Abstract
Cataract surgery can cause macular thickness change. We used optical coherence tomography (OCT) to assess the macular thickness of different regions after femtosecond laser–assisted cataract surgery of age-related cataracts (ARC) and myopia cases with cataract (myopia group). Fifty eyes of 50 patients in ARC group and fifty eyes of 50 patients in myopia with cataract group were included. All study underwent femtosecond laser–assisted cataract surgery and macular thickness of was measured at pre-operation and 1 week, 1 month after surgery. There are significant differences of foveal thickness (P = 0.02), foveal volume (P = 0.02) and average retinal thickness (P = 0.02) between two groups before operation. In the myopia group, statistically significant differences were not found in postoperative macular thickness as compared with ARC group. There are differences in macular thickness between pre-operation and 1 month after operation when compared with nasal outer macular ring thickness (P = 0.022), foveal volume (P = 0.005) and average retinal thickness (P = 0.012) in ARC group. The study suggest that femtosecond laser–assisted cataract extraction is safe in myopia group that did not cause significant increase of macular thickness. However, an increased post-operative local macular thickness was recoded while comparing macular thickness with the baseline in ARC group.
Similar content being viewed by others
Introduction
The subclinical macular edema after common and complex cataract surgery has brought substantial attention to surgeons due to the potential hazard of this complication to vision consequence1,2. Until now, the etiology and pathogenesis for the complication have not been completely clarified. Studies have showed that the anterior segment inflammation may play a vital role in the pathology after cataract surgery3,4. Other researches also showed that the retina pulled by posterior vitreous might contribute to the etiologic mechanism. It has been suggested that the phenomena can be caused by the shock wave of the phacoemulsification during cataract surgery. In myopia, complete or incomplete posterior vitreous detachment (PVD) is common phenomena due to fluidity of vitreous, which also presents after cataract surgery. During the process, macular pulled by vitreous may play a vital role for formation of subclinical macular edema. These findings support the notion that myopic eyes are more prone to macular edema formation after cataract surgery. But it is warranted for further study whether it is the case in femtosecond laser-assisted cataract surgery.
Femtosecond laser technology has become widely applied in various ophthalmic surgery especially for cataract5. On one hand, it brings precise surgical incision. On the other hand, it reduces the phacoemulsification power and improves the outcomes of cataract surgery. However, some surgeons have concerns on the suction ring used during the femtosecond laser procedure to avoid eye movements due to vacuum aspiration. A report showed that the suction ring causes temporally increase of intraocular pressure (IOP) during the vacuum aspiration (up to 40 mmHg in the LenSx laser system, Alcon Lasers, Inc.)6, which can induce various changes from anterior segment to posterior segment of ocular structure7. There is an increase of the vitreous distance using microkeratome suction ring for LASIK8. These alterations can cause a series of changes including bilateral vitreous detachment9, retinal hemorrhage10 and the change of ocular blood-flow11.
Optical coherence tomography (OCT) has been widely used in ophthalmic applications which is a noninvasive and high-resolution imaging modality for ocular internal structures12. Several studies used OCT to detect an increase of the parafoveal retinal thickness, foveal volume, and volume of the entire macula in glaucomatous eyes, manual small incision cataract surgery and phacoemulsification cataract surgery13,14,15. Studies also used OCT to assess the macular morphology after laser–assisted cataract surgery1,16. However, no study focuses on and compares the change of macular region thickness between ARC (age-related cataract) and myopic with cataract after femtosecond laser–assisted cataract surgery. The information of retinal thickness changes after the cataract operation especially for myopic eyes can provide insight to pathophysiology of subclinical macular edema occurring.
Patients and Methods
Patients
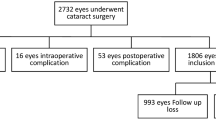
The study included 50 eyes from 50 patients with ARC and 50 eyes from 50 myopic with cataract (myopia group). The axial length is 23.03 ± 0.67 mm in the ARC group and 29.15 ± 4.17 mm in the myopia group. We excluded the patients with previous ocular surgery, trauma and known macular alteration (diabetic retinopathy or age-related macular degeneration). All patients were given a complete ophthalmologic evaluation before surgery including refraction, a slit lamp examination, B-scan ultrasonography and a dilated fundus evaluation.
The study received approval of the ethics committee at Affiliated Hospital of Nantong University and was conducted in compliance with the Declaration of Helsinki. All patients were willing to volunteer for the research and signed a written informed consent.
Surgery
All surgeries were performed by the same surgeon (H.J.G.) using the CENTURION® VISION SYSTEM (Alcon Laboratories Inc, Ft Worth, Texas). After pupillary dilation and topical anesthetics, a curved contact lens was used to applanate the cornea by the LenSx laser system. OCT was used to detect the location of the crystalline lens surface. After scanning a cylindrical pattern, a 5.5-mm diameter capsulotomy procedure was performed starting at 100 µm below the anterior capsule and ending at 100 µm above the capsule. The lens was fragmented into eight quadrants by a cross pattern. A self-sealing biplanar corneal incision (2.4 mm) and a side-port incision (1.0 mm) were created by femtosecond laser. In the study, proprietary energy and spot separation parameters used were 10 µJ spot and layer separation 8 µm for lens fragmentation, 6 µJ for capsulotomy, and 6-µJ spot separation 6 µm and layer separation 3 µm for primary and secondary corneal incision.
After treatment by femtolaser, the self-sealing corneal incisions was made by a blunt spatula and viscoelastic material was injected to the anterior chamber. A 5.5-mm diameter capsulotomy outside anterior chamber was identified and removed by rhexis forceps, followed by hydrodissection. The lens was removed using a stop-and-chop or a divide-and-conquer technique. The cortex was completely removed and then a one-piece, hydrophobic, acrylic, posterior chamber lens (SN60WF; Alcon Laboratories, Inc.; Fort Worth, TX) was implanted. At last, the viscoelastic material was removed by irrigation-aspiration. No any intra- or postoperative complications occurred during the surgery in the study.
Oct Measurements
OCT measurements (Cirrus HD-OCT 4000; Carl Zeiss Meditec, Dublin, CA) were performed 1 day before surgery and post-operation at 1 week and 1 month. The selection of the time points was based on that the most retinal thickening is observable after conventional phacoemulsification at those time points. The different macular region thickness was automatically determined by the instrument software as the distance between the internal limiting membrane and retinal pigment epithelium. Measurements were provided for three concentric regions. The central foveal region was a region with a diameter of 1 mm, and the inner and outer rings had outer diameters of 3 and 6 mm, respectively, and were divided into four quadrants respectively. We described them as superior outer macular ring thickness (SOMRT), bitamporal outer macular ring thickness (BOMRT), inferior outer macular ring thickness (IOMRT), nasal outer macular ring thickness (NOMRT), superior inter macular ring thickness (SIMRT), bitamporal inter macular ring thickness (BIMRT), inferior inter macular ring thickness (IIMRT), nasal inter macular ring thickness (NIMRT), foveal thickness (FT), foveal volume (FV) and average retinal thickness (ART).
Statistical Analysis
A SPSS 18.0 software (SPSS Inc, Chicago, Illinois) was performed for statistical analyses. Data are expressed as the mean and standard deviation. For comparisons of different macular region thickness between pre-operation and post-operation of femtosecond laser–assisted cataract surgery, the student’s t test was used. Pearson’s correlation analysis was used to assess the correlation between the nuclear hardness, phaco time, cumulative dissipated energy (CDE) and different macular region thickness. A P value less than 0.05 was considered statistically significant.
Results
Patient Characteristics
The ARC group comprised of 50 eyes of 50 patients with the mean age of 61.33 ± 7.52 years (range 49 to 76 years). The myopia group comprised of 50 eyes of 50 patients with the mean age of 56.66 ± 5.68 years (range 46 to 63 years) (Table 1).
Oct Parameters
Table 2 shows the pre- and postoperative macular thickness values in the ARC and myopia groups. The macular thicknesses measured in FT, FV and ART in myopia group are significantly higher than the ARC group in the baseline measurement (pre-operative). There are not statistically significant after surgery between the two groups. There are not statistically significant after surgery between the two groups. But in ARC group, we found there are different between pre-operation and post-operation in NOMRT, FV and ART (Tables 2 and 3). However, we did not detect any correlations between the nuclear hardness, phaco time, cumulative dissipated energy (CDE) and the macula thickness (Table 4).
Discussion
As a new technology, femtosecond laser applications in cataract surgery has several advantages including the incision stability17, the accurate IOL centration18,19,20 and the efficient lens fragmentation21,22. However, the suction ring used during the positioning of the femtosecond laser may have some harmful effect on macular region especially for the complex cataract cases.
In current clinical study, we analyzed the preoperative and postoperative macular thickness values in the myopia and ARC group by OCT. Postoperative cystoid macular edema (CME) is often asymptomatic and can be detected with only fluorescein angiography or OCT. Our results show that there are significant differences between the two groups when compared with FT, FV and ART before operation (Table 2). The results are consisted with previous research that the thicknesses significantly lower in the high myopic eyes than in the nonmyopic eyes23. The elongated axial length may be the reason for thinner macular thickness in myopic eyes24.
CME can be detected at the first week up to 6 months and peaks 4 to 6 weeks after surgery25. In this study, we did not find any difference between the two groups when compared the macular thickness of different region at 1 week or 1 month after surgery between the two groups. But in ARC group, we found there are different between pre-operation and post-operation in NOMRT, FV and ART (Table 3). However, we did not detect any correlations the nuclear hardness, phaco time, CDE and the macula thickness (Table 4). We speculate that the nuclear hardness and phaco time maybe are a crucial factor for the change. The means of nuclear hardness and phaco time is higher in ARC group when compare with myopia group. Though there are not any statistically significant between the two groups for nuclear hardness and phaco time. We also did not detect any statistically significant thickness change at myopia group after surgery. We speculate the reason is that used femtosecond laser technology reduced the phacoemulsification power and phaco time during surgery. The factors may be the cause for the CME formation.
In this study, the limitation includes a relatively small number patients and short follow-up period. Our original design is follow up at 1 week, 1 month, 3 months and 6 months after surgery. But due to the loss of follow up, we only collected the valid data of 50 patients for each group at 1 week and 1 month in current settings. There are not any different for macular thickness change between the two groups (ARC group: n = 22; Myopia group: n = 23) at 3 months (data not shown). The mean macular thickness of myopia group increased after surgery when compare with pre-operation, but this difference is not statistically significant. Our results suggest that used femtosecond laser applications to extract cataract is equally safe in the myopia group. Femtosecond laser–assisted cataract extraction did not result in macular thickness change at myopia group compared to the ARC group, although it needs to confirm at larger cohorts and longer follow up.
In conclusion, the femtosecond laser might provide us a efficacy surgical technology to treatment the myopic eyes with cataract. It is necessary to conduct the further randomized controlled studies with larger cohorts or other patients particularly with high risk for postoperative CME.
References
Conrad-Hengerer, I., Hengerer, F. H., Al Juburi, M., Schultz, T. & Dick, H. B. Femtosecond laser-induced macular changes and anterior segment inflammation in cataract surgery. Journal of refractive surgery 30, 222–226, https://doi.org/10.3928/1081597X-20140321-01 (2014).
Stifter, E., Menapace, R., Neumayer, T. & Luksch, A. Macular morphology after cataract surgery with primary posterior capsulorhexis and posterior optic buttonholing. American journal of ophthalmology 146, 15–22, https://doi.org/10.1016/j.ajo.2008.02.022 (2008).
Wielders, L. H. et al. Treatment of cystoid macular edema after cataract surgery. Journal of cataract and refractive surgery 43, 276–284, https://doi.org/10.1016/j.jcrs.2016.06.041 (2017).
Duan, P., Liu, Y. & Li, J. The comparative efficacy and safety of topical non-steroidal anti-inflammatory drugs for the treatment of anterior chamber inflammation after cataract surgery: a systematic review and network meta-analysis. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 255, 639–649, https://doi.org/10.1007/s00417-017-3599-8 (2017).
Alio, J. L., Abdou, A. A., Puente, A. A., Zato, M. A. & Nagy, Z. Femtosecond laser cataract surgery: updates on technologies and outcomes. Journal of refractive surgery 30, 420–427, https://doi.org/10.3928/1081597X-20140516-01 (2014).
Vetter, J. M. et al. Intraocular pressure during corneal flap preparation: comparison among four femtosecond lasers in porcine eyes. Journal of refractive surgery 27, 427–433, https://doi.org/10.3928/1081597X-20101210-01 (2011).
Davis, R. M. & Evangelista, J. A. Ocular structure changes during vacuum by the Hansatome microkeratome suction ring. Journal of refractive surgery 23, 563–566 (2007).
Mirshahi, A. & Kohnen, T. Effect of microkeratome suction during LASIK on ocular structures. Ophthalmology 112, 645–649, https://doi.org/10.1016/j.ophtha.2004.11.046 (2005).
Smith, R. J. et al. Complete bilateral vitreous detachment after LASIK retreatment. Journal of cataract and refractive surgery 30, 1382–1384, https://doi.org/10.1016/j.jcrs.2003.10.021 (2004).
Moshfeghi, A. A., Harrison, S. A., Reinstein, D. Z. & Ferrone, P. J. Valsalva-like retinopathy following hyperopic laser in situ keratomileusis. Ophthalmic surgery, lasers & imaging: the official journal of the International Society for Imaging in the Eye 37, 486–488 (2006).
Conway, M. L., Wevill, M., Benavente-Perez, A. & Hosking, S. L. Ocular blood-flow hemodynamics before and after application of a laser in situ keratomileusis ring. Journal of cataract and refractive surgery 36, 268–272, https://doi.org/10.1016/j.jcrs.2009.09.013 (2010).
Huang, D. et al. Optical coherence tomography. Science 254, 1178–1181 (1991).
Lederer, D. E. et al. Analysis of macular volume in normal and glaucomatous eyes using optical coherence tomography. American journal of ophthalmology 135, 838–843 (2003).
Biro, Z., Balla, Z. & Kovacs, B. Change of foveal and perifoveal thickness measured by OCT after phacoemulsification and IOL implantation. Eye 22, 8–12, https://doi.org/10.1038/sj.eye.6702460 (2008).
Ghosh, S. et al. Prospective randomized comparative study of macular thickness following phacoemulsification and manual small incision cataract surgery. Acta ophthalmologica 88, e102–106, https://doi.org/10.1111/j.1755-3768.2010.01896.x (2010).
Nagy, Z. Z. et al. Macular morphology assessed by optical coherence tomography image segmentation after femtosecond laser-assisted and standard cataract surgery. Journal of cataract and refractive surgery 38, 941–946, https://doi.org/10.1016/j.jcrs.2012.02.031 (2012).
Masket, S., Sarayba, M., Ignacio, T. & Fram, N. Femtosecond laser-assisted cataract incisions: architectural stability and reproducibility. Journal of cataract and refractive surgery 36, 1048–1049, https://doi.org/10.1016/j.jcrs.2010.03.027 (2010).
Nagy, Z. Z. et al. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. Journal of refractive surgery 27, 564–569, https://doi.org/10.3928/1081597X-20110607-01 (2011).
Friedman, N. J. et al. Femtosecond laser capsulotomy. Journal of cataract and refractive surgery 37, 1189–1198, https://doi.org/10.1016/j.jcrs.2011.04.022 (2011).
Dick, H. B., Canto, A. P., Culbertson, W. W. & Schultz, T. Femtosecond laser-assisted technique for performing bag-in-the-lens intraocular lens implantation. Journal of cataract and refractive surgery 39, 1286–1290, https://doi.org/10.1016/j.jcrs.2013.07.014 (2013).
Conrad-Hengerer, I., Hengerer, F. H., Schultz, T. & Dick, H. B. Effect of femtosecond laser fragmentation of the nucleus with different softening grid sizes on effective phaco time in cataract surgery. Journal of cataract and refractive surgery 38, 1888–1894, https://doi.org/10.1016/j.jcrs.2012.07.023 (2012).
Filkorn, T. et al. Comparison of IOL power calculation and refractive outcome after laser refractive cataract surgery with a femtosecond laser versus conventional phacoemulsification. Journal of refractive surgery 28, 540–544, https://doi.org/10.3928/1081597X-20120703-04 (2012).
Lam, D. S. et al. Regional variations in the relationship between macular thickness measurements and myopia. Investigative ophthalmology & visual science 48, 376–382, https://doi.org/10.1167/iovs.06-0426 (2007).
Hwang, Y. H. & Kim, Y. Y. Macular thickness and volume of myopic eyes measured using spectral-domain optical coherence tomography. Clinical & experimental optometry 95, 492–498, https://doi.org/10.1111/j.1444-0938.2012.00749.x (2012).
Ecsedy, M. et al. Effect of femtosecond laser cataract surgery on the macula. Journal of refractive surgery 27, 717–722, https://doi.org/10.3928/1081597X-20110825-01 (2011).
Acknowledgements
This study was supported by the Technology and Science Foundation of Jiangsu province (N0:BE2016699) and Frontiers and Key Technological Innovations-Social and People’s Livelihood Innovation Program Research- New Clinical Technology(MS22015072).
Author information
Authors and Affiliations
Contributions
Y.W. and J.D. performed the experiments. M.Y. and Y.X. participated in data analysis. Y.W. and J.W. wrote the manuscript. H.J.G. conceived the research, and critically reviewed the manuscript and interpreted the data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Du, J., Yang, M. et al. Distinct macular thickness changes after femtosecond laser–assisted cataract surgery of age-related cataract and myopia with cataract. Sci Rep 8, 3279 (2018). https://doi.org/10.1038/s41598-018-21698-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-21698-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.