Abstract
CDKAL1 rs10946398 is a type 2 diabetes (T2D)-associated variant. It is a new body mass index (BMI)-associated variant in Asian populations. We investigated the association between rs10946398 and T2D among 9908 participants aged 30–70 years based on BMI: normal weight; 18.5 ≤ BMI < 24 kg/m2, overweight; 24 ≤ BMI < 27 kg/m2, and obesity; BMI ≥27 kg/m2. The CC genotype conferred a higher risk of T2D than the CA genotype. The odds ratios (ORs) were 1.83; 95% confidence interval (CI) 1.49–2.26 and 1.20; 95% CI 1.02–1.40, respectively. The C allele was the significant risk allele compared with A allele (OR = 1.32; 95% CI 1.19–1.47). For normal, overweight and obese participants with CC genotype, the ORs were respectively 1.69; 95% CI 1.02–2.81, 2.34; 95% CI 1.50–3.66, and 1.58; 95% CI 1.02–2.45 among men and 1.22; 95% CI 0.67–2.22, 2.42; 95% CI 1.30–4.52, and 2.3; 95% CI 1.19–4.50 among women. The C allele ORs were higher in obese and overweight women. In conclusion, the rs10946398 CC/CA genotypes, as well as the C allele increased the risk of T2D. The ORs were higher in women who were overweight and obese than in those with normal weight. Nonetheless, significant results were prominent only among those with CC genotype and C allele.
Similar content being viewed by others
Introduction
Type 2 diabetes is a complex metabolic disorder characterized by interaction between peripheral insulin resistance, hepatic glucose production, and beta-cell dysfunction. It remains an increasingly challenging public health issue. Globally, the prevalence of the disease is approximately 8.5% and nearly 592 million people are estimated to be infected by 20351,2. In Taiwan, the prevalence is reported to have increased from 5.8% in 2000 to 12.4% in 20143. High blood glucose is one of the significant risk factors for deaths among Taiwanese adults4.
Traditional risk factors have not fully accounted for the higher prevalence of diabetes5. Modifiable factors such as physical activity, maintenance of normal BMI, and dietary intake are relevant to studies investigating type 2 diabetes. About 36% of individuals with type 2 diabetes were found to be obese6. Besides the traditional risk factors, genetic determinants play a vital role in the development of type 2 diabetes. Some of the loci that have been consistently associated with the disease risk include CDKAL1, HHEX, CDKN2A/2B, IGF2BP2, CDC123-CAMKID, TSPAN8-LGR5, THADA, SLC30A8, ADAMTS9, FTO, PCSK9, and NOTCH2, with odds ratios ranging from 1.09–1.797,8,9,10. New independent risk variants have also been reported11. Most of the studies investigating the association between genes and T2D have been carried out in Europe12. However, only a few genetic markers for type 2 diabetes have been reported in Asia11.
Cyclin-dependent kinase 5 regulatory subunit-associated protein 1-like 1 (CDKAL1) is among the genes consistently investigated for diabetes susceptibility among Europeans. One of its variants (rs10946398) has been significantly associated with T2D9,12,13,14,15, gestational diabetes16 and diabetic retinopathy17 in different subgroups. The C allele of rs10946398 is reported to be a T2D risk allele18. A meta-analysis of cohort studies has reported significant associations between CDKAL1 variant and T2D in general populations19. However, further analyses showed significant associations only in Asian but not African subgroups. This is an indication that results from individual studies are not consistent with one another.
Obesity (defined by BMI) is strongly associated with the risk of type 2 diabetes20. There are sex differences in the pathogenesis of this disease. For example, men are said to develop it at a relatively lower BMI than women21. Genetic components have different effects in men and women. However, most of the previous associations have focused only on one sex. SNP rs10946398 is one of the variants that have shown the strongest associations with diabetes particularly in European and South East Asian populations. Besides, it is a new BMI-associated locus specifically among Asian populations22. However, it has received less attention than other SNPs22. To date, only one study has investigated the effect of this SNP on T2D in Taiwan12. Using Taiwan biobank resources, we assessed whether there are sex-related differences in the association between rs10946398 SNP and T2D based on BMI.
Results
Table 1 presents the basic characteristics of study participants and odds ratios of type 2 diabetes. Among 974 participants identified with type 2 diabetes, 619 were men and 355 were women. The mean age was 48.60 years (SD = 10.99) for men and 48.64 years (SD = 10.63) for women. The risk of diabetes imparted by the CC genotype (OR = 1.83; 95% CI, 1.49–2.26) was higher than that of the CA genotype (OR = 1.20; 95 CI, 1.02–1.40). In addition, the C allele’s effect was more significant compared with the A allele (OR = 1.32; 95% CI 1.19–1.47). The odds ratio for T2D was higher among men compared to women (OR = 1.20; 95% CI, 1:00–1.44). Table 2 presents the baseline characteristics of study participants stratified by BMI. The proportion of individuals with T2D were significantly different (p < 0.0010). Obese individuals had the highest rate of diabetes (19.64%) compared with the overweight (10.01%) and normal weight (5.42%) individuals.
Table 3 shows the association of rs10946398 with type 2 diabetes across different categories of BMI. The risks imparted by the CC genotype were as follows: normal weight (OR = 1.47; 95% CI, 1.01–2.15), overweight (OR = 2.33; 95% CI, 1.62–3.33), and obesity (OR = 1.80; 95% CI, 1.25–2.57), respectively. For the CA genotype, a significant association was found only among obese individuals (OR, 1.31; 95% CI, 1.02–1.69). However, only a borderline association was found among overweight individuals (OR, 1.33, p = 0.0540). The C allele odds ratios (compared with the A allele) were 1.17 (0.97–1.41), 1.50 (1.25–1.79), and 1.33 (1.13–1.58) for normal weight, overweight and obese individuals. In the dominant model, the interaction between BMI and rs10946398 on T2D risk was significant among women (P for interaction = 0.0318), but not men (P for interaction = 0.969).
Table 4 shows the association between rs10946398 and type 2 diabetes stratified by sex and BMI. There was no significant interaction between rs10946398 and sex. The risk of T2D among men with CC genotype was as follows: OR = 1.69 (95% CI, 1.02–2.81) among normal weight, 2.34 (95% CI, 1.50–3.66) among overweight and 1.58 (95% CI, 1.02–2.45) among obese individuals. Association between the CA genotype and T2D was not significant regardless of BMI: The odds ratios were 1.16 (CI 0.78–1.72), 1.16 (CI 0.81–1.66), and 1.23 (CI 0.90–1.69) among the normal weight, overweight, and obese category, respectively. Normal weight, overweight and obese women with CC genotype had odds ratios of 1.22 (95% CI, 0.67–2.22), 2.42 (95% CI, 1.30–4.52), and 2.31 (95% CI, 1.19–4.50), respectively. Furthermore, normal weight, overweight, and obese women with the CA genotype had odds ratios of 0.77 (CI 0.49–1.21), 1.59 (CI 0.97–2.60), and 1.51 (CI 0.98–2.32), respectively. The risk of T2D conferred by the C allele was more prominent in overweight (OR = 1.56 [CI 1.15–2.12]) and obese (OR = 1.54 [CI 1.13–2.07]) women compared to those with normal weight (OR = 1.02 [0.75–1.37]). The C allele odds ratios were 1.28 (0.99–1.64), 1.47 (1.18–1.85), and 1.25 1.02–1.54) for normal weight, overweight, and obese men. For menopausal women, a significantly higher risk was found only in the normal weight category (OR, 2.61; 95% CI, 1.17–5.80). Broadly speaking, the risk of T2D conferred by the CC genotype was higher than that of the CA genotype regardless of sex. The CC vs CA odds ratio was 1.69 vs 1.16 for normal weight, 2.34 vs 1.16 for overweight and 1.58 vs 1.23 for the obese men. Likewise, the ratios were 1.12 vs 0.77 for normal weight, 2.42 vs 1.59 for overweight and 2.31 vs 1.51 for obese women, respectively. Smoking, physical activity, and drinking were not significantly associated with T2D.
Discussion
In this study, we found a significant association between CDKAL1 rs10946398 and type 2 diabetes among Taiwanese individuals. The association was substantially stronger among CC compared to CA carriers, as well as in C allele compared to A allele carriers. Based on stratified analyses, the CC genotype was significantly associated with T2D in overweight and obese women, as well as in men regardless of their BMI. Several studies have provided evidence for the significant contribution of CDKAL1 rs10946398 to T2D risk13,14,16,22,23. According to findings from a global meta-analysis, 8 studies have reported a trend of elevated ORs for the C risk allele, whereas only two studies have found no associations14.
In our initial analysis, the CA genotype was a risk factor for T2D. However, after stratification by BMI, a significant odds ratio was found only among obese individuals (OR, 1.31; 95% CI, 1.02–1.69). When stratified by sex, borderline associations were found among overweight (OR, 1.59, P = 0.064) and obese (OR, 1.51, P = 0.061) women. However, significant odds ratios were not observed in men.
Menopause has been associated with certain unfavorable changes in the body that serve as predisposing factors for type 2 diabetes24,25. Post-menopausal women are believed to be more susceptible to T2D due to their greater percentage of body fat and intra-abdominal visceral fat26. In the present study, an increased risk of T2D was found among normal weight menopausal women (OR, 2.61; 95% CI, 1.17–5.80).
Based on the criteria defined by the Department of Health, a BMI of 18.5–23.9 kg/m2 indicates normal weight, 24–26.9 kg/m2 indicates overweight while ≥27 kg/m2 indicates obesity27. The cut-point for T2D risk in different Asian populations varies from 22–25 kg/m2. Values above 26 kg/m2 are associated with a higher risk of T2D28. In a study conducted in Taiwan, Chang and colleagues reported that the rs10946398 C allele was associated with an increased risk of T2D. This association was attenuated in persons with a larger BMI12. Nonetheless, we found contrasting results. In their study, the sample size was comparatively small and stratifications did not include sex. In addition, there was no information about the total number of participants with a higher BMI (>26.9 kg/m2). In another study, ENPP1 rs1044498 was significantly associated with T2D but not with obesity29. It is worth mentioning that T2D had no significant association with smoking, physical activity, and alcohol drinking.
The mechanism through which the CDKAL1 gene influences T2D is not fully understood. However, it has been reported that it codes for the cyclin-dependent kinase 5 (CDK5) regulatory subunit-associated protein 1-like 1 which may affect the activity of the CDK5 protein15. This may subsequently lead to degeneration of β cells and development of type 2 diabetes mellitus14.
In this Taiwan-based study, we have attempted to validate the association between CDKAL1 rs10946398 and type 2 diabetes. Such findings are necessary considering that T2D is one of the significant risk factors associated with mortality in Taiwan. Furthermore, noting that SNP rs10946398 is a new BMI-associated locus specifically for individuals of Asian ancestry, large dedicated studies are necessary to confirm such associations22. Genetic variants associated with BMI may also have associations with metabolic traits. Stratification of samples helps to clarify the role of BMI in modulating pancreatic beta-cell function possibly influenced by the rs10946398 variant. So far, such stratifications have not been widely considered in Asian populations13. Our study is limited in that we used a nonrandom or purposive sampling technique; hence, results may not be fully reflective of the general population. Second, there is a possibility of a response bias considering that information were collected using questionnaires. Moreover, there was no information regarding diabetes regimens. Finally, multiple stratifications might have affected our results. From this aspect, there is a need for additional research.
In summary, our study provides the following conclusions: (1) there is a significant association between CDKAL1 rs10946398 and type 2 diabetes among Taiwanese men and women. (2) The CC genotype is a risk factor for type 2 diabetes in women with BMI ≥ 24 kg/m2, as well as in men regardless of their BMI. (3) The CA genotype appears to be a risk factor for T2D mainly in obese individuals. In conclusion, we found that rs10946398 CC/CA genotypes and C allele increased the risk of T2D among Taiwanese adults. Overweight and obese women had higher odds ratios than normal women. However, the effect was significant only among those with CC genotype and C allele. These findings should serve as an incentive for larger dedicated studies.
Methods
Data source
Data were obtained from Taiwan Biobank, a database with genetic information of over 89169 individuals aged 30–70 years30,31,32. The project aims to recruit over 200,000 volunteers by 202732. All methods were carried out in accordance with the relevant guidelines and regulations. Participants obtained written informed consents prior to data collection. The study protocol was approved by the Institutional Review Board of Chung Shan Medical University.
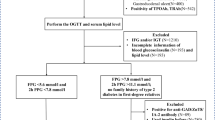
Study participants
Overall, 10853 Taiwan Biobank participants aged 30–70 years were recruited. Excluded were individuals with missing information (n = 652) and those with BMI under 18 (n = 93). The final enrollment included 9908 participants with complete phenotypic and genotypic data. Taiwan Biobank has 29 recruitment centers. Participants were assessed in specific recruitment centers during the period 2012–2016. Among those selected, 355 women and 619 men had type 2 diabetes. Individuals were defined as having type 2 diabetes mellitus if they (1) had a fasting glucose level ≥126 mg/dl; (2) had a glycosylated hemoglobin A1c value of at least 6.5%); or (3) self-reported a history of diabetes based on the question, “have you ever been diagnosed with type 1 or type 2 diabetes by a doctor or health professional?” In general, 49.49% (n = 482) of patients with type 2 diabetes were diagnosed by physicians. Participants were grouped into BMI categories: normal weight (18.5 ≤ BMI < 24 kg/m2), overweight (24 ≤ BMI < 27 kg/m2), and obesity (BMI ≥ 27 kg/m2). The selected phenotypic characteristics included age, sex, body mass index, total cholesterol (T-CHO), triglycerides (TG), high-density lipoprotein (HDL-C), low-density lipoprotein (LDL-C), uric acid, systolic blood pressure (SBP), and diastolic blood pressure (DBP). Lifestyle factors included physical activity, smoking (never/former and current smoker), and alcohol consumption (150 c.c per week or on a regular basis for 6 months). Information on menopause was based on self-report. Women who reported a complete absence of menstrual period for 12 consecutive months without hysterectomy were categorized as naturally menopausal. These variables were selected based on their previous assessments in previous studies33,34.
Genetic variant selection/Genotyping
We searched peer-reviewed literature databases (Pub Med, ScienceDirect, Google Scholar, SNPedia, and GWAS Catalog) to identify common CDKAL 1 gene variants that have been associated with type 2 diabetes. Four of the SNPs (rs10946398, rs7754840, rs7756992, and rs9465871) were chosen for analysis. However, only rs10946398 was included in the final analysis because of its highly significant association. Furthermore, it is the only CDKAL1 SNP associated with BMI among Asian populations. In addition, it has been shown to have a more striking replication signal. SNP genotyping was performed at the National Center for Genome Medicine in Academia Sinica using the Axiom-Taiwan Biobank Array Plate (Affymetrix, Santa Clara, CA, USA)31. The Axiom™ Genome-Wide ASI Array Plate maximizes genomic coverage of common and rare alleles of East Asian genome while the Axiom™ Genome-Wide CHB Array plate maximizes genomic coverage of common alleles of the Han Chinese genome. Only participants with call rates greater than 90% were included in the study. SNPs were excluded if the minor allele frequency (MAF) was <0.05. Also excluded were SNPs whose genotypes deviated from the Hardy-Weinberg equilibrium (HWE).
Statistical analysis
We used the PLINK 1.09 beta and SAS 9.3 software (SAS Institute, Cary, NC) for data management and statistical analyses. The distribution of variables were tested using Kolmogorov-Smirnov test and Shapiro-Wilk test. Data with normal distributions were analyzed by t-test and ANOVA while those not normally distributed were compared by Wilcoxon rank-sum test and Kruskal-Wallis test. Normally distributed variables were presented as mean and standard deviation (SD) while non-normally distributed variables (T-CHO, TG, HDL-C, and LDL-C) were presented as median and interquartile range (IQR). Genotypic associations of the SNP with T2D were determined using the Chi-square test. The risk allele/genotype-specific odds ratios and 95% confidence intervals were calculated using multivariate logistic regression models. Associations of genotypes with T2D were represented as co-dominant models. The interaction between BMI and rs10946398 on T2D risk was tested using a dominant model.
Data Availability
The data that support the findings of this study are available from Taiwan Biobank Institutional Dataset. To gain access, interested individuals should contact “biobank@gate.sinica.edu.tw”.
References
Forouhi, N. G. & Wareham, N. J. Epidemiology of diabetes. Medicine. 42, 698–702 (2014).
Guariguata, L. et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes. Res. Clin. Pract. 103, 137–149, https://doi.org/10.1016/j.diabres.2013.11.002 (2014).
Chen, C.-C. et al. Healthy lifestyle and normal waist circumference are associated with a lower 5-year risk of type 2 diabetes in middle-aged and elderly individuals: Results from the healthy aging longitudinal study in Taiwan (HALST). Medicine. 96 (2017).
Lo, W.-C. et al. Adult mortality of diseases and injuries attributable to selected metabolic, lifestyle, environmental, and infectious risk factors in Taiwan: a comparative risk assessment. Popul. Health. Metr. 15, 17 (2017).
Dagenais, G. R. et al. Variations in Diabetes Prevalence in Low-, Middle-, and High-Income Countries: Results From the Prospective Urban and Rural Epidemiological Study. Diabetes Care. 39, 780–787, https://doi.org/10.2337/dc15-2338 (2016).
Ulrichsen, S. P., Mor, A., Svensson, E., Larsen, F. B. & Thomsen, R. W. Lifestyle factors associated with type 2 diabetes and use of different glucose-lowering drugs: cross-sectional study. PloS one. 9, e111849 (2014).
Bonnefond, A., Froguel, P. & Vaxillaire, M. The emerging genetics of type 2 diabetes. Trends. Mol. Med. 16, 407–416 (2010).
Zeggini, E. et al. Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nature genetics. 40, 638–645 (2008).
Wu, Y. et al. Common variants in CDKAL1, CDKN2A/B, IGF2BP2, SLC30A8, and HHEX/IDE genes are associated with type 2 diabetes and impaired fasting glucose in a Chinese Han population. Diabetes. 57, 2834–2842 (2008).
Schmidt, A. F. et al. PCSK9 genetic variants and risk of type 2 diabetes: a mendelian randomisation study. Lancet. Diabetes. Endocrinol (2016).
Shu, X. O. et al. Identification of new genetic risk variants for type 2 diabetes. PLoS. Genet. 6, e1001127 (2010).
Chang, Y.-C. et al. Validation of type 2 diabetes risk variants identified by genome-wide association studies in Han Chinese population: A replication study and meta-analysis. PloS one. 9, e95045 (2014).
Peng, F. et al. The relationship between five widely-evaluated variants in CDKN2A/B and CDKAL1 genes and the risk of type 2 diabetes: a meta-analysis. Gene. 531, 435–443 (2013).
Dehwah, M., Wang, M. & Huang, Q. CDKAL1 and type 2 diabetes: a global meta-analysis. Genet. Mol. Res. 9, 1109–1120 (2010).
Al-Sinani, S. et al. Association of gene variants with susceptibility to type 2 diabetes among Omanis. World. J. Diabetes. 6, 358 (2015).
Tarnowski, M. et al. GCK, GCKR, FADS1, DGKB/TMEM195 and CDKAL1 Gene Polymorphisms in Women with Gestational Diabetes. Can. J. Diabetes (2017).
Liu, N.-J. et al. The association analysis polymorphism of CDKAL1 and diabetic retinopathy in Chinese Han population. Int. J. Ophthalmol. 9, 707 (2016).
Zeggini, E. et al. Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science. 316, 1336–1341 (2007).
Li, Y.-y et al. CDKAL1 gene rs7756992 A/G polymorphism and type 2 diabetes mellitus: a meta-analysis of 62,567 subjects. Sci. Rep. 3, 3131 (2013).
Ganz, M. L. et al. The association of body mass index with the risk of type 2diabetes: a case–control study nested in an electronic health records system in the United States. Diabetol. Metab. Syndr. 6, 50 (2014).
Logue, J. et al. Do men develop type 2 diabetes at lower body mass indices than women? Diabetologia. 54, 3003–3006 (2011).
Liang, J. et al. The CDKAL1 gene is associated with impaired insulin secretion and glucose‐related traits: the Cardiometabolic Risk in Chinese (CRC) study. Clin. Endocrinol. 83, 651–655 (2015).
Benson, K. A., Maxwell, A. P. & McKnight, A. J. A HuGE Review and meta-analyses of genetic associations in new onset diabetes after kidney transplantation. PloS one. 11, e0147323 (2016).
Gruppo di Studio Progetto Menopausa, I. Risk factors for type 2 diabetes in women attending menopause clinics in Italy: a cross-sectional study. Climacteric 8, 287–293, https://doi.org/10.1080/13697130500196866 (2005).
Shen, L. et al. Association between earlier age at natural menopause and risk of diabetes in middle-aged and older Chinese women: The Dongfeng–Tongji cohort study. Diabetes. Metab (2017).
Ghosh, A. & Bhagat, M. Indian diabetes risk score according to menopausal status in Asian Indian women: The Santiniketan Women study. Diabetes. Metab. 1, 140–141 (2009).
Fu, T., Wen, T., Yeh, P. & Chang, H. Costs of metabolic syndrome‐related diseases induced by obesity in Taiwan. Obes. Rev. 9, 68–73 (2008).
WHO, E. C. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 363, (157 (2004).
Hsiao, T.-J. & Lin, E. The ENPP1 K121Q polymorphism is associated with type 2 diabetes and related metabolic phenotypes in a Taiwanese population. Mol. Cell. Endocrinol. 433, 20–25, https://doi.org/10.1016/j.mce.2016.05.020 (2016).
Lin, E. et al. The ADAMTS9 gene is associated with cognitive aging in the elderly in a Taiwanese population. PloS one. 12, e0172440 (2017).
Lin, E. et al. Effects of circadian clock genes and health-related behavior on metabolic syndrome in a Taiwanese population: Evidence from association and interaction analysis. PloS one. 12, e0173861 (2017).
Fan, C.-T., Lin, J.-C. & Lee, C.-H. Taiwan Biobank: a project aiming to aid Taiwan’s transition into a biomedical island. Pharmacogenomics. 9, 235–246 (2008).
Luo, S. et al. A risk assessment model for type 2 diabetes in Chinese. PloS one. 9, e104046 (2014).
Bhole, V., Choi, J. W. J., Kim, S. W., De Vera, M. & Choi, H. Serum uric acid levels and the risk of type 2 diabetes: a prospective study. Am. J. Med. Sci. 123, 957–961 (2010).
Acknowledgements
This study was supported by the Ministry of Science and Technology. Support for this study was provided by the Ministry of Science and Technology (MOST 105–2627-M-040-002).
Author information
Authors and Affiliations
Contributions
O.N.N., Y.P.L. and D.M.T. conceived and designed the study. O.N.N., C.T.L., L.W., K.J.L. and T.D. acquired data and performed the literature search. C.T.L., W.H.L., S.Y.H., K.J.L., W.M.F., C.C.L. and Y.P.L. were responsible for statistical design and the analysis plan. L.W., S.Y.H., W.H.L. and C.C.H. generated the data. O.N.N. wrote the manuscript. D.M.T., T.D., C.C.H., W.M.F., C.C.L. and Y.P.L. made a critical revision of the manuscript for important intellectual content. All authors have read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nfor, O.N., Wu, MF., Lee, CT. et al. Body mass index modulates the association between CDKAL1 rs10946398 variant and type 2 diabetes among Taiwanese women. Sci Rep 8, 13235 (2018). https://doi.org/10.1038/s41598-018-31415-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-31415-4
This article is cited by
-
Association of CDKAL1 gene polymorphism (rs10946398) with gestational diabetes mellitus in Pakistani population
Molecular Biology Reports (2023)
-
Risk of uterine leiomyoma based on BET1L rs2280543 single nucleotide polymorphism and vegetarian diet
BMC Women's Health (2022)
-
Genetic Basis of Obesity and Type 2 Diabetes in Africans: Impact on Precision Medicine
Current Diabetes Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.