-human CD14 (clone: 61D3, 5 μg/ml) mAbs, (all from Affymetrix, eBioscience). After incubation for 15′ at room temperature in dark, cells were then fixed with 1% paraformaldehyde in PBS pH 7,4 and after washing, permeabilized with 0,02% saponin-PBS-1% FCS and labelled with phycoerythrin (PE)- anti-human S1P1/EDG-1 mAb (clone: 218713, 10 µl, R&D Systems). As control isotypes, mouse IgG2bk PE-conjugated (clone:A-1, MyBiosource), mouse IgG1k- PerCP-Cy5.5 -conjugated (clone: p3.6.2.8.1) and mouse IgG2bk-APC-conjugated (clone: eBMG2b) (all from Affymetrics, eBioscience) were used. Cells were analyzed on a FACSCalibur flow cytometer using Cell Quest Pro software (BD Biosciences). The extent of expression was assessed as Specific Fluorescence Index (SFI) calculated as ratio of the mean fluorescence values obtained with the specific anti-S1P1 as well as anti-CD markers mAbs to the respective isotype control antibody32.
Chemotaxis assay
To test the effects of FTY720 binding to S1P1 on migration of circulating immunocompetent cells, a chemotaxis assay was performed. PBMC were labelled with sulfo-NHS-biotin (Pierce, Rockford, IL) (0.2 mg/ml) for 30 minutes at room temperature according to a previously established method33. Biotin-labelled cells (25 × 103) in original culture medium (DMEM-10% FCS) were seeded in the upper compartment of a commercial chemotaxis chamber with 3 μm pore size membranes (NeuroProbe, MD, USA). As chemotactic agent, 100 nM sphingosine 1-phosphate (S1P) (Sigma) alone or, in some assays, in the presence of 100 nM FTY720 (Sigma), was placed in lower chamber. For each sample, as negative control, S1P was omitted in lower chamber. After 3 h at 37 °C, streptavidin-POD conjugate (1:5000) for 1 h at room temperature was added in lower chamber and after washes with PBS pH 7,4 and addition of the substrate 0,1% o-phenylendiamine (OPD) in citrate buffer pH 4,5, the product reaction was read at ELISA photometer at 490 nm and the absorbance of biotin-labelled cells after passage in the bottom compartment was measured. In some assays, PBMC (25 × 103) from NHS or from MS patients at baseline were exposed with 100 nM FTY720 for 24 h and then placed in chemotaxis chamber for assay as above described. Chemotactic activity was assessed as migration index calculated according to the following formula34:
Statistical analysis
Multiple comparisons were performed with ANOVA and Tukey post test for parametric data. Comparisons between paired groups was performed with Wilcoxon matched-pairs signed rank test for non-parametric data. Normality of data was estimated with D’Agostino & Pearson normality test. Correlation analysis was performed with Spearman’s test and Pearson r coefficient for non-parametric and parametric data, respectively. P < 0.05 values were considered significant. All statistical tests were performed with GraphPad Prism (version 7.02), San Diego, CA, USA.
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
References
Compston, A. & Coles, A. Multiple sclerosis. Lancet 372, 1502–1517 (2008).
Forster, C. Tight junctions and the modulation of barrier function in disease. Histochem. Cell Biol. 130, 55–70 (2008).
Kazmierski, R. et al. Serum tight-junction proteins predict hemorrhagic transformation in ischemic stroke patients. Neurology 79, 1677–1685 (2012).
Ingwersen, J. et al. Fingolimod in multiple sclerosis: mechanisms of action and clinical efficacy. Clin. Immunol. 142, 15–24 (2012).
Foster, C. A. et al. FTY720 rescue therapy in the dark agouti rat model of experimental autoimmune encephalomyelitis: expression of central nervous system genes and reversal of blood-brain-barrier damage. Brain Pathol. 19, 254–266 (2009).
Nishihara, H. et al. Fingolimod Prevents Blood-Brain Barrier disruption induced by the sera from patients with Multiple Sclerosis. PLoS One 10(3), e0121488 (2015).
Yanagida, K. et al. Size-selective opening of the blood–brain barrier by targeting endothelial sphingosine 1–phosphate receptor 1. Pnas 114, 4531–4536 (2017).
Noseworthy, J. H. et al. Multiple sclerosis. N. Engl J. Med. 343, 938–952 (2000).
Plumb, J. et al. Abnormal endothelial tight junctions in active lesions and normal-appearing white matter in multiple sclerosis. Brain Pathol. 12, 154–169 (2002).
Kirk, J. et al. Tight junctional abnormality in multiple sclerosis white matter affects all calibres of vessel and is associated with blood–brain barrier leakage and active demyelination. J. Pathol. 201, 319–327 (2003).
Claudio, L., Raine, C. S. & Brosnan, C. F. Evidence of persistent blood–brain barrier abnormalities in chronic progressive multiple sclerosis. Acta Neuropathol. 90, 228–238 (1995).
Minagar, A. et al. Serum from patients with multiple sclerosis downregulates occludin and VE-cadherin expression in cultured endothelial cells. Mult. Scler. 9, 235–238 (2003).
Smith, M. E. et al. Clinical worsening in multiple sclerosis is associated with increased frequency and area of gadopentate-dimeglumine- enhancing magnetic resonance imaging lesions. Ann. Neurol. 33, 480–489 (1993).
Weibe, S. et al. Serial cranial and spinal cord magnetic resonance imaging in multiple sclerosis. Ann. Neurol. 32, 643–650 (1992).
Barkhof, F. et al. Relapsing-remitting multiple sclerosis: sequential enhancing MR imaging vs clinical findings in determining disease activity. A.J.R. Am. J. Roentgenol. 159, 1041–104 (1992).
Cotton, F. et al. MRI contrast uptake in new lesions in relapsing-remitting MS followed at weekly intervals. Neurology 60, 640–646 (2003).
McCaffrey, G. et al. Tight junctions contain oligomeric protein assembly critical for maintaining blood–brain barrier integrity in vivo. J. Neurochem. 103, 2540–2555 (2007).
Ballabh, P., Braun, A. & Nedergaard, M. The blood–brain barrier: an overview. Structure, regulation, and clinical implications. Neurobiol. Dis. 16, 1–13 (2004).
Lassmann, H., van Horssen, J. & Mahad, D. Progressive multiple sclerosis: pathology and pathogenesis. Nat. Rev. Neurol. 8, 647–656 (2012).
Pham, T. H., Okada, T., Matloubian, M., Lo, C. G. & Cyster, J. G. S1P1 receptor signaling overrides retention mediated by G alpha-coupled receptors to promote T cell egress. Immunity 28, 122–133 (2008).
Oo, M. L. et al. Immunosuppressive and anti-angiogenic sphingosine 1-phosphate receptor-1 agonists induce ubiquitinylation and proteasomal degradation of the receptor. J. Biol. Chem. 282, 9082–9089 (2007).
Henault, D. et al. Basis for fluctuations in lymphocyte counts in fingolimod-treated patients with multiple sclerosis. Neurology 81, 1768–1772 (2013).
Blumenfeld, S., Staun-Ram, E. & Miller, A. Fingolimod therapy modulates circulating B cell composition, increases B regulatory subsets and production of IL-10 and TGFb in patients withMultiple Sclerosis. J. Autoimm. 70, 40–51 (2016).
Thomas, K. et al. Fingolimod additionally acts as immunomodulator focused on the innate immune system beyond its prominent effects on lymphocyte recirculation. J. Neuroinflamm. 14, 41 (2017).
Novakova, L. et al. Cerebrospinal fluid biomarkers of inflammation and degeneration as measures of fingolimod efficacy in multiple sclerosis. Mult. Scler. J. 23, 62–71 (2017).
Zhao, Y. et al. Fingolimod targets cerebral endothelial activation to block leukocyte recruitment in the central nervous system. J. Leuk. Biol. 103, 107–118 (2018).
Waubant, E. Biomarkers indicative of blood-brain barrier disruption in multiple sclerosis. Dis. Markers 22, 235–244 (2006).
Hawkins, C. P., Mackenzie, F., Tofts, P., Du Boulay, E. P. & McDonald, W. I. Patterns of blood-brain barrier breakdown in inflammatory demyelination. Brain 114, 801–810 (1991).
McDonald, W. I. et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann. Neurol. 50, 121–127 (2001).
AIFA. Gilenya©. Riassunto delle caratteristiche del prodotto. http://farmaci.agenziafarmaco.gov.it/aifa/10/06/2016 (2016).
Kurtzke, J. F. Rating neurologic impairment in multiple sclerosis: an expanded disability scale (EDSS). Neurology 33, 1444–1452 (1983).
De Santi, L. et al. Higher expression of BDNF receptor gp145trkB is associated with lower apoptosis intensity in T cell lines in multiple sclerosis. J. Neurol. Sci. 277, 65–70 (2009).
Pearce-Pratt, R., Phillips, D. M. & Bourinbaiar, A. S. Simple colorimetric cell-cell adhesion assay using biotinylated lymphocytes. J. Immunol. Methods 140, 159–165 (1991).
Capitani, N. et al. S1P1 expression is controlled by the pro-oxidant activity of p66Shc and is impaired in B-CLL patients with unfavorable prognosis. Blood 120, 4391–4399 (2012).
Acknowledgements
This study has received financial support from Novartis s.p.a. The sponsor had no role in writing the manuscript nor in the decision of submitting to the journal.
Author information
Authors and Affiliations
Contributions
P.A. designed the study, recruited and monitored the patients, contributed to the analysis of data and drafted the manuscript. G.M. and S.S. monitored the patients and contributed to the analysis of data. C.C., M.T. and G.M. performed experiments and contributed to the analysis of data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
P.A. reports personal fees for speaking and participation in scientific boards from Novartis, Biogen and Almirall, outside the submitted work; C.C., G.M., M.T., G.M. and S.S. declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Annunziata, P., Cioni, C., Masi, G. et al. Fingolimod reduces circulating tight-junction protein levels and in vitro peripheral blood mononuclear cells migration in multiple sclerosis patients. Sci Rep 8, 15371 (2018). https://doi.org/10.1038/s41598-018-33672-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33672-9
Keywords
This article is cited by
-
Sphingosine 1-phosphate Receptor Modulator Therapy for Multiple Sclerosis: Differential Downstream Receptor Signalling and Clinical Profile Effects
Drugs (2021)
-
Early central vs. peripheral immunological and neurobiological effects of fingolimod—a longitudinal study
Journal of Molecular Medicine (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.