Abstract
KCNK2 is a 2 pore domain potassium channel involved in maintaining cellular membrane resting potentials. Although KCNK2 is regarded as a mechanosensitive ion channel, it can also be gated chemically. Previous research indicates that KCNK2 expression is particularly enriched in neuronal and cardiac tissues. In this respect, KCNK2 plays an important role in neuroprotection and has also been linked to cardiac arrhythmias. KCNK2 has subsequently become an attractive pharmacologic target for developing preventative/curative strategies for neuro/cardio pathophysiological conditions. Zebrafish represent an important in vivo model for rapidly analysing pharmacological compounds. We therefore sought to identify and characterise zebrafish kcnk2 to allow this model system to be incorporated into therapeutic research. Our data indicates that zebrafish possess two kcnk2 orthologs, kcnk2a and kcnk2b. Electrophysiological analysis of both zebrafish Kcnk2 orthologs shows that, like their human counterparts, they are activated by different physiological stimuli such as mechanical stretch, polyunsaturated fatty acids and intracellular acidification. Furthermore, both zebrafish Kcnk2 channels are inhibited by the human KCNK2 inhibitory peptide spadin. Taken together, our results demonstrate that both Kcnk2a and Kcnk2b share similar biophysiological and pharmacological properties to human KCNK2 and indicate that the zebrafish will be a useful model for developing KCNK2 targeting strategies.
Similar content being viewed by others
Introduction
The two pore domain (K2P) channels are the most recent addition to the large family of potassium channels. They consist of two pore-forming P loops and four transmembrane segments1. These channels can be found in several excitable and non-excitable cell types where they play a role in maintaining the membrane resting potential1,2. The K2P potassium channel family is made up of fifteen members, divided into separate subfamilies based on their expression pattern, function and electro/biophysical properties1,2. Members of the K2P family perform a diverse range of physiological roles and have been associated with a variety of pathologies. For example, a missense mutation in KCNK9 causes Birk Barel mental retardation syndrome3, while a dominant negative mutation in KCNK18 has been linked to familial migraine4. In mice, deletion of both KCNK3 and KCNK9 leads to primary hyperaldosteronism syndrome5, while variants in KCNK3 have been associated with this condition in humans6. In zebrafish, Kcnk1 has a role in the regulation of heart rate and atrial size7. Among the K2P family, KCNK2 has been the subject of extensive research1,2. KCNK2 channel activity is polymodally regulated and as such a range of endogenous physiological stimuli can modulate its activity. For example, both mechanical membrane stretch and decreased intracellular pH promote KCNK2 activity8,9. KCNK2 is also sensitive to volatile anaesthetics such as chloroform, halothane, isoflurane and desflurane as well as other gases and gaseous compounds such as xenon, cyclopropane and nitric oxide10. Furthermore, polyunsaturated fatty acids (PUFAs) such as arachidonic acid (AA), docosahexaenoic acid (DHA) and alpha-Linolenic acid (ALA) along with lysophospholipids (LPL) such as lysophosphatidylcholine (LPC) are all capable of activating KCNK29,11,12,13,14. GPCRs are also able to both positively and negatively modulating KCNK2 activity, a process reliant on the phosphorylation of critical serine residues by either PKA or PKC15,16,17,18. Pharmacologically, KCNK2 is insensitive to all of the classical potassium channel inhibitors such as TEA (tetraethylamonium) and 4-AP (4-aminopyridine), which block voltage gated potassium channels, and glibenclamide, apamine and charybdotoxine which inhibit ATP and calcium sensitive potassium channels19. However, this channel is sensitive to antidepressant selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine, and next generation antidepressants such as the small peptide spadin, all of which effectively inhibit its activity9,15,16,17,20,21,22,23,24. Lastly, riluzole, a neuroprotective molecule, can both activate and inhibit KCNK29,25. Activation is accomplished by a direct interaction between KCNK2 and riluzole, while the inhibitory effect is indirect and mediated by PKA phosphorylation of KCNK2. Due to its polymodal activation/inhibition and expression in a variety of biological tissues, KCNK2 is involved in a broad range of physiological and pathophysiological processes13,15,16,22,23,26,27,28,29,30. KCNK2 is highly expressed in the central nervous system (CNS) and as such has been linked to a variety of neuropatholgies such as depression, pain and stroke31,32,33. Indeed, Kcnk2 knockout mice show a resistance to depression due to enhanced 5-hydroxytryptamine (serotonin) neurotransmission and an increase in neurogenesis15. As such KCNK2 has becoming a highly attractive target for treating this condition in humans. A pronounced expression of Kcnk2 has also been observed in sensory neurons where it is required for polymodal nociception. Consequently, disrupting Kcnk2 in mice makes them more sensitive to painful thermal and mechanical stimuli34. KCNK2 has also been shown to play an important role in neuroprotection against epilepsy and stroke. In particular, mice which lack a functional KCNK2 show an increased sensitivity to these pathologies. Mechanistically, it appears that KCNK2 mediates the beneficial neuroprotection provided by PUFAs and LPLs29. In the heart, KCNK2 is a key component of mechano-electric coupling and is able to modulate the ventricular action potential with an important role in the repolarization of the membrane potential35,36. In cardiac tissue, KCNK2 expression is regulated by the POPEYE domain proteins such as POPDC and POPDC2. Deletion of these proteins in mice induces an age and stress dependant sino-atrial bradycardia37. Moreover, an atrio-ventricular block has been observed in double POPDC1 and 2 knock out mice as well as in POPDC2 knock down zebrafish38,39. Consequently in humans, mutations in POPDC1 are responsible for atrio-ventricular block due to dysregulated KCNK2 activity35. Other recent studies have shown that aberrant KCNK2 expression is also associated with physiopathological cardiac conditions. Indeed, increased KCNK2 expression has been observed in patients suffering from pathological ventricular hypertrophy while decreased expression has been linked to atrial fibrillation after cardiac remodelling40,41.
The zebrafish is rapidly becoming an established in vivo model system for addressing a wide variety of physiological and pathophysiological situations. Indeed, assays have been developed which cover a wide range of conditions associated with KCNK2, ranging from depression and nociception to cardiac form and function. Because of the potential therapeutic applications associated with KCNK2, we have endeavoured to characterise this gene in zebrafish to imitate a novel in vivo model for developing KCNK2 targeted therapeutics.
Results
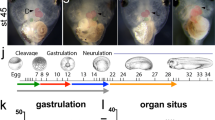
Zebrafish posess two KCNK2 orthologs
Analysis of the Ensembl database indicates that the zebrafish posess 2 orthologues of KCNK2 (kcnk2a ENSDARG00000055123 and kcnk2b ENSDARG00000007151 respectively); this is most likely the result of an ancient genome duplication. To study their biophysical properties, we first cloned both orthologs from a three days post fertilization (dpf) embryonic zebrafish cDNA library. Sequence analysis indicates that both genes are highly homolgous to human KCNK2 (kcnk2a-75.7%, kcnk2b-72.8%) (Suppl. Fig. 1). Because both kcnk2 orthologs show a high homology to the human KCNK2 gene, this indicates that the zebrafish represents a potentially useful in vivo model for developing pharmacological KCNK2 targeted therapeutics. Next we sought to determine where both zebrafish KCNK2 ortholgues are expressed during embryonic development. To achieve, this we performed in situ hybridisation on 4dpf zebrafish embryos using antisense RNA probes synthesised from either kcnk2a or kcnk2b. In this manner we were able to determine that both genes are highly expressed in the developing zebrafish brain as has been reported in mammals (Suppl. Fig. 2A,B).
Kcnk2a and Kcnk2b are activated by mechanical force
We next sought to determine whether both Kcnk2a and Kcnk2b responded to mechanical stretch in a similar manner to their mammalian counterparts. Both orthologs were subcloned into a pIRES2-GFP vector allowing us to express them in HEK cells for electrophysiological analysis. To ensure the consitiancy of our data, we first assessed the transfection efficiency of both constructs and found there were no significant differences associated with this procedure (Suppl. Fig. 3A–G). Using the cell attached (CA) configuration, we found that at 0 mV potential, the application of negative pressure to the cell membrane ranging from 0 to −80 mmHg resulted in an increase in current amplitude from 0 to 410.8 ± 158.3 pA for Kcnk2a (Fig. 1A,C) and 0 to 73 ± 11,4 pA for Kcnk2b (Fig. 2A,C). No current was detected from HEK cells transfected with an empty vector (Figs 1B,C and 2B,C). We repeated this analysis using an inside out (IO) configuration, and found an increase in current amplitude of 4064.6 ± 1239.4 pA at −80 mmHg for Kcnk2a (Fig. 1D,F), and 366,1 ± 59 pA at −80 mmHg for Kcnk2b (Fig. 2D,F). No current was observed from HEK cells transfected with an empty vector (Figs 1E,F and 2E,F). Our results show that Kcnk2a and Kcnk2b are mechanosentive channels which respond to membrane stretch in a similar manner to their mammalian counterparts. Interestingly, it appears that Kcnk2a is more responsive than Kcnk2b, a feature which is not caused by a difference in channel kinetics (Suppl. Fig. 4). Whether Kcnk2b can elicit physiologically relevant responses in vivo remains to be determined, however it is also possible that this gene has become redundant.
(A–C) Recorded currents at 0 mV potential by applying an increased negative pressure from 0 to −80 mmHg on HEK cells transfected with kcnk2a-pIRES-2-eGFP in CA configuration (n = 3) (A) on HEK cells transfected with pIRES-2-eGFP in CA (n = 4) (B) and their corresponding current/pressure curves (C). (D–F) Recorded currents at 0 mV potential by applying an increased negative pressure from 0 to −80 mmHg on HEK cells transfected with kcnk2a-pIRES-2-eGFP in IO configuration (n = 7) (D) on HEK cells transfected with pIRES-2-eGFP in IO configuration (n = 4) (E) and their corresponding current/pressure curves (F). *P value < 0.05; **P value < 0.01. (G) Recorded currents in IO configuration by applying a voltage ramp going from −100 to +100 mV on HEK cells transfected with kcnk2a-pIRES-2-eGFP at pH 7.2 (black line) at pH 6.2 (red line) at pH 6.2 (blue line) (n = 9). Recorded currents on HEK cells transfected with pIRES-2eGFP at pH 5.2 (green line) (n = 3). (H) Typical graph showing the current amplitudes at 0 mV potential for each test conditions, *P value < 0.05; **P value < 0.01.
(A–C) Recorded currents at 0 mV potential by applying an increased negative pressure from 0 to −80 mmHg on HEK cells transfected with kcnk2b-pIRES-2-eGFP in CA configuration (n = 8) (A) on HEK cells transfected with pIRES-2-eGFP in CA (n = 4) (B) and their corresponding current/pressure curves (C). (D–F) Recorded currents on HEK cells transfected with kcnk2b-pIRES-2-eGFP in IO configuration (n = 19) (D) on HEK cells transfected with pIRES-2-eGFP in IO configuration (n = 4) (E) and their corresponding current/pressure curves (F). **P value < 0.01; ***P value < 0.001. (G) Recorded currents in IO configuration by applying a voltage ramp going from −100 to +100 mV on HEK cells transfected with kcnk2b-pIRES-2-eGFP at pH 7.2 (black line) at pH 6.2 (red line) at pH 6.2 (blue line) (n = 11). Recorded currents on HEK cells transfected with pIRES-2eGFP at pH 5.2 (green line) (n = 3). (H) Typical graph showing the current amplitudes at 0 mV potential for each test conditions, **P value < 0.01.
Kcnk2a and Kcnk2b are activated by intracellular acidification
Previous research indicates that in mammals, KCNK2 can also be activated under acidic condition. To assess if this was also the case for either Kcnk2a or Kcnk2b, we repeated our electrophysiological analysis under decreasing pH conditions. Firstly, using the IO configuration, we lowered the pH of the perfused intracellular solution from 7.2 to 6.2 and then to 5.2. At 0 mV potential, the Kcnk2a current amplitude increased from 79.1 ± 9.3 pA at pH 7.2 to 183.6 ± 34.7 pA at pH 6.2 and to 428.8 ± 99 pA at pH 5.2 compared to the control which peaked at 25.7 ± 4.5 at pH 5.2 (Fig. 1G,H). However, for Kcnk2b the increase in current amplitudes was much more subdued ranging from 7,7 ± 1,2 pA at pH 7.2 to 29,9 ± 12,3 pA at pH 6.2 and to 81,5 ± 23,6 pA at pH 5.2 while the control reached 6,9 ± 1,3 pA at pH 5.2 (Fig. 2G,H). Taken together our data indicates that Kcnk2a and Kcnk2b both show increased activity under acidic conditions as has been reported for their mammalian counterpart. However, as we observed during the mechanical stimulation analysis, Kcnk2b appears to generate much lower current amplitudes that Kcnk2a, again indicating that these genes may be redundant.
Kcnk2a and Kcnk2b can be activated by the polyunsaturated fatty acids DHA and AA
We next sought to evaluate if PUFAs such as DHA and AA are able to activate either Kcnk2a or Kcnk2b in a similar manner as has been observed for mammalian Kcnk2. Basal Kcnk2a currents were recorded in the whole cell (WC) configuration using HEK cells transfected with Kcnk2a-pIRES-2-eGFP in the presence of a cocktail of potassium channel inhibitors (4-AP, TEA, glibenclamide, apamin, charybdotoxin) (Fig. 3A,D). Currents are presented as current densities pA/pF. Perfusion of DHA 10 µM promotes an increase of current density amplitudes from 72,52 ± 3,48 pA/pF to 615,10 ± 166,87 at 0 mV potential (Fig. 3B,D). In the presence of K+ blockers cocktail DHA perfusion on HEK cells transfected with pIRES-2-eGFP empty vector does not promote an increase of basal current amplitude (Fig. 3C). For Kcnk2b we found that the same treatment with DHA from kcnk2b basal current (Fig. 4A) resulted in an increase of current density amplitudes from 37,3 ± 9,8 pA/pF to 165,3 ± 45,1 at 0 mV potential on (Fig. 4B,D). In the presence of K+ blockers cocktail DHA perfusion on HEK cells transfected with pIRES-2-eGFP empty vector does not promote an increase of basal current amplitude (Fig. 4C). Next we repeated these assays substituting DHA for AA. In this manner we found that perfusion of 10 µM of AA from basal kcnk2a and kcnk2b currents (Figs 3E, 4E) promoted an increase of current density amplitudes from 42,35 ± 8,81 to 304,70 ± 41,96 pA/pF at 0 mV potential for Kcnk2a (Fig. 3F,H) and 19,7 ± 7,6 to 284,7 ± 143,6 for Kcnk2b (Fig. 4F,H). In the presence of K+ blockers cocktail AA perfusion on HEK cells transfected with pIRES-2-eGFP empty vector does not promote an increase of basal current amplitude (Fig. 3G, 4G).These data indicate that both Kcnk2a and Kcnk2b are positively regulated by the PUFAs DHA and AA as has been reported for the mammalian counterpart.
(A,B,E,F) Recorded currents in WC configuration by applying a voltage steps protocole going from −100 to + 60 mV by – 20 mV increments. on HEK cells transfected with kcnk2a-pIRES-2-eGFP in the presence of potassium cocktail blockers (A,E) (n = 5), in the presence of potassium cocktail blockers and unsaturated fatty acid 10 µM of Docosahexaenoic acid (DHA) (n = 5) (B) or 10 µM of arachidonic acid (AA) (n = 5) (F). (C,G) Recorded currents on HEK cells transfected pIRES-2-eGFP in presence of the potassium cocktail blockers and 10 µM of each polyunsaturated fatty acid DHA (n = 5) (C) or AA (n = 5) (G). (D,H) Corresponding Current/potential curves for each tested condition.
(A,B,E,F) Recorded currents in WC configuration by applying a voltage steps protocole going from −100 to +60 mV by −20 mV increments on HEK cells transfected with kcnk2b-pIRES-2-eGFP in the presence of potassium cocktail blockers (n = 5) (A,E) in the presence of potassium cocktail blockers and unsaturated fatty acid 10 µM of Docosahexaenoic acid (DHA) (n = 5) (B) or 10 µM of arachidonic acid (AA) (n = 5) (F). (C,G) Recorded currents on HEK cells transfected pIRES-2-eGFP in presence of the potassium cocktail blockers and 10 µM of each polyunsaturated fatty acid DHA (n = 5) (C) or AA (n = 5) (G). (D,H) Corresponding Current/potential curves for each tested condition.
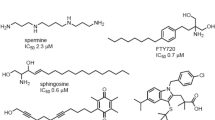
Spadin, a KCNK2 inhibitory peptide, also blocks Kcnk2a and Kcnk2b activity
In order to evaluate the effects of Spadin, a KCNK2 channel inhibitor, on Kcnk2a and Kcnk2b, we repeated the mechanostimulation protocol in the presence or absence of this molecule. Typical Kcnk2a currents were recorded in control conditions with an amplitude of 3526 ± 482,4 pA at −60 mmHG pressure stimulation (Fig. 5A,C). Following the introduction of 10 µM of spadin into the pipette medium, we observed a significant decrease of the recorded current from 3526 ± 482,4 to 148,4 ± 56,5 pA at – 60 mmHG (Fig. 5B,C). Likewise we also observed that Spadin produced a significant inhibitory effect on Kcnk2b by reducing the control current amplitude (Fig. 5D,F) from 156,3 ± 36,5 to 42 ± 9,2 pA at – 60 mmHG (Fig. 5E,F). Furthermore, spadin inhibition only affected the current amplitude and did not disrupt the channel kinetics (Suppl. Fig. 4). Lastly, we assessed whether spadin was capable of inhibiting kcnk2 currents in zebrafish cardiomyocytes. To achieve this we first established primary cultures of adult zebrafish cardiomyocytes and performed electrophysiological recordings from individual cardiomyocytes. In this manner we were able to detect Kcnk2 like currents following negative pressure simulation (Suppl. Fig. 5A,C). Importantly these currents could be significantly inhibited when the cardiomyocytes were treated with spadin, indicating that a Kcnk2 must be responsible for significant proportion of the measured current observed in zebrafish cardiomyocytes (Suppl. Fig. 5B,C).These data indicate that spadin, an inhibitory peptide developed to target KCNK2, significantly inhibits both Kcnk2a and Kcnk2b. This also indicates that the zebrafish orthologs of KCNK2 will be useful for developing targeting strategies for this gene.
Recorded currents in IO configuration by applying an increasing negative pressure protocol from 0 to −80 mmHg by – 10 mmHG pressure step increments on HEK cells transfected with kcnk2a-pIRES-2-eGFP (control condition) (n = 7) (A) in the presence of 10 µM of spadin into the pipette medium (n = 6) (B) and their corresponding current/pressure curves (C). Recorded currents in IO configuration by applying an increasing negative pressure protocol from 0 to −80 mmHg by – 10 mmHG pressure step increments on HEK cells transfected with kcnk2b-pIRES-2-eGFP (control condition) (n = 7) (D) in the presence of 10 µM of spadin into the pipette medium (n = 6) (E) and their corresponding current/pressure curves (F). *P value < 0.05, ***P value < 0.001.
Discussion
Here we have identified two zebrafish orthologs of KCNK, namely kcnk2a and kcnk2b. Both orthologs are highly homologous to their human counterpart including many known KCNK2 regulatory residues. Furthermore, both orthologs are also highly expressed in the developing zebrafish brain as has been reported in mammals and humans. We were also able to detect Kcnk2 channel currents in zebrafish cardiomyocytes, however we were not able to determine whether these currents were generated solely by one of the orthologs or, are a combination of the the two. Our electrophysiological recordings indicate that both channels are sensitive to mechanostimulation as has been observed for the mammalian KCNK8. Indeed, the increase in current amplitude observed between cell attached and inside out configurations indicates that both Kcnk2a and Kcnk2b are also negatively regulated by the cytoskeleton in response to mechanostimulation8,9. KCNK2 also acts as a cytoplasmic pH sensor whereby increasing intracellular acidity induces channel activation8,9. This particular property suggests a putative protective role for KCNK2 against ischemia and pain, in which disrupted metabolism promotes intracellular acidification29,42,43,44. Consequently, the increasing acidity triggers KCNK2 to open resulting in cell membrane hyperpolarisation, a protective phenomenon also produced by ATP sensitive potassium channels during cardiac and cerebral ischemia45,46. Here we also demonstrate that both Kcnk2a and Kcnk2b respond positively when the intracellular pH decreases from 7.2 to 5.2. PUFAs represent another mode by which KCNK2 can be activated. Indeed, arachidonic acid (AA), docosahexaenoic acid (DHA), alpha linolenic acid ALA, ecosapentaenoic acid (EPA), lysophospholipids (LP) such as lysophosphatidylcholine (LPC) have all been shown to be capable of inducing KCNK2 activity9,11,12,13,14. Preventative therapies utilising PUFAs have been developed to tackle cardiovascular and cerebrovascular diseases such as myocardial infarction, cerebral stroke, pain and epillepsia. One of the ways in which PUFAs produce a protective effect is via potassium channel mediated cell membrane hyperpolarization, which in turn promotes cell survival under pathological conditions. For example, cell membrane hyperpolarization promotes a significant decrease in stroke damage in mouse models of cerebral focal ischemia12,13,29,42,47. These results are supported by in vitro data showing the protective role PUFA mediated KCNK2 activation has on primary cultures of neurons during oxygen/glucose deprivation studies9,47. Here we have shown that both zebrafish KCNK2 orthologs are also activated by the PUFAs DHA and AA in a similar manner to their mammalian counterparts indicating that zebrafish represent a potentially useful in vivo model for further development of PUFAs based therapeutic strategies. Although both Kcnk2a and Kcnk2b show similar biophysical properties and polymodal activation to mammalian KCNK2 channels, we were able to determine a very obvious difference in active current amplitudes between the two zebrafish orthologs. The presence of two copies of the same gene in zebrafish is not uncommon and has been attributed to an ancient whole genome duplication event. Our data indicates that Kcnk2b appears to generate much lower current amplitudes than Kcnk2a following different modes of activation (although there appears to be no difference in the channel kinetics). One explanation for this difference is that over time Kcnk2b has become redundant to Kcnk2a, however more extensive research, for example generation of CRISPR/Cas9 knockout zebrafish lines, will be required to determine whether Kcnk2b can compensate for Kcnk2a and vice versa. Furthermore, a detailed comparison of the composition/structure between Kcnk2a and Kcnk2b may provide valuable information about how these channels function. Depression in humans can be treated by selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine and norefluoxetine15,17,48. Both these compounds have been shown to effectively inhibit KCNK2 which has made this channel an attractive pharmacological target to treat depression2,15. Indeed, over the last decade, several molecules have been developed to specifically inhibit KCNK2 activity such as the short peptide Spadin9,16,20,21,22,23,24. This molecule has been shown to display a therapeutic effect in mouse models of depression, a feature linked to its specific inhibition KCNK2. Our data indicates that Spadin also effectively inhibits both Kcnk2a and Kcnk2b following mechanostimulation indicating that there is sufficient homology between the zebrafish and mammalian channels for testing KCNK2 specific pharmacology. Taken together, our data lays the groundwork for developing the zebrafish as an in vivo model for KCNK2 targeted therapeutic strategies.
Methods
Kcnk2a and Kcnk2b cloning
Kcnk2a and kcnk2b were cloned from a 3 days post fertilisation zebrafish cDNA library using the following nested sets of primers:
kcnk2a
Forward primer 5′ AGCGAGAACAGCAGATCCCA 3′
Reverse primer 5′ GCTTACATTTTAGTATGTGC 3′
Forward nested primer 5′ ATGGCTGCACCTGATCTTTT 3′
Reverse nested primer 5′ TTATTTGAGATGTTCAATGA 3′
kcnk2b
Forward primer 5′ GCTGCTGAAGCCTCCAGAGG 3′
Reverse primer 5′ CAGCTTGTCCTTTGAATTTC 3′
Forward nested primer 5′ ATGCGCTGGAAGACCGTGCT 3′
Reverse nested primer 5′ TCATTTTGTCTGTATTCTAG 3′.
PCR products were initially cloned into pGEMT Easy and sequenced before subcloning into pIRES2-GFP.
In situ hybridisation
Anti-sense probes were synthesized as described previously49. In situ hybridization were performed as described previously50.
Cell culture and transfection
Both channels were expressed in HEK-293 cells (American type culture collection, Manassas, VA, USA) by transient transfection using JetPei cationic lipids (Ozyme, France) following the manufacturers protocol. HEK-293 cells were grown in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% (v/v) heat inactivated fetal bovine serum (FBS) and 1% (v/v) penicillin/streptomycin and 95% air/5% CO2. HEK-293 cells were plated in 35 mm diameter dishes for transfection at a density of 15 000 cells per dish. 0.5–1 µg of each plasmid was used to transfect 10 dishes of HEK-293 cells. Transfected cells were assayed two days after transfection and during the three following days. Transfected cells were maintained in DMEM culture medium (10% FBS, 1% penicillin/streptomycin) in 95% air/5% CO2.
Cardiomyocyte isolation and culture
Adult zebrafish cardiomyocytes were isolated and cultured as described previously51.
Electrophysiology
Whole cell current recordings: Each current was calculated by using an axopatch 200B amplifier (Axon Instrument, Sunnyvale, CA, USA), low-pass filtered 3 kHz and digitized at 10 kHz using a 12-bits analog to digital converter digidata (1440 A series, Axon Instrument, Sunnyvale, CA, USA). Patch clamp pipettes were pulled using vertical puller PC-10 (Narashighe, London, UK) from borosilicate glass capillaries with a resistance between 3–5 MΩ. The bath solution contained (in mM) 150 NaCl, 5 KCl, 3 MgCl2, 1 CaCl2 and 10 HEPES adjusted to pH 7.4 with NaOH. The pipette solution contained (in mM) 155 KCl, 3 MgCl2, 5 EGTA and 10 HEPES adjusted to pH 7.2 with KOH. All experiments were performed at room temperature (22 °C). Kcnk2a and Kcnk2b currents were measured in the presence of a cocktail of potassium channel inhibitors (K+ blockers: 3 mM 4-aminopyridine (4-AP), 10 mM tetraethylamonium (TEA), 10 µM glibenclamide, 100 nM apamin and 50 nM charybdotoxin). Stimulation protocols and data acquisition were carried out using a microcomputer (Dell pentium), which used commercial software and hardware (pClamp 10.2). Cells were clamped at −80 mV and voltage changes were applied by steps of 20 mV from −100 to +60. Duration of depolarization pulses was 0.825 ms and the pulse cycling rate was 5 s. Kcnk2a and Kcnk2b current amplitudes were calculated at the end of the stimulation pulses. Cells were continousely perfused with a microsuperfusion system. Electrophysiological and pharmacological Kcnk2a and Kcnk2b current characterization was obtained using two KCNK2 activators, arachidonic acid AA and docosaexaenoic acid DHA. One concentration at 10 µM was used to perfuse the cells with these two PUFAs. Current amplitudes were expressed in current densities. Results are expressed as mean ± standard error of the mean (SEM).
Mechanical activation by cell membrane stretch
Kcnk2a and Kcnk2b mechanical activation by cell membrane stretch was performed in both cell attached (CA) and inside out (IO) configurations. The bath solution contained (in mM) 155 KCl, 3 MgCl2, 5 EGTA and 10 HEPES adjusted to pH 7.2 with KOH. The pipette solution contained (in mM) 150 NaCl, 5 KCl, 2 CaCl2 and 10 HEPES adjusted to pH 7.4 with NaOH. Patch pipettes were around 1.2–1.5 MΩ and cell membranes were stimulated with negative pressure pulses from 0 to −80 mmHG in −10 mmHG increments during 300 ms each 3 s, through the recording electrode using a pressure clamp device (ALA High Speed Pressure Clamp-1 system, ALA-scientific).
Activation by intracellular acidification
Kcnk2a and Kcnk2b activation by intracellular acidification was performed in inside out (IO) configuration. Cells were stimulated by a voltage ramp protocol from −120 mV to 60 mV during 550 ms each 3 s. Holding potential was maintained at −80 mV. Cell membranes were continuously perfused by the pH 7.2 control solution, and by both experimental pH 6.2 and 5.2 solutions until a steady state was achieved. The bath and pipette mediums for the pH experiments were the same inside out mediums described in the mechanical activation method. For all experiments, currents were filtered at 1 KHz, digitized at 20 kHz and analyzed with pClamp 10.2 and Origin 8.0 softwares. Data is expressed as mean ± S.E.M. Statistical analysis of differences between groups was performed using a students unpaired t test. In all analyses, the level of significance is (*)p < 0.05, (**)P < 0.01 and (***)P < 0.001.
References
Kim, D. Physiology and pharmacology of two-pore domain potassium channels. Curr Pharm Des 11, 2717–2736 (2005).
Honore, E. The neuronal background K2P channels: focus on TREK1. Nat Rev Neurosci 8, 251–261, https://doi.org/10.1038/nrn2117 (2007).
Barel, O. et al. Maternally inherited Birk Barel mental retardation dysmorphism syndrome caused by a mutation in the genomically imprinted potassium channel KCNK9. American journal of human genetics 83, 193–199, https://doi.org/10.1016/j.ajhg.2008.07.010 (2008).
Lafreniere, R. G. et al. A dominant-negative mutation in the TRESK potassium channel is linked to familial migraine with aura. Nat Med 16, 1157–1160, https://doi.org/10.1038/nm.2216 (2010).
Davies, L. A. et al. TASK channel deletion in mice causes primary hyperaldosteronism. Proc Natl Acad Sci USA 105, 2203–2208, https://doi.org/10.1073/pnas.0712000105 (2008).
Manichaikul, A. et al. KCNK3 Variants Are Associated With Hyperaldosteronism and Hypertension. Hypertension 68, 356–364, https://doi.org/10.1161/HYPERTENSIONAHA.116.07564 (2016).
Christensen, A. H. et al. The two-pore domain potassium channel, TWIK-1, has a role in the regulation of heart rate and atrial size. Journal of molecular and cellular cardiology 97, 24–35, https://doi.org/10.1016/j.yjmcc.2016.04.006 (2016).
Maingret, F., Patel, A. J., Lesage, F., Lazdunski, M. & Honore, E. Mechano- or acid stimulation, two interactive modes of activation of the TREK-1 potassium channel. The Journal of biological chemistry 274, 26691–26696 (1999).
Moha ou Maati, H. et al. A human TREK-1/HEK cell line: a highly efficient screening tool for drug development in neurological diseases. PloS one 6, e25602, https://doi.org/10.1371/journal.pone.0025602 (2011).
Gruss, M., Mathie, A., Lieb, W. R. & Franks, N. P. The two-pore-domain K(+) channels TREK-1 and TASK-3 are differentially modulated by copper and zinc. Mol Pharmacol 66, 530–537, https://doi.org/10.1124/mol.66.3. (2004).
Fink, M. et al. A neuronal two P domain K+ channel stimulated by arachidonic acid and polyunsaturated fatty acids. The EMBO journal 17, 3297–3308, https://doi.org/10.1093/emboj/17.12.3297 (1998).
Heurteaux, C., Laigle, C., Blondeau, N., Jarretou, G. & Lazdunski, M. Alpha-linolenic acid and riluzole treatment confer cerebral protection and improve survival after focal brain ischemia. Neuroscience 137, 241–251, https://doi.org/10.1016/j.neuroscience.2005.08.083 (2006).
Lauritzen, I. et al. Polyunsaturated fatty acids are potent neuroprotectors. The EMBO journal 19, 1784–1793, https://doi.org/10.1093/emboj/19.8.1784 (2000).
Maingret, F., Patel, A. J., Lesage, F., Lazdunski, M. & Honore, E. Lysophospholipids open the two-pore domain mechano-gated K(+) channels TREK-1 and TRAAK. The Journal of biological chemistry 275, 10128–10133 (2000).
Heurteaux, C. et al. Deletion of the background potassium channel TREK-1 results in a depression-resistant phenotype. Nature neuroscience 9, 1134–1141, https://doi.org/10.1038/nn1749 (2006).
Moha ou Maati, H. et al. The peptidic antidepressant spadin interacts with prefrontal 5-HT(4) and mGluR(2) receptors in the control of serotonergic function. Brain Struct Funct 221, 21–37, https://doi.org/10.1007/s00429-014-0890-x (2016).
Sandoz, G., Bell, S. C. & Isacoff, E. Y. Optical probing of a dynamic membrane interaction that regulates the TREK1 channel. Proc Natl Acad Sci USA 108, 2605–2610, https://doi.org/10.1073/pnas.1015788108 (2011).
Ryoo, K. & Park, J. Y. Two-pore Domain Potassium Channels in Astrocytes. Experimental neurobiology 25, 222–232, https://doi.org/10.5607/en.2016.25.5.222 (2016).
Tamargo, J., Caballero, R., Gomez, R., Valenzuela, C. & Delpon, E. Pharmacology of cardiac potassium channels. Cardiovasc Res 62, 9–33, https://doi.org/10.1016/j.cardiores.2003.12.026 (2004).
Borsotto, M. et al. Targeting two-pore domain K(+) channels TREK-1 and TASK-3 for the treatment of depression: a new therapeutic concept. British journal of pharmacology 172, 771–784, https://doi.org/10.1111/bph.12953 (2015).
Devader, C. et al. In vitro and in vivo regulation of synaptogenesis by the novel antidepressant spadin. British journal of pharmacology 172, 2604–2617, https://doi.org/10.1111/bph.13083 (2015).
Mazella, J. et al. Spadin, a sortilin-derived peptide, targeting rodent TREK-1 channels: a new concept in the antidepressant drug design. PLoS Biol 8, e1000355, https://doi.org/10.1371/journal.pbio.1000355 (2010).
Moha Ou Maati, H. et al. Spadin as a new antidepressant: absence of TREK-1-related side effects. Neuropharmacology 62, 278–288, https://doi.org/10.1016/j.neuropharm.2011.07.019 (2012).
Veyssiere, J. et al. Retroinverso analogs of spadin display increased antidepressant effects. Psychopharmacology (Berl) 232, 561–574, https://doi.org/10.1007/s00213-014-3683-2 (2015).
Duprat, F. et al. The neuroprotective agent riluzole activates the two P domain K(+) channels TREK-1 and TRAAK. Mol Pharmacol 57, 906–912 (2000).
Bittner, S. et al. Endothelial TWIK-related potassium channel-1 (TREK1) regulates immune-cell trafficking into the CNS. Nat Med 19, 1161–1165, https://doi.org/10.1038/nm.3303 (2013).
Franks, N. P. & Honore, E. The TREK K2P channels and their role in general anaesthesia and neuroprotection. Trends Pharmacol Sci 25, 601–608, https://doi.org/10.1016/j.tips.2004.09.003 (2004).
Gil, V. et al. Relative contribution of SKCa and TREK1 channels in purinergic and nitrergic neuromuscular transmission in the rat colon. Am J Physiol Gastrointest Liver Physiol 303, G412–423, https://doi.org/10.1152/ajpgi.00040.2012 (2012).
Heurteaux, C. et al. TREK-1, a K+ channel involved in neuroprotection and general anesthesia. The EMBO journal 23, 2684–2695, https://doi.org/10.1038/sj.emboj.7600234 (2004).
Hivelin, C. et al. Potentiation of Calcium Influx and Insulin Secretion in Pancreatic Beta Cell by the Specific TREK-1 Blocker Spadin. J Diabetes Res 2016, 3142175, https://doi.org/10.1155/2016/3142175 (2016).
Hervieu, G. J. et al. Distribution and expression of TREK-1, a two-pore-domain potassium channel, in the adult rat CNS. Neuroscience 103, 899–919 (2001).
Medhurst, A. D. et al. Distribution analysis of human two pore domain potassium channels in tissues of the central nervous system and periphery. Brain Res Mol Brain Res 86, 101–114 (2001).
Talley, E. M., Solorzano, G., Lei, Q., Kim, D. & Bayliss, D. A. Cns distribution of members of the two-pore-domain (KCNK) potassium channel family. J Neurosci 21, 7491–7505 (2001).
Alloui, A. et al. TREK-1, a K+ channel involved in polymodal pain perception. EMBO J 25, 2368–2376, https://doi.org/10.1038/sj.emboj.7601116 (2006).
Decher, N., Kiper, A. K. & Rinne, S. Stretch-activated potassium currents in the heart: Focus on TREK-1 and arrhythmias. Prog Biophys Mol Biol 130, 223–232, https://doi.org/10.1016/j.pbiomolbio.2017.05.005 (2017).
Unudurthi, S. D. et al. Two-Pore K+ Channel TREK-1 Regulates Sinoatrial Node Membrane Excitability. J Am Heart Assoc 5, e002865, https://doi.org/10.1161/JAHA.115.002865 (2016).
Froese, A. et al. Popeye domain containing proteins are essential for stress-mediated modulation of cardiac pacemaking in mice. The Journal of clinical investigation 122, 1119–1130, https://doi.org/10.1172/JCI59410 (2012).
Kirchmaier, B. C. et al. The Popeye domain containing 2 (popdc2) gene in zebrafish is required for heart and skeletal muscle development. Developmental biology 363, 438–450, https://doi.org/10.1016/j.ydbio.2012.01.015 (2012).
Simrick, S., Schindler, R. F., Poon, K. L. & Brand, T. Popeye domain-containing proteins and stress-mediated modulation of cardiac pacemaking. Trends Cardiovasc Med 23, 257–263, https://doi.org/10.1016/j.tcm.2013.02.002 (2013).
Schmidt, C. et al. Stretch-activated two-pore-domain (K2P) potassium channels in the heart: Focus on atrial fibrillation and heart failure. Prog Biophys Mol Biol 130, 233–243, https://doi.org/10.1016/j.pbiomolbio.2017.05.004 (2017).
Wang, W. et al. An increased TREK-1-like potassium current in ventricular myocytes during rat cardiac hypertrophy. J Cardiovasc Pharmacol 61, 302–310, https://doi.org/10.1097/FJC.0b013e318280c5a9 (2013).
Blondeau, N. et al. Polyunsaturated fatty acids are cerebral vasodilators via the TREK-1 potassium channel. Circ Res 101, 176–184, https://doi.org/10.1161/CIRCRESAHA.107.154443 (2007).
Buckler, K. J. & Honore, E. The lipid-activated two-pore domain K+ channel TREK-1 is resistant to hypoxia: implication for ischaemic neuroprotection. J Physiol 562, 213–222, https://doi.org/10.1113/jphysiol.2004.077503 (2005).
Yang, X. et al. Functional study of TREK-1 potassium channels during rat heart development and cardiac ischemia using RNAi techniques. J Cardiovasc Pharmacol 64, 142–150, https://doi.org/10.1097/FJC.0000000000000099 (2014).
Chen, X. Q., Wu, S. H., Zhou, Y. & Tang, Y. R. Involvement of K+ channel-dependant pathways in lipoxin A4-induced protective effects on hypoxia/reoxygenation injury of cardiomyocytes. Prostaglandins Leukot Essent Fatty Acids 88, 391–397, https://doi.org/10.1016/j.plefa.2013.03.007 (2013).
Moha Ou Maati, H. et al. Activation of ATP-sensitive potassium channels as an element of the neuroprotective effects of the Traditional Chinese Medicine MLC901 against oxygen glucose deprivation. Neuropharmacology 63, 692–700, https://doi.org/10.1016/j.neuropharm.2012.05.035 (2012).
Blondeau, N., Lauritzen, I., Widmann, C., Lazdunski, M. & Heurteaux, C. A potent protective role of lysophospholipids against global cerebral ischemia and glutamate excitotoxicity in neuronal cultures. J Cereb Blood Flow Metab 22, 821–834, https://doi.org/10.1097/00004647-200207000-00007 (2002).
Kennard, L. E. et al. Inhibition of the human two-pore domain potassium channel, TREK-1, by fluoxetine and its metabolite norfluoxetine. British journal of pharmacology 144, 821–829, https://doi.org/10.1038/sj.bjp.0706068 (2005).
Thisse, C., Thisse, B., Schilling, T. F. & Postlethwait, J. H. Structure of the zebrafish snail1 gene and its expression in wild-type, spadetail and no tail mutant embryos. Development 119, 1203–1215 (1993).
Jopling, C. & den Hertog, J. Fyn/Yes and non-canonical Wnt signalling converge on RhoA in vertebrate gastrulation cell movements. EMBO Rep 6, 426–431 (2005).
Sander, V., Sune, G., Jopling, C., Morera, C. & Izpisua Belmonte, J. C. Isolation and in vitro culture of primary cardiomyocytes from adult zebrafish hearts. Nature protocols 8, 800–809, https://doi.org/10.1038/nport.2013.041nport.2013.041 (2013).
Acknowledgements
Work in the C.J. lab is supported by INSERM and CNRS. Work in the C.J. lab is supported by a grant from the Fondation Leducq, a grant from the FRC and a grant from the Fédération Française de Cardiologie. H.M.M. is supported by a grant from the Association Française contre les Myopathies (AFM-Telethon). N.N. is supported by the LabexICST PhD program. A.F., H.M.M., N.N. and C.J. are members of the Laboratory of Excellence ≪Ion Channel Science and Therapeutics≫ supported by a grant from the ANR.
Author information
Authors and Affiliations
Contributions
Conceived and designed experiments: C.J., H.M.M., N.N., A.F., M.B., C.H., J.M. Performed experiments: N.N., H.M.M., A.F. Analysed the data: N.N., A.F., M.B., C.H., J.M., C.J., H.M.M. Contributed reagents/materials/analysis tools: N.N., A.F., C.J., H.M.M. Wrote the paper: N.N., A.F., C.J., H.M.M.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nasr, N., Faucherre, A., Borsotto, M. et al. Identification and characterization of two zebrafish Twik related potassium channels, Kcnk2a and Kcnk2b. Sci Rep 8, 15311 (2018). https://doi.org/10.1038/s41598-018-33664-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33664-9
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.