Abstract
In this article, we offer an artificial intelligence method to estimate the carotid-femoral Pulse Wave Velocity (PWV) non-invasively from one uncalibrated carotid waveform measured by tonometry and few routine clinical variables. Since the signal processing inputs to this machine learning algorithm are sensor agnostic, the presented method can accompany any medical instrument that provides a calibrated or uncalibrated carotid pressure waveform. Our results show that, for an unseen hold back test set population in the age range of 20 to 69, our model can estimate PWV with a Root-Mean-Square Error (RMSE) of 1.12 m/sec compared to the reference method. The results convey the fact that this model is a reliable surrogate of PWV. Our study also showed that estimated PWV was significantly associated with an increased risk of CVDs.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) and stroke are among the major causes of death in the United States and the total cost related to them was more than $316 billion in 2011–20121,2. New cardiovascular monitoring methods are urgently needed in order to limit the growing burden of CVDs. Arterial stiffening is one of the risk factors for CVDs3,4, which can be assessed non-invasively by calculating the carotid to femoral PWV5. This parameter is a gold standard of arterial stiffness, the rate at which pressure waves move down the aortic vessel6. Increased arterial stiffness is related to an increased risk of cardiovascular events; therefore, it has become an independent marker for CVDs6,7. Because of its clinical significance, there has been a surge in addressing arterial stiffness and PWV8. Arterial stiffness and its surrogates such as PWV have been suggested as one of the risk factors along with other biomarkers such as high cholesterol, diabetes, and left ventricular hypertrophy when cardiovascular risk is being evaluated8. Past studies have shown a strong correlation between PWV and the presence of CVDs9,10,11,12,13,14.
Although carotid-femoral PWV measurement is non-invasive, this process is intrusive as it requires the waveform collection from inguinal region. Obtaining accurate carotid-femoral PWV measurements often requires a well-trained staff within a clinical setting15. The need of the medical community is an easy-to-use and non-intrusive method to measure carotid-femoral PWV with acceptable accuracy and precision; see ref.16.
At the same time, recent advances in the field of artificial intelligence have opened up new areas and methods in creating novel modeling and predictive methods for clinical use17. The model and analysis in this paper are in accord to this path of introducing artificial intelligence to the field of medical sciences.
In this study, a novel, easy-to-use, and non-invasive approach to estimate carotid-femoral PWV, from a single carotid waveform measurement, is explored. This method is based on the newly developed Intrinsic Frequency (IF) algorithm18,19. IF method solely needs one uncalibrated trace of a carotid, or aortic, pressure waveform. Our method takes an uncalibrated trace of carotid pressure waveform and performs IF analysis and basic signal processing on it. Then, it combines the results of these analyses with easy-to-obtain clinical parameters such as age. Finally, it models the PWV by neural networks through bootstrap averaging. The main advantages in having an estimated PWV from an uncalibrated carotid pressure waveform, with few typical clinical variables such as blood pressure, would be that it is does not need an ECG measurement nor a femoral tonometry recording. As a result, it is easier, and potentially can be done by a smart phone as we have shown in our previous publication20.
Data Description
We used the Framingham Heart Study (FHS) data, a longitudinal epidemiological cohort analysis, in this manuscript21. The participants were part of FHS Cohorts Gen 3 Exam 122, Offspring Exam 723, and Original Exam 2624. They underwent a comprehensive, noninvasive assessment of central hemodynamics generating a successful collection of a total of N = 6698 tonometry recordings. The recorded PWV measurements were calculated using a simultaneous right carotid tonometry pressure waveform with electrocardiogram recording and a right femoral tonometry pressure waveform with electrocardiogram recording combined with body surface measurements of the participants7. This method of measuring is sometimes called the sequential measurement25. One can find a comparison of this method to the reference method of measuring PWV in25. For a broader description regarding FHS data, please see7 and references contained within.
Some participants had missing or erroneous tonometry waveforms data. We marked these recordings as “faulty record” (N = 1011). From the rest of the data (N = 5687), some recorded PWV measurements had values equal to or greater than 30 m/sec, or even 0 m/sec. We considered these values to be “measurement error” (N = 21). We also excluded the population of age greater than 70 (N = 661) to minimize the CVD treatment effects. Also, we know that individuals having an age of 70 or greater already experience arterial stiffness due to age factor. These filterings led to a total of N = 5020 usable observations. Furthermore, for the prognostics study, we excluded individuals having cardiovascular diseases prior to, or on, their tonometry exam date leading to N = 4798 participants.
Artificial Intelligence Methodology
General Signal Processing
Each uncalibrated tonometry recording from the FHS data included a 10 to 20 second trace. Some of the signal processing parameters were provided by FHS data. For example the unit-less variables Augmentation Index (AIx) and Mean Carotid Shape Factor (MCSF) were included as they were provided (See26 and references contained within). As a quick reference, MCSF is the average value of an arterial cardiac cycle signal normalized by its range. Furthermore, Reflected Wave Arrival Time (RWAT) was also among the variables that FHS had provided with the data (See26 and references within).
However, to use the IF algorithm, we had to extract arterial cycles from the raw signal.
At first, a short-window moving average was used to eliminate the unwanted noise from the signals. The window size was taken to be 0.02 sec. This window size would eliminate noise levels above ~50 Hz. The blood pressure waveform can be encoded with frequencies less than ~25 Hz (50 Hz is twice this value)27. In mathematical terms, the moving average \(\bar{s}(t)\) we used in our study, for a signal s(t), can be expressed as
Our method is not dependent on this choice of noise-filtering and other low-pass filtering approaches could also be used. Then the signals were normalized to remove the effects of breathing and other artificial motions. The normalization was performed using the location of maxima and minima of each recording28. We then used a modified version of the automatic cycle selection introduced in29 to pick cycles. Dicrotic notch was found based on the derivatives and filtering of the picked cycles28. These cycles were then fed into the IF algorithm.
Intrinsic Frequency
A typical arterial pressure waveform consists of a systolic and diastolic part. The systolic part is when the aortic valve is open and heart is pumping blood into the aorta and arterial system. The diastolic part is when the aortic valve is closed preventing the blood from re-entering the left ventricle. The closure of the aortic valve, on the pressure waveform trace, is commonly called the dicrotic notch. The IF method18,19 assumes that there are two constant dominant dynamical frequencies before and after the closure of the aortic valve. These frequencies are called Intrinsic Frequencies (IFs). This method does not need a calibrated aortic or carotid pressure signal; and can even be applied to signals collected by a smart phone20.
In the IF method18,19, it is assumed that the instantaneous frequencies are piecewise constant throughout the cardiac cycle. The dicrotic notch separates these frequencies. For an aortic pressure waveform, the IF problem can be formulated as
with a continuity condition at T0 (the time of the dicrotic notch) and periodicity at T (the duration of the cardiac cycle). Here, the indicator function is defined as
Also, a1, b1, a2 and b2 are the envelopes of the IF model fit. ω1 and ω2 are Intrinsic Frequencies (IFs) of the waveform. Further, \(\bar{p}\) is the mean pressure for the period [0, T). The goal of the IF model (2) is to extract a fit, called Intrinsic Mode Function (IMF), that carries most of the energy (information) from a pressure waveform s(t) in one period. The latter is done by solving the following optimization problem19:
Here, \({\Vert \Vert }_{2}\) is the L2-norm defined on [0, T). One assumption in this optimization is that the extracted IMF is continuous at the dicrotic notch time T0 (the first condition in (5)). The other assumption is that the extracted IMF is periodic (the second condition in (5)). The method of the solution of the optimization problem mentioned by (4) and (5) can be found in19.
Statistical Learning
Dimensionless parameters or combinatorial mixtures can be extracted from the solutions of (4) and (5). These parameters are both of mathematical and physiological importance as shown in our recent work of noninvasive iPhone measurement of left ventricular ejection20. For example, we can normalize ω1 and ω2 with respect to systolic and diastolic periods, T0 and T − T0 respectively20. Even, we can normalize ω1 and ω2 by the whole cardiac cycle T. In fact, there is a systematic way to create new variables from a set of given features. We have used the method introduced in30 to create new features from ω1, ω2, T, and T − T0. Some of the outputs of this method were used in our PWV model.
The original set of variables used for feature extraction included IFs and their variants, carotid waveform shape factors such as reflected wave arrival time and augmentation index, and clinical features and blood pressure and age. We specifically used the mentioned clinical variables since a 2010 study published by European heart journal has emphasized that PWV is affected by age and blood pressure31. In short, the original set of features is
In (6), we have constructed new features from {ω1, ω2, T, T − T0}. To be more specific, we used the methodology introduced in30 and field expert knowledge to introduce
Furthermore, in (6), MCSF is the mean carotid shape factor, AIx is the augmentation index, SSN is the supra-sternal notch to femoral site length, RWAT is the reflected wave arrival time for a cardiac arterial waveform cycle, Age is the age of the participant at the time of tonometry reading, P s is the brachial systolic pressure, and P d is the brachial diastolic pressure.
In order to provide the most useful subset of these variables into the PWV model, we applied a combination of best subset variable selection methods based on multi-linear regression32. Using this approach, we ended up with the variables set
After this stage, we kept 20% of the data as a hold back test set (N = 1004). The other part was kept as a train set (N = 4016). These sets were picked at random from the original data. However, we chose them in a uniform way such that, both in train and test sets, the PWV distribution would follow the population distribution.
After this stage, on the train set, we performed a bootstrap aggregation (bagging) without replacement (sub-sampling)33 having single layer neural networks at the base regressors with a total number of |V| neurons in each network. Here, |V| is the number of elements in V. The bagging was conducted with sampling 66% at each iteration. A total number of 1000 iteration was used. It is needless to mention that one could stop the iterations when the out-of-bag RMSE reaches a plateau. At each iteration, the neural networks were trained for 100 epochs. A squared penalty of 0.01 was used to prevent over-fitting at each iteration. MATLAB implemented Levenberg-Marquardt backpropagation was used in training the neural nets34,35,36.
The whole machine learning pipeline can be expressed as follows:
-
1.
The uncalibrated waveforms where analysed to extract cardiac cycles;
-
2.
IF parameters and waveform features, such as shape factors, were extracted from the selected cardiac cycles;
-
3.
The waveform features were blended in with the routine clinical parameters to construct the original set of features V0;
-
4.
The best subset variable selection method was applied to reduce the dimensionality of the feature-space, namely V;
-
5.
A sub-sampled bagged system of neural networks was trained and tested.
To further analyze our method and the effectiveness of estimated PWV, we conducted a prospective cohort study and used proportional hazards regression models to evaluate the association between PWV and incident CVD. We evaluated this relationship for PWV measurements as well as for estimated PWV values produced by our noninvasive IF method. Subsequently, we compared the hazards of PWV for CVD with that of estimated PWV. Baseline population consisted of participants free from CVDs. Adjusted models included components from Framingham risk score: sex, age, total cholesterol, HDL cholesterol, blood pressure, diabetes and smoking. Smoking was defined as regular usage within the last 12-months prior to the examination date. The assumption of proportionality was met. All continuous variables were log transformed to address skewness. Predictive value was evaluated via likelihood ratio test and the Akaike Information Criterion (AIC). Only complete cases without missing data were studied. Kaplan-Meier plots of cumulative probability of a first major CVD event were constructed for PWV and also for estimated PWV, when participants were grouped according to tertiles of PWV and tertiles of estimated PWV. Log rank test was used to compare the unadjusted Kaplan-Meier curves. p-values < 0.05 were considered as significant.
Results and Discussion
PWV Model Results
The population demographics of these variables are shown in Table 1. Convergence of the ensemble of the models was guaranteed by a flat RMSE plot, of both train (RMSE = 1.04) and test (RMSE = 1.12) sets, over the total number of iterations, Fig. 1. The 0.09 gap between the train and test sets, in Fig. 1, shows that the model has an acceptable generalization capability. The total RMSE, on the whole dataset including the train and test sets, was 1.05 m/sec. Our simulations with Decision Tree (DT), boosted DT, boosted Neural Networks33 show similar but marginally larger RMSE values.
The estimated PWV versus the measured values are plotted in Fig. 2. Our model’s correlation of the estimated PWV with respect to FHS sequential measured PWV is 0.85. The Bland-Altman plot of the results is shown in Fig. 3. The limits of agreement are approximately ±2.07.
Prognosis Results
Study exclusion criteria resulted in a sample of 4798 usable observations, which included individuals 19 to 69 years old without CVD at the baseline examination. The characteristics of the study sample are presented in Table 2. Within a follow up period of 10 years, 171 participants had a CVD event. Cox proportional hazards models for PWV and estimated PWV are presented in Table 3. After adjusting for standard risk factors, both PWV and estimated PWV were significantly associated with an increased risk for a first major CVD event. Rounding for two digits after zero, the Hazard Ratio (HR) PWV is 4.00, with p = 0.0002, and the HR of the estimated PWV is 4.43, with p = 0.008.
Model Error Analysis
We can observe, from Figs 2 and 3, that as PWV goes above 12 m/sec the error starts to increase. It is both because of the inherent measurement error37,38,39,40 and also sparsity of data in that region. For smaller values of PWV, this behavior is less pronounced as data concentration is higher and also the measurement errors are smaller.
We can estimate the error of our model compared to the reference method25 of simultaneous tonometry measurement of PWV. Assign the presented model output with the random variable PWV predicted . Also, one can label the FHS measured PWV values with the random variable PWV measured . On the other hand we can name the reference values as PWV ref . Based on the results of our model, the error of our model with respect to the sequential measurement of PWV is 1.05 m/sec. In other words,
where std() is the standard deviation operator. From the model results, we also have
where \({\mathbb{E}}()\) is the expected value operator. Assuming that the error of the sequential PWV measurement is equal to the PulsePen device41,42, explained in25, we can state
It is logical to state that the error between the reference and sequential methods is independent from the error between our model and sequential methods. As a result, using this fact and Equations (17)–(20), we can deduce that
In other words, the estimation error, using the model presented in this paper, is approximately 1.1 m/sec. This analysis shows that our model is a reliable surrogate of PWV25.
Comparison to other methods
Our model generated results similar to other non-invasive devices and/or methods currently in use, such as Complior43, PulseTrace44 and Oscillometric45.
With Complior, there is simultaneous measurement of the pressure pulse. The technician places one probe at the patient’s carotid location and a second probe at the femoral location. Then the distance between these two locations is calculated and entered into Complior software. Cuff blood pressure is also measured and entered into the software. PWV measures are subsequently generated after a proprietary algorithm is used to measure the pulse transit time between the two locations. With PulseTrace, the stiffness index is estimated by analyzing the photoplethysmographic waves obtained on the fingertip of the individual. The index is calculated by dividing the height of the participant by the time delay between the first systolic peak and the early diastolic peak of the signal. In a study led by Salvi et al. in 200825, on a population of 50 participants (aged between 20–84) free from cardiac arrhythmia, these devices produced the following outputs when compared to the reference tonometry method in which waveforms were simultaneously acquired: Complior Bias = 2.09 m/sec and LoA = ±2.68 m/sec, r = 0.83 and PulseTrace Bias = −1.2 m/sec, LoA = ±4.92 m/sec, r = 0.55. Although these devices are non-invasive, they are relatively expensive and the procedure is time consuming.
In a prospectively designed validation study led by Feistrizer et al.46, aortic PWV estimates from oscillometric technique were generated from 40 participants free of CVDs between 24 and 55 years old. These measurements were compared to the aortic PWV values produced by the reference method of cardiac magnetic resonance. Analysis of agreement between the two methods showed Bias = 0.57 m/sec, LoA = ±1.92 m/sec m/sec and r = 0.86. In the aforementioned study, only 28% of the participants were females and the median age of the cohort was 34 years. According to the authors of the paper, the study population does not meet the Artery Society guideline’s for PWV validation. In specific, the Artery Society needs a homogeneous sex distribution (a minimum of 40% for either sex) as well as a homogeneous distribution along the age groups. Another study designed by Hametner et al.45, compared oscillometric estimations of aortic PWV against intra-aortic arterial PWV measurements using a population of 120 patients undergoing elective cardiac catheterization for suspected coronary artery disease (22 patients with age ≤ 50 years old and 29 patients with age ≥ 70 years old). Exclusion criteria consisted of unstable clinical conditions, arrhythmias and valvular heart disease. In their work, to estimated PWV a number of variables from pulse wave analysis and wave separation were combined in a mathematical model in which the major determinants were age, central pressure and aortic characteristic impedance. The following results were then reported by the authors: Bias = 0.43 m/sec, LoA = ±2.45 m/sec with a correlation of r = 0.81. This study also does not follow the Artery Society guidelines as only 10% of participants were females.
In a recent study by Campo et al.47, it is shown that the aortic PWV can be measured non-invasively with a bathroom scale. The authors combined the principles of ballistocardiography and impedance plethysmography on a single foot to estimate the aortic PWV. They compared their PWV estimations to measured PWV s, on a group of 205 participants. On the validation set, they reported r = 0.7, Bias = 0.25 m/sec, and LoA = [−2.48, 2.98]. According to the authors, this new technique presents a few limitations including the gait instability, which affects more frail elderly and some neurological diseases. Other types of diseases may also influence the applicability of the measurement, like for example atrial fibrillation or skin diseases. The population study had several exclusions too. For example, pregnant participants or participants that had morbid obesity (BMI > 35) were excluded.
In another recent publication48, Greve et al. argued that the need for a non-invasive PWV estimation is imminent because of the relative inaccessibility of devices such as high-quality applanation tonometry. They have proposed using an equation based on age and mean arterial pressure to perform the estimation. They show that in a healthy group without cardiovascular risk factors, the correlation of the estimation with measured values is r = 0.52. This could be seen as a major limitation of that study. Furthermore, they showed that in an apparently healthy patients with cardiovascular risk factors the correlation is r = 0.67. Finally, within the group with known CVDs, the correlations is reported to be very low (r = 0.37). They also concluded that the estimated PWV could predict cardiovascular events independently of the traditional cardiovascular risk factors. However,in another smaller study49, Greve et al. claimed that the estimated PWV only predict CVDs in apparently healthy individuals. Moreover, the estimated PWV reclassifies apparently healthy participants to a higher risk category.
Innovative aspects of proposed method
The above results show that the estimated PWV by Intrinsic Frequencies has the potential to become a reliable non-invasive method of PWV measurement. Compared to Complior, PulseTrace and Oscillometric, the IF technique is less intrusive and easier to operate that offers a more practical solution to PWV estimations.
The presented study uses an artificial intelligence technique to render an accurate estimation of central arterial stiffness (carotid-femoral PWV). The sample size used in this study is large enough and includes both healthy and CVD volunteers to offer an adequate statistical power. This study also uses a homogeneous age and gender distribution population.
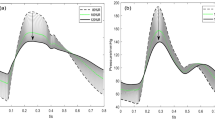
We further analyzed our results based on the Artery Society guidelines for validation of non-invasive hemodynamic measurement devices50. We subsequently excluded the following from our results before generating updated Bland-Altman plots: individuals with a BMI 30 (due to problems regarding the measurement of an accurate path length) and PWV ≥ 15. The updated results after the fore-mentioned filtering were: Bias = 0.03 m/sec, LoA = ±1.76 m/sec (SD = 0.88); see Figs 4 and 5. These outputs would be graded as acceptable by the Artery Society.
Risk Evaluation
The results, see Table 3, suggest that PWV and our estimated PWV both convey comparable risks for incident CVD in a model adjusted for standard risk factors. The use of Kaplan-Meier failure method showed that when participants were grouped according to tertiles of PWV, the probability of developing a CVD event increased with the group displaying higher PWV values (log-rank test p < 0.0001); see Fig. 6. The same observation was made when participants were grouped by tertiles of the estimated PWV. The group with estimated PWV of 7.86 m/sec or higher was at an increased risk of developing a CVD event (log-rank test p < 0.0001); see Fig. 7. These results show that estimated PWV by Intrinsic frequencies is as effective as PWV measurements obtained by direct methods, such as sequential method, in predicting the risk for CVD.
Model Performance
Following the Kaplan-Meier failure method analysis, we segmented the PWV data into three different groups, to check the model performance for different subsets according to PWV values. Figure 8 shows that in all three tertiles PWV ≤ 6.5, 6.5 ≤ PWV ≤ 7.9 and PWV ≤ 7.9, the model presented in this paper has an acceptable performance.
PWV model Bland-Altman for tertiles. All axes have units of m/sec. The tertiles are coming from the Kaplan-Meier analysis of the original PWV values. The upper-left plot is the Bland-Altman for PWV ≤ 6.5. The upper-right plot is for 6.5 < PWV < 7.9. The lower-left plot is the Bland-Altman for 7.9 ≤ PWV. All three different tertiles show that the model presented in this paper have an acceptable performance.
Study Limitations
The major limitations of this study are:
-
1.
The population used in this study was not racially diverse (mostly Caucasian). For a more general conclusion, we need to have a more diverse study population.
-
2.
The automatic cycle selection, used in this study, is prone to mis-identification of cardiac cycles and dicrotic notches. However, the effect of the related error on overall finding of this study is insignificant.
-
3.
The sequential method used to calculate the PWV might depict error either in body surface measurements of wave travel times at high PWV values.
Conclusions
In this paper, we have introduced a novel artificial intelligence method to estimate the carotid-femoral pulse wave velocity. This method is based on the newly introduced Intrinsic Frequency method19 and as inputs uses only an uncalibrated carotid pressure waveform with typical clinical variables such as blood pressure.
The main advantages in having an estimated PWV from an uncalibrated carotid pressure waveform, with few typical clinical variables such as blood pressure, would be that it is does not need an ECG measurement nor a femoral tonometry recording. As a result, it is easier, and potentially can be done by a smart phone as we have shown in our previous publication that carotid waveform can be easily measured using a regular iPhone camera20.
Here, in this article, we have been able to address the need of estimating PWV by providing an accurate and precise statistical model estimating pulse wave velocity. The model presented in this manuscript can estimate PWV with an RMSE of 1.12 m/sec, compared to the reference method.
We have provided an error analysis and comparison to other methods currently in use in order to support the conclusion that the presented model is an acceptable surrogate for arterial stiffness. Furthermore we conducted a prospective investigation to analyze the predictive value of estimated PWV in relation to the onset of CVDs. Our study showed that estimated PWV was significantly associated with increased risk of CVDs.
Data Availability
The data used in this study can be requested from FHS directly. It is publicly available to qualified investigators. An approved research proposals could be qualified to receive the de-identified data. FHS data, in general, can be requested by a research application submission to one of the following:
-
Directly from Framingham Heart Study (https://www.framinghamheartstudy.org/), BioLINCC (https://biolincc.nhlbi.nih.gov/home/), or
-
dbGaP (https://www.ncbi.nlm.nih.gov/gap).
The manuscript data can be found using the following links:
-
1.
(https://biolincc.nhlbi.nih.gov/studies/gen3/?q=framingham) - Gen3 cohort
-
2.
(https://biolincc.nhlbi.nih.gov/studies/framcohort/?=framingham) - Original Cohort
-
3.
(https://biolincc.nhlbi.nih.gov/studies/framoffspring/?q=framingham) - Offspring Cohort.
Research Ethics
All experiments and procedures were reviewed and approved by FHS. The Framingham Heart Study is conducted and supported by the National Heart Lung, and Blood Institute (NHLBI) in collaboration with Boston University (Contract No. N01- HC-25195).
Permission to Carry Out Fieldwork
This study did not have fieldwork.
References
Lloyd-Jones, D. et al. Heart disease and stroke statistics 2010 update. Circulation 121, e46–e215 (2010).
Mozaffarian, D. et al. Executive summary: Heart disease and stroke statistics-2016 update: A report from the american heart association. Circulation 133, 447 (2016).
Laurent, S. et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 37, 1236–1241 (2001).
Sutton-Tyrrell, K. et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 111, 3384–3390 (2005).
Laurent, S. et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. European heart journal 27, 2588–2605 (2006).
Mitchell, G. F. et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women the framingham heart study. Hypertension 43, 1239–1245 (2004).
Mitchell, G. F. et al. Arterial stiffness and cardiovascular events the framingham heart study. Circulation 121, 505–511 (2010).
Townsend, R. R. Arterial stiffness: recommendations and standardization. Pulse 4, 3–7 (2016).
Blacher, J. et al. Impact of aortic stiffness on survival in end-stage renal disease. Circulation 99, 2434–2439 (1999).
Choi, C. U. et al. Impact of aortic stiffness on cardiovascular disease in patients with chest pain: assessment with direct intra-arterial measurement. American journal of hypertension 20, 1163–1169 (2007).
Cruickshank, K. et al. Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance. Circulation 106, 2085–2090 (2002).
Hansen, T. W. et al. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 113, 664–670 (2006).
Mattace-Raso, F. U. et al. Arterial stiffness and risk of coronary heart disease and stroke. Circulation 113, 657–663 (2006).
Shokawa, T. et al. Pulse wave velocity predicts cardiovascular mortality. Circulation Journal 69, 259–264 (2005).
Rajzer, M. W. et al. Comparison of aortic pulse wave velocity measured by three techniques: Complior, sphygmocor and arteriograph. Journal of hypertension 26, 2001–2007 (2008).
Pereira, T., Correia, C. & Cardoso, J. Novel methods for pulse wave velocity measurement. Journal of medical and biological engineering 35, 555–565 (2015).
Ramesh, A., Kambhampati, C., Monson, J. & Drew, P. Artificial intelligence in medicine. Annals of The Royal College of Surgeons of England 86, 334 (2004).
Pahlevan, N. M. et al. Intrinsic frequency for a systems approach to haemodynamic waveform analysis with clinical applications. Journal of The Royal Society Interface 11, 20140617 (2014).
Tavallali, P., Hou, T. Y., Rinderknecht, D. G. & Pahlevan, N. M. On the convergence and accuracy of the cardiovascular intrinsic frequency method. Royal Society Open Science 2, 150475 (2015).
Pahlevan, N. M. et al. Noninvasive iphone measurement of left ventricular ejection fraction using intrinsic frequency methodology. Critical care medicine (2017).
Framingham heart study. https://www.framinghamheartstudy.org/. Accessed: (2016).
Splansky, G. L. et al. The third generation cohort of the national heart, lung, and blood institute’s framingham heart study: design, recruitment, and initial examination. American journal of epidemiology 165, 1328–1335 (2007).
Kannel, W. B., Feinleib, M., McNAMARA, P. M., Garrison, R. J. & Castelli, W. P. An investigation of coronary heart disease in families the framingham offspring study. American journal of epidemiology 110, 281–290 (1979).
Dawber, T. R., Meadors, G. F. & Moore, F. E. Jr. Epidemiological approaches to heart disease: The framingham study*. American Journal of Public Health and the Nations Health 41, 279–286 (1951).
Salvi, P. et al. Comparative study of methodologies for pulse wave velocity estimation. Journal of human hypertension 22, 669–677 (2008).
O’Rourke, M. F. & Gallagher, D. E. Pulse wave analysis. Journal of Hypertension-Supplement- 14, S147–S158 (1996).
Fan, Z., Zhang, G. & Liao, S. Pulse wave analysis. In Advanced Biomedical Engineering (InTech, 2011).
Li, B. N., Dong, M. C. & Vai, M. I. On an automatic delineator for arterial blood pressure waveforms. Biomedical Signal Processing and Control 5, 76–81 (2010).
Zong, W., Heldt, T., Moody, G. & Mark, R. An open-source algorithm to detect onset of arterial blood pressure pulses. In Computers in Cardiology, 2003, 259–262 (IEEE, 2003).
Tavallali, P., Razavi, M. & Brady, S. A non-linear data mining parameter selection algorithm for continuous variables. PloS one 12, e0187676 (2017).
Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: establishing normal and reference values. European heart journal 31, 2338–2350 (2010).
Furnival, G. M. & Wilson, R. W. Regressions by leaps and bounds. Technometrics 42, 69–79 (2000).
Friedman, J., Hastie, T. & Tibshirani, R. The elements of statistical learning, vol. 1 (Springer series in statistics Springer, Berlin, 2001).
Demuth, H. B., Beale, M. H., De Jess, O. & Hagan, M. T. Neural network design (Martin Hagan, 2014).
Hagan, M. T. & Menhaj, M. B. Training feedforward networks with the marquardt algorithm. IEEE transactions on Neural Networks 5, 989–993 (1994).
Marquardt, D. W. An algorithm for least-squares estimation of nonlinear parameters. Journal of the society for Industrial and Applied Mathematics 11, 431–441 (1963).
Karamanoglu, M. Errors in estimating propagation distances in pulse wave velocity. Hypertension 41, e8–e8 (2003).
Mestre, C., Lantelme, P., Lievre, M., Gressard & Milon, H. Heart rate: An important confounder of pulse wave velocity assessment. In Journal of Hypertension, vol. 20, S183–S183 (Lippincott Williams & Wilkins 530 Walnut St, Philadelphia, PA 19106-3621 USA, 2002).
Segers, P. et al. Limitations and pitfalls of non-invasive measurement of arterial pressure wave reflections and pulse wave velocity. Artery Research 3, 79–88 (2009).
Weir-McCall, J. R. et al. Effects of inaccuracies in arterial path length measurement on differences in mri and tonometry measured pulse wave velocity. BMC cardiovascular disorders 17, 118 (2017).
Othmane, T. E. H. et al. Effect of sevelamer on aortic pulse wave velocity in patients on hemodialysis: a prospective observational study. Hemodialysis International 11, S13–S21 (2007).
Salvi, P. et al. Validation of a new non-invasive portable tonometer for determining arterial pressure wave and pulse wave velocity: the pulsepen device. Journal of hypertension 22, 2285–2293 (2004).
Complior. http://www.complior.com/products/. Accessed: (2017).
Pulsetrace. http://www.micromedical.co.uk/. Accessed: (2017).
Hametner, B. et al. Oscillometric estimation of aortic pulse wave velocity: comparison with intra-aortic catheter measurements. Blood pressure monitoring 18, 173–176 (2013).
Feistritzer, H.-J. et al. Comparison of an oscillometric method with cardiac magnetic resonance for the analysis of aortic pulse wave velocity. PLoS one 10, e0116862 (2015).
Campo, D. et al. Measurement of aortic pulse wave velocity with a connected bathroom scale. American Journal of Hypertension hpx059 (2017).
Greve, S. V. et al. Estimated carotid–femoral pulse wave velocity has similar predictive value as measured carotid–femoral pulse wave velocity. Journal of hypertension 34, 1279–1289 (2016).
Greve, S. V., Laurent, S. & Olsen, M. H. Estimated pulse wave velocity calculated from age and mean arterial blood pressure. Pulse 4, 175–179 (2016).
Wilkinson, I. B. et al. Artery society guidelines for validation of non-invasive haemodynamic measurement devices: Part 1, arterial pulse wave velocity. Artery Research 4, 34–40 (2010).
Acknowledgements
The Framingham Heart Study is supported by Contract No. HHSN268201500001I from the National Heart, Lung, and Blood Institute (NHLBI) with additional support from other sources. This manuscript was not prepared in collaboration with investigators of the Framingham Heart Study and does not necessarily reflect the opinions or conclusions of the Framingham Heart Study or the NHLBI.
Author information
Authors and Affiliations
Contributions
P.T. conceived of the mathematical and numerical methods of the study; carried out the modeling pipeline design; programmed the cycle-notch selection method; designed and programmed the IF algorithm; designed and programmed the ensemble learning code of the method; helped with finding the optimum hyper-parameters of the ensemble learning code; helped with risk analysis; helped with variable selection; and drafted the manuscript. M.R. conducted the variable selection; conducted the literature survey; found the optimum hyper-parameters of the ensemble learning code; conducted risk analysis; and helped draft and revise the manuscript. N.M.P. helped draft and revise the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Dr. Tavallali had employment agreement with Avicena at the time of the manuscript preparation. Dr. Razavi has employment agreement with Avicena. Dr. Pahlevan has consulting agreements with Avicena.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tavallali, P., Razavi, M. & Pahlevan, N.M. Artificial Intelligence Estimation of Carotid-Femoral Pulse Wave Velocity using Carotid Waveform. Sci Rep 8, 1014 (2018). https://doi.org/10.1038/s41598-018-19457-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-19457-0
This article is cited by
-
Association between insulin resistance and uncontrolled hypertension and arterial stiffness among US adults: a population-based study
Cardiovascular Diabetology (2023)
-
Abdominal aortic aneurysm monitoring via arterial waveform analysis: towards a convenient point-of-care device
npj Digital Medicine (2022)
-
Improving the accuracy and robustness of carotid-femoral pulse wave velocity measurement using a simplified tube-load model
Scientific Reports (2022)
-
Determination of aortic pulse transit time based on waveform decomposition of radial pressure wave
Scientific Reports (2021)
-
E-Health in Hypertension Management: an Insight into the Current and Future Role of Blood Pressure Telemonitoring
Current Hypertension Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.