Abstract
The aim of this study was to examine whether using subcuticular sutures during initial hepatectomy for hepatocellular carcinoma is associated with shorter postoperative length of hospital stay (PLOS) than using staples for patients treated in the enhanced recovery after surgery (ERAS) approach. A total of 376 patients were randomized to receive either subcuticular sutures or staples (188 per group), and the two groups were compared in terms of the incidence of wound complications and PLOS. Independent risk factors for PLOS were identified by multivariate analysis. Sutures were associated with significantly lower incidence of wound infection (4.3% vs. 13.3%, P = 0.020) and significantly shorter PLOS (7.97 vs. 8.45 days, P = 0.048). Independent risk factors for wound infection after hepatectomy were advanced age, increased preoperative body mass index, decreased preoperative serum albumin, and skin closure using staples. These results suggest that subcuticular sutures may be more effective than staples for conducting hepatectomy in patients with hepatocellular carcinoma who receive ERAS care.
Similar content being viewed by others
Introduction
In recent decades, the approach of enhanced recovery after surgery (ERAS) has become popular for several abdominal procedures1,2, where rapid rehabilitation, prompt discharge, and aesthetic wound healing are important. One of the most frequent causes of longer hospitalization is postoperative wound infection3, which adds substantially to healthcare costs and lowers patients’ quality of life by aggravating wound pain and causing cosmetic problems4. At least one study has suggested that as many as 30.9% patients undergoing hepatobiliary surgery subsequently suffer wound infection5.
Several studies suggest that closing skin incisions with subcuticular sutures rather than staples can reduce incidence of postoperative wound infection and associated complications3,6,7. Although staples are fast and easy to use for skin closure following gastrointestinal surgery, subcuticular sutures are associated with better cosmetic outcomes and do not need to be removed later.
We wished to examine whether using such sutures could lead to shorter postoperative length of hospital stay (PLOS) than using staples in patients undergoing hepatectomy to treat hepatocellular carcinoma (HCC) within the ERAS care regime. We also compared sutures and staples in terms of the rate of postoperative wound infection, since such infection is the most frequent cause for prolonged PLOS. We performed multivariate analysis to identify independent risk factors of wound infection after hepatectomy. To the best of our knowledge, ours is the first study to examine the effect of subcuticular sutures on PLOS within the ERAS approach.
Patients and Methods
Ethics Statement
This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Affiliated Tumor Hospital of Guangxi Medical University. Written informed consent was given by all participants for their clinical records to be used in this study.
Patients and randomization
This prospective study involved 376 patients with HCC who were admitted for initial hepatectomy to the Department of Hepatobiliary Surgery at the Affiliated Tumor Hospital of Guangxi Medical University between January 2012 and July 2017. All these patients fulfilled the following inclusion criteria: (1) they were between 18 and 65 years old, and they were conscious, lucid and able to answer questions; (2) they had been definitively diagnosed with HCC; and (3) they did not have severe organ dysfunction, hypertension, or diabetes. Patients were excluded if they had previously undergone hepatic artery chemoembolization or radiofrequency ablation. They were also excluded if their hepatectomy was laparoscopic.
The 376 patients were randomized into 8 blocks, which were then allocated randomly to receive subcuticular sutures or staples during hepatectomy (188 patients per group). Block randomization allowed us to eliminate effects of differences in admission time and ensure that the two intervention groups would have the same size.
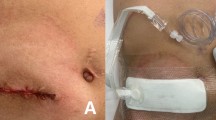
Hepatectomy and methods for sutures of the incision
The hepatectomy technique was performed as described8,9. In the group receiving staples, metallic skin staples were applied 10–15 mm apart. In the group receiving subcuticular sutures, the fascia was closed using interrupted sutures with 0 or 1 absorbable monofilament polydioxanone suture (PDS-II, Ethicon), and the subcutaneous space was irrigated with saline without antibiotics. The subcutaneous fat layer was not sutured, nor was a subcutaneous drain placed. In the subcuticular suture group, surgeons used interrupted subcuticular sutures with a 4-0 monofilament absorbable polydioxanone suture (PDS-II, Ethicon). The suture interval was 15–25 mm, and suture bite length was 15–25 mm from the edge of the skin. This provided tight skin closure.
Average blood loss during surgery was 400 ml or less, and autotransfusion was performed.
ERAS program
The same ERAS program was applied to both groups of patients (Table 1). ERAS involved a multidisciplinary team of surgeons, nurses, physical therapists, and operating room personnel. Patients were educated preoperatively about ERAS, and they did not need to empty their bowels beforehand. On the day before surgery, they were actively warmed with a coat, their central venous pressure was confirmed to be <5 mmHg, and they received warm fluids. Less intravenous fluid was delivered postoperatively than in conventional care, and intravenous fluid delivery was discontinued earlier. Nasogastric tubes were also removed earlier, and the peritoneal cavity was drained earlier. Early after surgery, patients resumed drinking and oral feeding and were encouraged to become mobile. Patients also received simo decoction and acupuncture at the tsusanli acupoint, which we have found to reduce incidence of postoperative ileus and shorten PLOS for HCC patients after hepatectomy10. Patients also received continuous portable analgesia epidurally or via a fentanyl transdermal system instead of via a patient-controlled intravenous analgesia pump.
Throughout the hospitalization period before and after surgery, patients were not allowed to smoke, and respiratory inhalation therapy was given before the operation.
Outcomes assessment
The outcomes were PLOS, wound infection, and wound separation.
We adopted the definition of superficial surgical site infections established by the US Centers for Disease Control11 as infections involving only skin or subcutaneous incisional tissues that occur within 30 days of surgery. Such infections must satisfy at least one of the following criteria: (a) purulent drainage from superficial incisions; (b) presence of microorganisms in an aseptically obtained fluid culture or from superficial incisional tissue; or (c) a sign or symptom of infection such as pain, sensitivity, localized swelling, inflammation or heat in superficial incisions intentionally caused by the surgeon (unless the incision was culture-negative).
Discharge criteri
Functional recovery was defined as adequate pain control requiring only oral analgesia, adequate oral intake with no intravenous fluid requirement, independent mobility sufficient to perform activities of daily life, and blood test values for liver function and inflammatory markers within normal ranges12. Patients were assessed daily against these criteria, and an experienced clinician determined readiness for hospital discharge.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation, and continuous data were compared between the suture and staple groups using Student’s t test. Inter-group differences in categorical data were compared using the chi-squared or Fisher exact test. Multinomial logistic regression was used to identify independent risk factors of postoperative wound infection, based on odds ratios (ORs) and associated 95% confidence intervals (CIs). All statistical analyses were performed using SPSS 19.0 (IBM, Armonk, NY, USA). P < 0.05 was considered statistically significant.
Results
Patient characteristics
Table 2 summarizes clinicopathological characteristics of the suture and staple groups. The groups showed no significant differences on any of the baseline variables examined (all P > 0.05).
Outcomes
The suture group showed significantly better outcomes than the staple group (Table 3), including lower incidence of wound infection (4.3% vs. 13.3%, P = 0.020) and wound separation (2.7% vs. 6.4%, P = 0.082). The suture group also showed significantly shorter PLOS (7.97 vs. 8.45 days, P = 0.048; Fig. 1).
Risk factors of wound infection after hepatectomy
Multivariate analyses of 11 variables identified the following as independent risk factors of wound infection after hepatectomy (Table 4): advanced age (OR 1.05, 95%CI 1.07–1.14), increased preoperative body mass index (OR 1.15, 95%CI 1.05–1.38), decreased preoperative serum albumin (OR 1.32, 95%CI 1.24–1.56), and skin closure using staples (OR 1.21, 95%CI 1.38–2.27).
Discussion
ERAS, which strives to accelerate rehabilitation and discharge, can benefit patients undergoing hepatectomy for HCC, such as by shortening PLOS13. However, postoperative wound infection can work against ERAS and prolong PLOS. Here we explore whether using subcuticular sutures instead of staples can reduce the incidence of wound infection after hepatectomy and thereby shorten PLOS. We provide the first evidence that, indeed, using sutures can reduce incidence of postoperative wound infection and concomitantly shorten PLOS as part of the ERAS approach.
Subcuticular sutures are already widely used for skin closure in several types of surgery6,14,15,16. In fact, subcuticular sutures rather than staples are indicated for skin closure in certain types of surgery, such as clean (class 1) surgery6,7,17. Subcuticular sutures are particularly popular in plastic surgery because of the relatively low incidence of wound complication and the good aesthetic appearance of the wound18,19,20. Here we demonstrate that subcuticular sutures can be safe and effective for skin closure in hepatobiliary surgery.
The incidence of wound infection in our suture and staple groups is similar to the incidence reported in other studies (5.5–19.2%)21,22,23,24,25. We observed sutures to be associated with significantly lower incidence of wound infection than staples. One reason may be that subcuticular sutures allow greater blood flow to cutaneous wounds, which promotes wound healing. One study using infrared laser Doppler flowmetry to calculate blood flow to abdominal incisions in patients after closure with staples, mattress sutures, or subcuticular sutures found postoperative blood flow to be highest in the subcuticular suture group26. Those authors suggested that staples and mattress sutures can cause tissue ischemia, perhaps because their closure area affects a greater skin area. In the current study, subcuticular sutures had a bite of 15–25 mm from the skin edge, with the needle introduced at the dermo-epidermal junction27. This effectively brings together the dermo-epidermal junction and dermis, both of which contain capillaries, type IV collagen, and fibronectin, all of which are essential for wound healing28,29.
We also observed significantly lower incidence of wound separation in the subcuticular suture group than in the staple group. We chose 4/0 PDS II as the material for the subcuticular sutures30 because it retains 74% of its tensile strength for up to two weeks and 50% after four weeks. Our results support the idea that this suture is effective for closing wounds requiring prolonged tensile strength following hepatectomy.
Our multivariate analysis identified the following risk factors of wound infection after hepatectomy: advanced age, increased preoperative body mass index, decreased preoperative serum albumin, and skin closure with staples. Several of these factors and others have been linked to wound infection following other types of surgery: advanced age22, body mass index21, increased operative time23, use of silk sutures23, increased blood loss22,31, postoperative complications, hyperglycemia21, and bile leakage21,23. Other work has also implicated that perioperative smoking cessation intervention reduces wound infections32. Thus smoking may not largely contribute to our results because smoking was banned throughout the hospital stay and respiratory inhalation therapy was given before hepatectomy. Other studies on risk factors of postoperative wound infection have not systematically examined or even reported the method of skin closure, so it is difficult to compare our results with theirs. Future work may wish to examine whether risk factors differ among different patient populations.
The current study contains several limitations that may affect the results and conclusions. First, we did not assess patient satisfaction, patient preference or potential overall effects on the healthcare system, including actual treatment costs. Second, we emphasize that some aspects of the ERAS approach in this study are not widely practiced, such as the use of a nasogastric tube, prophylactic perioperative antibiotics, or post-hepatectomy peritoneal drain. These procedures were standard practice in our hospital at the time of our study. Future work should clarify whether our results are also valid for ERAS approaches that differ from the procedures applied here.
Despite these limitations, the current study provides the first evidence that subcuticular suturing may be more effective than staples for HCC patients undergoing hepatectomy within an ERAS approach.
References
Melloul, E. et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg. 40, 2425 (2016).
Rawlinson, A., Kang, P., Evans, J. & Khanna, A. A systematic review of enhanced recovery protocols in colorectal surgery. Ann R Coll Surg Engl. 93, 583–8 (2011).
Kirkland, K. B., Briggs, J. P., Trivette, S. L., Wilkinson, W. E. & Sexton, D. J. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Cont Hose Ep. 20, 725 (1999).
Sanni, A. & Dunning, J. Staples or sutures for chest and leg wounds following cardiovascular surgery. Interact Cardiova Th. 6, 243–246 (2007).
Iñigo, J. J. et al. Surgical site infection in general surgery: 5-year analysis and assessment of the National Nosocomial Infection Surveillance (NNIS) index. Cir Espan. 79, 224–30 (2006).
Basha, S. L. et al. Randomized controlled trial of wound complication rates of subcuticular suture vs staples for skin closure at cesarean delivery. Am J Obstet Gyneco. 201(6), 1–8 (2010).
Shetty, A. A. et al. Comparing wound complication rates following closure of hip wounds with metallic skin staples or subcuticular vicryl suture: a prospective randomised trial. J Orthop Surg (Hong Kong). 12, 191–3 (2004).
Zhu, S. L. et al. Comparison of Long-Term Survival of Patients with Solitary Large Hepatocellular Carcinoma of BCLC Stage A after Liver Resection or Transarterial Chemoembolization: A Propensity Score Analysis. PloS One. 9, e115834 (2014).
Zhong, J. H. et al. Comparison of long-term survival of patients with BCLC stage B hepatocellular carcinoma after liver resection or transarterial chemoembolization. PloS One. 8, e68193 (2013).
You, X. M. et al. Randomized Clinical Trial Comparing Efficacy of Simo Decoction and Acupuncture or Chewing Gum Alone on Postoperative Ileus in Patients With Hepatocellular Carcinoma After Hepatectomy. Medicine (Baltimore). 94(45), e1968 (2015).
Listed, N. Guideline for prevention of surgical site infection. Bull Am Coll Surg. 85, 23 (2000).
van Dam, R. M. et al. Enhanced Recovery After Surgery (ERAS) Group. Initial experience with a multimodal enhanced recovery programme in patients undergoing liver resection. Br J Surg. 95, 969–75 (2008).
Kaibori, M. et al. Effects of implementing an “enhanced recovery after surgery” program on patients undergoing resection of hepatocellular carcinoma. Surg Today. 47, 1–10 (2016).
Angelini, G. D., Butchart, E. G., Armistead, S. H. & Breckenridge, I. M. Comparative study of leg wound skin closure in coronary artery bypass graft operations. Thorax. 39, 942–5 (1984).
Yamaoka, Y. et al. Efficacy of skin closure with subcuticular sutures for preventing wound infection after resection of colorectal cancer: a propensity score-matched analysis. Langenbecks Arch Surg. 400, 961–966 (2015).
Figueroa, D. et al. Surgical Staples Compared With Subcuticular Suture for Skin Closure After Cesarean Delivery: A Randomized Controlled Trial. Obstet Gynecol. 122(4), 878 (2013).
Johnson, R. G. et al. Cutaneous closure after cardiac operations: a controlled, randomized, prospective comparison of intradermal versus staple closures. Ann Surg. 226, 606 (1997).
Fisher, G. T., Fisher, J. B. & Stark, R. B. Origin of the use of subcuticular sutures. Ann Plast Surg. 4, 144 (1980).
Beasley, S. W. A combination of subcuticular suture and sterile Micropore tape compared with conventional interrupted sutures for skin closure. Ann R Coll Surg Engl. 65, 164–167 (1983).
Inotsume-Kojima, Y., Uchida, T., Abe, M., Doi, T. & Kanayama, N. A combination of subcuticular sutures and a drain for skin closure reduces wound complications in obese women undergoing surgery using vertical incisions. J Hosp Infect. 77, 162–5 (2011).
Okabayashi, T. et al. Risk factors and predictors for surgical site infection after hepatic resection. J Hosp Infect. 73, 47–53 (2009).
Kobayashi, S. et al. Risk Factors of Surgical Site Infection After Hepatectomy for Liver Cancers. World J Surg. 33, 312 (2009).
Togo, S. et al. Usefulness of absorbable sutures in preventing surgical site infection in hepatectomy. J Gastrointest Surg. 12, 1041 (2008).
Sadamori, H. et al. Risk factors for major morbidity after hepatectomy for hepatocellular carcinoma in 293 recent cases. J Hepatobiliary Pancreat Sci. 17, 709–718 (2010).
Liu, C. L. et al. Abdominal drainage after hepatic resection is contraindicated in patients with chronic liver diseases. Ann Surg. 239, 194 (2004).
Zografos, G. C., Martis, K. & Morris, D. L. Laser Doppler flowmetry in evaluation of cutaneous wound blood flow using various suturing techniques. Ann Surg. 215, 266 (1992).
Retzlaff, K., Agarwal, S., Song, D. H. & Dorafshar, A. H. The four-step subcuticular suture technique. Plast Reconstr Surg. 126(1), 50e–51e (2010).
Robinson, J. K. & Anderson, E. R. Skin structure and surgical anatomy. Surgery of the Skin. Elsevier Inc (2005).
Singer, A. J. & Clark, R. A. Cutaneous wound healing. N Engl J Med. 341, 738 (1999).
Ray, J. A., Doddi, N., Regula, D., Williams, J. A. & Melveger, A. Polydioxanone (PDS), a novel monofilament synthetic absorbable suture. Surg Gyneco Obstet. 153, 497 (1981).
Harimoto, N. et al. Prospective randomized controlled trial investigating the type of sutures used during hepatectomy. World J Gastroentero. 17, 2338 (2011).
Sørensen, L. T. Wound healing and infection in surgery: the clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg. 147, 373–383 (2012).
Acknowledgements
This research was supported by the National Science and Technology Major Special Project (2012ZX10002010001009) and the Guangxi University of Science and Technology Research Fund (KY2015LX056).
Author information
Authors and Affiliations
Contributions
Designed the study: Le-Qun Li and Zu-Shun Chen. Performed the research: Zu-Shun Chen and Shao-Liang Zhu. Statistical analyses: Lu-Nan Qi. Wrote the manuscript: Zu-Shun Chen, Shao-Liang Zhu and Lu-Nan Qi. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, ZS., Zhu, SL., Qi, LN. et al. A combination of subcuticular suture and enhanced recovery after surgery reduces wound complications in patients undergoing hepatectomy for hepatocellular carcinoma. Sci Rep 8, 12942 (2018). https://doi.org/10.1038/s41598-018-31287-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-31287-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.