Abstract
Activin A and its binding protein follistatin may be crucial in glucose homeostasis, as multifunctional proteins mediating inflammatory and anti-inflammatory effects. However, clinical data on the activin A level in prediabetes, and the association between the circulating activin A level and carotid intima-media thickness (cIMT), are lacking. We aimed to investigate activin A and follistatin levels and their associations with cIMT. In total, 470 inhabitants of I-Lan county (235 men; mean age 69 ± 9 years) with measurements of serum activin A and follistatin levels were included. Patients with prediabetes and diabetes had significantly increased activin A concentrations compared with those in the normal glycemic group (both p < 0.001). A multivariable logistic regression model demonstrated that the circulating activin A level was associated with prediabetes and diabetes independently of other risk factors. Moreover, the circulating activin A levels were associated positively with cIMT in prediabetes (rs = 0.264, p = 0.001). In conclusion, activin A level, but not follistatin, was elevated independent of demographic variables with borderline significance and was correlated positively with cIMT in prediabetes. Activin A and follistatin levels were elevated in diabetes. In addition, elevated activin A was an independent risk factor for prediabetes and diabetes.
Similar content being viewed by others
Introduction
Type 2 diabetes is a major risk factor for cardiovascular disease with a rapidly increasing prevalence worldwide1. Abundant evidence suggests that cardiovascular complications are the leading causes of diabetes-related morbidity and mortality1,2. Individuals with insulin resistance or diabetes in combination with one or more cardiovascular risk factors have elevated risks of heart disease and stroke3,4. In addition, type 2 diabetes has been regarded as an equivalent of coronary artery disease (CAD), and the exploration of diabetic atherogenic mechanisms and biomarkers with the aim of reducing cardiovascular risk in patients with diabetes is crucial5.
Activin A, a member of the transforming growth factor (TGF)-β superfamily, has been recognized as a multifunctional cytokine expressed in a wide range of tissues and cells6. The functional roles of activin A in the regulation of wound repair, cell differentiation, apoptosis, and embryogenesis have been demonstrated6. Additionally, activin A was reported to induce insulin secretion in cultured human islets7 and rat pancreatic islets8, and to act on hepatocytes to enhance insulin sensitivity9. Therefore, activin A might induce islet cells to secrete insulin and modulate insulin resistance in liver and peripheral tissues7,8,9. Follistatin, a binding protein of activin A, is a glycosylated protein associated with the TGF-β family10. Follistatin was shown to bind and neutralize circulating activin A, and was suggested to be involved in insulin resistance and inflammation11. A recent study showed that circulating follistatin is mostly from the liver and is regulated by the glucagon-to-insulin ratio12.
Emerging evidence indicates that activin A plays a pivotal role in the pathogenesis of acute and chronic inflammatory disorders13. Enhanced circulating activin A levels have been observed in patients with acute coronary syndrome14,15, and in those with diabetes combined with CAD16. Furthermore, elevated activin A levels in patients experiencing acute myocardial infarction were associated with abnormal glucose tolerance17 and infarction size18. Ofstad et al.19 further reported that the activin A level was a predictive factor for cardiovascular events and mortality in patients with type 2 diabetes. However, clinical data on activin A and follistatin levels in patients with prediabetes, and their associations with atherosclerosis, are lacking. This community-based study was conducted to clarify the roles of activin A and follistatin in prediabetes and diabetes, and to explore the relationship between these levels and carotid intima-media thickness (cIMT), a surrogate marker of atherosclerosis.
Results
General participant characteristics
In total, 470 participants (235 men, 235 women) with a mean age of 69 ± 9 years were enrolled. Relative to subjects with normal glucose, those in the prediabetes and diabetes groups were older and had higher body mass indexes (BMIs), waist circumferences, and systolic blood pressure; they had increased fasting plasma glucose and glycated hemoglobin (HbA1c) concentrations and the homeostasis model of assessment–insulin resistance (HOMA-IR) levels. The diabetes group were higher incidence of lipid lowering therapy and lower levels of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), but higher concentrations of triglyceride (TG), and uric acid; they also had lower Mini-Nutritional Assessment (MNA) scores, and hypertension was more common (Table 1).
Elevation of serum activin A levels in prediabetes and diabetes
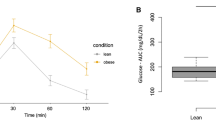
The distributions of activin A and follistatin levels are illustrated in Fig. 1. Patients with prediabetes and diabetes had significantly increased activin A concentrations compared with the normal glycemic group (Table 2). After adjustment of demographic parameters, the activin A levels were still significantly elevated in diabetes and elevated with borderline significance in prediabetes (Table 2). The activin A level was associated with prediabetes and diabetes independently of all confounders in Table 1 by forward stepwise logistic regression analysis (OR 2.68, 95% CI 1.52–4.73, p = 0.001; Table 3), by backward stepwise (OR 1.73, 95% CI 1.02–2.91, p = 0.041; supplementary Table 1A) and by enter mode (OR 3.21, 95% CI 1.03–10.06, p = 0.045; supplementary Table 1B). In the multivariate analysis, an increased activin A level was not an independent risk factor for diabetes by forward stepwise logistic regression analysis (Table 4), backward stepwise (supplementary Table 2A) and by enter mode (supplementary Table 2B).
Box plots of the circulating concentrations of (Panel A) activin A (lower quartile, median, upper quartile: 419.5, 499.0, 608.0 pg/ml) and (Panel B) follistatin (lower quartile, median, upper quartile: 1164.3, 1479.0, 1890.5 pg/ml) in subjects with normal glucose concentrations, prediabetes, and diabetes mellitus.
Patients with diabetes had significantly enhanced follistatin concentrations compared with those with prediabetes and normal glucose levels. The follistatin level did not differ between the prediabetes and normal glycemic groups (Table 2). In the logistic regression model adjusted for other risk factors, the serum follistatin concentration was not an independent risk factor for diabetes (Table 4).
In all subjects, the serum level of activin A was correlated positively with the HOMA-IR value, but the follistatin level was not related to the HOMA-IR value. Spearman (rs) correlation coefficients were: activin A, rs = 0.137 (p = 0.004); follistatin, rs = −0.023 (p = 0.635).
Activin A and follistatin levels correlated with cIMT
The diabetes group showed increased cIMT relative to the normal and prediabetes groups (p = 0.015; Table 2). Spearman’s rank correlation analysis showed that the serum activin A level was correlated positively with cIMT in all cases for which cIMT data were available (n = 457; rs = 0.263, p < 0.001). The correlation between activin A and cIMT was significant in the normal glycemic (n = 208; rs = 0.236, p = 0.001) and prediabetes (n = 165; rs = 0.264, p = 0.001) groups, but no such correlation was found in the diabetes group (n = 84).
The serum follistatin level was also correlated with cIMT in all cases (n = 452; rs = 0.223, p < 0.001). The correlation between follistatin and cIMT was also significant in the normal glycemic (n = 205; rs = 0.221, p = 0.001) and prediabetes (n = 164; rs = 0.271, p < 0.001) groups, but not in the diabetes group (n = 83).
Discussion
In this study, we found that circulating concentrations of activin A and follistatin are elevated in patients with diabetes independent of demographic parameters. We have advanced knowledge in this area by further showing that activin A levels, but not follistatin levels, increased in subjects with prediabetes independent of demographic variables with borderline significance. Moreover, a positive correlation between the serum activin A level and HOMA-IR value, but no association between the peripheral follistatin level and HOMA-IR value, was identified. We also show for the first time that the serum activin A level, as well as the serum follistatin level, was correlated positively with cIMT in subjects with prediabetes and those with normal glucose levels, which suggests a potential role of activin A in atherosclerosis in prediabetic stages.
Few previous clinical studies have explored correlations of activins and follistatin with the clinical status of glucose homeostasis. In concordance with our findings, Hansen et al.20 reported that plasma follistatin is elevated in patients with type 2 diabetes. On the other hand, Wu et al.21 reported no significant difference in circulating concentrations of activins and follistatin among subjects with normal glucose tolerance, impaired fasting glucose or glucose tolerance, and type 2 diabetes. The relatively small sample in that study may explain the non-significant trend toward an increased level of activin A in the type 2 diabetes group21. In the present study, we reported a positive correlation between the serum activin A level and HOMA-IR value. Our results are in line with those of a previous study20, suggesting the lack of a correlation between the peripheral follistatin level and HOMA-IR value. Nevertheless, in young to middle-aged women with polycystic ovary syndrome, the circulating follistatin level was elevated and correlated with the HOMA-IR value22. Interestingly, our findings are similar to those obtained in subjects with nonalcoholic fatty liver disease (NAFLD), ranging from simple steatosis to nonalcoholic steatohepatitis (NASH)23. The plasma activin A levels showed a trend toward progressive increases from the control group to subjects with simple steatosis and NASH23,24. After adjustment for adiposity, the activin A level remained higher in the NASH group than in obese controls23. The follistatin level did not differ between participants with NAFLD and controls23. After adjustment for potential risk parameters, the follistatin level was significantly higher in the NASH group than in the simple steatosis subgroup of the NAFLD group23. Based on Yndestad et al.’s24 previous study, Polyzos et al.23 speculated that activin A production increases with NAFLD progression, initially limiting steatosis, but then contributing to the pathogenesis of NASH. NAFLD, a spectrum of diseases ranging from simple steatosis to NASH, is frequently associated with obesity, dyslipidemia, and insulin resistance in a metabolic syndrome24. We thus speculate that the complex roles of activin A and follistatin in the development of prediabetes and diabetes resemble those reported for NAFLD. The upregulation of activin A may initially limit the abnormality of glucose homeostasis, while follistatin levels remain the same as in controls, allowing activin A to exert protective effects in the prediabetic stage. However, when the disease progresses, increased activin A induces follistatin elevation to self-limit detrimental effects in the diabetic stage. Further studies are needed to verify this speculation.
Additionally, we extended previous findings showing that elevated circulating activin A levels are associated with cIMT in subjects with prediabetes and those with normal glucose levels. cIMT has been used as a surrogate marker not only of carotid atherosclerosis, but also of coronary atherosclerosis25. The cIMT has been reported to be greater in subjects with abnormal glucose homeostasis, including impaired glucose tolerance, impaired fasting glucose, and diabetes26,27. The cIMT was also associated positively with the incidence of cardiovascular events in individuals with diabetes28. Several possible rationales could explain the association between activin A and atherosclerosis. In addition to above-mentioned effects of activin A in the pathogenesis of NAFLD and glucose homeostasis, some experimental cardiovascular studies have revealed potential roles of activin A in inflammation and ischemia/reperfusion injury14,17,29,30,31. Association of activin A and atherosclerosis has already been demonstrated in human vascular tissue specimens of atherosclerosis32. Increasing evidence suggests that activin A exerts an anti-inflammatory effect on peripheral mononuclear cells in patients with angina14. Overexpression of activin A with an adenoviral vector or treatment with recombinant activin A protein protected cultured neonatal rat ventricular myocytes from ischemia/reperfusion injury29. However, other studies have yielded contrasting findings30,31. In a mouse cardiomyocyte ischemia/reperfusion model, activin A damaged cardiomyocytes independently of increased reactive oxygen species concentrations30. Activin A was also shown to attenuate cardiomyocyte contractile function in adult rat cardiomyocyte cultures31. One could reasonably speculate that activin A plays similar roles in the development of NAFLD, diabetes, and atherosclerosis.
Community-dwelling adults aged ≥ 50 years were enrolled in this study using random sampling of household registries in a rural area of Taiwan. We recorded several baseline parameters including MNA scores for the future longitudinal analysis. The MNA score not less than 24 identified a good nutritional status33. This population has a low prevalence of established CAD history, a good nutritional status, and acceptable lipid profiles and blood pressure range. Therefore, this study might have been underpowered for the detection of negligible differences in cIMT values between subjects with prediabetes and with normal glucose levels. However, the lack of correlation between cIMT and activin A or follistatin in subjects with diabetes requires explanation. The incidence of lipid-reducing therapy was higher and the LDL level was lower in our diabetes group than in the normal glycemic and prediabetes groups. LDL is the most important risk factor for atherosclerosis, and lipid-reducing therapy can decrease the incidence of cardiovascular complications3,34. The high prevalence of such treatment in the diabetes group likely had a major influence on the correlation between activin A and cIMT in this cross-sectional study. Besides, phenomena of competing risk would be of relevance here. The diabetic population has in general higher levels of measured and unmeasured risk factors promoting cardiovascular disease. Thus, the competing risk of potential unmeasured risk factors may diminish the relative significance of inflammation, represented by activin A and follistatin, in promoting the atherosclerosis. Another possible explanation is the relatively small size of the diabetes group. Our speculations must be interpreted with caution, and further studies are warranted to clarify the underlying mechanisms.
This study has several limitations. A major limitation is the differences among groups in key variables, including age, BMI, and waist circumference. Although we used multivariate analysis to adjust for such differences, bias may still exist. Another limitation is that the study’s cross-sectional design did not permit the exploration of causal relationships between glucose homeostasis and serum activin A or follistatin levels. Activin A and follistatin could be induced at variable sites and might be correlated with multiple pathophysiological changes at the cellular level (as autocrine or paracrine), and the serum concentrations measured in this study might not accurately reflect intra/intercellular concentrations35. This study explored the relationship between cIMT and activin A, as well as follistatin, in different glucose homeostasis statuses. However, cIMT is a surrogate atherosclerotic marker and not a hard endpoint. In addition, lack of association of cIMT and activin A in diabetic subjects was another limitation of this study.
In conclusion, circulating activin A levels, but not follistatin levels, increased in subjects with prediabetes independent of demographic parameters with borderline significance. Activin A and follistatin levels were elevated in diabetic patients, but only elevated activin A was an independent risk factor for prediabetes and diabetes after adjustment for the available confounders. Furthermore, serum activin A and follistatin levels were correlated positively with cIMT in this study. However, this correlation was not significant in the diabetic subgroup. Future studies are needed to confirm and expand these findings, and studies exploring the underlying mechanisms are also warranted.
Methods
Study design and population
We analyzed baseline data from the I-Lan Longitudinal Aging Study and General Assessment36. This study enrolled community-dwelling adults aged 50 years and older by random sampling of household registries maintained by the county government in Yuanshan Township of I-Lan County, Taiwan. The whole study was approved by the Institutional Review Board of the National Yang Ming University36. All participants provided written informed consent. In addition, all methods were performed in accordance with relevant guidelines and regulation.
Medical history and physical examination data
Basic medical histories of participants, including underlying disease, recent medication use, and personal histories (including factors linked to cardiovascular disease, such as smoking and alcohol consumption) were obtained through personal interviews and recorded medical notes. Participants’ weight (kilogram), height (meter), and BMI, calculated by dividing weight by height squared, were recorded. Insulin resistance was quantified with HOMA-IR using the following formula: HOMA-IR = glucose (mmol/l) × insulin (uU/ml)/22.5. Brachial blood pressure was measured with a mercury sphygmomanometer after subjects had rested for at least 15 min.
Classification of normal glucose, prediabetes, and diabetes
Subjects were classified as having prediabetes based on impaired fasting glucose or elevated serum HbA1c concentrations. Impaired fasting glucose was defined by glucose levels of 100–125 mg/dl, according to the 1997 and 2003 reports of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus37,38. HbA1c concentrations of 5.7–6.4% were used to define prediabetes, according to a previous systematic review39. Participants with fasting plasma glucose levels ≥ 126 mg/dl or HBA1c concentrations ≥ 6.5% were assigned to the diabetes group37. Subjects who did not meet the criteria for prediabetes or diabetes were classified as having normal glucose levels.
cIMT assessment
The cIMT was measured using an ultrasound device (LOGIQ 400 PRO; GE, Cleveland, OH, USA) equipped with a high-resolution broad-width linear array transducer. The same technician performed all examinations, measuring arteries including the proximal to distal parts of the bilateral common carotid artery, its bifurcation, and the internal and external carotid arteries. The cIMT was measured on the far wall of the common carotid artery on longitudinal views. Mean cIMT was calculated by averaging right and left values36.
Laboratory examinations
Blood samples were collected from seated patients after a 10-h overnight fast and examined to determine HbA1c (%), fasting plasma glucose (mg/dl), TC (mg/dl), HDL-C (mg/dl), LDL-C (mg/dl), TG (mg/dl), uric acid (mg/dl), activin A (pg/ml), and follistatin (pg/ml) concentrations. Serum concentrations of glucose, TC, TG, LDL-C, HDL-C, and insulin were determined using an automatic analyzer (ADVIA 1800; Siemens, Malvern, PA, USA). Serum insulin-like growth factor-1 concentrations were measured by enzyme-linked immunosorbent assay (ELISA) (Ray Biotech, Norcross, GA, USA). The whole-blood HbA1c concentration was measured using an enzymatic method with a high-performance liquid chromatography analyzer (G8; Tosoh Bioscience, Inc., San Francisco, CA, USA). A single voided morning urine sample was used to measure the urinary albumin-to-creatinine ratio40. Activin A and follistatin concentrations were measured by ELISA (Quantikine human immunoassays; R&D Systems, Minneapolis, MN, USA). All serum samples were tested in duplicate, and coefficients of variation of duplicate samples were less than 20%.
Nutritional status assessment
Trained interviewers assessed participants’ functional nutritional status using the MNA, which is used globally to rapidly evaluate nutritional status in elderly individuals. The MNA covers multiple factors, including anthropometric measures (weight, height, and weight loss), global assessment (six questions related to lifestyle, medication, and mobility), dietary assessment (eight questions related to the number of meals, food and fluid intake, and autonomy of feeding), and subjective assessment (self-perceived health and nutrition)33.
Statistical analysis
The normality of data was assessed using the Shapiro–Wilk test. All continuous descriptive variables are reported as means ± standard deviations except non-normally distributed data (median ± interquartile range), and categorical variables are expressed as numbers (percentages). Continuous variables were compared among the three groups using parametric (analysis of variance and post-hoc analysis with least significant difference method) or non-parametric (Kruskal–Wallis with pairwise comparisons) tests. Subgroup comparisons of categorical variables were performed using the chi-squared test. We added p value in cell as significant difference existed by chi-squared test. Analysis of covariance was used with adjustment for potential covariates. Correlations of serum activin A and follistatin concentrations with variables in the study groups were calculated using Spearman’s rank correlation. To identify potential risk factors for prediabetes or diabetes, variables with univariate all were included in a forward stepwise logistic regression analysis to calculate odds ratios (ORs) and 95% confidence intervals (CIs). Backward stepwise and the “enter” mode of logistic regression were also performed as supplementary data. Statistical analyses were performed using SPSS version 23.0 (SPSS Inc., Chicago, IL, USA). P values < 0.05 were considered to be statistically significant.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Laakso, M. Cardiovascular disease in type 2 diabetes: challenge for treatment and prevention. J. Intern. Med. 249, 225–235 (2001).
PyoÈraÈlaÈ, K., Laakso, M. & Uusitupa, M. Diabetes and atherosclerosis: an epidemiologic view. Diabetes Metab. Rev. 3, 463–524 (1987).
Mahmood, S. S., Levy, D., Vasan, R. S. & Wang, T. J. The Framingham Heart Study and the epidemiology of cardiovascular diseases: A historical perspective. Lancet 383, 999–1008 (2014).
Weyer, C., Bogardus, C., Mott, D. M. & Pratley, R. E. The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J. Clin. Invest. 104, 787–794 (1999).
Fruchart, J. C. et al. Residual risk reduction initiative (R3i). Residual macrovascular risk in 2013: what have we learned? Cardiovasc. Diabetol. 13, 26 (2014).
Risbridger, G. P., Schmitt, J. F. & Robertson, D. M. Activins and inhibins in endocrine and other tumors. Endocr. Rev. 22, 836–858 (2001).
Florio, P. et al. Activin A stimulates insulin secretion in cultured human pancreatic islets. J. Endocrinol. Invest. 23, 231–234 (2000).
Totsuka, Y., Tabuchi, M., Kojima, I., Shibai, H. & Ogata, E. A novel action of activin A: stimulation of insulin secretion in rat pancreatic islets. Biochem. Biophys. Res. Commun. 156, 335–339 (1988).
Ungerleider, N. A., Bonomi, L. M., Brown, M. L. & Schneyer, A. L. Increased activin bioavailability enhances hepatic insulin sensitivity while inducing hepatic steatosis in male mice. Endocrinology 154, 2025–2033 (2013).
Hansen, J. S. & Plomgaard, P. Circulating follistatin in relation to energy metabolism. Mol. Cell Endocrinol. 433, 87–93 (2016).
de Kretser, D. M., O’Hehir, R. E., Hardy, C. L. & Hedger, M. P. The roles of activin A and its binding protein, follistatin, in inflammation and tissue repair. Mol. Cell Endocrinol. 359, 101–106 (2012).
Hansen, J. S. et al. Circulating Follistatin Is Liver-Derived and Regulated by the Glucagon-to-Insulin Ratio. J. Clin. Endocrinol. Metab. 101, 550–560 (2016).
Phillips, D. J., de Kretser, D. M. & Hedger, M. P. Activin and related proteins in inflammation: not just interested bystanders. Cytokine Growth Factor Rev. 20, 153–164 (2009).
Smith, C. et al. Potential anti-inflammatory role of activin A in acute coronary syndromes. J. Am. Coll. Cardiol. 44, 369–375 (2004).
Anastasilakis, A. D. et al. Circulating irisin levels are lower in patients with either stable coronary artery disease (CAD) or myocardial infarction (MI) versus healthy controls, whereas follistatin and activin A levels are higher and can discriminate MI from CAD with similar to CK-MB accuracy. Metabolism 73, 1–8 (2017).
Ueland, T. et al. Activin A and cardiovascular disease in type 2 diabetes mellitus. Diab. Vasc. Dis. Res. 9, 234–237 (2012).
Andersen, G. Ø. et al. Activin A levels are associated with abnormal glucose regulation in patients with myocardial infarction potential counteracting effects of activin A on inflammation. Diabetes 60, 1544–1551 (2011).
Miyoshi, T. et al. Relationship between activin A level and infarct size in patients with acute myocardial infarction undergoing successful primary coronary intervention. Clin. Chim. Acta 401, 3–7 (2009).
Ofstad, A. P. et al. Interleukin-6 and activin A are independently associated with cardiovascular events and mortality in type 2 diabetes: the prospective Asker and Bærum Cardiovascular Diabetes (ABCD) cohort study. Cardiovasc. Diabetol. 12, 126 (2013).
Hansen, J. et al. Plasma follistatin is elevated in patients with type 2 diabetes: relationship to hyperglycemia, hyperinsulinemia, and systemic low-grade inflammation. Diabetes Metab. Res. Rev. 29, 463–472 (2013).
Wu, H. et al. Correlation between blood activin levels and clinical parameters of type 2 diabetes. Exp. Diabetes Res. 2012, 410579 (2012).
Teede, H., Ng, S., Hedger, M. & Moran, L. Follistatin and activins in polycystic ovary syndrome: relationship to metabolic and hormonal markers. Metabolism. 62, 1394–1400 (2013).
Polyzos, S. A., Kountouras, J., Anastasilakis, A. D., Triantafyllou, G. A. & Mantzoros, C. S. Activin A and follistatin in patients with nonalcoholic fatty liver disease. Metabolism 65, 1550–1558 (2016).
Yndestad, A. et al. A complex role of activin A in non-alcoholic fatty liver disease. Am. J. Gastroenterol. 104, 2196–2205 (2009).
Lorenz, M. W., Markus, H. S., Bots, M. L., Rosvall, M. & Sitzer, M. Prediction of clinical cardiovascular events with carotid Intima-media thickness. A systemic review and meta-analysis. Circulation 115, 459–467 (2007).
Brohall, G., Oden, A. & Fagerberg, B. Carotid artery intima-media thickness in patients with Type-2 diabetes mellitus and impaired glucose tolerance: a systematic review. Diabet. Med. 23, 609–616 (2006).
Einarson, T. R., Hunchuck, J. & Hemels, M. Relationship between blood glucose and carotid intima media thickness: A meta-analysis. Cardiovasc. Diabetol. 9, 37 (2010).
Yamasaki, Y. et al. Carotid intima-media thickness in Japanese type 2 diabetic subjects: predictors of progression and relationship with incident coronary heart disease. Diabetes Care 23, 1310–1315 (2000).
Oshima, Y. et al. Activin A and follistatin-like 3 determine the susceptibility of heart to ischemic injury. Circulation 120, 1606–1615 (2009).
Chen, Y. et al. Regulation and actions of activin A and follistatin in myocardial ischaemia-reperfusion injury. Cytokine 69, 255–262 (2014).
Greulich, S. et al. Secretory products from epicardial adipose tissue of patients with type 2 diabetes mellitus induce cardiomyocyte dysfunction. Circulation 126, 2324–2334 (2012).
Engelse, M. A. et al. Human activin-A is expressed in the atherosclerotic lesion and promotes the contractile phenotype of smooth muscle cells. Circ. Res. 85, 931–939 (1999).
Vellas, B. et al. The mini nutritional assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15, 116–122 (1999).
Mora, S. et al. Statins for the primary prevention of cardiovascular events in women with elevated high-sensitivity C-reactive protein or dyslipidemia. Results from the Justification for the Use of Statins in Prevention: An intervention trial evaluating rosuvastatin (JUPITER) and meta-analysis of women from primary prevention trials. Circulation 121, 1069–1077 (2010).
Eijken, M. et al. The activin A-follistatin system: potent regulator of human extracellular matrix mineralization. FASEB J. 21, 2949–2960 (2007).
Liu, L. K. et al. Sarcopenia, and its association with cardiometabolic and functional characteristics in Taiwan: results from I-Lan Longitudinal Aging Study. Geriatr. Gerontol. Int. 14(Suppl 1), 36–45 (2014).
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 20, 1183–1197 (1997).
Genuth, S. et al. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26, 3160–3167 (2003).
Zhang, X. et al. A1C level and future risk of diabetes: a systematic review. Diabetes Care 33, 1665–73 (2010).
Chang, C. C. et al. Association between low-grade albuminuria and frailty among community-dwelling middle-aged and older people: a cross-sectional analysis from I-Lan Longitudinal Aging Study. Sci. Rep. 6, 39434, https://doi.org/10.1038/srep39434 (2016).
Acknowledgements
This study was supported, in part, by research grants from the Ministry of Science and Technology of Taiwan (MOST 104–2314-B-075-047, MOST 106-2314-B-010-033-MY3, MOST 106-2314-B-075-078-MY3), the Novel Bioengineering and Technological Approaches to Solve Two Major Health Problems in Taiwan sponsored by the Taiwan Ministry of Science and Technology Academic Excellence Program (MOST 106-2633-B-009-001), the Ministry of Health and Welfare (MOHW106-TDU-B-211-113001), and Taipei Veterans General Hospital (V105C-207, V106C-045). These funding agencies had no influence on the study design, data collection or analysis, or decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Study concept and design: C.-S.K., Y.-W.L., C.-Y.H., P.-H.H. and S.-J.L.; acquisition of data: L.-K.L. and L.-K.C.; analysis and interpretation of data: C.-Y.H., C.-C.C. and R.-H.C.; drafting of the manuscript: C.-S.K., Y.-W.L., C.-C.C., R.-H.C., L.-K.L. and P.-H.H.; statistical analysis: C.-Y.H., C.-C.C. and R.-H.C.; administrative, technical, or material support: L.-K.C., P.-H.H., J.-W.C. and S.-J.L.; critical revision: C.-S.K., P.-H.H. and S.-J.L.; study supervision: L.-K.C. S.-J.L. and P.-H.H. The Corresponding Authors have the right to grant on behalf of all authors and do grant on behalf of all authors a worldwide license to the Publisher and its licensees in perpetuity.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kuo, CS., Lu, YW., Hsu, CY. et al. Increased activin A levels in prediabetes and association with carotid intima-media thickness: a cross-sectional analysis from I-Lan Longitudinal Aging Study. Sci Rep 8, 9957 (2018). https://doi.org/10.1038/s41598-018-27795-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-27795-2
This article is cited by
-
Role of circulating molecules in age-related cardiovascular and metabolic disorders
Inflammation and Regeneration (2022)
-
The association between serum activin A levels and albuminuria among community-dwelling middle-aged and older adults in Taiwan
Scientific Reports (2021)
-
Circadian rhythm of activin A and related parameters of mineral metabolism in normal and uremic rats
Pflügers Archiv - European Journal of Physiology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.