Abstract
The macrophage migration inhibitory factor (MIF) is a cytokine that plays an important role in inhibiting the growth of pathogenic Mycobacterium tuberculosis (M.tb) and regulates immune responses against M.tb pathogen. MIF -173 G > C gene polymorphism may affect immunity in an individual and leads to susceptibility to tuberculosis (TB). A large number of studies have investigated the relevance of this polymorphism with TB risk, but their results were inconclusive. To obtain a precise conclusion, a meta-analysis was performed by retrieving six eligible studies from Google Scholar, PubMed (Medline), and EMBASE online databases. Overall combined analysis suggested increased TB risk between MIF -173 G > C polymorphism and overall risk in four genetic models, i.e., allelic (C vs. G: p = 0.001; OR = 1.517, 95% CI = 1.312 to 1.753), homozygous (CC vs. GG: p = 0.026; OR = 1.874, 95% CI = 1.079 to 3.257), heterozygous (GC vs. GG: p = 0.001; OR = 1.542, 95% CI = 1.273 to 1.868) and dominant model (CC + GC vs. GG: p = 0.001; OR = 1.631, 95% CI = 1.362 to 1.955). Similarly, increased TB risk was observed in subgroup analysis of Asian ethnicity. No publication bias was observed. These results suggested that MIF -173 G > C variant is a significant risk factor for TB in overall and in Asian populations, and can be used as prognostic marker for TB susceptibility.
Similar content being viewed by others
Introduction
Mycobacterium tuberculosis (M.tb) is the responsible microorganism of tuberculosis (TB) that still remains a second leading cause of death from any infectious disease worldwide. It is estimated that ~2 billion people are affected with M.tb, however only 5–10% of the infected population develop the active form of the disease1. The development of TB is affected by many factors including M.tb virulence, environmental factors, and various other risk factors comprising malnutrition, HIV infection, receipt of immunosuppressive therapy, and diabetes mellitus2. As mentioned earlier, only minority of the infected individuals actually develops clinical disease, this highlights an increased interest in understanding the role of genetic background of M. tuberculosis in infection outcome. Host genetic factors identified, why some people are more or less susceptible to TB infection. Several lines of evidences, including twin studies3, genome-wide linkage studies4, and lately reported genome-wide association studies (GWAS)5,6 have proven that host genetics strongly influences the susceptibility of TB. Hence, understanding the contribution of host genetic factor(s) in the development of TB infection could be proven as an extremely valuable tool in clinical and medicine research, especially because the susceptibility to an infectious agent lies at least partly hidden or masked in inborn errors or immune response7.
Human macrophage migration inhibitory factor (MIF) gene is located on chromosome 22q11.2 and encodes a multifunctional cytokine (MIF) that contributes to innate and adaptive immune responses against the pathogenic infection8. MIF is also known as a soluble factor produced by T-lymphocytes that can inhibit the migration and promote the aggregation of macrophages at the sites of local inflammation or infection9. In addition, MIF plays an important role in the regulation of the Th1/Th2 balance in the host’s inflammatory reaction and immune responses10. Two major polymorphisms are found in MIF gene, a functional variant (-173 G > C, rs755622) present within the 5′ promoter region, located at the position -173 involves a G > C substitution, appears to affect promoter activity in a cell-type dependent manner11. Previous clinical studies reported higher level of MIF in the serum of TB patients in comparison with the healthy controls12. Since, MIF protein appears to play a key role in mediating a wide variety of immune responses against the invading pathogens, for e.g., M.tb in humans. A large number of researchers performed genetic association studies to correlate MIF -173 G > C polymorphism with TB infection development13,14,15,16,17,18. However, the results from the published studies of -173 G > C gene polymorphism and TB susceptibility are inconsistent and inconclusive. The inconsistency in the results across many of the case-control studies could possibly because of lower sample size and individual studies. Furthermore, as the immune interactions determine TB susceptibility and severity, combined studies may give more meaningful information than a single, independent/individual study in determining the outcome of TB infection. Nowadays, meta-analysis, a statistical tool is used to pool the results from the individual studies to increase the sample size and provides more robust as well as reliable conclusion19. Therefore, a meta-analysis was carried out to evaluate the precise relationship between MIF -173 G > C genetic variant and the risk of developing TB, and its ethnicity based effect on TB infection. In this study, the quality of the included studies was checked by performing Newcastle Ottawa Scale (NOS) analysis. Additionally, publication bias and random errors (type-I statistical errors) occurred due to sparse data were minimized by performing Trial Sequential Analysis (TSA) for quantifying the statistical reliability of the data included in the cumulative meta-analysis with the threshold of statistical significance. This is the primary meta-analysis dealing with the precise appraisal of the association between the MIF -173 G > C gene polymorphism and the risk of TB.
Results
Literature search strategy
According to the literature search strategy applied in this study, as stated in the methodology section, six articles13,14,15,16,17,18 were found relevant showing MIF -173 G > C polymorphism and occurrence of TB, and found eligible for inclusion in the current meta-analysis. All the retrieved research articles were evaluated carefully by examining their titles (headlines) and abstracts/summaries. Complete texts of the potentially germane research articles were further tested for their aptness for inclusion in the present meta-analysis. Studies either showing MIF genetic variant to predict survival in TB patients and/or considering MIF gene polymorphisms as indicators for response to therapy were disqualified straightaway. Likewise, research articles reporting MIF mRNA levels or protein expression or relevant reviews were omitted too. In this study, we included only case-control or cohort design based reports mentioning the frequency of all the three genotypes. Besides the database search, the references available in the retrieved studies were also examined for other probable articles. The major characteristics of all the six studies incorporated in this pooled study, i.e., distributions of genotypes, minor allele frequency (MAF) in the controls and cases, have been shown in Tables 1 and 2. The needful information related to the selection of the pertinent studies has been given in Fig. 1 (PRISMA 2009 Flow Diagram). All the six studies were assessed for their quality score as prescribed by the Newcastle Ottawa scale and most of the studies (80%) scored 5 or more stars and indicated moderate to good quality (Table 3).
Diagnosis of publication bias
In order to evaluate the publication bias among the incorporated studies, Begg’s funnel plot and Egger’s test were carried out in this meta-analysis. The appearance of the shape of funnel plots and the outcomes of Egger’s test have not shown the indication of publication bias in all the five genetic models (Table 4, Supplementary Information: Figure SI1).
Evaluation of heterogeneity
In order to check heterogeneity among the included studies, Q-test and I2 statistics were used. Heterogeneity was not observed in all the four studied genetic models. However, heterogeneity was observed in one genetic model CC vs GC + GG. Thus, random effects model was used for synthesizing the data (Table 4).
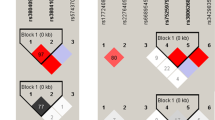
Association of MIF -173 G > C gene polymorphism and TB susceptibility
All the six studies collectively produced 1069 confirmed TB cases and 956 healthy subjects. All the subjects were examined for the association between MIF -173 G > C polymorphism and overall TB risk. Overall pooled analysis suggested increased risk between MIF -173 G > C polymorphism and overall TB susceptibility in four genetic models, i.e., allelic (C vs G: p = 0.001; OR = 1.517, 95% CI = 1.312 to 1.753), homozygous (CC vs GG: p = 0.026; OR = 1.874, 95% CI = 1.079 to 3.257), heterozygous (GC vs GG: p = 0.001; OR = 1.542, 95% CI = 1.273 to 1.868), and dominant model (CC + GC vs GG: p = 0.001; OR = 1.631, 95% CI = 1.362 to 1.955). However, recessive (CC vs GC + GG: p = 0.125; OR = 1.588, 95% CI = 0.880 to 2.864) model did not display any risk between MIF -173 G > C polymorphism and overall TB risk (Fig. 2).
Association of MIF -173 G > C gene variant & TB risk in Asian population
In sub-group analysis of Asian ethnicity population, four studies with a total number of 716 TB cases and 567 controls were included. Heterogeneity was not observed in all the four studied genetic models. However, heterogeneity was observed in recessive genetic model (Table 5). Also, we did not find any publication bias (Table 5; Figure SI2). After combining the all four studies, we observed that allelic (C vs G: p = 0.001; OR = 1.717, 95% CI = 1.424 to 2.071), homozygous (CC vs. GG: p = 0.001; OR = 2.204, 95% CI = 1.390 to 3.494), heterozygous (GC vs. GG: p = 0.001; OR = 1.866, 95% CI = 1.458 to 2.388) and dominant (CC + GC vs. GG: p = 0.001; OR = 1.944, 95% CI = 1.542 to 2.449) genetic models demonstrated increased risk of developing TB. Whereas, no TB risk was revealed by recessive genetic model (CC vs. GC + GG: p = 0.346; OR = 1.476, 95% CI = 0.657 to 3.319) (Fig. 3).
Sensitivity analysis
To evaluate the effect of individual studies for the risk of overall TB, we performed leave-one-out sensitivity analysis and recomputed the pooled ORs. The estimated pooled ORs calculated after excluding a single study did not show any differences from the primary values of overall and Asian risk of TB. This suggests that the results of this meta-analysis were stable and robust (Figures SI3 and SI4).
Trial Sequential Analysis (TSA) of MIF -173 G > C gene polymorphism
By employing TSA (taking the data of the dominant model), the cumulative Z curve crossed with TSA monitoring boundary confirmed that this polymorphism is associated with an increased risk of TB and further relevant trials are unnecessary (Fig. 4). Similar result was observed, when we performed the sub-group analysis (Asian) based on the ethnicity, TSA confirmed that MIF -173 G > C gene polymorphism is significantly associated with TB risk and further relevant trials are unnecessary (Fig. 5).
Re-sampling results
The bootstrap re-sampling method was adopted to check the robustness of the findings of the present meta-analysis, and the relevant results have been given in the Supplementary Information (Microsoft Excel File SI5: Re-sampling analysis results of overall risk; Microsoft Excel File SI6: Re-sampling analysis results of Asian population) files provided with this manuscript. A total of 1000 re-sampling groups were created for both, overall and Asian ethnic groups that yielded 2025000 and 1283000 subjects, respectively. Re-sampling statistics of overall analysis revealed significant association of MIF -173 G > C (rs755622) polymorphism with TB susceptibility. The distribution of odds ratios, 95% CI, odds ratio and p-values for all the five genetic models (dominant, recessive, homozygous comparison, heterozygous comparison and allelic contrast) of overall analysis (2025000 subjects) have been shown in Table 6. Re-sampling statistics was also adopted to evaluate the association of MIF -173 G > C (rs755622) polymorphism with TB risk in Asian ethnicity (1283000 subjects). Similar to the re-sampling results of overall analysis, it was found that MIF -173 G > C (rs755622) polymorphism is also linked with TB susceptibility (Table 6).
Discussion
As it is established that TB is a very complex, multi-factorial disease and environmental and host genetic factors are strongly involved in the development of TB infection20. Thus, prevention and control of TB is attracting more and more attention of the medical world. Identification of the host genes responsible for the susceptibility and resistance to TB may lead towards a better understanding of the pathogenesis of TB and management or even help in the treatment strategies. Evidences indicated that host genetic factors may play an important role in TB susceptibility that contains single nucleotide polymorphisms (SNPs) as a major factor21. Immune responses play a major role in the host defense against M. tuberculosis infection and can cause a broad spectrum of clinical manifestations22,23. Macrophages are the first line of the defense against M.tb infection. Invasive M.tb is eliminated or suppressed by phagosomal and lysosomal fusion, apoptosis induction, and free radicals23. The cytokines produced at the site of the disease after the interaction between T lymphocytes and infected macrophages are necessary for the pathogenesis of TB24.
MIF is an immunoregulatory cytokine that is expressed by T cells, macrophages and pulmonary epithelial cells, and has been considered as potential defense against the invading pathogen25. In addition, this gene has a key role in innate immune response against the bacteria and intracellular pathogens26. In the recent year, many researchers paid attention on the possible role of MIF gene in the innate immune system, pathogenesis of infection and inflammation27,28.
Considering the importance of MIF gene in view, previously many studies examined the possible link between MIF -173 G > C gene variant and the development of TB infection but failed to give concrete conclusion, and still the said relationship is controversial. Until now, there is no well-organized meta-analysis available that evaluated the precise association between MIF -173 G > C gene polymorphism and risk of TB infection development. Therefore, we conducted the present meta-analysis to precisely investigate this possible relationship. On the basis of six independent publications, our meta-analysis clearly produced statistical evidence that MIF -173 G > C variant is significantly associated with an increased risk of TB infection. As we know that host genetic factors are potentially responsible for the development of TB infection20. Hence, a single genetic polymorphism is normally inadequate to prophesized the susceptibility towards this dreadful disease. The important feature of this gene variant is that its occurrence may vary sufficiently among different ethnic populations or races. Therefore, ethnicity-wise sub-group analysis using stratification analysis was performed, which revealed that MIF -173 G > C is more prominent in the Asian subjects. Also, the precise association suggested by the current meta-analysis was confirmed by the TSA, which further escalated the conclusion that MIF -173 G > C polymorphism is correlated with an increased risk of TB. The polymorphism of the promoter region may alter the expression of mRNA and the level of protein. Earlier studies reported that MIF -173 C allele significantly increase the promoter activity of MIF gene26. Earlier, studies stated that circulating levels of MIF concentration were significantly higher in those affected with TB infection than in the healthy controls12,13. Promoter sequence analysis has deciphered that MIF -173 C allele creates a potential activator protein 4 transcription factor binding site, and the circulating levels of MIF are significantly vary among MIF -173 G > C genotypes29. MIF is also considered an essential component of the host antimicrobial alarm system and plays an important role in the stress response that promotes the proinflammatory functions of immune cells30. Although, it is worth mentioning that the immune interactions between the host and the molecular structure of M.tb are not solely depend upon one single factor or one single gene variant, but rather on many gene variants or gene-environment interactions.
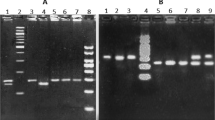
Regardless of achieving some crucial findings, the present meta-analysis suffered with several limitations. First, we considered the research articles that were published only in the English language, which resulted into limited number of studies. The research studies published in other languages and probable unpublished articles were not included in this meta-analysis, which may cause publication bias. Second, in the stratification analysis by sub-group ethnicity-wise analysis, the numbers of individual studies are less that might have a small statistical power to detect the actual association. Third, the study Li et al.16 did not fit with the HWE test in the control group. The most probable reason for this variation is either the controls were not recruited from exactly the same genetic population as the TB patients or may controls suffered from other infectious diseases. But, after the omission of the study of Li et al.16 during the sensitivity analysis, it did not alter the conclusions observed in the meta-analysis. Fourth, the results presented here in this study were based on unadjusted estimates, as ORs in all the included studies were not adjusted by the same potential confounders, such as age, sex, and exposure. Fifth, some studies included in the present meta-analysis used PCR-RFLP whereas other studies adopted sequencing for the genotyping purpose. The basic difference between these two techniques is that, RFLP-PCR exploits variations in homologous DNA sequences and allows rapid detection of the mutation after genomic sequences PCR amplification followed by specific restriction enzyme digestion and visualization in stained agarose gel. Whereas, DNA sequencing is any chemical, enzymatic or technological procedure for determining the linear order of nucleotide bases in DNA, it is generally used to detect any mutation in the DNA sequence being analyzed and this method is often considered as the ‘gold standard’ for DNA sequence analysis. Both of these methods have their own limitations such as sensitivity, performance ease, and instrumentation constraints etc., that might affect the overall results in one or another way.
Notwithstanding above limitations, there are some advantages associated with this meta-analysis. First, the quality assessment of the selected studies was stringently performed by applying NOS scale, where most of the studies scored five or more stars in quality assessment score and indicated moderate to good quality of each study by clearly mentioning about the sample size, genotype, and inclusion criteria of confirmed TB patients and healthy controls. Second, in order to achieve more robust conclusion, publication bias analysis was done and the results did not show any publication bias. Third, we minimized the likelihood of bias by following a detailed protocol of study identification, statistical analysis and data selection. Fourth, sensitivity analysis, Trial sequential analysis, and re-sampling statistics further strengthened the conclusion of the present study.
In conclusion, this meta-analysis provides a strong evidence that MIF -173 G > C gene polymorphism is associated with the development of TB infection in overall and Asian population. MIF genotyping may offer the possibility of identifying individuals those are at a greater risk of TB. Overall, these results would help in understanding the role of this promoter variant in TB infection development and can aid in identifying new molecular targets by focusing on TB patients most likely to get benefit from the pharmacological targeting of MIF. Further well-designed and large sample studies are warranted to confirm the findings reported in this study. Additionally, studies investigating the effect of gene-environment interactions in relation with TB risk are also required.
Materials and Methods
Identification and suitability of the pertinent studies
A comprehensive and systematic search of the relevant studies based on the association between MIF -173 G > C (rs755622) gene polymorphism and the development of TB conducted on internet using online databases, i.e., PubMed (Medline), Google Scholar, and EMBASE to retrieve the compatible and peer reviewed research articles. The last search updated on February 2017. The pertinent study search was performed using the combination of the following keywords: ‘macrophage migration inhibitory factor OR MIF AND Tuberculosis OR TB susceptibility OR TB risk. Combination of single nucleotide polymorphism (SNP) OR genetic variant OR mutation OR genetic polymorphism of MIF -173 G > C AND/OR MIF rs755622 was also tried for the retrieval of the relevant studies. The search was focused on the studies that had been conducted in humans only. All the retrieve studies were evaluated by reading their titles (headlines) and abstracts/summaries, and all the published articles matching with the pre-set eligibility norms were retrieved for the present meta-analysis. We also did some manual search of the references listed in the retrieved articles for other eligible articles.
Inclusion and exclusion criteria
In order to include the research articles in the current meta-analysis, retrieved studies had to fulfill all the pre-set criteria, (a) it must have evaluated the relationship between MIF -173 G > C gene polymorphism and susceptibility to TB, (b) adopted a case-control study design, (c) must recruited confirmed TB patients and healthy control subjects, (d) availability of genotype frequency in cases (confirmed TB patients) and controls to count the odds ratio (OR) and 95% confidence intervals, (e) must published in the English language. Likewise, some preset criteria for the study exclusion were also applied. The major reasons for the study exclusion were (i) not designed as a case-control study, (ii) reviews, and abstracts or overlapping studies, (iii) not reported the genotype frequencies or numbers in the studies. The schematic flow diagram of the selection of the pertinent studies for this meta-analysis following the pre-set including/excluding criteria is shown in Fig. 1: PRISMA 2009 Flow-Diagram.
Data extraction
For every retrieved published study, the procedural data extraction was independently performed in replica copies by two independent (self-regulating) investigators (SAD & RKM) by following a standard validated protocol. In order to ratify the accuracy of the abstracted data, strict pre-set selection criteria were followed during the collection of the data by filling a standard data-collection form. The major characteristics summarized from the retrieved articles include the name of the first author, year of publication, the number of cases and controls, the country of origin, type of study, TB type, methods of genotyping and genotype frequencies for the cases and the controls. Cases pertaining to any type of disagreement or discrepancy in any of the items of the abstracted data from the selected articles were fully resolved by conducting many rounds of group discussions involving adjudicator (SH) to accomplish a final agreement.
Quality score assessment by Newcastle-Ottawa Scale (NOS) criteria
The methodological quality evaluation of the selected studies was also performed separately by two independent investigators (SAD & RKM) by following the preset NOS criteria31. The NOS criteria predominantly comprised of three aspects: (i) subject selection: 0–4 points; (ii) comparability of subjects: 0–2 points; (ii) clinical outcomes: 0–3 points. The selected studies, which were awarded 5 stars or more, can be considered as moderate to high quality32. The quality assessment of the selected individual study was performed independently in duplicate by two investigators (as stated above SAD & RKM) and in case of any discord, it was resolved by a systematic discussion or expert consultation, if necessary with the help of adjudicator SH).
Statistical analysis
The precise strength of the association of MIF -173 G > C gene variant with the chances of developing TB was assessed by using OR and 95% CI. The pooled ORs were computed for allele contrast, log-additive, recessive, and dominant genetic models33. Heterogeneity assumption between the studies across the eligible comparison was done by the chi-square based Q-test34. Heterogeneity was deliberated significant in case p-value < 0.05, to avoid underestimation of the presence of heterogeneity. A fixed effect model (if p > 0.05) or a random effect model (if p < 0.05)35,36 was applied for the pooling of the results. In addition, I2 statistics was used to efficiently check the heterogeneity among the chosen studies37. Hardy-Weinberg equilibrium (HWE) in the controls was computed by employing chi-square test. Additionally, funnel plot asymmetry was measured by Egger’s linear regression test (a type of linear-regression approach) that calculates the funnel plot asymmetry based on the natural logarithm scale of the ORs. The significance of the intercept was determined by the t-test, where p-value < 0.05 was deliberated as the symbol of significant statistical publication bias38. The entire statistical analysis involved in this meta-analysis was performed by using Comprehensive Meta-Analysis (CMA) version 2 software program (Biostat, NJ, USA). All the p-values were two sided and the statistical significance level was considered as p-value < 0.05 for this pooled analysis.
Re-sampling statistics
As number of the studies included in this meta-analysis is small, a bootstrap re-sampling method was adopted by creating 1000 re-sampling groups followed by statistical analysis for possible association of MIF polymorphism (rs755622) with TB susceptibility39,40. The details of re-sampling program along with its results are shown in the Supplementary Information (Microsoft Excel File SI5 and Microsoft Excel File SI6). In the re-sampling program, Microsoft excel file data of the recruited studies (for overall association analysis) comprising 1069 confirmed TB patients and 956 healthy controls were coded as follows: number 1 for TB patients with GG genotype, 2 for TB patients with GC genotype, 3 for TB patients with CC genotype, 4 for healthy controls with GG type, 5 for controls with GC genotype, and 6 for healthy controls with CC genotype. For each re-sampling group, genotypes of 2025 samples were generated by bootstrap method and ORs were calculated for various genetic models. A total sum of 1000 re-sampling groups were created for robust and replicable results. Overall, ORs, 95% CI, range of ORs and p-values were calculated for all the five genetic models (Supplementary Information: Microsoft Excel File SI5). Furthermore, similar re-sampling analysis was applied for Asian cohort comprising 716 confirmed TB patients: 716 and 567 healthy controls (Supplementary Information: Microsoft Excel File SI6).
Trial sequential analysis (TSA)
According to Cochrane handbook, meta-analyses are considered to be the best if all the eligible trials are included in the analysis, however, it may not be able to provide adequate and satisfactory evidence. As meta-analysis may leads to systematic errors (bias) or random errors (play of chance). In order to minimize these errors, a novel statistical analysis program, Trial Sequential Analysis (TSA) tool from Copenhagen Trial Unit, Center for Clinical Intervention Research, Denmark) has been introduced that estimates required information size and adjusts the threshold for the statistical significance and estimates the power of current conclusion41,42,43. If, a TSA monitoring boundary is crossed with Z curve before the required information size is reached, robust evidence might have been confirmed and further trials are unnecessary. In contrast, if the Z curve does not cross the monitoring boundaries and the required information size has not been reached, then it is necessary to continue doing the trials. Trial Sequential Analysis (version 0.9, http://www.ctu.dk/tsa/) was utilized for performing the present investigation.
References
Andrews, J. R. et al. Risk of progression to active tuberculosis following reinfection with Mycobacterium tuberculosis. Clin Infect Dis 54, 784–791 (2012).
Mathema, B., Kurepina, N. E., Bifani, P. J. & Kreiswirth, B. N. Molecular epidemiology of tuberculosis: current insights. Clin Microbiol Rev 19, 658–685 (2006).
Van der Eijk, E. A., Van, D. V., Vandenbroucke, J. P. & Van Dissel, J. T. Heredity versus environment in tuberculosis in twins: the 1950s United Kingdom Prophit survey: Simonds and Comstock revisited. Am J Respir Crit Care Med 176, 1281–1288 (2007).
Moller, M., de Wit, E. & Hoal, E. G. Past, present and future directions in human genetic susceptibility to tuberculosis. FEMS Immunol Med Microbiol 58, 3–26 (2010).
Thye, T. et al. Genome-wide association analyses identifies a susceptibility locus for tuberculosis on chromosome 18q11.2. Nat Genet 42, 739–741 (2010).
Mahasirimongkol, S. et al. Genome-wide association studies of tuberculosis in Asians identify distinct at-risk locus for young tuberculosis. J Hum Genet 57, 363–367 (2012).
Alcaïs, A., Abel, L. & Casanova, J. L. Human genetics of infectious diseases: Between proof of principle and paradigm. Journal of Clinical Investigation 119, 2506–2514 (2009).
Calandra, T., Froidevaux, C., Martin, C. & Roger, T. Macrophage migration inhibitory factor and host innate immune defenses against bacterial sepsis. J Infect Dis 187(Suppl 2), S385–90 (2003).
Martinez, A. et al. Macrophage migration inhibitory factor gene: influence on rheumatoid arthritis susceptibility. Hum Immun 68, 744–7 (2007).
Bacher, M. et al. An essential regulatory role for macrophage migration inhibitory factor in T-cell activation. Proc Natl Acad Sci USA 93, 7849–7854 (1996).
Mitchell, R. et al. Cloning and characterization of the gene for mouse macrophage migration inhibitory factor (MIF). J Immunol 154, 3863–3870 (1995).
Yamada, G. et al. Elevated levels of serum macrophage migration inhibitory factor in patients with pulmonary tuberculosis. Clin Immun 104, 123–7 (2002).
Liu, A. et al. Single nucleotide polymorphisms in cytokine MIF gene promoter region are closely associated with human susceptibility to tuberculosis in a southwestern province of China. Infect Genet Evol 39, 219–24 (2016).
Wang, J. et al. MIF, TGF-β1, IFN-γ and NRAMP1 gene polymorphisms in relation to the clinicopathological profile of spinal tuberculosis in Chinese Han population. Int J Clin Exp Pathol 9(4), 4438–4447 (2016).
Hashemi, M. et al. Macrophage migration inhibitory factor -173 G/C polymorphism is associated with an increased risk of pulmonary tuberculosis in Zahedan, Southeast Iran. EXCLI J 21(14), 117–22 (2015).
Li, Y. et al. Association of tuberculosis and polymorphisms in the promoter region of macrophage migration inhibitory factor (MIF) in a Southwestern China Han population. Cytokine 60(1), 64–7 (2012).
Sadki, K. et al. Analysis of MIF, FCGR2A and FCGR3A gene polymorphisms with susceptibility to pulmonary tuberculosis in Moroccan population. J Genet Genomics 37(4), 257–64 (2010).
Gómez, L. M. et al. Macrophage migration inhibitory factor gene influences the risk of developing tuberculosis in northwestern Colombian population. Tissue Antigens 70(1), 28–33 (2007).
Ohn, L. D. & Becker, B. J. How meta-analysis increases statistical power. Psychological Methods 8, 243–253 (2003).
Moller, M. & Hoal, E. G. Current findings, challenges and novel approaches in human genetic susceptibility to tuberculosis. Tuberculosis (Edinburgh, Scotland) 90, 71–83 (2010).
Asner, S. A., Morré, S. A., Bochud, P. Y. & Greub, G. Host factors and genetic susceptibility to infections due to intracellular bacteria and fastidious organisms. Clin Microbiol Infect 20(12), 1246–53 (2014).
Hernandez-Pando, R., Orozco, H. & Aguilar, D. Factors that deregulate the protective immune response in tuberculosis. Arch Immunol Ther Exp (Warsz) 57, 355–67 (2009).
Winek, J. et al. Comparison of Th1 and Th2 response in blood of tuberculosis patients and healthy contacts. Pneumonol Alergol Pol 77, 446–52 (2009).
Sher, A. & Coffman, R. L. Regulation of immunity to parasites by T cells and T cell-derived cytokines. Annu Rev Immunol 10, 385–409 (1992).
Donnelly, S. C. & Bucala, R. Macrophage migration inhibitory factor: a regulator of glucocorticoid activity with a critical role in inflammatory disease. Mol Med Today 3, 502–7 (1997).
Calandra, T. & Roger, T. Macrophage migration inhibitory factor: a regulator of innate immunity. Nat Rev Immunol 3, 791–800 (2003).
Greven, D. Autoimmune diseases: MIF as a therapeutic target. Expert Opinionon Therapeutic Targets 14, 253–264 (2010).
Grieb, G., Merk, M., Bernhagen, J. & Bucala, R. Macrophage migration inhibitory factor (MIF): a promising biomarker. Drug News Perspect 23(4), 257–64 (2010).
Temple, S. E. L., Cheong, K. Y., Price, P. & Waterer, G. W. The microsatellite, macrophage migration inhibitory factor -794, may influence gene expression in human mononuclear cells stimulated with E. coli or S. pneumoniae. Intl J Immunogen 35, 309–316 (2008).
Calandra, T., Bernhagen, J., Mitchell, R. A. & Bucala, R. The macrophage is an important and previously un- recognized source of macrophage migration inhibitory factor. J Exp Med 179, 1895–902 (1994).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta- analyses. Eur J Epidemiol 25, 603–605 (2010).
Hu, P. et al. Meta-analysis of C242T polymorphism in CYBA genes: risk of acute coronary syndrome is lower in Asians but not in Caucasians. J Zhejiang Univ Sci B 16, 370–379 (2015).
Woolf, B. On estimating the relation between blood group and disease. Ann Hum Genet 19(4), 251–3 (1955).
Wu, R. & Li, B. A multiplicative-epistatic model for analyzing interspecific differences in outcrossing species. Biometrics 2, 355–365 (1999).
Mantel, N. & Haenszel, W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 4, 719–748 (1959).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials 7, 177–188 (1986).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 7414, 557–560 (2003).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 7109, 629–634 (1997).
Efron, B. & Tibshirani, R. J. An introduction to the Bootstrap. Chapman & Hall, New York 6, 71–77 (1993).
Li, J. et al. Identification of high-quality cancer prognostic markers and metastasis network modules. Nat Commun 1, 34, https://doi.org/10.1038/ncomms1033 (2010).
Wetterslev, J. et al. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 61, 64–75 (2008).
Turner, R. M., Bird, S. M. & Higgins, J. P. The impact of study size on metaanalyses: examination of underpowered studies in Cochrane reviews. PLoS One 8, e59202 (2013).
Brok, J. et al. Apparently conclusive metaanalyses may be inconclusive–Trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta-analyses. Int J Epidemiol 38, 287–298 (2009).
Acknowledgements
We sincerely acknowledge the infrastructural support and dry-lab facility provided by the Deanship of Scientific Research, Jazan University, Jazan-45142, Saudi Arabia for this study.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study and experiments: M.Y.A., S.A.D., R.K.M., A.J., M.W., M.L., A.K.P., B.N.M., S.H., N.A. Performed the experiments: R.K.M., M.Y.A., S.A.D., A.K.P. Analyzed the data: M.Y.A., R.K.M., S.A.D., A.K.P., A.J., M.W. Contributed materials/analysis tools/reagents: S.A.D., A.J., M.W., M.L., B.N.M., N.A., S.H. Wrote the paper: R.K.M., S.A.D., S.H. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Areeshi, M.Y., Mandal, R.K., Dar, S.A. et al. MIF -173 G > C (rs755622) Gene Polymorphism Modulates Tuberculosis Risk: Evidence from a Meta-analysis and Trial Sequential Analysis. Sci Rep 7, 17003 (2017). https://doi.org/10.1038/s41598-017-17308-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-17308-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.