Abstract
To examine the association between BMI and QOL in breast cancer survivors in China, we conducted a cross-sectional survey and recruited 10708 breast cancer survivors. Survivors self-reported QOL was measured using the EORTC QLQ-C30 and the QLQ-BR23. The impact of BMI on QOL was examined through standard least squares regression. Normal weight and overweight survivors were more likely to have a better QOL than underweight and obese survivors and the results were similar to survivors diagnosed as having chronic diseases. After adjustment for clinical and sociodemographic factors, the QOL increased with increasing BMI in breast cancer survivors ranged from underweight to overweight with no chronic diseases, especially in the scales of emotional function and fatigue. Obese breast cancer survivors reported a significantly worse QOL compared to normal weight and overweight breast cancer survivors. Within breast cancer survivors with one or more chronic diseases, it was more obvious that overweight ones had a significantly better QOL with clear evidence of a dose relationship across underweight to overweight in almost all scales. Unlike obese breast cancer survivors without chronic diseases, the ones with chronic disease(s) had a similar QOL compared to normal weight breast cancer survivors in all scales except in the domain of fatigue.
Similar content being viewed by others
Introduction
The increasing prevalence of overweight and obesity has become a major threat to public health1 and the World Health Organization (WHO) listed obesity as one of today’s most blatantly visible yet most neglected public health problems and dubbed the global epidemic “globesity”2. Indeed, overweight and obesity are well-known risk factors that can cause and aggravate a number of chronic diseases3,4 including cardiovascular diseases5, certain forms of cancer6,7, and metabolic diseases8. Nevertheless, substantial data have shown a survival benefit of overweight and moderate obesity in patients with chronic diseases9,10,11, a better outcome was seen in the overweight and moderately obese patients compared with the normal weight patients12,13,14,15.
Breast cancer is the most prevalent malignant cancer in China, accounting for 15% of all female primary cancers16, and has a significant upward trend in the incidence rates. It is quite challenging for now and the future based on the huge population of China. The outcomes of breast cancer have been consistently improved and the current 5-year survival rate reaches 73%17. Therefore, the quality of life (QOL) of the long-term breast cancer survivors is more and more important. According to the previous studies, overweight and obesity are risk factors in patients with breast cancer18. Despite few studies on the assessment of QOL on overweight and obese breast cancer survivors at present, the presentation of QOL of obese and normal weight survivors were not consistent among previous studies19. Some studies had investigated the relationship between body mass index (BMI) and QOL, and indicated that higher BMI was associated with poor QOL20,21,22,23,24. However, conflicting evidences have questioned the adverse influence of overweight and obesity on the QOL. Some research suggested that within people with chronic disease(s), the ones with overweight or obesity had better QOL than the ones without these25,26,27. Therefore, the aim of this study was to investigate the association between BMI and QOL in breast cancer survivors in China.
Materials and Methods
Subjects
The present study was a population-based cross-sectional study. Breast cancer survivors were recruited from the affiliated groups of Cancer Rehabilitation Clubs in 34 cities across China. Exclusion criteria involved: severe physical and mental comorbidity, being illiterate, and missing BMI data. Approval for the research protocol was received from the Ethic Committee of Public Health School of Fudan Univeristy (protocol number RB # 2013-04-0450). A written Informed Consent was obtained from each participant prior to participation in the study and all methods were performed in accordance with the guidelines and regulations.
A self-completed questionnaire was used to collect information of participants including birthday, height, weight, marital status, educational level, financial, tumor stage, time since diagnosis, treatment, exercise, chronic conditions, and their use of tobacco and alcohol, QLO-C30 and QLQ-BR23. The chronic diseases included hypertension, hyperlipidemia, hyperuricemia, type I and II diabetes mellitus, coronary heart disease, stroke, respiratory disease, digestive system disease, and musculoskeletal disorders, which were collected from the participants self-reported results. Inclusion criteria were met by 10708 of the 10794 breast cancer survivors.
Measurement of QOL
The simplified Chinese version of the Quality of Life Questionnaire-Core 30 items (EORTC QLQ-C30) and the Breast Cancer-specific module QLQ-23 also developed by the EORTC were used as the measures of QOL. The QLQ-C3028 encompassed five functional scales (Physical, Role, Cognitive, Emotional, and Social Functioning); three symptom scales (Fatigue, Pain, and Nausea/Vomiting); and a Global Health Status/QOL scale. Six single item scales were also included (Dyspnoea, Insomnia, Appetite Loss, Constipation, Diarrhoea, and Financial Difficulties). The EORTC QLQ-BR2329 incorporated two functional scales (Body image and Sexual Function) and three symptom scales (Systemic therapy side effects, Arm and Breast symptoms). Three single item scales (Upset by hair loss, Future respective, and Sexual enjoyment) were also included. A 4-point response scale - except for the global health status which were rated on a 7-point scale from 1 (very poor) to 7 (excellent), was used (1 = not at all; 4 = very much). The time frame was “during the past week”, except for the sexual functioning and sexual enjoyment (“during the past four weeks”). Scale scores were calculated by averaging items within scales and transforming average scores linearly into a 0 to 100 scale. A high score for a functional scale represented a high/healthy level of functioning whereas a high score for a symptom scale or item represented a high level of symptomatology or other problems. More details on the scoring procedures could be found in the EORTC QLQ-C30 Scoring Manual30. The psychometric properties of the questionnaire were tested and in conclusion it was found to possess the required standards such as validity (measuring what it is intended to measure), reliability (measuring with sufficient precision) and sensitivity (ability to detect changes)31.
Categorization of BMI
In this study, BMI, a person’s weight (in kilograms) divided by the square of his or her height (in metres), was divided into four categories according to the WHO guidelines:32 underweight (<18.5 Kg/m2), normal weight (18.5–24.9 Kg/m2), overweight (25.0–29.9 Kg/m2) and obesity (≥30 Kg/m2).
Data Analysis
All statistical analyses were performed using the Statistical Analysis System (SAS, Version 9.4). Participants’ characteristics and QOL were summarized by ratios and percentages for categorical variables and mean (standard deviation) for continuous variables. Differences in means for continuous variables were compared using analysis of variance (ANOVA), and differences in proportions were tested by \({\chi }^{2}\) test. Standard least squares regression was used to evaluate the independent association between BMI and QOL. Bonferroni test was applied to analyze the difference between groups. Statistical inferences were two-sided and P value less than 0.05 were considered as statistically significant.
Results
Clinical Characteristics
Among 10794 breast cancer survivors, 10708 subjects met the inclusion criteria. Table 1 summarized the clinical characteristics of the 10708 breast cancer survivors who were included in the analysis. The proportions of the participants were 3.42%, 67.90%, 25.60% and 3.08% for the underweight, normal weight, overweight and obese respectively based on the international BMI categories. The mean (SD) age and BMI were 56.99 (5.50) years and 23.63 (3.20) Kg/m2. The characteristics of the subjects didn’t equally distribute among the BMI categories (P < 0.05), except for marital status, financial, tumor stage and surgery. A majority (70.85%) of the participants had one or more comorbid conditions. Subjects with excess weight were more likely to suffer from chronic diseases, relapse, metastasis, and tended to drink and smoke more. Obesity was more frequent in subjects who never exercised.
Relationship between BMI and QOL
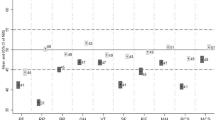
Overweight breast cancer survivors reported significantly (P < 0.05) better QOL in almost all domains compared with underweight, normal weight and obese ones (Table 2). Overweight breast cancer survivors had significantly better QOL than normal weight ones in domains of global health status, emotional function, social function, cognitive function, fatigue, nausea and vomiting, insomnia, appetites loss, constipation, diarrhea, systemic therapy side effects, and arm symptoms (P < 0.05). The obese breast cancer survivors had a similar QOL with normal weight ones in almost all scales (P > 0.05) except for domains of dyspnoea and arm symptoms (P < 0.05). Compared with the normal weight breast cancer survivors, the underweight ones had significantly (P < 0.05) lower QOL in the domains of global health status, physical function, fatigue, pain, dyspnoea, insomnia, and appetites loss. In domains of role function, sexual function, sexual enjoyment, body image, future respective, breast symptom and upset by hair loss, no significant (P > 0.05) differences were found among the four BMI groups. The mean scores of the QOL increased with the increasing BMI from the underweight to the overweight in function scales, but decreased in symptom scales.
Relationship between BMI and QOL stratified by status of chronic conditions
Mean scores of the reported QOL in breast cancer survivors according to BMI categories and status of chronic conditions were described in Table 3. The covariates which the present study chose to adjust included age, educational level, number of chronic diseases, marital status, occupation, relapse, transfer, exercise, use of alcohol, breakfast diet, vegetables and fruits consumption as well as tobacco use. In the group of breast cancer survivors with no chronic disease, the QOL increased gradually along with BMI in the groups ranged from the underweight to the overweight in almost all domains; obese breast cancer survivors reported significantly worse QOL compared with normal weight and overweight ones; Overweight breast cancer survivors reported significantly higher QOL in domains of emotional function and fatigue, and had similar scores in all other domains when compared with normal weight ones; Underweight breast cancer survivors had significantly worse QOL in domains of constipation and diarrhea compared with normal weight ones.
In the group of breast cancer survivors with one or more chronic diseases, the QOL increased gradually along with BMI in the groups ranged from underweight to obese in almost all scales. Compared with the normal weight breast cancer survivors group, the overweight group had significantly higher QOL in domains of global health status, emotional function, social function, fatigue, insomnia, appetites loss, constipation, diarrhoea, systemic therapy side effects, and arm symptoms; and the underweight group had significantly lower QOL in global health status, physical function, fatigue, pain, insomnia and appetites loss. The obese breast cancer survivors had similar QOL with normal weight ones in all scales (P > 0.05) except in domains of fatigue (P < 0.05).
The counterintuitive relationship between BMI and QOL was similar in the groups of breast cancer survivors without chronic diseases and in those with one or more chronic diseases. Nevertheless, the effect was more pronounced in the group of breast cancer survivors who had one or more chronic diseases.
Discussion
Contemporarily, innovative clinical treatments have greatly improved the survivals of breast cancer, making QOL the next important requirement of survivors. QOL has received extensive attention as an outcome measurement in public health and clinical medicine. In the present study, QOL of breast cancer survivors was measured by EORTC QLQ-C30 and EORTC QLQ-BR23. Although certain clinical factors33 and socioeconomic status34, such as stage, age, income, marital status et al. are considered to be the most important factors influencing survivals of breast cancer, these are factors which can’t be modified. In contrast, body weight was one of the few potentially modifiable lifestyle factors. Therefore, the goal of this study was to explore the association between BMI and QOL in Chinese women with breast cancer.
Since chronic diseases were important determinant of QOL35 and BMI was associated with chronic diseases36,37, we divided two groups to determine the association between BMI and QOL according to whether or not comorbidities existed. Different patterns were observed in breast cancer survivors with and without chronic diseases. The symptom scores seemed to be more impacted than function scores, which might be due to the defensive function of fat. In some domains of the significant increases of QOL in overweight group, the absolute values of score increments were less than 5 points. Osoba et al38. recommended that a difference of more than 5 points on the 0–100 scale were considered as a clinically important difference. Maringwa JT et al39. suggested that 5 to 10 units of the QLQ-C30 scales might be used as guidance for clinicians and researchers to classify patients as improved or deteriorated in QOL and symptoms over time, and hence to determine the proportion of patients benefiting from treatment. Since we did not regard BMI as a clinical treatment for the breast cancer survivors, we think the differences in the QOL score in BMI categories still had great significance for readers and should be aware of. It may be useful in directing intervention efforts for improving QOL.
For the aspects of overweight and obesity, people usually associate them with worse outcomes, while their prevalence increasing worldwide. There had been numerous studies40,41,42 which reported that overweight and moderately obese patients had a lower mortality rate and a better survival. This counterintuitive result - a new review of being overweight or obese - was called “obesity paradox”43. In the previous studies of BMI and QOL, the “obesity paradox” phenomenon has been found existed in healthy people44,45,46 and people with chronic diseases46,47,48. Our results suggest that the “obesity paradox” phenomenon also existed in breast cancer survivors in China. The positive influence of being overweight on QOL in breast cancer survivors remains somewhat debatable due to specific limitations in the present study. Nutritional factors might contribute to this positive effect. Diseases and treatments could weaken the patients’ strength and make them more fragile, while overweight patients might have certain resistance to this. On the other hand, obese people were less likely to suffer from depressive symptoms compared with those with normal weight49, which supported the “liberal mind brings health” or “jolly fat” hypothesis. A positive attitude could also be beneficial to QOL. Although a series of hypotheses had been put forward to explain the “obesity paradox”50, the underlying reasons and the biological mechanisms for the increased QOL among overweight and even obese breast cancer survivors still remained elusive. Further research was needed to explore the reasons for these phenomena.
We also found that: underweight impaired the QOL of breast cancer survivors, which was consistent with previous researches46,51,52,53. Although our results showed that obese breast cancer survivors with one or more chronic diseases had a similar QOL compared with normal weight ones in almost all scales, the overall scores decreased significantly, which was consistent with other studies which included that chronic diseases could impair QOL35. Considering obesity was the confirmed risk factor for chronic diseases, being slightly overweight is recommended for breast cancer survivors.
Some limitations of this study should be addressed. This study was a cross-sectional survey and the participants might only represent for the breast cancer survivors in China. The BMI was calculated from the basis of breast cancer survivors self-reported body weight and height, which might cause certain errors and misclassifications. Nevertheless, the results of Dekkers et al. indicated that self-reported BMI was competently accurate to evaluate the prevalence of overweight/obesity in a middle-aged overweight working population54. The association between breast cancer and BMI was different in pre and post-menopausal women, as well as side effects of cancer treatment that affected QOL. Unfortunately, we did not collect the information of menopause in our questionnaire, we would like to carry out a more extensive study on the question in the future. In spite of these limitations, our results from large population-based study may be useful in directing intervention efforts for improving QOL and provide a reference and foundation for future researches.
Conclusions
Through large population-based cross-sectional study, we observed significantly increasing trend of BMI associated with QOL for women with breast cancer in China. Overweight breast cancer survivors had a significantly better QOL than survivors with a BMI below 25 Kg/m2. Both underweight and obese breast cancer survivors showed impaired QOL, and further research focus should lie on them.
References
Seidell, J. C. & Halberstadt, J. The Global Burden of Obesity and the Challenges of Prevention. Annals of Nutrition & Metabolism 66, 7–12 (2015).
Doehner, W., Clark, A. & Anker, S. D. The obesity paradox: weighing the benefit. European Heart Journal 31, 146 (2010).
pmhdev, PubMedHealth. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Jama 309, 71–82 (2013).
Romero-Corral, A. et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. The Lancet 368, 666–678, https://doi.org/10.1016/s0140-6736(06)69251-9 (2006).
Gelber, R. P. et al. Measures of Obesity and Cardiovascular Risk Among Men and Women. Journal of the American College of Cardiology 52, 605 (2008).
Bianchini, F., Kaaks, R. & Vainio, H. Overweight, obesity, and cancer risk. Lancet Oncology 3, 565 (2002).
Key, T. J., Appleby, P. N., Reeves, G. K. et al. Endogenous Hormones Breast Cancer Collaborative, Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. Journal of the National Cancer Institute 95, 1218–1226 published online EpubAug20 (2003).
Wing, R. R. et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34, 1481 (2011).
Fonarow, G. C., Srikanthan, P., Costanzo, M. R., Cintron, G. B. & Lopatin, M. An obesity paradox in acute heart failure: analysis of body mass index and inhospital mortality for 108,927 patients in the Acute Decompensated Heart Failure National Registry. American Heart Journal 153, 74 (2007).
Miyagishima, K. et al. Body Mass Index (BMI) and Prognosis in Patients With Chronic Heart Failure. Journal of Cardiac Failure 14, S176–S176 (2008).
Oreopoulos, A., Padwal, R. Z., Fonarow, K. G., Norris, C. & Mcalister, F. Mcalister, Body mass index and mortality in heart failure: a meta-analysis. American Heart Journal 156, 13–22 (2008).
Kennedy, L. M. et al. The prognostic importance of body mass index after complicated myocardial infarction. Journal of the American College of Cardiology 45, 156 (2005).
Uretsky, S. et al. Obesity Paradox in Patients with Hypertension and Coronary Artery Disease. American Journal of Medicine 120, 863–870 (2007).
S. Information. HOT TOPICS ORIGINAL: Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. http://www.e-medicum.com/newsletters/fcmunlp/verNoticia.php?noticia=59399.
Romero-Corral, A. et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet (London, England) 368, 666 (2006).
Chen, W. et al. Cancer statistics in China, 2015. CA: a cancer journal for clinicians 66, 115–132; published online EpubMar-Apr (https://doi.org/10.3322/caac.21338) (2016).
Chen, W., Zheng, R., Incidence,mortality and survival analysis of breast cancer in China. Chinese Journal of Clinical Oncology (2015).
Abrahamson, P. E. et al. General and abdominal obesity and survival among young women with breast cancer. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 15, 1871 (2006).
Ul-Haq, Z., Mackay, D. F., Fenwick, E. & Pell, J. P. Meta-analysis of the association between body mass index and health-related quality of life among adults, assessed by the SF-36. Obesity 21, E322–327; published online EpubMar (https://doi.org/10.1002/oby.20107) (2013).
Coakley, E. H. et al. Lower levels of physical functioning are associated with higher body weight among middle-aged and older women. Int J Obes Relat Metab Disord 22, 958–965 (1998).
W., Y. Jr, Olsen, M. K., Westman, E. C., Bosworth, H. B. & Edelman, D. Relationship between obesity and health-related quality of life in men. Obes Res 10, 1057–1064 (2002).
Pimenta, F. B. C., Elodie, B., Mograbi, D. C., Helene, S. & Landeira-Fernandez, J. The relationship between obesity and quality of life in Brazilian adults. Frontiers in Psychology 6, 966 (2015).
Kwan, M. L. et al. Pre-diagnosis body mass index and survival after breast cancer in the After Breast Cancer Pooling Project. Breast cancer research and treatment 132, 729–739; published online EpubApr (https://doi.org/10.1007/s10549-011-1914-3) (2012).
Friedenreich, C. M., Review of anthropometric factors and breast cancer risk. European journal of cancer prevention: the official journal of the European Cancer Prevention Organisation 10, 15–32; published online EpubFeb (2001).
Hastie, C. E. et al. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. Eur Heart J 31, 222–226; published online EpubJan (https://doi.org/10.1093/eurheartj/ehp317) (2010).
Van den Brandt, P. A. et al. Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. American journal of epidemiology 152, 514–527; published online EpubSep15. (2000).
Katz, D. A., Mchorney, C. A. & Atkinson, R. L. Impact of Obesity on Health-related Quality of Life in Patients with Chronic Illness. Journal of general internal medicine 15, 789 (2000).
Aaronson, N. K. et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. Jnci Journal of the National Cancer Institute 85, 365–376 (2005).
Sprangers, M. A. et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. Journal of Clinical Oncology Official Journal of the American Society of Clinical Oncology 14, 2756 (1996).
Fayers, P. M., Aaronson, N. K., Bjordal, K., The EORTC QLQ-C30 scoring manual (2001).
Tang Zheng, W. J.-w., Jin-ming, Y. U., et al. QLQ-BR23 and EORTC + QLQ-C30 for measurement of the impact of rehabilitation exercise on quality of life in breast cancer patients. Fudan Univ J Med Sci (2015).
World Health Organization. BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html (2017).
Schemper, M. The relative importance of prognostic factors in studies of survival. Statistics in medicine 12, 2377–2382; published online EpubDec30 (1993).
Bradley, C. J., Given, C. W. & Roberts, C. Race, socioeconomic status, and breast cancer treatment and survival. Journal of the National Cancer Institute 94, 490–496 (2002); published online EpubApr03.
Burström, K., Johannesson, M. & Diderichsen, F. Health-related quality of life by disease and socio-economic group in the general population in Sweden. Health Policy 55, 51–69 (2001).
Supranowicz, P. et al. The risk of overweight and obesity in chronic diseases among Warsaw inhabitants measured by self-reported method. Roczniki Państwowego Zakadu Higieny 64, 197–203 (2013).
Fu, P. et al. Study on the relationship between body mass index and risk factors of chronic diseases of Beijing urban residences. Wei Sheng Yan Jiu 32, 363–366 (2003).
Osoba, D., Rodrigues, G., Myles, J., Zee, B. & Pater, J. Interpreting the significance of changes in health-related quality-of-life scores. Journal of Clinical Oncology Official Journal of the American Society of Clinical Oncology 16(1), 139 (1998).
Maringwa, J. T. et al. Minimal important differences for interpreting health-related quality of life scores from the eortc qlq-c30 in lung cancer patients participating in randomized controlled trials. Supportive Care in Cancer 19(11), 1753–1760 (2011).
Jee, S. H. et al. Body-mass index and mortality in Korean men and women. The New England journal of medicine 355, 779–787; published online EpubAug24 (https://doi.org/10.1056/NEJMoa054017) (2006).
Auyeung, T. W. et al. Survival in Older Men May Benefit From Being Slightly Overweight and Centrally Obese—A 5-Year Follow-up Study in 4,000 Older Adults Using DXA. Journals of Gerontology.series A.biological Sciences & Medical Sciences 65A, 99–104 (2010).
Wu, S. et al. Association of obesity and overweight with overall survival in colorectal cancer patients: a meta-analysis of 29 studies. Cancer Causes & Control 25, 1489–1502 (2014).
Gruberg, L. et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol 39, 578–584; published online EpubFeb20 (2002).
Lópezgarcía, E. et al. Relation between body weight and health-related quality of life among the elderly in Spain. International Journal of Obesity 27, 701–709 (2003).
Zhu, Y. B., Luo, X. X. & Wang, Q. Study on the relationship between body mass index and health-related quality of life in middle-aged or older Chinese adults. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi 30, 687 (2009).
Zhu, Y. et al. Association between Body Mass Index and Health-Related Quality of Life: The “Obesity Paradox” in 21,218 Adults of the Chinese General Population. PloS one 10, e0130613, https://doi.org/10.1371/journal.pone.0130613) (2015).
Ulhaq, Z., Mackay, D. F., Fenwick, E. & Pell, J. P. Meta-analysis of the association between body mass index and health-related quality of life among adults, assessed by the SF-36. Obesity 21, E322 (2013).
Yan, L. L. et al. BMI and health-related quality of life in adults 65 years and older. Obes Res 12, 69–76; published online EpubJan (https://doi.org/10.1038/oby.2004.10) (2004).
Li, Z. B. et al. Obesity and depressive symptoms in Chinese elderly. International journal of geriatric psychiatry 19, 68–74; published online EpubJan (https://doi.org/10.1002/gps.1040) (2004).
Flegal, K. M., Kalantar-Zadeh, K., Overweight, mortality and survival. Obesity 21, 1744–1745; published online EpubSep (https://doi.org/10.1002/oby.20588) (2013).
Wee, H. L. et al. The association of body mass index with health-related quality of life: an exploratory study in a multiethnic Asian population. Value in health: the journal of the International Society for Pharmacoeconomics and Outcomes Research 11(Suppl 1), S105–114; published online EpubMar (https://doi.org/10.1111/j.1524-4733.2008.00374.x) (2008).
Søltoft, F., Hammer, M. & Kragh, N. The association of body mass index and health-related quality of life in the general population: data from the 2003 Health Survey of England. Quality of Life Research 18, 1293 (2009).
WM, H. et al. C. R. Group, The association between body mass index and health-related quality of life: data from CaMos, a stratified population study. Quality of Life Research 16, 1595–1603 (2007).
Dekkers, J. C., Van Wier, M. F., Hendriksen, I. J., Twisk, J. W., Van Mechelen, W. Accuracy of self-reported body weight, height and waist circumference in a Dutch overweight working population. BMC medical research methodology 8, 69; published online EpubOct28 (https://doi.org/10.1186/1471-2288-8-69) (2008).
Acknowledgements
We thank the study participants and the research staff for their contribution to this project. This work was supported by the National Social Science Foundation of China [grant number 13CSH076]; and Shanghai Municipal Commission of Health and Family Planning [grant number 20134068].
Author information
Authors and Affiliations
Contributions
Jinming Yu and Jiwei Wang formulated the overarching research goals and aims. Juan Xia analyzed the study data and wrote the main manuscript text. Zheng Tang, performed the research, collected the data and review and revision the mauscript. Qinlong Deng participated the investigation and collected the data.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xia, J., Tang, Z., Deng, Q. et al. Being slightly overweight is associated with a better quality of life in breast cancer survivors. Sci Rep 8, 3022 (2018). https://doi.org/10.1038/s41598-018-20392-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-20392-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.