Abstract
The association between corneal biomechanical properties and glaucoma is an area of much interest. We determined the relationship between corneal hysteresis (CH) and optic nerve parameters in healthy myopic subjects in the current study. CH was measured with Reichert Ocular Response Analyzer in 108 eyes from 108 healthy myopic subjects. All subjects received retinal nerve fiber layer and optic disc imaging Cirrus HD-OCT, GDx ECC, and Heidelberg Retina Tomograph II. None of the tested optic nerve parameters showed statistical significance with CH by using correlation analysis. For RNFL parameters, there was a negative but not statistically significant correlation between CH and average RNFL thickness obtained with OCT (r = −0.15, p = 0.13). For optic disc parameters, there was a negative but not statistically significant correlation between CH and rim area measured with OCT (r = −0.10, p = 0.29). The current study did not find any statistically significant relationship between CH and optic nerve parameters as measured by all three imaging modalities in healthy myopic eyes. Therefore, the relationship observed previously in glaucoma subjects is likely coming to fruition as optic nerve damage is caused by the disease.
Similar content being viewed by others
Introduction
The association between corneal biomechanical properties and glaucoma is an area of much interest1,2,3. The Ocular Response Analyzer (ORA) has been developed to analyze in vivo corneal biomechanical properties including the corneal hysteresis (CH) and the corneal resistance factor (CRF)4. It is speculated that corneal biomechanical properties could reflect structural vulnerabilities of the entire eye that increase its susceptibility to glaucoma. Previous studies have reported that lower CH is associated with both structural and functional damage in glaucoma2,5. Moreover, it has been shown, in recent studies, that CH measurements are significantly associated with risk of glaucoma progression6,7. However, while the association has been examined in glaucomatous eyes, there is limited and conflicting data regarding the relationship between CH and optic nerve parameters in healthy subjects. In a population-based study, neither CH nor CCT was found to correlate with measures of optic disc cupping8. In contrast, CH was reported to positively correlate with rim area and RNFL measurement in 5134 British subjects9. Thus, controversies exist regarding the association between corneal biomechanical properties and structural measurements of the optic nerve.
Myopia is a common ocular disorder which has been shown to be one of the risk factor for primary open angle glaucoma10,11. Although the underlying mechanism between myopia and risk of glaucoma is not fully understood, it has been suggested that eyes with a long axial length have a greater deformability of the lamina cribrosa which might contribute to a higher susceptibility to glaucomatous damage12. Furthermore, lamina cribrosa defects have been reported to be associated with glaucomatous damage in myopic eyes13,14 As the sclera and cornea are composed of an integrated connective tissue layer, alteration of CH (a quantitative measurement of cornea deformation) may reflect the change of lamina cribrosa. Previously, CH has been found to be lower in myopic eyes, glaucomatous eyes, and in patients with unilateral nonarteritic anterior ischemic optic neuropathy2,5,15,16,17.All these findings suggest that decrease of CH could probably reflect structural weakness in the lamina cribrosa which increase its susceptibility to glaucoma in myopic eyes. Therefore, evaluation of the fundamental relationship between corneal biomechanical properties and optic nerve morphology in healthy myopic eyes may provide an insight into the increased susceptibility to glaucoma in myopia subjects.
In view of the clinical importance of corneal hysteresis and the controversies about the relationships between corneal hysteresis and optic nerve parameters, we aimed to investigate the association of corneal hysteresis with the structural measurements of the optic nerve by using 3 commonly used imaging devices in healthy myopic subjects.
Results
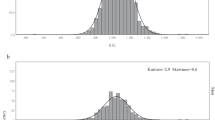
Eight subjects were excluded because of unreliable visual field tests (5 subjects) and poor OCT scan quality (3 subjects). As a result, we included 108 eyes from 108 subjects (66 females and 58 right eyes). Table 1 shows the demographics of the study population. The mean refractive error and axial length were −4.91 ± 2.03 D (range, −9.63 to −1.00 D) and 25.60 ± 1.04 mm (range, 22.62 to 28.77 mm), respectively. The mean CH and CCT was 9.77 ± 1.35 mmHg (range, 7.03 to 12.73 mm) and 540.9 ± 28.8 μm (range, 444 to 612 μm), respectively. Figure 1 displays the distribution of CH and refractive status across all subjects. CH was significantly associated with axial length and refractive error(r = −0.20, p = 0.03 and r = 0.21, p = 0.03, respectively). CCT did not correlate with axial length and refractive error (p ≥ 0.73).
Table 2 demonstrates the mean measurements of optic nerve parameters and their relationship with CH and CCT. No significant correlation was detected between CH and RNFL measurements. For RNFL parameters obtained with OCT, there was a negative but not statistically significant correlation between CH and average RNFL thickness (r = −0.15, p = 0.13). With respect to SLP parameters, no significant relationship between CH and the RNFL parameters was detected. None of the tested disc parameters showed statistical significance with CH. For optic disc parameters measured with OCT, there was a negative but not statistically significant correlation between CH and rim area (r = −0.10, p = 0.29). CCT did not correlate with any of the RNFL measurements in OCT and SLP (Table 2). Positive but not statistically significant correlations between CCT and several disc measurements were found by using HRT (with r ranging from 0.11 to 0.17, all p ≥ 0.08, Table 2).
Table 3 presents the subgroup analysis regarding the associations between CH and various optic nerve parameters in low to moderate myopia and high myopia. A similar pattern of correlations was observed. No significant relationship between CH and optic nerve parameters was detected (all p ≥ 0.10, Table 3) in both groups.
Discussion
Corneal biomechanics has been an area of much recent interest as a risk factor for glaucoma development and progression1,2,3,5,6,7. In the present study, we aimed to evaluate the relationship between CH and quantitative measurements of the RNFL and optic disc. By using all three devices, we did not detect any statistically significant relationship between CH and various optic nerve parameters in healthy myopic eyes.
Limited data regarding the association between CH and RNFL thickness has been reported in previous studies9,18,19. Bueno-Gimeno et al. found a positive correlation between CH and peripapillary RNFL thickness in 199 children18. Recently, in the EPIC-Norfolk Eye Study, CH was reported to positively correlate with RNFL measurement by using SLP technology in 5134 British subjects9. In contrast, Chang et al. reported that CH was not associated with peripapillary RNFL or macular inner retinal layer thickness in 100 myopic eyes of 50 myopic subjects by using spectral-domain OCT19. In the present study, we use both the SD-OCT and SLP to measure the RNFL thickness in healthy myopic eyes. Consistent with Chang’s study19, we did not find a significant relationship between CH and RNFL measurements in both devices. The discrepancy in the finding between these studies might partially be explained by differences in the study population, methodology and sample size. According to the methodology of the EPIC-Norfolk Eye Study, both healthy eyes and eyes with glaucomatous damage were included in the analysis9. Previous studies have shown that CH is significantly lower in glaucomatous eyes3,5. A positive correlation found between CH and RNFL measurement in their study might at least partially be explained by the effect of glaucoma damage on CH and RNFL. Moreover, it has to be noted that the correlation of CH to RNFL measurement shown in the EPIC-Norfolk Eye Study was rather weak (partial correlation coefficient = 0.106, p = 0.006)9, so a chance finding cannot be excluded, and the clinical implication of such a weak correlation remain to be confirmed.
Previous studies have evaluated the association between CH and optic disc parameters8,19,20,21. Lim et al. show that both CH and CRF were not associated with various optic disc parameters by using HRT 2 in 102 Singaporean children20. In a large cohort of 1645 healthy British twins, Carbonaro et al. reported that CH was not significantly correlated with measurements of optic disc cupping8. However, Chang et al. reported that both CH and CCT correlated negatively with several optic disc parameters by using SD-OCT in myopic subjects19. Of note, measurement error in OCT due to ocular magnification was not considered in Chang’s study. Previous studies have shown that ocular magnification in myopic eyes has important effect on the optic disc measurements22. In this study, the Littmann’s formula was used to adjust the ocular magnification for measurements obtained with OCT. In agree with most previous studies8,20,21, we did not find a significant association between CH and any of the optic disc parameters by using OCT and HRT technology.
The association between CCT and optic nerve parameters in healthy subjects has been reported in previous studies23,24,25. Although a rather weak correlation was detected between CCT and optic disc measurements in the Tajimi study23, most of the studies reported that CCT was not associated with the structural measurements of the optic nerve24,25. In concordance with the previous reports24,25, we found that CCT was not associated with any of optic nerve parameters measured with 3 imaging devices.
There are strengths in the present study. The comprehensive ocular examination in each subject permitted the exclusion of ocular pathologies (myopic chorioretinopathy, vitreomacular traction, myelinated retinal nerve fibres, peripapillary choroidal neovascularization and glaucoma) that are likely to influence the structural measurements of the optic nerve. All three imaging devices were performed on the same visit by the experienced technicians following a standardized protocol. Finally, various parameters were evaluated in correlation with corneal hysteresis. Our findings of no significant relationship between CH and optic nerve parameters were consistent across all three modalities, which reinforce the validity of these findings in the present study population.
However, there are also limitations in the present study. One limitation is that only young myopic subjects of the same ethnicity (all were Chinese) were included in the analysis. Thus, the current results may not apply to other populations. Another limitation is the cross-sectional nature of the present study. Thus, future longitudinal studies with large sample size are warranted to confirm our findings.
In conclusion, no statistically significant relationship was observed between CH and optic nerve parameters as measured by all three imaging modalities in healthy myopic eyes. Therefore, the relationship observed previously in glaucoma subjects is likely coming to fruition as optic nerve damage is caused by the disease.
Methods
Subjects
In this prospective, cross-sectional observational study, 116 Chinese healthy myopic subjects were consecutively recruited from the refractive surgery clinic of Joint Shantou International Eye Center. Each included subjects underwent a detailed ophthalmic examination including the measurement of refraction, visual acuity, intraocular pressure (IOP), central corneal thickness (CCT) measurement by an A-ultrasound pachymeter (Reichert Ophthalmic Instruments, Depew, NY, USA), axial length (IOL master; Carl-Zeiss Meditec, Dublin, CA), and a dilated stereoscopic fundus examination. All the included eyes had a spherical equivalent (SE) less than −0.50 diopters (D) and had no other concurrent ocular disease. One eye from each subject was chosen for analysis; if both eyes were eligible, a random eye was selected by using a computer programme26. Based on the refractive status, subjects were subdivided into two groups: high myopia group (SE ≤ −6.00 D) and low to moderate group (−6.00 D < SE ≤ −0.50). Subjects with best corrected visual acuity less than 20/40, contact lens use, IOP over 21 mmHg, family history of glaucoma, intraocular surgery, myopic macular degeneration, glaucoma, refractive surgery, neurological diseases or diabetes were excluded. The present study followed the tenets of the declaration of Helsinki and was approved by the local ethical committee. Written informed consent was obtained from each subject before enrolment.
Visual field testing
Visual field testing was performed with the static automated white-on-white threshold 24-2 Swedish interactive threshold algorithm standard strategy (Humphrey Field Analyzer II; Carl Zeiss Meditec, Inc.). Only reliable visual field tests (with fixation loss, false positive and false negative were all less than 20%) were used in the study. All the included visual field tests were those with pattern standard deviation (PSD) with P > 5% and within normal limits in glaucoma hemifield test (GHT).
Ocular Response Analyzer Measurement
Corneal hysteresis in each subject was performed with ORA (Reichert Ophthalmic Instruments, Depew, NY, USA), prior to CCT measurement. The details of the principles of the device have been described previously4. The device reports four parameters including corneal hysteresis (CH), corneal resistance factor (CRF), cornea-compensated intraocular pressure (IOPcc) and Goldmann-correlated intraocular pressure (IOPg). For each subject, the ORA examination was performed at least 3 times. The ORA software (Software Version: 2.02) reports a waveform score, ranging from 0 to 10, to ensure accurate measurement. All included ORA measurements had a waveform score no less than 5 in this study. Disqualified measurements (the waveform score less than 5) and irreproducible values were discarded and repeated measurements were performed. The average values of three measurements with desirable curves were recorded for subsequent analysis.
Confocal Scanning Laser Ophthalmoscopy Imaging
Confocal scanning laser ophthalmoscopy (HRT 2; Heidelberg Engineering, GmbH, Dossenheim, Germany) was performed in all included eyes to obtain various optic disc parameters. After image acquisition, a single mean topography for analysis is generated by averaging three aligned consecutive scans. Image quality was checked carefully for all the optic disc images. All the contour lines were manually drawn by a trained ophthalmologist (KQ) and the disc margin was defined as the inner edge of the Elschnig’s ring. Only good quality images with an average pixel height standard deviation no more than 30 µm were included in the analysis. Global optic nerve head parameters including disc area, rim area, cup-to-disc ratio, cup volume and mean cup depth were used for analysis.
Scanning Laser Polarimetry Imaging
Scanning laser polarimetry (SLP) imaging was performed by using GDx ECC algorithm (Carl Zeiss Meditec, Dublin, CA, USA). The eye-specific corneal birefringence consisting of the corneal polarization axis and magnitude was first determined for each subject. The RNFL was then quantified with GDx ECC algorithm (software version 5.5.0.14). Only images with an image quality check score no less than 8 were included. The raw data were exported from the instrument for subsequent analysis. The typical scan score (TSS) of each eye was collected to evaluate the atypical birefringence patterns. Only scans with a TSS no less than 80 were included in the present study27. The parameters of nerve fiber index (NFI), the temporal superior nasal inferior temporal (TSNIT) average RNFL measurement and TSNIT standard deviation (TSNIT-SD) were collected for subsequent analysis.
Optical Coherence Tomography
Each of the included eye received optic disc imaging with the Cirrus High Definition OCT (Cirrus HD OCT, software version 5.0.0.326; Carl Zeiss Meditec, Dublin, CA) by using the Optic Disc Cube 200 × 200 protocol. The axial resolution for this spectral-domain OCT is 5 μm and the scan speed is 27000 A-scans per second. Scans with eye movements (with misaligned vessels within the scanning area) were excluded by reviewing the real-time SLO fundus images. All the included optic disc images had minimum signal strength of 7. The overall average RNFL thickness and optic disc parameters including disc area, rim area, average cup disc area ratio (ACDR) and vertical cup disc ratio (VCDR) were recorded from the analysis printout generated by Cirrus HD OCT.
Adjustment for Ocular Magnification of Cirrus HD-OCT
According to previous studies, the relationship between the OCT measurement and its actual size can be expressed as t = p × q × s, where t is the actual fundus dimension, p is the magnification factor of the camera of the HD-OCT system, s the measurement obtained from the OCT system, and q the magnification factor of the eye22. For the HD-OCT system, p is known to be 3.382. The ocular magnification factor q of the eye can be calculated with the formula q = 0.01306 × (axial length − 1.82). Because t = p × q × s refers to linear magnification, the equation would be modified to t 2 = p 2 × q 2 × s 2 for both area and volume measurements (ocular magnification has no influence on the z-axis).
-
To adjust area parameters (disc area and rim area), the following formula was used:
Corrected area = 3.3822 × 0.013062 × (axial length −1.82)2 × measured area
-
As ocular magnification has no influence on the z-axis, the following formula was used to adjust volume parameters:
Corrected volume = 3.3822 × 0.013062 × (axial length−1.82)2 × measured volume
-
To adjust average RNFL thickness measurement, the following formula was used:
Corrected average RNFL thickness = 3.382 × 0.01306 × (axial lengh −1.82) × measured average RNFL thickness
The corrected average RNFL thickness and optic disc measurements were used in the statistical analysis.
Statistical Analysis
The statistical analyses were performed by using the SPSS software (ver. 17.0; SPSS Inc, Chicago, IL) and MedCalc software (ver. 12.1.4.0; Belgium). Spearman’s correlation analysis was performed to determine the effects of axial length/refractive error, CCT, and corneal biomechanics on various optic nerve parameters. Sample size calculation revealed that at least 85 eyes would be required to determine whether a correlation coefficient +/− 0.30 (a weak correlation) differs from zero with a statistical power of 80% at an alpha of 0.05. A p value less than 0.05 was considered statistically significant.
References
Matsuura, M. et al. The usefulness of CorvisST Tonometry and the Ocular Response Analyzer to assess the progression of glaucoma. Sci Rep. 17(7), 40798, https://doi.org/10.1038/srep40798 (2017 Jan).
Pillunat, K. R., Hermann, C., Spoerl, E. & Pillunat, L. E. Analyzing biomechanical parameters of the cornea with glaucoma severity in open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 254(7), 1345–51, https://doi.org/10.1007/s00417-016-3365-3 (2016 Jul).
Zimmermann, M., Pitz, S., Schmidtmann, I., Pfeiffer, N. & Wasielica-Poslednik, J. Tonographic Effect of Ocular Response Analyzer in Comparison to Goldmann Applanation Tonometry. PLoS One. 12(1), e0169438, https://doi.org/10.1371/journal.pone.0169438 (2017).
Luce, D. A. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg 31, 156–62 (2005).
Prata, T. S. et al. Association between corneal biomechanical properties and optic nerve head morphology in newly diagnosed glaucoma patients. Clin Experiment Ophthalmol 40, 682–88, https://doi.org/10.1111/j.1442-9071.2012.02790.x (2012).
Medeiros, F. A. et al. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology 120, 1533–40, https://doi.org/10.1016/j.ophtha.2013.01.032 (2013).
Zhang, C. et al. Corneal Hysteresis and Progressive Retinal Nerve Fiber Layer Loss in Glaucoma. Am J Ophthalmol. 166, 29–36, https://doi.org/10.1016/j.ajo.2016.02.034 (2016 Jun).
Carbonaro, F., Hysi, P. G., Fahy, S. J., Nag, A. & Hammond, C. J. Optic disc planimetry, corneal hysteresis, central corneal thickness, and intraocular pressure as risk factors for glaucoma. Am J Ophthalmol 157, 441–46, https://doi.org/10.1016/j.ajo.2013.10.017 (2014).
Khawaja, A. P. et al. Corneal biomechanical properties and glaucoma-related quantitative traits in the EPIC-Norfolk eye. Invest Ophthalmol Vis Sci. 55(1), 117–24, https://doi.org/10.1167/iovs.13-13290 (2014).
Katz, J., Tielsch, J. M. & Sommer, A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci 38(2), 334–40 (1997).
Marcus, M. W., de Vries, M. M., Junoy Montolio, F. G. & Jansonius, N. M. Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology. 118(10), 1989–94, https://doi.org/10.1016/j.ophtha.2011.03.012 (2011 Oct).
Fong, D. S., Epstein, D. L. & Allingham, R. R. Glaucoma and myopia: are they related? Int Ophthalmol Clin 30, 215–18 (1990).
Han, J. C., Cho, S. H., Sohn, D. Y. & Kee, C. The Characteristics of Lamina Cribrosa Defects in Myopic Eyes With and Without Open-Angle Glaucoma. Invest Ophthalmol Vis Sci. 57(2), 486–94, https://doi.org/10.1167/iovs.15-17722 (2016 Feb).
Sawada, Y., Araie, M., Ishikawa, M. & Yoshitomi, T. Multiple Temporal Lamina Cribrosa Defects in Myopic Eyes with Glaucoma and Their Association with Visual Field Defects. Ophthalmology. pii: S0161-6420(17)30254-3. https://doi.org/10.1016/j.ophtha.2017.04.027 (2017 May 24).
Del Buey, M. A. et al. Assessment of corneal biomechanical properties and intraocular pressure in myopic spanish healthy population. J Ophthalmol. 905129, https://doi.org/10.1155/2014/905129 (2014).
Roberts, C. J. et al. Comparison of ocular biomechanical response parameters in myopic and hyperopic eyes using dynamic bidirectional applanation analysis. J Cataract Refract Surg. 40(6), 929–36, https://doi.org/10.1016/j.jcrs.2014.04.011 (2014 Jun).
Uysal, B. S. et al. Can Corneal Biomechanical Properties Give Clues About Elasticity of Optic Nerve Scleral Component in Nonarteritic Anterior Ischemic Optic Neuropathy? Neuroophthalmol. 36(3), 285–9, https://doi.org/10.1097/WNO.0000000000000406 (2016).
Bueno-Gimeno, I., Gene-Sampedro, A., Piñero-Llorens, D. P., Lanzagorta-Aresti, A. & España-Gregori, E. Corneal biomechanics, retinal nerve fiber layer, and optic disc in children. Optom Vis Sci. 91(12), 1474–82, https://doi.org/10.1097/OPX.0000000000000406 (2014 Dec).
Chang, P. Y. & Chang, S. W. Corneal biomechanics, optic disc morphology, and macular ganglion cell complex in myopia. J Glaucoma. 22(5), 358–62, https://doi.org/10.1097/IJG.0b013e3182447a17 (2013).
Lim, L. et al. Corneal biomechanics, thickness and optic disc morphology in children with optic disc tilt. Br J Ophthalmol. 92(11), 1461–66, https://doi.org/10.1136/bjo.2008.139113 (2008 Nov).
Insull, E. et al. Optic disc area and correlation with central corneal thickness, corneal hysteresis and ocular pulse amplitude in glaucoma patients and controls. Clin Experiment Ophthalmol. 38(9), 839–44, https://doi.org/10.1111/j.1442-9071.2010.02373.x (2010 Dec).
Kang, S. H., Hong, S. W., Im, S. K., Lee, S. H. & Ahn, M. D. Effect of myopia on the thickness of the retinal nerve fiber layer measured by Cirrus HD optical coherence tomography. Invest Ophthalmol Vis Sci. 51(8), 4075–83, https://doi.org/10.1167/iovs.09-4737 (2010 Aug).
Abe, H. et al. Laser scanning tomography of optic discs of the normal Japanese population in a population based setting. Ophthalmology. 116, 223–30, https://doi.org/10.1016/j.ophtha.2008.09.013 (2009).
Hawker, M. J., Edmunds, M. R., Vernon, S. A., Hillman, J. G. & MacNab, H. K. The relationship between central corneal thickness and the optic disc in an elderly population: the Bridlington Eye Assessment Project. Eye. 23, 56–62 (2009).
Mumcuoglu, T. et al. Assessing the Relationship between Central Corneal Thickness and Retinal Nerve Fiber Layer Thickness in Healthy Subjects. Am J Ophthalmol. 146(4), 561–6, https://doi.org/10.1016/j.ajo.2008.05.038 (2008 Oct).
Urbaniak, G. C. & Plous, S. Research Randomizer (Version 4.0) [Computer software]. Retrieved on January 20, from http://www.randomizer.org/ (2017).
Qiu, K. et al. Predictors of atypical birefringence pattern in scanning laser polarimetry. Br J Ophthalmol. 93(9), 1191–94, https://doi.org/10.1136/bjo.2008.152595 (2009 Sep).
Acknowledgements
The present study was supported by Grant No. 81486126, from the National Nature Science Foundation of China; from the National Nature Science Foundation of China; by Grant No. 2013B022000091, from Science and Technology Planning Project of Guangdong Province, China; by Grant No. 2014KQNCX075, from Foundation for Distinguished Young Talents in Higher Education of Guangdong, China; and by the University of Groningen Abel Tasman Talent Program (University Medical Center Groningen/Shantou University Medical College). The funding organizations had no role in the design, conduct, analysis, or publication of this research.
Author information
Authors and Affiliations
Contributions
Involved in study design and conduct (M.Z., K.Q.); data collection, management, analysis (K.Q., X.L., G.W., R.Z.), and interpretation (M.Z., K.Q.); and manuscript preparation, review, or approval (M.Z., K.Q.)
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qiu, K., Lu, X., Zhang, R. et al. Relationship of corneal hysteresis and optic nerve parameters in healthy myopic subjects. Sci Rep 7, 17538 (2017). https://doi.org/10.1038/s41598-017-15386-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-15386-6
This article is cited by
-
Comparison of two analyzer measurements focusing on material stiffness among normal, treatment-naïve, and treated glaucoma eyes
Scientific Reports (2023)
-
Nasal and temporal curvatures of lamina CRIBROSA in myopic eyes
Scientific Reports (2022)
-
Effect of biomechanical properties on myopia: a study of new corneal biomechanical parameters
BMC Ophthalmology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.