Abstract
A hospital-based case-control study was conducted to investigate potential association between mitochondrial DNA and Type 2 diabetes mellitus (T2DM) in Chinese Uyghur population. We sequenced mitochondrial DNA from 210 Uyghur individuals including 88 T2DM patients and 122 controls. Using haplogroup classification and association test, we found that haplogroup H (odds ratio [OR] = 1.40; 95% confidence interval [CI]: 1.20–1.64; P = 0.0005138) and D4 (odds ratio = 1.47; 95% CI: 1.22–1.77; P = 0.001064) were associated with an increased risk of T2DM in Chinese Uyghur population. Two markers of haplogroup D4 and H, MT-ATP8 m.8414 T > G (p.Leu17Phe) and m.2706 G > A encoding 16S rRNA in mitochondria, were predicted to affect the structure of MT-ATP8 and 16S RNA, respectively, and may be involved in the pathogenesis of T2DM. Our study provides a new clue for mitochondrial DNA in the etiology of T2DM in Chinese Uyghur population.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) has become one of the greatest challenges for public health worldwide in the 21st century1. Diabetic complications, including cardiovascular disease, stroke, kidney disease and even cancer, contribute to about 4 million deaths per year globally2. According to International Diabetes Federation, the number of diabetic patients could possibly increase from 366 million in 2011 to 552 million by 20303. In Xinjiang Uyghur Autonomous Region, the prevalence of T2DM is significantly higher in Uyghur people than in other ethnic minorities of close phylogenetic relationship4. At the same body mass index (BMI) level, Uyghurs have greater risks for diabetes compared to other ethnic minorities in this area5. However, the factors attributed to this high prevalence of T2DM in Uyghur people remain unexplored.
T2DM is a progressive multifactorial disease, characterized by insulin resistance and reduction in insulin secretion6. Insulin resistance has developed many years before the diagnosis of T2DM7. Mitochondrial DNA (mtDNA) plays an important role in insulin resistance and T2DM. Mitochondrial dysfunctions, such as reduced capacity to mitochondrial oxidative phosphorylation, submaximal ADP-stimulated oxidative phosphorylation and mitochondria plasticity, have been implicated in the pathogenesis of insulin resistance and diabetes7,8,9,10. The effects of mitochondrial haplogroups and SNPs on diabetes have also been explored. In Japanese and Korean populations, the haplogroup N9a was indicated to possibly confer resistance against T2DM11. In contrast, in Chinese population, N9a is significantly associated with an increased risk of diabetic nephropathy12. D4 haplogroup had borderline resistance to T2DM in Chinese Han individuals, whereas B haplogroup associated with an increased risk of T2DM13. In Finnish, m.16189 T > C (D-loop) and m.3010 G > A (16S rRNA) was found to be more frequent in patients with diabetes than in controls14. In Chinese Han population, m.3243 A > G (16S rRNA) was associated with high prevalence of T2DM15.
T2DM is a multi-factorial common disease affected by both genetic and environmental factors. For example, racial/ethnic factor can significantly modify the prevalence of T2DM. Studies performed in different populations often exhibit diverse even conflicting results due to different health behaviors, genetic factors and individual-level sociodemographics16. To investigate the association between mtDNA and T2DM in Uyghur people, we conducted a hospital-based case-control study on 210 Uyghur individuals including 88 T2DM patients and 122 controls.
Results
Mitochondrial genome analysis
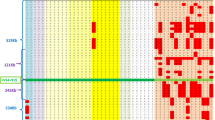
According to mitochondrial phylogenetic tree from Phylo-tree17, we classified the samples into 12 haplogroups (A, B, C, D4, F, G, H, HV, J, T, U and W), haplogroups (D5, I, X, Z, O, W, K, M7, M8, M9, N30) with a limited number (smaller than 6, 3%) were clustered to group Others in M and group Others in N. Haplogroups A, B, C, D4, F and G were common in Asians but rare in Europeans, while haplogroups H, HV, J, T, U and W were very rare in Asians but common in Europeans. This result was consistent with human mitochondrial haplogroup distribution formed by the Human migration (www.mitomap.org), suggesting that Uyghur people was an admixture of populations from Europe and Asia. Therefore, subject clustering was required before investigating potential association between mtDNA and T2DM. PCA analysis was performed and all 210 subjects were classified into 4 clusters (Fig. 1). The distribution of haplogroups in each cluster were shown in Fig. 2.
Subjects distribution according to the PCA analysis. We employed Smartpca from EIGENSOFT package and K-means method from Weka to classify all 210 subjects into 4 clusters. Different colors indicated different clusters. Triangle indicates case subjects. Crossover indicates control subjects. Principal component 1 (PC1) and principal component 2 (PC2) were the first two axes of PCA and represented 7.626% and 5.276% variance.
Using multivariate logistic regression analysis, we found that people harboring haplogroup H (odds ratio [OR] = 1.40; 95% confidence interval [CI]: 1.20–1.64; P = 0.0005138) and D4 (odds ratio = 1.47; 95% CI: 1.22–1.77; P = 0.001064) was more frequent in patients with diabetes than in controls (Table 1).
In addition, the markers related to haplogroups D4 and H, including variants m.3010 G > A (D4), m.8414 C > T (D4), m.14668 C > T (D4), m.2706 G > A (H) and m.7028 T > C (H) were more frequent in cases than in controls (Table 2), by Fisher’s exact test. Of these variants, m.8414 C > T from the haplogroup D4 was non-synonymous and located in mitochondrially encoded ATP synthase protein 8 (MT-ATP8). The m.2706 G > A and m.3010 G > A were located in mitochondrially encoded 16S RNA.
Variant damage analysis
We then extracted unique non-synonymous variants in cases (Table 3) to explore their potential functions. Four popular predictors were applied to assess the impact of AA substitution caused by these variants on the properties of mitochondrial proteins. The predictors were PolyPhen-218, CADD19, PANTHER20 and CAROL21.
Interestingly, m.8414 C > T was highly suspicious. Three of four predictors suggested that m.8414 C > T was likely to influence the stability of the protein and may contribute to disease development (Table 4).
Protein 3D structure analysis
We performed 3D structure analysis using CABS-fold22 to assess the effect of variant p.Leu17Phe (m.8414 T > G) on the structure of MT-ATP8. The 3D structure of MT-ATP8 was displayed in Supplementary Figure 1.
In term of molecular modeling, potential energy of a system of atoms is calculated as force field, in which angles, bonds, torsions and impropers are taken into consideration. In current study, GROMOS96 force field was used to estimate the potential energy of MT-ATP8 by Swiss-PDBviewer23 (version 4.10). When MT-ATP8 17th amino acid (AA) was mutated from Leu to Phe by Swiss-PDBviewer, a decrease in H-bond number indicated a more unstable structure (Fig. 3). Using Swiss-PDBviewer, the force field around 17th AA was estimated to be increased from −40.646 to −12.161 (Fig. 4), which may lead to unstable protein structure around this area.
Protein transmembrane property analysis
The subcellular location of ATP synthase is on the mitochondrial inner membrane, and the ATP synthase protein 8 is a single-pass membrane protein, according to annotations from Uniprot. So it is necessary to investigate whether the mutation p.L17F (m.8414 C > T) in the MT-ATP8 has an impact on the protein’s transmembrane area.
TMpred was used to assess protein sequence with a mutation p.L17F in the MT-ATP8. The result indicated that the transmembrane area of MT-ATP8 was changed from 8th-24th AAs to 11th-29th AAs, which might affect the assembly of ATP synthase (Fig. 5).
RNA structure analysis
The rRNA plays an important role in human mitochondrial ribosome assembly and RNA modification, which are strongly linked with energy metabolism. RNA-fold server was used to predict the structural change caused by variant m.2706 G > A (Fig. 6). Oligowalk from RNAstructure24 (version 5.3) was employed to compare the target binding ability between 16S rRNA with and without m.2706 G > A. Notably, the structural change caused by variant m.2706 G > A from haplogroup H might weaken the binding between mitochondrial 16S RNA and its nucleic acid targets (Fig. 7). Therefore, structural change of mitochondrial 16S rRNA caused by variant m.2706 G > A might affect RNA modifications and ribosome assembly, in Uyghur population.
Discussion
In this case-control study, we have identified an association between mitochondrial DNA and T2DM in Chinese Uyghur population. Mitochondrial DNA sequencing was conducted in 88 T2DM patients and 122 controls. Haplogroups H and D4 were found to be more frequent in T2DM patients than in controls.
A variety of diseases, such as Alzheimer’s disease, cardiovascular disease, Leber’s hereditary optic neuropathy (LHON) and T2DM have been associated with mitochondrial haplogroups25,26,27,28. It was reported that racial factors played an important role in the prevalence of T2DM16. Researches performed in different populations presented different even conflicting results. For Han Chinese, haplogroup N9a increased the risk of T2DM complications12, while in Japanese population, N9a was associated with resistance against T2DM11 or against metabolic syndrome in Japanese women29. In Chinese Taiwan population, haplogroup D4 was related to a borderline reduced risk for T2DM13. In contrast, haplogroup D4 was associated with an increased risk of T2DM in Korean population11 and Chinese Uyghur population in present research.
In our study, haplogroup D4 was more frequent in Chinese Uyghur T2DM patients, which was consistent with the findings in Finnish population, showing that variant m.3010 G > A was more frequent in cases than in controls. The variant m.3010 G > A marked haplogroup D4 in Chinese Uyghur subjects and haplogroup H1 in Finnish population. This indicated that m.3010 G > A variant was likely to be involved in the pathogenesis of T2DM. However, its biologic functions in the pathogenesis of T2DM require further investigation.
Haplogroup H was found to be associated with enhanced mitochondrial activities, including higher mitochondrial respiratory capacity (intrinsic activity)30, mitochondrial oxidative damage31 and intracellular ATP concentration32, while its sub-haplogroup H1 was associated with T2DM in Finnish population. In present study, haplogroup H showed a significant association with T2DM. Variants m.2706 G > A and m.7028 T > C were related to increased incidence of T2DM in Uyghur people harboring haplogroup H. The SNP m.2706 G > A was located in mitochondrially encoded 16S RNA, while m.7028 T > C was synonymous.
The structure of mitochondrially encoded rRNA is critical for human mitochondrial ribosome assembly33. RNA modifications also affect energy metabolism34. Structural changes of mitochondrial 16S rRNA might regulate RNA modifications, protein synthesis as well as ribosome assembly. In present study, a structural change in 16S rRNA caused by m.2706 G > A from haplogroup H was observed, and thus the binding ability of mutated 16S rRNA might be altered. This structural change might affect 16S rRNA modifications and mitochondrial encoded protein synthesis, which are important for energy metabolism.
In this study, we found that haplogroup D4 and H were more frequent in Chinese Uyghur T2DM patients. Variants m.2706 G > A and m.8414 C > T might be risk factors in the development of T2DM in Chinese Uyghur population.
Materials and Methods
Samples and mitochondrial genome sequencing
The healthy controls and cases, residents of Heitan, Keshi, and Korla districts in Xinjiang Uyghur Autonomous Region, were recruited from May 2010 to November 2011 at the Fifth Affiliated Hospital of Xinjiang Medical University. A written informed consent has been obtained from each subject. This study has been approved by Ethics Committee at the Fifth Affiliated Hospital of Xinjiang Medical University. All procedures were conducted according to the regulations and guidelines approved by the ethics committee at the Fifth Affiliated Hospital of Xinjiang Medical University.
Demographic and clinical information was extracted from electronic medical record, including age, gender, ethnicity, medical history, smoking and alcohol drinking. Smoking was defined as a current smoker or a former smoker (who quits) with tobacco/cigarettes consumption of more than 10 packs per year. Alcohol drinking was defined as alcohol consumption of at least 50 g per week for at least 6 months. Body weight and height were measured with light clothing and in bare feet. Blood samples were collected after overnight fasting. Glucose, Total Cholesterol, LDL, HDL and Triglyceride were measured with standard biochemical assays. T2DM was diagnosed according to WHO 1999 Diagnostic Criteria. Hypertension was defined as systolic pressure ≥140 mmHg and/or diastolic pressure ≥90 mmHg (from an average of 2 measurements or pre- and post-therapy). Hyperlipidemia was defined as fasting venous total cholesterol ≥200 mg/dL or LDL-C ≥ 130 mg/dL.
A total of 210 Uyghur objects, including 88 subjects with T2DM and 122 control subjects, were recruited in this study. Genomic DNA was extracted from peripheral whole blood using a DNA Blood Mini Kit 250 (QIAGEN Translational Medicine Co., Ltd., German). Fragments of mitochondrial DNA were amplified by PCR. The reaction mixture (100 μl) contained 20 ng of genomic DNA, 30 pmol of each primer, 5 mmol of each dNTP, and 2.5 U of DNA polymerase in a 10× PCR buffer. The cycling conditions were as follows: 94 °C for 5 min, followed by 35 cycles of denaturation at 94 °C for 30 sec, annealing at 65 °C for 40 sec, and extension at 72 °C for 4 min, with a final extension at 72 °C for 10 min. The fragments were purified and sequenced by Applied Biosystems 3730 DNA automatic sequencer at the Beijing Genomics Institute (Beijing, China). Primers for sequencing and PCR were shown in Supplementary Tables 1 and 2, respectively. The sequence data reported in this paper have been deposited in the Genome Sequence Archive of Beijing Institute of Genomics, Chinese Academy of Sciences. The information about age, gender and BMI of samples were shown in Supplementary Table 3.
Mitochondrial haplogroups classification
The resultant sequence data are aligned against with the Cambridge reference sequence (GenBank No., NC_012920). We determine the haplogroups of mitochondrial DNA according to the mtDNA tree17 and Mitomaster35.
Statistical analysis
We applied smartpca program from the EIGENSOFT version 3.0 to analyze the PCA and used K-means method from software Weka to cluster the PC1, PC2 and PC3 from PCA analysis.
We performed multivariate logistic regression analyses to demonstrate the association between the haplogroups and T2DM by glm function from R package (version 3.3.2), considering T2DM as a dependent variable, whereas information on haplogroups, the first two PCs from PCA, BMI, age and sex of each subject as independent variables. In multivariate logistic regression analyses, haplogroups with sample size smaller than 6 (3%) are allocated into group ‘Others in M’ and group ‘Others in N’ according to the phylogenetic tree. All P-values are corrected by Bonferroni method.
We used Fisher’s Exact Test to compare the frequencies of SNPs between cases and controls within each cluster. We calculated the P-values by two-tailed Fisher’s Exact Tests from R version 3.3.2, along with odds ratio (OR) and 95% confidence interval (CI). All P values were adjusted by Bonferroni correction. For Bonferroni correction, P values are adjusted according to the amount of haplogroups and SNPs in different clusters.
Variant damage analysis
We used a series of predicting tools, including PolyPhen-218, CADD19, PANTHER20 and CAROL21, to analyze a specific protein with special mutations. These tools focus on different areas, disease related SNPs, including conservation in the phylogenetic tree and structure features in transmembrane, intramembrane, signal peptide, binding region, etc. A variant was likely to be suspicious as disease-causing if more than 2 tools suggest deleterious.
Protein 3D structure analysis
We used CABS-fold server22 to predict the 3D structure of MT-ATP8 protein, due to lack of available X-ray 3D structure of human MT-ATP8 molecule. Afterwards, we used SWISS-Pdbviewer (version 4.10) to analyze mutations and to estimate force field.
RNA structure analysis
The RNA-fold sever (http://rna.tbi.univie.ac.at/cgi-bin/RNAfold.cgi) was employed to predict the secondary structure of mitochondrially encoded 16S RNA. We adopted the minimum free energy prediction model. Oligowalk algorithm from RNAstructure program24 was employed to assess the target binding ability.
Data availability
The sequence data reported in this paper have been deposited in the Genome Sequence Archive of Beijing Institute of Genomics, Chinese Academy of Sciences, with an accession number CRA000365.
References
Zimmet, P., Alberti, K. G. & Shaw, J. Global and societal implications of the diabetes epidemic. Nature 414, 782–787 (2001).
Roglic, G. & Unwin, N. Mortality attributable to diabetes: estimates for the year 2010. Diabetes Res Clin Pract 87, 15–19 (2010).
Whiting, D. R., Guariguata, L., Weil, C. & Shaw, J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94, 311–321 (2011).
Tao, Y. et al. The prevalence of type 2 diabetes and hypertension in Uygur and Kazak populations. Cardiovasc Toxicol 8, 155–159 (2008).
Zhang, J. et al. Adipose Tissues Characteristics of Normal, Obesity, and Type 2 Diabetes in Uygurs Population. J Diabetes Res 2015, 905042 (2015).
Festa, A., Williams, K., D’Agostino, R. Jr., Wagenknecht, L. E. & Haffner, S. M. The natural course of beta-cell function in nondiabetic and diabetic individuals: the Insulin Resistance Atherosclerosis Study. Diabetes 55, 1114–1120 (2006).
Szendroedi, J., Phielix, E. & Roden, M. The role of mitochondria in insulin resistance and type 2 diabetes mellitus. Nat Rev Endocrinol 8, 92–103 (2011).
Petersen, K. F., Dufour, S., Befroy, D., Garcia, R. & Shulman, G. I. Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 350, 664–671 (2004).
Bonnard, C. et al. Mitochondrial dysfunction results from oxidative stress in the skeletal muscle of diet-induced insulin-resistant mice. J Clin Invest 118, 789–800 (2008).
Gordon, J. W., Dolinsky, V. W., Mughal, W., Gordon, G. R. & McGavock, J. Targeting skeletal muscle mitochondria to prevent type 2 diabetes in youth. Biochem Cell Biol 93, 452–465 (2015).
Fuku, N. et al. Mitochondrial haplogroup N9a confers resistance against type 2 diabetes in Asians. Am J Hum Genet 80, 407–415 (2007).
Niu, Q. et al. Effects of mitochondrial haplogroup N9a on type 2 diabetes mellitus and its associated complications. Exp Ther Med 10, 1918–1924 (2015).
Liou, C. W. et al. Mitochondrial DNA coding and control region variants as genetic risk factors for type 2 diabetes. Diabetes 61, 2642–2651 (2012).
Soini, H. K., Moilanen, J. S., Finnila, S. & Majamaa, K. Mitochondrial DNA sequence variation in Finnish patients with matrilineal diabetes mellitus. BMC Res Notes 5, 350 (2012).
Wang, S. et al. Mitochondrial DNA mutations in diabetes mellitus patients in Chinese Han population. Gene 531, 472–475 (2013).
Christine, P. J. et al. Longitudinal Associations Between Neighborhood Physical and Social Environments and Incident Type 2 Diabetes Mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). JAMA Intern Med 175, 1311–1320 (2015).
van Oven, M. & Kayser, M. Updated comprehensive phylogenetic tree of global human mitochondrial DNA variation. Hum Mutat 30, E386–394 (2009).
Adzhubei, I. A. et al. A method and server for predicting damaging missense mutations. Nat Methods 7, 248–249 (2010).
Kircher, M. et al. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet 46, 310–315 (2014).
Tang, H. & Thomas, P. D. PANTHER-PSEP: predicting disease-causing genetic variants using position-specific evolutionary preservation. Bioinformatics 32, 2230–2232 (2016).
Lopes, M. C. et al. A combined functional annotation score for non-synonymous variants. Hum Hered 73, 47–51 (2012).
Blaszczyk, M., Jamroz, M., Kmiecik, S. & Kolinski, A. CABS-fold: Server for the de novo and consensus-based prediction of protein structure. Nucleic Acids Res 41, W406–411 (2013).
Guex, N., Peitsch, M. C. & Schwede, T. Automated comparative protein structure modeling with SWISS-MODEL and Swiss-PdbViewer: a historical perspective. Electrophoresis 30(Suppl 1), S162–173 (2009).
Reuter, J. S. & Mathews, D. H. RNAstructure: software for RNA secondary structure prediction and analysis. BMC Bioinformatics 11, 129 (2010).
Zhang, A. M. et al. Mitochondrial DNA haplogroup background affects LHON, but not suspected LHON, in Chinese patients. PLoS One 6, e27750 (2011).
Guo, L. J. et al. Mitochondrial genome polymorphisms associated with type-2 diabetes or obesity. Mitochondrion 5, 15–33 (2005).
Santoro, A. et al. Evidence for sub-haplogroup h5 of mitochondrial DNA as a risk factor for late onset Alzheimer’s disease. PLoS One 5, e12037 (2010).
Kong, Q. P. et al. Updating the East Asian mtDNA phylogeny: a prerequisite for the identification of pathogenic mutations. Hum Mol Genet 15, 2076–2086 (2006).
Tanaka, M. et al. Women with mitochondrial haplogroup N9a are protected against metabolic syndrome. Diabetes 56, 518–521 (2007).
Larsen, S. et al. Increased intrinsic mitochondrial function in humans with mitochondrial haplogroup H. Biochim Biophys Acta 1837, 226–231 (2014).
Martinez-Redondo, D. et al. Human mitochondrial haplogroup H: the highest VO2max consumer–is it a paradox? Mitochondrion 10, 102–107 (2010).
Arning, L. et al. Mitochondrial haplogroup H correlates with ATP levels and age at onset in Huntington disease. J Mol Med (Berl) 88, 431–436 (2010).
Amunts, A., Brown, A., Toots, J., Scheres, S. H. & Ramakrishnan, V. Ribosome. The structure of the human mitochondrial ribosome. Science 348, 95–98 (2015).
Bar-Yaacov, D. et al. Mitochondrial 16S rRNA Is Methylated by tRNA Methyltransferase TRMT61B in All Vertebrates. PLoS Biol 14, e1002557 (2016).
Brandon, M. C. et al. MITOMASTER: a bioinformatics tool for the analysis of mitochondrial DNA sequences. Hum Mutat 30, 1–6 (2009).
Acknowledgements
This work was supported by grants from the Natural Science Foundation of Xinjiang Autonomous Region (2010211A33, 2012211A033) and the National Natural Science Foundation of China (81260057).
Author information
Authors and Affiliations
Contributions
J.Y., W.J. and M.G. coordinated and managed the project. P.W., T.W., J.L. conducted the experimental work. R.L. and Y.Z. conducted data analysis. R.L., Y.Z., W.J. and M.G. participated in manuscript writing and editing. All authors have read and approved the final version of the manuscript. We declare that this work, as original research conducted in China, in whole or in part has never been published previously, and is not under consideration for publication elsewhere.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, W., Li, R., Zhang, Y. et al. Mitochondrial DNA Mutations Associated with Type 2 Diabetes Mellitus in Chinese Uyghur Population. Sci Rep 7, 16989 (2017). https://doi.org/10.1038/s41598-017-17086-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-17086-7
This article is cited by
-
Analysis of MT-ATP8 gene variants reported in patients by modeling in silico and in yeast model organism
Scientific Reports (2023)
-
Contribution of environmental, genetic and epigenetic factors to obesity-related metabolic syndrome
The Nucleus (2023)
-
Enhanced mitochondrial DNA editing in mice using nuclear-exported TALE-linked deaminases and nucleases
Genome Biology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.