Abstract
Fast-track surgery (FTS), which includes a series of evidence-based adjustments, is expected to reduce complications, relieve surgical stress reaction, accelerate recovery, and shorten hospitalization, as well as improve safety. The aim of this study was to critically evaluate the safety and effectiveness of FTS in Chinese prostate cancer (Pca) patients who underwent robot-assisted laparoscopic prostatectomy (RALP). A retrospective analysis was performed on 73 consecutive Chinese Pca patients who underwent RALP and who were divided into two groups: conventional surgery (CS) and FTS. Preoperative clinical data, intraoperative characteristics, postoperative outcomes and incidence of complications were compared between the two groups. No significant differences in preoperative parameters were observed between the two groups. Compared with the CS group, the FTS group showed a significantly shorter time to first flatus, time to regular diet, postoperative hospitalization time, lower incidence of complications, and lower reactions of postoperative stress and pain. Our study demonstrates that FTS is feasible and safe for Chinese Pca patients undergoing RALP and that it accelerates recovery, attenuates surgical stress response, and reduces morbidity compared to CS.
Similar content being viewed by others
Introduction
Prostate cancer (Pca) is the most common cancer of the genitourinary tract in men1. Radical prostatectomy (RP) is considered an important treatment option for patients with low-risk and intermediate-risk localized Pca and a life expectancy no less than 10 years. With the widespread application and increasing experience of robot-assisted laparoscopic techniques, robot-assisted laparoscopic radical prostatectomy (RALP) has become an increasingly popular minimally invasive choice for managing localized Pca among urologists. Compared with laparoscopic and open RP, a series of randomized trials and comparative studies have provided sufficient evidence about oncologic and functional results to suggest that RALP is a safe and well-tolerated intervention for the treatment of localized Pca2,3,4.
Fast-track surgery (FTS), also defined as enhanced recovery after surgery, was first performed by Kehlet5. The FTS protocol includes a variety of techniques with evidence-based interventions, such as surgical, medical, nursing, anaesthetic, preoperative, intraoperative and postoperative managements. The key aims of these protocols are to reduce intraoperative and postoperative complications and relieve surgical stress response, thereby accelerating recovery, shorting hospitalization and reducing medical costs.
The incidental diagnosis of Pca has increased due to the widespread use of modern imaging modalities and PSA screening. Meanwhile, as a result of its inner features, most Pca patients are elderly people, which means that comorbidities are very common. Therefore, it is necessary for urologists to reduce complications and accelerate recovery from medical treatment. Although recent studies have proven the safety and effectiveness of FTS for Western populations in general and urological surgery6,7,8,9, there is a lack of data in the current literature about whether the FTS protocol is superior to the conventional protocol for Chinese Pca patients who have undergone RALP. To further evaluate the effectiveness and safety of FTS, we compared perioperative parameters and short-term outcomes of Chinese Pca patients who underwent RALP with FTS or conventional surgery (CS) in our department.
Methods
The records of 73 men who underwent RALP from October 2015 to November 2017 were retrospectively reviewed. All relevant clinical data were collected, and preoperative evaluation of each patient was performed, including age, body mass index (BMI), PSA level, the biopsy Gleason score, clinical stage, medical history, the American Society of Anesthesiologists (ASA) classification score, and laboratory blood tests. All of the patients enrolled were diagnosed with Pca. According to the different perioperative protocols, all the patients were divided into two groups (the CS group and FTS group). The main principles of the FTS and CS protocols are listed in Table 1.
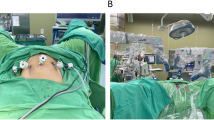
RALP was carried out by a single team of surgeons using the da Vinci Robotic 3-Arm System (Intuitive Surgical, Sunnyvale, CA, USA) via a transperitoneal approach with either standard lymphadenectomy or no lymphadenectomy10. The criteria for hospital discharge included tolerance of a regular diet, normal body temperature, mobilization out of bed, and satisfactory pain control. All complications were classified using the Clavien system.
The study was approved by the Ethics Review Board of Second Xiangya Hospital and conformed to the Declaration of Helsinki. Informed consent was obtained from all participants.
Preoperative education
In the FTS group, patients were given detailed information on the FTS protocol as well as information about the RALP surgery. In the CS group, we only informed patients about the RALP surgery itself.
Preoperative bowel preparation and fasting
In the FTS group, all the patients were instructed to consume a clear liquid diet one day before the operation and take 137.15 g polyethylene glycol electrolyte powder mixed with 2 L of water in the afternoon prior to the operation. No mechanical bowel preparation was performed. A mandatory fast was started 6 h before operation. In the CS group, patients were given streptomycin (oral 1.0 g tid 2 d) and metronidazole (oral 0.4 g tid 2 d). On the second day before operation, patients were instructed to have a semiliquid diet. On the day before operation, patients were instructed to consume a clear liquid diet and take 137.15 g polyethylene glycol electrolyte powder mixed with 2 L of water in the afternoon. Meanwhile, a mandatory overnight 12 h fast was carried out before operation, and a mechanical bowel preparation was performed in the evening before the operation.
Intraoperative and postoperative fluid infusion
In the FTS group, all patients received an intraoperative restricted fluid infusion protocol (5 ml/kg/h) and 1000–2000 ml fluid infusion per day for 2–3 days after the operation. In the CS group, all patients received intraoperative standard fluid therapy, which meant that a total of 3000–5000 ml fluid was infused per patient on the day of the operation. Then, all patients were given approximately 2500–3000 ml fluid per day for the next 3–4 days.
Postoperative mobilization
In the FTS group, patients were encouraged to ambulate postoperatively as soon as possible. If the patients’ conditions allowed, early mobilization was carried out on postoperative day (POD) 0 and the rest of the PODs (sit up on day 0, sit out of bed on day 1, walk on day 2). However, patient ambulation in the CS group was mainly based on the patient’s own desire.
Postoperative analgesia
In the FTS group, a single dose of parecoxib 40 mg I.V. on the day of surgery followed by 20 mg I.V. every 12 h for the next 72 h was given to patients. In the CS group, opium analgesics were used on demand.
Postoperative diet
In the FTS group, chewing gum was used on POD 111. Then, patients were allowed to drink clear liquid on POD 2. On POD 3, a semiliquid diet was given. On POD 4, a normal diet was resumed. In the CS group, patients were only instructed to have a liquid and diet after first flatus.
Statistical analysis
All statistical analyses were performed using SPSS 17.0 for Windows (SPSS Inc., Chicago). All results are presented as the mean ± standard deviation (SD) and frequency (number of cases). Comparisons between two groups were carried out by Student’s t-test for continuous variables and the Mann-Whitney U test for categorical variables. For all tests, P values of <0.05 were considered statistically significant.
Results
A retrospective analysis of 73 consecutive Chinese patients with localized Pca who underwent RALP in our department between October 2015 and November 2017 was carried out. Of the 73 patients, 37 underwent RALP before the introduction of the FTS protocol (CS group), and 36 underwent RALP after the introduction of the FTS protocol (FTS group). The demographic and preoperative clinical data are shown in Table 2. No significant differences in age, BMI, PSA level, ASA, clinical stage, biopsy Gleason score, white blood cell (WBC) count, haemoglobin (Hb) level, or serum C-reactive protein (CRP) level were observed between the two groups (all P > 0.05).
Table 3 shows details about the operative outcomes. There were no significant differences in operative time or estimated blood loss between the two groups (both P > 0.05). Compared with the CS group, the patients in the FTS group had a significantly shorter postoperative hospital stay, time to first flatus and time to regular diet (all P < 0.05). With the purpose of assessing the surgical stress response, the WBC counts and serum CRP levels were measured on PODs 1, 3, 5 and 7 (Table 4). No significant differences in WBC count or CRP level were observed between the two groups at POD 1 or 3 (all P > 0.05). However, at PODs 5 and 7, WBC count and CRP levels in the CS group were significantly higher than in the FTS group (all P < 0.05). Meanwhile, the postoperative pain control in the FTS group was better than that in the CS group, which meant less additional opium analgesic consumption (P = 0.004).
The details of complications in both groups are listed in Table 3. All the complications in both groups were minor complications that were classified as Clavien grade I or II. The complication rates in the CS group were significantly higher than those in the FTS group (P = 0.025). There were no cases of conversion to open surgery.
Discussion
In recent years, there has been a rapid adoption of RALP among urologists for the management of Pca patients. Furthermore, with evidence of improved convalescence, RALP has advantages in minimizing operative injury and reducing complications in comparison to open surgery and laparoscopic RP3,12. However, with increasing experience in RALP, a trend has emerged in experienced medical centres to implement the FTS into RALP programmes. The FTS or EARS protocol is a standardized multimodal perioperative care pathway that aims to reduce postoperative morbidity, minimize the negative stress effects of surgery, accelerate recovery and shorten hospital length of stay (LOS). After RALP was first introduced in the 1990s in colorectal surgery, it has been widely implemented in abdominal and gynaecologic surgery13,14,15. However, there is a lack of studies on fast-track programmes in RALP. In the current study, we describe the short-term outcomes of RALP for Chinese Pca patients with FTS or CS in our department. Our results demonstrate that the implementation of FTS obviously accelerated postoperative recovery and was safe and effective.
In the traditional programme, the operation and medication are the keys to the whole treatment. However, in our study, preoperative education played an important role in FTS patients’ learning about Pca, about RALP, about each detailed step of the FTS protocol and about the potential morbidities. The key aims of preoperative education are to help patients relieve their psychological and physiological stress and proactively cooperate with urologists and nurses. A previous study has demonstrated that patient education about FTS, preoperative investigations and relevant information offered is essential for patients to have a better physiological state, a more rapid return to normal quality of life, a shorter stay in intermediate care, and a faster recovery from surgery16.
Mechanical bowel preparation accompanied by medication and long-term fasting has been routinely performed in Pca patients undergoing RP to reduce the risk of postoperative infections and morbidities resulting from potential rectal injury during the procedure. However, previous studies have questioned the benefit of bowel preparation17,18. Indeed, traditional bowel preparation can lead to some adverse side effects, such as dehydration, electrolyte or acid-base disturbance, and intestinal mucosal architectural change19,20. Therefore, we performed an improved one-day bowel preparation in the FTS group. Our results demonstrate that the FTS protocol was associated with significantly more rapid intestinal motility and a shorter period to bowel function recovery without obviously increasing the risk of postoperative complications than with the CS protocol.
Traditionally, the main propose of intraoperative and postoperative fluid infusion is to maintain hydro-electrolyte balance and supply the basic energy needs for metabolism. However, administering excessive fluid causes intestinal oedema, coagulation dysfunction, impaired wound healing, increased interstitial lung water, hypervolemia and cardiopulmonary complications, which can all negatively influence recovery21. Therefore, if the patient is normovolaemic and under the careful monitoring of vital signs, the intraoperative and postoperative restricted fluid infusion will not only ease the patient’s pain but also accelerate recovery22. Our results indicate that the restricted fluid therapy was safe and feasible.
Early mobilization is beneficial, as it is associated with supportive effects on muscle strength, bowel function, cardiovascular and respiratory function, and psychological well-being and diminishes the cardiopulmonary complications and thromboembolic effects23,24. A previous study analysing the impact of preoperative and postoperative exercise compared with FTS mobilization did not show any significant differences in LOS, readmission, complications or mortality in patients undergoing radical cystectomy. However, there were significant differences in the ability to perform personal activities and mobilize between the FTS and conventional groups in the first 7 d25. Unfortunately, poorly controlled postoperative pain not only is an adverse side effect of surgery that limits early mobilization but also leads to the stress response accompanying surgical injury itself, with the potential to cause a series of complications. Adequate and appropriate analgesia is essential to early mobilization and reduction of the postoperative stress response26. Because of its intrinsic side effects, opioids have the potential to cause nausea, vomiting and intestinal ileus26. Therefore, polypharmacological opioid-sparing analgesia is recommended, and the basic drug should include an NSAID27. Parecoxib, an injectable selective cyclooxygenase enzyme-2 (COX-2) inhibitor, can not only relieve postoperative pain but also reduce the postoperative stress response28. In the current study, the degree of postoperative stress response was evaluated by measuring the WBC count and serum CRP level. Patients in the FTS group were encouraged to mobilize early, and parecoxib was used in the FTS group instead of the opioid given to the CS group. Our results reveal that the FTS protocol facilitated opiate minimization, reduction of the stress response, and lowered the risk of cardiopulmonary and coagulation complications.
Traditionally, patients undergoing surgery were only allowed to intake liquid after the first flatus passed because the early resumption of oral nutrition was considered to increase the incidence of intestinal complications. Previous studies have demonstrated that early oral intake can not only stimulate gastrointestinal pathways to promote bowel movement but also positively affect the brain-gut axis to facilitate higher cognitive function, such as emotion and decision making, which are associated with a decreased paralytic ileus, fewer infectious complications, increased patient satisfaction, shorter LOS, and a faster recovery29,30,31,32. Thus, early oral intake is recommended as a key component of the FTS protocol. However, postoperative nausea, vomiting and ileus are the risks of early oral intake. Cephalic-vagal stimulation from gum chewing promotes propulsive and hormonal gastrointestinal activity similar to what appears with normal eating. Gum chewing is a form of sham feeding that can stimulate bowel motility through neurohumoural reflexes11. In this study, early oral intake and chewing gum were applied in the FTS group. In concordance with previous studies, all early oral intake and gum chewing were safe and were associated with a lower incidence of complications, minimal problems of tolerance, decreased fluid infusion, and a faster recovery.
There are several limitations to the analysis reported in this study. First, it was a retrospective study with a small sample size in a single clinical centre and not a randomized controlled trial. Thus, the small sample size and the chosen P value may be associated with inflation of the type I error. Due to the statistical nature of a hypothesis test, all statistical results have a probability of inducing type I and type II errors. The only way to reduce both error rates is to increase the sample size. Additionally, the duration of follow-up was not enough to evaluate the long-term outcomes of the FTS protocol. Finally, because the FTS protocol aimed to standardize every phase of preoperative, intraoperative, and postoperative management to enable patients to recover faster, the protocol should be applied by a standardized team consisting of urologists, anaesthetists, nurses, and physiotherapy staff. Further studies with a randomized controlled design, adequate sample size, long-term follow-up, and more than one centre are required to illustrate the value of FTS protocols in RALP.
In conclusion, the results of this study indicate that the introduction of this FTS protocol for Chinese Pca patients undergoing RALP was safe and was associated with reduced stress response, accelerated recovery and shorter LOS.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer Statistics, 2017. CA. Cancer J. Clin. 67, 7–30, https://doi.org/10.3322/caac.21387 (2017).
Ilic, D. et al. Laparoscopic and robot-assisted vs open radical prostatectomy for the treatment of localized prostate cancer: a Cochrane systematic review. BJU Int., https://doi.org/10.1111/bju.14062 (2017).
Allan, C. & Ilic, D. Laparoscopic versus Robotic-Assisted Radical Prostatectomy for the Treatment of Localised Prostate Cancer: A Systematic Review. Urol. Int. 96, 373–378, https://doi.org/10.1159/000435861 (2016).
Ficarra, V. et al. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur. Urol. 55, 1037–1063, https://doi.org/10.1016/j.eururo.2009.01.036 (2009).
Kehlet, H. & Wilmore, D. W. Multimodal strategies to improve surgical outcome. Am. J. Surg. 183, 630–641 (2002).
Damania, R. & Cocieru, A. Impact of enhanced recovery after surgery protocols on postoperative morbidity and mortality in patients undergoing routine hepatectomy: review of the current evidence. Ann Transl Med 5, 341, https://doi.org/10.21037/atm.2017.07.04 (2017).
Powell, A. C., Stopfkuchen-Evans, M., Urman, R. D. & Bleday, R. Decreasing the Surgical Stress Response and an Initial Experience from the Enhanced Recovery After Surgery Colorectal Surgery Program at an Academic Institution. Int. Anesthesiol. Clin. 55, 163–178, https://doi.org/10.1097/AIA.0000000000000162 (2017).
Major, P. et al. Postoperative Care and Functional Recovery After Laparoscopic Sleeve Gastrectomy vs. Laparoscopic Roux-en-Y Gastric Bypass Among Patients Under ERAS Protocol. Obes. Surg., https://doi.org/10.1007/s11695-017-2964-3 (2017).
Pang, K. H., Groves, R., Venugopal, S., Noon, A. P. & Catto, J. W. F. Prospective Implementation of Enhanced Recovery After Surgery Protocols to Radical Cystectomy. Eur. Urol., https://doi.org/10.1016/j.eururo.2017.07.031 (2017).
Yuh, B. E., Ruel, N. H., Mejia, R., Novara, G. & Wilson, T. G. Standardized comparison of robot-assisted limited and extended pelvic lymphadenectomy for prostate cancer. BJU Int. 112, 81–88, https://doi.org/10.1111/j.1464-410X.2012.11788.x (2013).
Fitzgerald, J. E. & Ahmed, I. Systematic review and meta-analysis of chewing-gum therapy in the reduction of postoperative paralytic ileus following gastrointestinal surgery. World J. Surg. 33, 2557–2566, https://doi.org/10.1007/s00268-009-0104-5 (2009).
Sujenthiran, A. et al. National cohort study comparing severe medium-term urinary complications following radical prostatectomy: robot-assisted versus laparoscopic versus retropubic open radical prostatectomy. BJU Int, https://doi.org/10.1111/bju.14054 (2017).
Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 78, 606–617 (1997).
Li, L., Chen, J., Liu, Z., Li, Q. & Shi, Y. Enhanced recovery program versus traditional care after hepatectomy: A meta-analysis. Medicine (Baltim.) 96, e8052, https://doi.org/10.1097/md.0000000000008052 (2017).
Trowbridge, E. R. et al. Review of enhanced recovery programs in benign gynecologic surgery. Int Urogynecol J, https://doi.org/10.1007/s00192-017-3442-0 (2017).
Miller, C. et al. Introduction of robot-assisted radical cystectomy within an established enhanced recovery programme. BJU Int. 120, 265–272, https://doi.org/10.1111/bju.13702 (2017).
Gralla, O. et al. Fast-track surgery in laparoscopic radical prostatectomy: basic principles. World J. Urol. 25, 185–191, https://doi.org/10.1007/s00345-006-0139-2 (2007).
Ferguson, K. H., McNeil, J. J. & Morey, A. F. Mechanical and antibiotic bowel preparation for urinary diversion surgery. J. Urol. 167, 2352–2356 (2002).
Holte, K., Nielsen, K. G., Madsen, J. L. & Kehlet, H. Physiologic effects of bowel preparation. Dis. Colon Rectum 47, 1397–1402 (2004).
Bucher, P., Gervaz, P., Egger, J. F., Soravia, C. & Morel, P. Morphologic alterations associated with mechanical bowel preparation before elective colorectal surgery: a randomized trial. Dis. Colon Rectum 49, 109–112, https://doi.org/10.1007/s10350-005-0215-5 (2006).
Abraham-Nordling, M. et al. Randomized clinical trial of fluid restriction in colorectal surgery. Br. J. Surg. 99, 186–191, https://doi.org/10.1002/bjs.7702 (2012).
Gustafsson, U. O. et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS((R))) Society recommendations. World J. Surg. 37, 259–284, https://doi.org/10.1007/s00268-012-1772-0 (2013).
Agnelli, G. Prevention of venous thromboembolism in surgical patients. Circulation 110, Iv4–12, https://doi.org/10.1161/01.CIR.0000150639.98514.6c (2004).
Drolet, A. et al. Move to improve: the feasibility of using an early mobility protocol to increase ambulation in the intensive and intermediate care settings. Phys. Ther. 93, 197–207, https://doi.org/10.2522/ptj.20110400 (2013).
Jensen, B. T., Petersen, A. K., Jensen, J. B., Laustsen, S. & Borre, M. Efficacy of a multiprofessional rehabilitation programme in radical cystectomy pathways: a prospective randomized controlled trial. Scand J Urol 49, 133–141, https://doi.org/10.3109/21681805.2014.967810 (2015).
Nimmo, S. M., Foo, I. T. H. & Paterson, H. M. Enhanced recovery after surgery: Pain management. J. Surg. Oncol., https://doi.org/10.1002/jso.24814 (2017).
Adding, C., Collins, J. W., Laurin, O., Hosseini, A. & Wiklund, N. P. Enhanced recovery protocols (ERP) in robotic cystectomy surgery. Review of current status and trends. Curr. Urol. Rep. 16, 32, https://doi.org/10.1007/s11934-015-0497-7 (2015).
Huang, Z. et al. Efficacy of parecoxib on the level of Il-6, CRP, and postoperative pain relief after percutaneous nephrolithotomy. (2016).
Azhar, R. A. et al. Enhanced Recovery after Urological Surgery: A Contemporary Systematic Review of Outcomes, Key Elements, and Research Needs. Eur. Urol. 70, 176–187, https://doi.org/10.1016/j.eururo.2016.02.051 (2016).
Al Omran, Y. & Aziz, Q. The brain-gut axis in health and disease. Adv. Exp. Med. Biol. 817, 135–153, https://doi.org/10.1007/978-1-4939-0897-4_6 (2014).
Dutton, T. J., Daugherty, M. O., Mason, R. G. & McGrath, J. S. Implementation of the Exeter enhanced recovery programme for patients undergoing radical cystectomy. BJU Int. 113, 719–725, https://doi.org/10.1111/bju.12533 (2014).
Gianotti, L., Nespoli, L., Torselli, L., Panelli, M. & Nespoli, A. Safety, feasibility, and tolerance of early oral feeding after colorectal resection outside an enhanced recovery after surgery (ERAS) program. Int. J. Colorectal Dis. 26, 747–753, https://doi.org/10.1007/s00384-011-1138-3 (2011).
Acknowledgements
The authors are grateful for the invaluable support from the other members of the Urological Department.
Author information
Authors and Affiliations
Contributions
Z.H. and Y.W. conceived the idea for the study. Z.H., H.Z., and Y.N. analysed the data. Z.H., Y.L., L.Y., and Y.W. performed the surgeries. Z.H., P.X. and Y.W. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, Z., Yi, L., Zhong, Z. et al. Comparison of Fast-Track Versus Conventional Surgery Protocol for Patients Undergoing Robot-Assisted Laparoscopic Radical Prostatectomy: A Chinese Experience. Sci Rep 8, 8017 (2018). https://doi.org/10.1038/s41598-018-26372-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-26372-x
This article is cited by
-
Clinical efficacy of enhanced recovery after surgery (ERAS) program in patients undergoing radical prostatectomy: a systematic review and meta-analysis
World Journal of Surgical Oncology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.