Abstract
This study aimed to assess changes in pupil size, uncorrected visual acuity, refraction, and the direct and consensual light reflexes after instillation of brimonidine 0.1% in healthy subjects. The investigation comprised 46 eyes of 23 healthy subjects with no eye diseases in whom brimonidine 0.1% was instilled in the right eye. Pupil size was measured quantitatively under photopic and scotopic conditions, uncorrected visual acuity, refraction, and direct and consensual light reflexes before and at 1, 6, and 24 h after instillation. We found No significant change was found in refraction or uncorrected visual acuity (P = 0.999 and P = 0.998, respectively). A significant reduction in pupil size was observed under scotopic conditions at 1 h and 6 h after instillation (P = 0.007 and P = 0.005, respectively). The rate of pupil contraction and constriction speed measured by light reflexes were significantly increased at 1 h and 6 h after instillation (P = 0.021 and P = 0.033, respectively). Brimonidine 0.1% induced a significant reduction in pupil size under scotopic conditions without a significant change in refraction or visual acuity due to suppression of the sympathetic nervous system.
Similar content being viewed by others
Introduction
After refractive surgery, patients may experience problems with nighttime glare and halos1. Currently, concerns exist regarding these issues, which deteriorate visual performance and subsequent patient satisfaction. A reduction in night vision occurs due to increases in the high-order aberrations that occur with large pupils; however, this may be improved by miosis2,3. Nighttime glare and halos have been reported to improve with miosis from pilocarpine hydrochloride. However, pilocarpine has been reported to cause excessive miosis, increased lens thickness, and adjustable tension from increases in transient myopia4.
Brimonidine, a selective alpha-2 adrenergic receptor agonist, is used in the treatment of glaucoma and ocular hypertension. Its reduces intraocular pressure by reducing aqueous humor production and increasing uveoscleral outflow5,6. Brimonidine 0.2% peak ocular hypotensive effect occurs 2 h after instillation7, and there was no significant difference from timolol maleate at the maximum effect8. Therefore, it can be expected to provide effective intraocular pressure reduction in combination with other ophthalmic solutions. Brimonidine has been reported to have neuroprotective effect9,10. Krupin et al.11 reported that low-pressure glaucoma patients treated with brimonidine 0.2% are less likely to experience field progression. Brimonidine tartrate 0.2% and 0.15% ophthalmic solution has been reported to be significantly miotic under scotopic conditions12,13, and effective in reducing glare and halos after refractive surgery14,15. The pupil size contracts under scotopic conditions is that brimonidine stimulates prejunctional alpha-2 agonist receptor and reduces norepinephrine release in the synapse. Therefore, brimonidine inhibits pupil dilation under scotopic vision. Although previous studies have investigated pupil size, there have been no reports investigating a detailed description of direct and consensual light reflexes. The aim of this study was to assess changes in pupil size, uncorrected visual acuity, corrected visual acuity, subjective refraction, objective refraction, and the direct and consensual light reflexes after instillation of brimonidine 0.1% in the eyes of healthy subjects.
Results
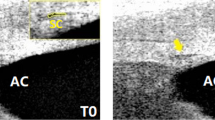
All of the results were examined at 1, 6, and 24 h after instillation compared with pre-instillation. We found no significant change in pupil size in the brimonidine-treated eyes under photopic conditions, but a significant reduction in pupil size under scotopic conditions at 1 h (5.4 ± 0.8 mm) and 6 h (5.4 ± 0.8 mm) after instillation (P = 0.007 and P = 0.005, respectively) compared to before instillation of brimonidine (6.0 ± 0.6 mm) (Fig. 1, Table 1). We found no significant change in pupil size in the brimonidine-treated eyes under scotopic conditions at 24 h (5.7 ± 0.7 mm) after instillation (P = 0.144). The pupil size in the control eyes was not significantly changed under photopic or scotopic conditions (Fig. 1). We found no significant change in uncorrected visual acuity, subjective refraction, or objective refraction (Table 2). The logarithm of the minimal angle of resolution (logMAR) of corrected visual acuity was −0.18 in all cases before and after instillation.
Regarding the results of the direct light reflex in the brimonidine-treated eyes, initial pupil size was significantly reduced at 1 h (5.3 ± 0.9 mm) and 6 h (5.4 ± 0.9 mm) after instillation (P = 0.001 and P = 0.002, respectively) compared to before instillation of brimonidine (6.3 ± 0.7 mm) (Table 3). Minimum pupil size after light stimulation was also significantly reduced at 1 h (3.3 ± 0.7 mm) and 6 h (3.4 ± 0.7 mm) after instillation (P < 0.001 and P < 0.001, respectively) compared to before instillation of brimonidine (4.2 ± 0.7 mm). Rate of pupil contraction [(Initial pupil size − minimum pupil size after light stimulation)/(initial pupil size)] was significantly increased at 1 h (0.37 ± 0.06) and 6 h (0.37 ± 0.04) after instillation (P = 0.020 and P = 0.037, respectively) compared to before instillation of brimonidine (0.33 ± 0.07). Time until the pupil size was minimized was significantly reduced at 1 h (863.8 ± 169.8 ms) and 6 h (871.7 ± 200.5 ms) after instillation (P = 0.010 and P = 0.015, respectively) compared to before instillation of brimonidine (1018.8 ± 141.4 ms). Time when the pupil size had been restored to 63% was not observed to change significantly at any time point. Maximum constriction speed was significantly increased at 1 h (5.6 ± 0.9 mm2/s) and 6 h (5.7 ± 0.8 mm2/s) after instillation (P = 0.027 and P = 0.016, respectively) compared to before instillation of brimonidine (5.0 ± 0.8 mm2/s). Maximum dilatation speed did not change significantly at any time point. No significant change in any parameter from baseline was observed at 24 h after instillation. The results of the indirect reaction in the brimonidine-treated eyes were similar to the results of the direct reaction (Table 4). No parameter was observed to change significantly in the control eyes at any time point. In addition, no side effects were observed in any case.
Discussion
We found that pupil size was significantly reduced under scotopic conditions at 1 h and 6 h after instillation (0.64 mm and 0.67 mm, respectively). The rate of pupil contraction and maximum constriction speed were significantly increased at 1 h and 6 h after instillation. McDonald et al.12 found no significant change in pupil size under photopic conditions; however, 100% (16 eyes) exhibited significant miosis after 30 min, and 81.3% (13 eyes) miosis at 6 h under scotopic conditions after brimonidine 0.2% instillation in healthy subjects. The results reported by McDonald et al. did not differ from those in the present study in that pupil size before instillation under photopic conditions was 2.9 mm, and 2.8 mm 6 h after instillation. However, pupil size under scotopic conditions was 5.8 mm before instillation and 4.4 mm 6 h after instillation, which is miotic compared with our study. One of possibility is that the study by McDonald et al. used a 0.2% concentration of eye drops compared with 0.1% in our study. Kesler et al.16 found significant miosis after brimonidine 0.2% instillation in healthy subjects up to 4 h under photopic conditions and up to 6 h under scotopic conditions. The authors reported a pupil size of 4.81 mm before instillation under photopic conditions and 3.80 mm 4 h after instillation, which is significantly miotic. Because the photopic condition is defined at 5 cd/m2, we believe that the pupil size was larger than that in our study, and significantly miotic. Shemesh et al.13 found no significant change in pupil size under photopic conditions; however, a significant reduction in pupil size under scotopic conditions up to 6 h after brimonidine 0.1% instillation was found in healthy subjects. Because Shemesh et al. used 5 cd/m2 under photopic conditions, the pupil size before instillation was as large as 4.98 mm from this study. However, the pupil size 6 h after instillation was 4.64 mm, which is not considered to be a significant difference because 0.1% brimonidine was used. Therefore, pupil size 6 h after instillation under scotopic conditions was 5.38 mm, which is similar to the result in the present study. Thordsen et al.17 reported measurements of pupil size after 0.15% brimonidine was instilled in healthy subjects. Under scotopic conditions, pupil size was decreased by ≥1.0 mm in 100% and 60% of eyes at 30 min and 6 h, respectively. The instruments used to measure pupil size in previous studies were types of closed-view pupilometers. In the present study, measurements were performed with both eyes open because this is considered to provide a more accurate measurement of pupil size. In addition, the past study reported measurements up to 6 h after instillation. In our study, it was measured for 24 h after instillation, with no significant difference from 24 h before instillation found.
Direct and consensual light reflexes under scotopic conditions were compared with reports of pupil diameter under scotopic conditions because of miosis 6 h after instillation and were considered to be similar. Parameters of light reflexes are related to miosis and those related to mydriasis. Parameters related to miosis include initial pupil size, minimum pupil size after light stimulation, rate of pupil contraction, time until pupil size is minimized, and maximum constriction speed. Parameters related to mydriasis include time to pupil size restored to 63%, and maximum dilatation speed. Parameters related to miosis in pupils significantly miotic at 1 and 6 h after instillation include increased rates of pupil contraction and maximum constriction speed. In contrast, no significant difference was observed in the two parameters related to mydriasis after instillation, and brimonidine did not affect mydriasis. In addition, this result is the same for consensual light reflexes, and it is understood that brimonidine also similarly acts through an indirect reaction route.
There were at least two limitations to this study, the first of which was the relatively small sample size. A larger number of healthy subjects is required to confirm our preliminary findings. Second, this study was performed in an unblinded fashion. A double-blinded study may be more appropriate to confirm the veracity of the results.
Pilocarpine hydrochloride, a parasympathetic stimulant, has been reported to increase myopia and the perception of darkness due to excessive miosis; it is considered unsuitable to reduce night vision glare and halos after refractive surgery. Pupil size was significantly reduced under scotopic conditions at 1 h after instillation of brimonidine. When used for nighttime glare and halos, we believe that it is effective once per day when instilled in the evening. Brimonidine has slight miotic properties under scotopic conditions by suppressing the sympathetic nervous system. There was no significant change in pupil size under photopic conditions; therefore, the pupil was also considered to be a factor that did not significantly influence uncorrected visual acuity. Brimonidine 0.1% induced a significant reduction in pupil size without a significant change in refraction or visual acuity under scotopic conditions. Therefore, it may be effective for the reduction of glare and halos after refractive surgery.
Materials and Methods
This study comprised 46 eyes of 23 healthy subjects (13 men, 10 women; mean age 31.4 ± 7.3 years) with no eye diseases other than refractive error. Brimonidine 0.1% (Alphagan®, Senju Pharmaceutical Co., Ltd., Osaka, Japan) was instilled in the right eye and artificial tears were instilled in the left; we quantitatively measured pupil size under photopic and scotopic conditions, uncorrected visual acuity, corrected visual acuity, subjective refraction, objective refraction, and the direct and consensual light reflexes before and at 1, 6, and 24 h after instillation. In all cases, the time measurements were unified: measurements were made at 8:30 AM, instillation was performed at 9:00 AM, and outcomes were measured at 1, 6, and 24 h after instillation. The subjects were instructed to refrain from smoking and ingesting caffeine, since these can affect the pupil. Pupil size was measured with both eyes open using an electronic pupil meter (FP-10000 II; T.M.I. Company, Saitama, Japan) and was quantitatively measured under photopic and scotopic conditions (130 cd/m2 and 0.1 cd/m2, respectively). Objective refraction was measured using a combination system including an auto refractometer, auto keratometer, non-contact tonometer, and non-contact pachymeter (Auto Ref Kerato Meter; TONOREF II®; NIDEK CO., LTD., Aichi, Japan). The direct and consensual light reflexes was measured with an infrared iriscorder (Iriscorder Dual C-10641, Hamamatsu Photonics Co., Ltd., Shizuoka, Japan); it measured the direct and indirect reactions of both eyes to red light stimulation (635 nm) after scotopic adaptation for 15 min.
The direct and consensual light reflexes parameters were initial pupil size, minimum pupil size after light stimulation, rate of pupil contraction, time until the pupil size was minimized, time when the pupil size had been restored to 63%, maximum constriction speed, and maximum dilatation speed. The instilled right eyes were defined as the brimonidine-treated eyes and the left eyes were defined as the control eyes. The study was approved by the Institutional Review Board at Kitasato University School of Medicine, and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects. All statistical analyses were performed off-line using spreadsheet software (Excel, Microsoft Corporation, Redmond, WA, USA). Because all data were normally distributed, all statistical analysis was performed using the ANOVA test (Dunnett’s test); p < 0.05 was considered to be statistically significant.
References
Fan-Paul, N. I., Li, J., Miller, J. S. & Florakis, G. J. Night vision disturbances after corneal refractive surgery. Surv Ophthalmol. 47, 533–46 (2002).
Kamiya, K., Igarashi, A., Shimizu, K., Matsumura, K. & Komatsu, M. Visual performance after posterior chamber phakic intraocular lens implantation and wavefront-guided laser in situ keratomileusis for low to moderate myopia. Am J Ophthalmol. 153, 1178–86. e1 (2012).
Igarashi, A., Kamiya, K., Shimizu, K. & Komatsu, M. Visual performance after implantable collamer lens implantation and wavefront-guided laser in situ keratomileusis for high myopia. Am J Ophthalmol. 148, 164–70 (2009).
Webster, A. R., Luff, A. J., Canning, C. R. & Elkington, A. R. The effect of pilocarpine on the glaucomatous visual field. Br J Ophthalmol. 77, 721–5 (1993).
Matsuura, K., Terasaka, Y. & Sasaki, S. Brimonidine as adjunctive therapy in uncontrolled patients using combination of prostaglandin, β-blocker and carbonic anhydrase inhibitor. Atarashii Ganka. 31, 1059–62 (2014).
Mataki, N., Saito, H. & Iwase, A. Adjunctive effect on intraocular pressure and ocular and systemic side effects of topical 0.1% brimonidine in open-angle glaucoma. Atarashii Ganka. 31, 1063–66 (2014).
LeBlanc, R. P. Twelve-month results of an ongoing randomized trial comparing brimonidine tartrate 0.2% and timolol 0.5% given twice daily in patients with glaucoma or ocular hypertension. Brimonidine Study Group 2. Ophthalmology. 105, 1960–7 (1998).
Van, der, Valk, R, et al. Intraocular pressure-lowering effects of all commonly used glaucoma drugs: a meta-analysis of randomized clinical trials. Ophthalmology. 112, 1177–85 (2005).
Ahmed, F. A., Hegazy, K., Chaudhary, P. & Sharma, S. C. Neuroprotective effect of alpha(2) agonist (brimonidine) on adult rat retinal ganglion cells after increased intraocular pressure. Brain Res. 913, 133–9 (2001).
Vidal-Sanz, M. et al. Brimonidine’s neuroprotective effects against transient ischaemia-induced retinal ganglion cell death. Eur J Ophthalmol. 11, 36–40 (2001).
Krupin, T., Liebmann, J. M., Greenfield, D. S., Ritch, R. & Gardiner, S. Low-Pressure Glaucoma Study Group. A randomized trial of brimonidine versus timolol in preserving visual function: results from the low-pressure glaucoma treatment study. Am J Ophthalmol. 151, 671–81 (2011).
McDonald, J. E. II., El-Moatassem, K. A. M. & Decker, B. B. Effect of brimonidine tartrate ophthalmic solution 0.2% on pupil size in normal eyes under different luminance conditions. J Cataract Refract Surg. 27, 560–4 (2001).
Shemesh, G., Moisseiev, E., Lazar, M. & Kesler, A. Effect of brimonidine tartrate 0.10% ophthalmic solution on pupil diameter. J Cataract Refract Surg. 37, 486–9 (2011).
Lee, J. H., You, Y. S., Choe, C. M. & Lee, E. S. Efficacy of brimonidine tartrate 0.2% ophthalmic solution in reducing halos after laser in situ keratomileusis. J Cataract Refract Surg. 34, 963–7 (2008).
Edwards, J. D. et al. Effect of brimonidine tartrate 0.15% on night-vision difficulty and contrast testing after refractive surgery. J Cataract Refract Surg. 34, 1538–41 (2008).
Kesler, A., Shemesh, G., Rothkoff, L. & Lazar, M. Effect of brimonidine tartrate 0.2% ophthalmic solution on pupil size. J Cataract Refract Surg. 30, 1707–10 (2004).
Thordsen, J. E., Bower, K. S., Warren, B. B. & Stutzman, R. Miotic effect of brimonidine tartrate 0.15% ophthalmic solution in normal eyes. J Cataract Refract Surg. 30, 1702–06 (2004).
Author information
Authors and Affiliations
Contributions
The authors were involved in the design and conduct of the study (S.K., K.S., K.K., H.I.); collection, management, analysis, and interpretation of data (S.K., K.K., A.I.); and preparation, review, and approval of the manuscript (S.K., K.S., K.K., H.I., A.I.).
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kato, C.O., Shimizu, K., Kamiya, K. et al. Effects of brimonidine tartrate 0.1% ophthalmic solution on the pupil, refraction, and light reflex. Sci Rep 8, 9003 (2018). https://doi.org/10.1038/s41598-018-27436-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-27436-8
This article is cited by
-
Topical brimonidine induced acute uveal effusion in a patient with nanophthalmos: a case report
BMC Ophthalmology (2023)
-
Brimonidine eye drops reveal diminished sympathetic pupillary tone in comatose patients with brain injury
Acta Neurochirurgica (2023)
-
Effect of brimonidine tartrate 0.15% on scotopic pupil size and upper eyelid position: controlled trial
Eye (2021)
-
Effect of over-the-counter brimonidine tartrate 0.025% ophthalmic solution on pupil size in healthy adults
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.