Abstract
Recently, MDM4 gene has been reported to be a susceptibility gene for glioma in Europeans, but the molecular mechanism of glioma pathogenesis remains unknown. The aim of this study was to investigate whether common variants of MDM4 contribute to the risk of glioma in Han Chinese individuals. A total of 24 single-nucleotide polymorphisms (SNPs) of the MDM4 gene were assessed in a dataset of 562 glioma patients (non-glioblastoma) and 1,192 cancer-free controls. The SNP rs4252707 was found to be strongly associated with the risk of non-GBM (P = 0.000101, adjusted odds ratio (OR) = 1.34, 95% confidence interval (CI) = 1.16–1.55). Further analyses indicated that there was a significant association between A allele of rs4252707 associated with the increased non-GBM risk. Haplotype analysis also confirmed a result similar to that of the single-SNP analysis. Using stratification analyses, we found the association of rs4252707 with an increased non-GBM risk in adults (≥18 years, P = 0.0016) and individuals without IR exposure history (P = 0.0013). Our results provide strong evidence that the MDM4 gene is tightly linked to genetic susceptibility for non-GBM risk in Han Chinese population, indicating a important role for MDM4 gene in the etiology of glioma.
Similar content being viewed by others
Introduction
Glioma is the most common primary central nervous system (CNS) tumor worldwide and accounts for approximately 80% of all brain tumors1. According to the 2007 World Health Organization (WHO) Classification of Tumors of the Central Nervous System, gliomas can be broadly classified into glioblastoma (GBM) and lower-grade non-GBM tumors. Recently, the revised 2016 WHO classification has included the tumor molecular features of IDH1/ATRX mutation and 1 p/19q co-deletion2. Although the annual incidence of glioma is 5.26 per 100,000 people, or 17,000 new diagnoses per year3, the etiology of glioma is very poorly understood. To date, high-dosage ionizing radiation (IR)4 and genetic variations5 have been identified as major risk factors for glioma. Exposure to moderate-to-high doses of IR typically causes DNA damage6, which increases the risk of glioma. An increased risk for first-degree relatives of patients with glioma has been observed, indicating that glioma may be partially explained by genetic factors7. In addition, only a small proportion of individuals who are exposed to IR environments will develop glioma, suggesting hereditary factors also contribute to susceptibility to glioma8. Hence, it is necessary to identify genes through candidate gene studies that are responsible for glioma susceptibility.
The mouse double minute 4 homolog gene (MDM4), also known as MDMX, is one of the members of the MDM family, which is composed of MDM2, MDM4 and their derivatives9. One of the fundamental roles for these two proteins is the precise regulation of the tumor suppressor p53, which is vital for coordinated suppression of malignancy and cell survival10. Many studies have found that MDM4 was overexpressed in multiple primary human tumors, including breast cancer, lung cancer, colon cancer and retinoblastoma11,12,13. Approximately 40% of gliomas exhibit a p53 mutation or deletion, and approximately 80% of gliomas have a p53 pathway defect14, which may be caused by MDM4 overexpression. Previous studies showed that transcript variants of MDM4 with a short internal deletion are more efficiently translocated to the nucleus than full-length MDM4, which generates much better suppressions of p53-mediated transcription, such as MDM4-B15 and MDM4-S16. The expression levels of these transcript variants were significantly associated with tumor stage17. Hence, MDM4 may be involved in the onset and development of glioma. However, most studies focus on transcriptional levels, and little research has been designed to investigate the association between glioma and mutations of MDM4, which may be the root cause of the transcript variants of MDM4.
Understanding the genetic basis of complex human diseases has been increasingly emphasized. Recently, a meta-analysis of existing genome-wide association studies (GWASs) and two new GWASs of over 12,496 cases and 18,190 controls of European ancestry produced highly significant evidence of a strong association between the single-nucleotide polymorphism (SNP) rs4252707 (G/A) and non-glioblastoma glioma (p-value = 3.34 × 10−9, OR = 1.19)18. This SNP is located within intron 8 of the gene encoding MDM4. More importantly, the SNP rs4252707 shows strong linkage disequilibrium (LD) with rs12031912 and rs12028476, both of which map to the MDM4 promoter18. These findings may suggest that MDM4 is involved in the pathogenesis of glioma. However, these results were only identified in samples from patients of European ancestry. Given that different ethnic populations may exhibit glioma genetic heterogeneity, replications of the study using more samples from different populations are needed to confirm these results, and thus far, no information is available from the Han Chinese population regarding MDM4. Therefore, in the present study, we aimed to examine whether MDM4 was associated with the risk of non-GBM in Han Chinese population.
Materials and Methods
Study subjects
In the present study, 562 patients with non-GBM glioma (351 men and 211 women) and 1,192 cancer-free individuals (746 men and 446 women) were enrolled from Tangdu Hospital at the Fourth Military Medical University between August 2013 and October 2016. To restrict the genetic background of our study subjects, all included patients were unrelated individuals from Shaanxi Province, and their immediate family members from the previous three generations were also born locally. All patients with non-GBM gliomas (astrocytomas, ependymomas, oligodendrogliomas and mixed glioma) were histopathologically diagnosed and confirmed by at least 2 pathologists. Tumor type and stage were classified according to the 2007 WHO classification19. The exclusion strategies for the enrolled patients were as follows: (1) patients with any history of cancer; (2) patients with previous and undergoing chemotherapy and radiotherapy. As controls, the cancer-free individuals were recruited based on the selection criteria of frequency-matched gender and age (±5 years) of the patients. Inclusion criteria of the control group were as follows: (1) individuals without central nervous system-related diseases, (2) individuals without recent infections, (3) individuals without any history of cancer, and (4) individuals without the history of chemotherapy or radiotherapy. The clinical and demographic information of all subjects are summarized in Table 1, including age, gender, IR exposure history, smoking status, family history of cancer and tumor type. Informed consent were signed by all subjects. This study strictly complied with the ethical guidelines of the Helsinki Declaration (2002 version) during the implementation process and was approved by the Medical Ethics Committee of the Fourth Military Medical University.
SNP selection and genotyping
We searched for all SNPs with minor allele frequencies (MAFs) ≥ 0.02 within the region of the MDM4 gene in the 1000 Genomes Project Chinese Han Beijing population database. MAF ≥ 0.02 and tagging r2 ≥ 0.8 were used as a screening standard in the selection of tag SNP, which generated 24 tag SNPs for our study. As a result, these 24 tag SNPs (rs3014610, rs2169137, rs117139931, rs137991330, rs4252707, rs190876924, rs12024619, rs72644182, rs117137314, rs76605997, rs76432362, rs116854458, rs12138846, rs61421373, rs191840558, rs116907825, rs115517182, rs12567161, rs150337092, rs80242302, rs3789044, rs3789043, rs884108 and rs61817485) were included in further analyses. All our selected SNPs had P values greater than 0.05 by the HWE test. Commercial kits were used to extract genomic DNA from peripheral blood leukocytes (Genomic DNA kit, Axygen Scientific Inc., CA, USA). Genotyping was conducted for 24 selected SNPs by using the platform of Sequenom Mass ARRAY RS1000 system (Sequenom, San Diego, CA, USA). Typer Analyzer software (Sequenom, San Diego, California, USA) was used to process signal results to ultimately generate genotype data20. Case and control statuses were blinded during all genotyping processes for quality control. Five percent of the random samples were repeated, and the results were 100% concordant.
Statistical analyses
We examined the differences in characteristic information between case and control groups. χ2 tests and Student’s t-tests were performed for categorical variables and continuous variables, respectively. HWE for all SNPs were calculated by Haploview v4.2. Single marker-based association analyses were conducted using Plink v1.9. Logistic models were fitted for each SNP, and age and gender were included as covariates to eliminate potential confounding effects. ORs and 95% confidence intervals (CIs) were reported. Bonferroni correction was conducted to balance multi-test correction. False-positive report probability (FPRP) was calculated to evaluate the significant results in the stratification analyses by using “R” software. A FPRP threshold of 0.2 with a prior probability of 0.1 were applied for examining the correlated risk, and FPRP values less than 0.2 were suggested to be noteworthy21. LD blocks were constructed using Haploview v4.2, and the haplotypic frequencies were calculated by GENECOUNTING v2.2. The differences in haplotypic frequencies between cases and controls were investigated, and haplotypic association analyses were performed. All statistical tests in the study were two-tailed, and p values less than 0.05 were considered statistically significant.
Results
The clinical and demographic information of the patient and control groups are summarized in Table 1. Among the 562 non-GBM glioma cases, 290 patients had astrocytomas that were not classified as glioblastoma, and 272 had other types of gliomas, including ependymomas, oligodendrogliomas and mixed glioma. As shown in Table 1, we found no significant difference in age, smoking status, gender or ionizing radiation exposure history between case and control groups (P = 0.895, 0.959, 0.969 and 0.839, respectively). Approximately 16% of patients had family history of cancer, which was similar with that of the control groups (P = 0.865).
In the present study, a total of 24 SNPs within the MDM4 gene were successfully genotyped in the samples of 562 cases and 1,192 controls, and all information is presented in Supplementary Table S1. The results of single SNP association analysis of 24 SNPs as well as Hardy-Weinberg equilibrium tests are shown in Table 2 and Supplementary Table S2. All SNP genotypes were in HWE (P > 0.05) (Table 2 and Supplementary Table S2). As shown in Table 2, we identified association signals for the SNP rs4252707 with non-GBM glioma risk by multivariate logistic regression analysis. The allelic P value was 0.000101 after accounting for the effects of age and gender. The significance remained (P = 0.002424) after Bonferroni correction (P × 24). Further analyses also suggested that A allele of rs4252707 was strongly correlated with the increased non-GBM risk (odds ratio (OR) = 1.34, with the adjustment of age and gender). Genotypic association analyses also confirmed a similar pattern of results (Table 2). An increased risk was associated with A carrier genotypes of rs4252707 compared with the non-A carrier genotype (Table 2). The other 23 SNPs did not differ significantly in their allelic or genotype distributions (Supplementary Table S2). Moreover, stratified analyses were conducted based on age, IR exposure history, smoking status and tumor type for the significant SNP (rs4252707). By stratification analyses, we found the association of rs4252707 with an increased non-GBM risk in adults (≥18 years, P = 0.0016), individuals without IR exposure history (P = 0.0013), all smokers and non-smokers (P < 0.05), and all patients with non-GBM glioma (P < 0.05) (Table 3). The results of FPRP analyses for significant findings in the subgroups were presented in Table 4. We found that all significant signals for the rs4252707 were still almost noteworthy at the prior probability level of 0.1 in the subgroups except for the subgroup of ependymomas. A possible reason was the smaller sample size than other subgroups, which resulted into an insufficient power.
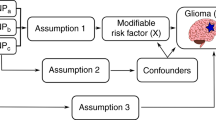
Based on the genotype data from this study, we constructed the linkage disequilibrium (LD) structure of all genotyped SNPs. As shown in Fig. 1, three LD blocks were identified in the data, and the SNP rs4252707 was included in block 1. Haplotypic association analyses were performed to test the LD block including rs4252707. The correlations between haplotypic frequencies and glioma risk are presented in Table 5, and a significant global P value (global P = 0.015) was secured from the LD region (Table 5). These results provided additional evidence for the significant correlation of the SNP of rs4252707 with the risk of non-GBM susceptibility. Haplotype of TGA was positively correlated with the risk of non-GBM glioma. Given its more prevalence in controls, the TGG haplotype may provide a protective effect (Table 5).
Discussion
Candidate gene-based association studies have successfully mapped susceptibility for many complex diseases22,23,24,25,26,27,28. Accumulating evidence indicates that many genes contribute to glioma susceptibility and risk, but the underlying molecular mechanisms remain unknown. Several studies have reported that MDM4 is involved in GBM29,30, but to date, only one study has investigated the association between MDM4 polymorphisms and non-GBM glioma occurrence in patients of European heritage18. Here, we conducted a case-control study of the MDM4 gene to evaluate the potential associations between genetic variations and glioma risk in Han Chinese population. To the best of our knowledge, this is the first study focusing on the relationship between MDM4 and glioma risk in Asians. Our study showed that rs4252707 SNP was strongly correlated with the non-GBM risk. Patients with this disease showed significantly higher frequencies of the A allele (P = 0.00010) and the AA genotype (P = 0.00016) than normal controls, which is consistent with what was observed in the European population18. Moreover, the ORs of rs4252707 in the study were similar with those reported by Melin et al.18. Considering the limitations to drawing a conclusion from the analysis of SNPs31,32,33,34,35, we examined LD structure using genotype data based on candidate SNPs to further strengthen our findings. The results revealed that the haplotype T-G-G (rs117139931 - rs137991330 - rs4252707) containing rs4252707 was also strongly correalted with the increased non-GBM risk (P = 0.00016). These findings suggest that the rs4252707 SNP of the MDM4 gene may affect the susceptibility of non-GBM glioma in Han Chinese individuals.
It has been shown that the p53 pathway is inactivated in almost all human cancers36. Approximately half of human malignancies have been estimated to carry mutations in the TP53 gene itself, whereas the remaining tumors with wild type TP53 contain genetic alterations in other key regulatory genes in the p53 pathway37,38. MDM4 is one of the key negative regulators of p53, and its overexpression or amplification contributes to carcinogenesis by inhibiting p53 tumor suppressor activity39. Genetic amplification of the MDM2 or MDM4 genes, among others, can result in aberrant protein expression and suppression of the p53 response over the course of tumor development40,41. More importantly, previous studies suggest that polymorphisms of the MDM2 or MDM4 genes may contribute to increased basal expression of these important p53 antagonists and thereby increase cancer susceptibility42,43. For example, the SNP rs4245739 in MDM4 is significantly associated with ovarian cancer, retinoblastoma and breast cancer13,44,45. Allele C of rs4245739 can cause decreased expression of MDM4 mRNA46, leading to a protective effect against cancer. In our study, the associated SNP rs4252707, which is located in intron 8 of the MDM4 gene and in LD with the MDM4 promoter, may enhance MDM4 expression and ultimately promote tumorigenesis. Therefore, based on our results, we hypothesize that the SNP rs4252707 may contribute to the risk of developing non-GBM glioma by somehow influencing the expression of MDM4, such as by affecting the splice sites or by being closely linked with some functional variations. However, the potential biological explanations for the significant associations should be confirmed by direct biological evidence in future research.
The interesting finding of our study was that the increase in the risk of developing non-GBM glioma associated with the AA genotype of rs4252707 remained significant for subjects without a history of IR exposure but not for subjects with a history of IR exposure. Thus far, the only established environmental risk factor for non-GBM glioma is exposure to therapeutic or high-dose IR4,47. A previous study found that genetic variability in DNA repair genes contributes to a hypersensitivity to IR and increased susceptibility to cancer48. Here, the association of rs4252707 was not significant in the cohort reporting IR exposure, but the result should be interpreted by cautions. Because the subset of the study subjects was very small, there was no sufficient power to test the association in the subgroup. Moreover, given of the lack of biological experimental evidence, it is still unknown whether this SNP may cause cancer through an effect on DNA damage and repair pathways or by changing the expression and activity of the p53 pathway. In the present study, only a small fraction of samples had the history of IR exposure. A possible explanation is that subjects may not be aware of exposed low-dose IR or IR of unknown sources. Additionally, we further analyzed the association between rs4252707 genotypes and environmental factors, such as age, tumor type and smoking history, that may influence the occurrence of glioma. We found that the rs4252707 genotype is closely associated with the occurrence of non-GBM glioma in the adult subgroup but is not related to smoking or the type of glioma, which is consistent with a previous epidemiological study suggesting that glioma is usually more prevalence in adults than in children49.
Although similar results were obtained in two distinctly different ethnic groups (Han Chinese and Europeans), our study has some limitations that need to be addressed. First, we only evaluated common SNPs across the MDM4 gene. Given the lack of rare variant data, these SNPs may not be sufficient to comprehensively evaluate glioma risk associated with the MDM4 gene. Second, further study is needed to determine whether the AA genotype of rs4252707 affects the expression of MDM4. Third, increasing evidences suggest an association between the history of allergy or asthma and glioma risk50,51. However, because of the lack of the relevant environmental data in our cohort, it is unclear whether this would affect the observed association in the study. The revised 2016 WHO classification redefines low grade gliomas with morphological and molecular subtype information. As known, low grade gliomas are histologically and genetically heterogeneous. Although histological grade is still effective for the diagnosis of glioma, the prognosis of patients are more closely correlated with molecular subtype than with histological grade. However, there were some difficulties in understanding genetic heterogeneity of lower grade glioma, as we have not yet obtained the molecular subtype information of the patients of glioma. Thus, future studies would be desired to confirm our results. Finally, this study was performed at a single center, which may potentially limit the generalizability of the findings. Therefore, a larger and well-designed analysis based on different populations is required to fully elucidate the relevant mechanisms in future research.
In summary, our study provides strong evidence that the MDM4 gene is tightly associated with genetic susceptibility risk of non-GBM in Han Chinese individuals. This significant finding is further confirmed by haplotypic analysis. More studies focusing on the pathological mechanisms of non-GBM glioma and MDM4 are still needed to unravel the role of MDM4 in the onset and development of non-GBM glioma.
References
Bondy, M. L. et al. Brain tumor epidemiology: consensus from the Brain TumorEpidemiology Consortium. Cancer 113(7 Suppl), 1953–1968 (2008).
Louis, D. N. et al. The2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131, 803–820 (2016).
Omuro, A. & DeAngelis, L. M. Glioblastoma and other malignant gliomas: a clinical review. Jama 310, 1842–1850, https://doi.org/10.1001/jama.2013.280319 (2013).
Lee, J. J. et al. PTEN status switches cell fate between premature senescence and apoptosis in glioma exposed to ionizing radiation. Cell Death Differ 18, 666–677, https://doi.org/10.1038/cdd.2010.139 (2011).
Gu, J., Liu, Y. H., Kyritsis, A. P. & Bondy, M. L. Molecular Epidemiology of Primary Brain Tumors. Neurotherapeutics 6, 427–435, https://doi.org/10.1016/j.nurt.2009.05.001 (2009).
Allalunisturner, M. J., Zia, P. K. Y., Barron, G. M., Mirzayans, R. & Day, R. S. Radiation-Induced DNA-Damage and Repair in Cells of a Radiosensitive Human-Malignant Glioma Cell-Line. Radiat Res 144, 288–293, https://doi.org/10.2307/3578948 (1995).
Malmer, B. et al. Genetic epidemiology of glioma. British journal of cancer 84, 429–434, https://doi.org/10.1054/bjoc.2000.1612 (2001).
Yan, M. D. et al. A case-control study of the association between the EGFR gene and glioma risk in a Chinese Han population. Oncotarget 8, 59823–59830, https://doi.org/10.18632/oncotarget.16946 (2017).
Toledo, F. & Wahl, G. M. MDM2 and MDM4: p53 regulators as targets in anticancer therapy. International Journal of Biochemistry & Cell Biology 39, 1476–1482, https://doi.org/10.1016/j.biocel.2007.03.022 (2007).
Jeyaraj, S. C., O’Brien, D. M. & Chandler, D. S. MDM2 and MDM4 splicing: an integral part of the cancer spliceome. Front Biosci 14, 2647–2656, https://doi.org/10.2741/4002 (2009).
Swetzig, W. M., Wang, J. & Das, G. M. Estrogen receptor alpha (ERalpha/ESR1) mediates the p53-independent overexpression of MDM4/MDMX and MDM2 in human breast cancer. Oncotarget 7, 16049–16069, https://doi.org/10.18632/oncotarget.7533 (2016).
Xiong, S., Pelt, C. V., Elizondofraire, C. & Lozano, G. Overexpression of Mdm4 in mouse induced spontaneous tumorgenesis. Cancer research 67, 3060–3060 (2007).
McEvoy, J. et al. Analysis of MDM2 and MDM4 single nucleotide polymorphisms, mRNA splicing and protein expression in retinoblastoma. PloS one 7, e42739, https://doi.org/10.1371/journal.pone.0042739 (2012).
Dunn, G. P. et al. Emerging insights into the molecular and cellular basis of glioblastoma. Gene Dev 26, 756–784, https://doi.org/10.1101/gad.187922.112 (2012).
Wang, X. W. et al. Identification and expression of a novel MDM4 splice variant in human glioma. Brain research 1537, 260–266, https://doi.org/10.1016/j.brainres.2013.07.054 (2013).
Bardot, B. et al. Mice engineered for an obligatory Mdm4 exon skipping express higher levels of the Mdm4-S isoform but exhibit increased p53 activity. Oncogene 34, 2943–2948, https://doi.org/10.1038/onc.2014.230 (2015).
Mancini, F., Di Conza, G. & Moretti, F. MDM4 (MDMX) and its Transcript Variants. Curr Genomics 10, 42–50, https://doi.org/10.2174/138920209787581280 (2009).
Melin, B. S. et al. Genome-wide association study of glioma subtypes identifies specific differences in genetic susceptibility to glioblastoma and non-glioblastoma tumors. Nature genetics 49, 789–794, https://doi.org/10.1038/ng.3823 (2017).
Louis, D. N. et al. The2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 114, 97–109 (2007).
Guan, F. et al. Association study of a new schizophrenia susceptibility locus of 10q24.32-33 in a Han Chinese population. Schizophr Res. 138, 63–68 (2012).
Wacholder, S., Chanock, S., Garcia-Closas, M., El Ghormli, L. & Rothman, N. Assessing the probability that a positive report is false: an approach for molecular epidemiology studies. J Natl Cancer Inst. 96, 434–42 (2004).
Guan, F. et al. Association of PDE4B polymorphisms and schizophrenia in Northwestern Han Chinese. Hum Genet. 131, 1047–1056 (2012).
Guan, F. et al. MIR137 gene and target gene CACNA1C of miR-137 contribute to schizophrenia susceptibility in Han Chinese. Schizophr Res. 152, 97–104 (2014).
Chen, G., Guan, F., Lin, H., Li, L. & Fu, D. Genetic analysis of common variants in the HDAC2 gene with schizophrenia susceptibility in Han Chinese. Journal of human genetics. 60, 479–484 (2015).
Guan, F. et al. Evaluation of genetic susceptibility of common variants in CACNA1D with schizophrenia in Han Chinese. Scientific reports. 5, 12935 (2015).
Zhang, B. et al. Common variants in SLC1A2 and schizophrenia: Association and cognitive function in patients with schizophrenia and healthy individuals. Schizophr Res. 169, 128–134 (2015).
Guan, F. et al. Evaluation of association of common variants in HTR1A and HTR5A with schizophrenia and executive function. Scientific reports. 6, 38048 (2016).
Guan, F. et al. Evaluation of voltage-dependent calcium channel γ gene families identified several novel potential susceptible genes to schizophrenia. Scientific reports. 6, 24914 (2016).
Rajaraman, P. et al. Genome-wide association study of glioma and meta-analysis. Hum Genet 131, 1877–1888, https://doi.org/10.1007/s00439-012-1212-0 (2012).
Furgason, J. M. et al. Whole genome sequence analysis links chromothripsis to EGFR, MDM2, MDM4, and CDK4 amplification in glioblastoma. Oncoscience 2, 618–628, https://doi.org/10.18632/oncoscience.178 (2015).
Guan, F. et al. A population-based association study of 2q32.3 and 8q21.3 loci with schizophrenia in Han Chinese. Journal of psychiatric research. 47, 712–717 (2013).
Yang, H. et al. 4q22.1 contributes to bone mineral density and osteoporosis susceptibility in postmenopausal women of Chinese Han population. PloS one. 8, e80165 (2013).
Guan, F. et al. Two-stage association study to identify the genetic susceptibility of a novel common variant of rs2075290 in ZPR1 to type 2diabetes. Scientific reports. 6, 29586 (2016).
Guan, F. et al. Two-stage replication of previous genome-wide association studies of AS3MT-CNNM2-NT5C2 gene cluster region in a large schizophrenia case-control sample from Han Chinese population. Schizophr Res. 176, 125–130 (2016).
Jia, X. et al. Two-stage additional evidence support association of common variants in the HDAC3 with the increasing risk of schizophrenia susceptibility. American journal of medical genetics. Part B, Neuropsychiatric genetics. 171, 1105–1111 (2016).
Vousden, K. H. & Lane, D. P. p53 in health and disease. Nature reviews. Molecular cell biology 8, 275–283, https://doi.org/10.1038/nrm2147 (2007).
Ecke, T. H. et al. TP53 gene mutations in prostate cancer progression. Anticancer research 30, 1579–1586 (2010).
Liu, W. Q., He, L. J., Ramirez, J. & Ratain, M. J. Interactions between MDM2 and TP53 Genetic Alterations, and Their Impact on Response to MDM2 Inhibitors and Other Chemotherapeutic Drugs in Cancer Cells. Clinical Cancer Research 15, 7602–7607, https://doi.org/10.1158/1078-0432.CCR-09-0890 (2009).
Teveroni, E. et al. Peptides and peptidomimetics in the p53/MDM2/MDM4 circuitry - a patent review. Expert Opin Ther Pat 26, 1417–1429, https://doi.org/10.1080/13543776.2017.1233179 (2016).
Wade, M., Wang, Y. V. & Wahl, G. M. The p53 orchestra: Mdm2 and Mdmx set the tone. Trends Cell Biol 20, 299–309, https://doi.org/10.1016/j.tcb.2010.01.009 (2010).
Riemenschneider, M. J., Knobbe, C. B. & Reifenberger, G. Refined mapping of 1q32 amplicons in malignant gliomas confirms MDM4 as the main amplification target. International Journal of Cancer 104, 752–757, https://doi.org/10.1002/ijc.11023 (2003).
Kulkarni, D. A. et al. A polymorphic variant in human MDM4 associates with accelerated age of onset of estrogen receptor negative breast cancer. Carcinogenesis 30, 1910–1915, https://doi.org/10.1093/carcin/bgp224 (2009).
Atwal, G. S. et al. Altered tumor formation and evolutionary selection of genetic variants in the human MDM4 oncogene. Proceedings of the National Academy of Sciences of the United States of America 106, 10236–10241, https://doi.org/10.1073/pnas.0901298106 (2009).
Wynendaele, J. et al. An Illegitimate microRNA Target Site within the 3′ UTR of MDM4 Affects Ovarian Cancer Progression and Chemosensitivity. Cancer research 70, 9641–9649, https://doi.org/10.1158/0008-5472.CAN-10-0527 (2010).
Pedram, N. et al. Analysis of the Association between MDM4 rs4245739 Single Nucleotide Polymorphism and Breast Cancer Susceptibility. Clin Lab 62, 1303–1308, https://doi.org/10.7754/Clin.Lab.2016.151128 (2016).
Zhou, L. Q. et al. Association of a Genetic Variation in a miR-191 Binding Site in MDM4 with Risk of Esophageal Squamous Cell Carcinoma. PloS one 8, https://doi.org/10.1371/journal.pone.0064331 (2013).
Davis, F., Il’yasova, D., Rankin, K., McCarthy, B. & Bigner, D. D. Medical Diagnostic Radiation Exposures and Risk of Gliomas. Radiat Res 175, 790–796, https://doi.org/10.1667/RR2186.1 (2011).
Hu, J. J., Smith, T. R., Miller, M. S., Lohman, K. & Case, L. D. Genetic regulation of ionizing radiation sensitivity and breast cancer risk. Environ Mol Mutagen 39, 208–215, https://doi.org/10.1002/em.10058 (2002).
Ohgaki, H. & Kleihues, P. Epidemiology and etiology of gliomas. Acta Neuropathol 109, 93–108, https://doi.org/10.1007/s00401-005-0991-y (2005).
Turner, M. C. et al. Allergy and brain tumors in the INTERPHONE study: pooled results from Australia, Canada, France, Israel, and New Zealand. Cancer Causes Control 24(5), 949–960, https://doi.org/10.1007/s10552-013-0171-7 (2013).
Pouchieu, C. et al. Allergic conditions and risk of glioma and meningioma in the CERENAT case-control study. J Neurooncol 138(2), 271–281, https://doi.org/10.1007/s11060-018-2816-6 (2018).
Author information
Authors and Affiliations
Contributions
Authors Sun P. and Song J.N. conceived and designed the study. Sun P. and Yan F. carried out candidate SNPs selection and statistical analyses. Sun P., Fang W., Zhao J.J., Hu C. and Ma X.D. conducted subject screening. Sun P., Yan F., Fang W. and Zhao J.J. contributed to the collection and preparation of control DNA samples. Sun P. wrote the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, P., Yan, F., Fang, W. et al. MDM4 contributes to the increased risk of glioma susceptibility in Han Chinese population. Sci Rep 8, 11093 (2018). https://doi.org/10.1038/s41598-018-29468-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-29468-6
This article is cited by
-
MDM4: What do we know about the association between its polymorphisms and cancer?
Medical Oncology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.