Abstract
Currently, little information is available to stratify the risks and predict acute kidney injury (AKI)-associated death. In this present cross-sectional study, a novel scoring model was established to predict the probability of death within 90 days in patients with AKI diagnosis. For establishment of predictive scoring model, clinical data of 1169 hospitalized patients with AKI were retrospectively collected, and 731 patients of them as the first group were analyzed by the method of multivariate logistic regression analysis to create a scoring model and further predict patient death. Then 438 patients of them as the second group were used for validating this prediction model according to the established scoring method. Our results showed that Patient’s age, AKI types, respiratory failure, central nervous system failure, hypotension, and acute tubular necrosis-individual severity index (ATN-ISI) score are independent risk factors for predicting the death of AKI patients in the created scoring model. Moreover, our scoring model could accurately predict cumulative AKI and mortality rate in the second group. In conclusion, this study identified the risk factors of 90-day mortality for hospitalized AKI patients and established a scoring model for predicting 90-day prognosis, which could help to interfere in advance for improving the quality of life and reduce mortality rate of AKI patients.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a common complication among hospitalized patients, and is an important cause for in-hospital death. In recent years, the incidence of AKI continues increasing at an annual growth rate of 11%1. In the past 25 years, this incidence has increased by at least 20 times2. AKI has a death rate as high as 20%, which may reach up to 50% in the intensive care unit (ICU)3, 4. Each year, around two million people die of AKI worldwide5. AKI is not only a medical problem, but also has become a major public health concern.
Referring to different diagnostic criteria of AKI, currently there are 35 descriptions recorded in literature worldwide6, 7. The acute kidney injury network (AKIN) criteria are further formulated according to the RIFLE criterion (risk, injury, failure, loss, end stage renal disease)8. Evidently, RIFLE and AKIN criteria have made tremendous contributions for the diagnosis and treatment of AKI9. However, due to various restrictions, AKI was redefined on the basis of RIFLE and AKIN criteria by the Kidney Disease Improving Global Organization (KDIGO)8. In March 2012 the “KDIGO acute kidney injury clinical practice guidelines” was released10. Studies had identified that the outcome prediction performance of KDIGO classification is superior to that of AKIN or RIFLE classification in critically ill patients8, 11. The patients were diagnosed and classified again according to the latest KDIGO clinical practice guidelines in our research.
The representative AKI prognosis scoring systems included Acute Physiology and Chronic Health Evaluation (APACHE II), Simplified Acute Physiology Score (SAPS II), Mortality Probability Models (MPM II), Acute tubular necrosis-individual severity degree index (ATN-ISI), Sequential Organ Failure Assessment (SOFA) and Stuivenberg hospital acute renal failure scores (SHARF) can predict outcomes in patients with AKI. Most study index of the above scoring systems were derived from ICU and were more suitable for the critically ill patients with multiple organ failures in ICU12,13,14. Therefore, the aims of present study were to further evaluate the risk factors of death for hospitalized AKI patients and establish a new scoring model for predicting 90-day mortality rate after AKI diagnosis according to KDIGO criteria.
Methods
Study design and patient population
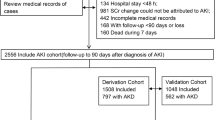
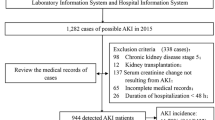
1169 cases of AKI inpatients admitted in the Second Xiangya Hospital of Central South University were selected from January 1996 to April 2013, and all conformed to the KDIGO criteria. A total of 731 patients were treated as the test group, including 454 males and 277 females with an average age of 48.49. And 438 cases were treated as the validation group, including 266 males and 172 females, with an average age of 52.66. Patients with uncompleted medical history or lack of basic information, with stages 5 chronic kidney disease (CKD) and those receiving maintenance dialysis or renal transplantation were excluded. For patients with multiple hospitalizations, we only included only the first hospitalization in the analysis set15. The medical ethics community of the Second Xiangya Hospital approved the study protocol and waived patient consent. AKI types included hospital-acquired AKI and community-acquired AKI16. Flow chart of study population selection and research process was shown in Fig. 1. In addition, we established another validating dataset containing 409 AKI patients hospitalized in another three hospitals (Xiangya Hospital, Third Xiangya Hospital of Central South University and the First Affiliated Hospital of Hunan University of Chinese Medicine) from January 2015 to June 2015 and further validated the predictive performance, stability and repeatability of new score, basic data was shown in Supplementary Table S1.
Study parameters, endpoint and outcomes
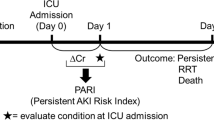
The patients’ data, including age, gender, AKI types, causes of AKI, urine volume, past medical history (CKD, diabetes, hypertension, etc.), mechanical ventilation, sepsis, shock, organ failure, laboratory indexes on admission (hemoglobin, serum albumin, blood urea nitrogen (BUN) peak value, Scr peak value, serum potassium ions (K+) peak value, etc.), ATN-ISI, hospital stay, renal replacement therapy (RRT), clinical outcome and other clinical data were analyzed. The observation starting point was community-acquired AKI 24 hours after admission to hospital or hospital-acquired AKI diagnosis after 24 hours. The observation endpoint was patients’ death or 90 days after AKI diagnosis. The survival state (survive or death) during 90 days were calculated as the endpoint event, ruling out accident harm to death et al.
Definitions
AKI (based on the KDIGO classification); CKD (based on abnormalities of kidney function or structure, and present for >3 months; Proteinuria (defined as exceed 150 mg/24 h); Baseline Scr was the first value measured during hospitalization or the value within 3 months at most 1 year when baseline Scr was unknown within 1 week during hospitalization, the estimated GFR was calculated according to MDRD equation17, 18.
Oliguria (defined as urine volume <400 ml/24 h); Anuria (defined as urine volume <100 ml/24 h); Shock (defined as hypotension with systolic arterial blood pressure of 90 mm Hg despite adequate fluid resuscitation); Heart failure (based on Framingham criteria and defined as New York Heart Association functional class IV); Respiratory failure (need for mechanical ventilation); Gastrointestinal failure (stress ulcers requiring transfusion, acalculus cholecystitis); Central nervous system failure (Progressive coma); Hepatic failure (clinical jaundice with bilirubin. 8–l0 mg/dL).
Cardio-renal syndromes was defined by Acute Dialysis Quality Initiative consensus group; Hepatorenal syndrome: was defined according to the European Association of Liver Study criteria; sepsis (according to the American College of Chest Physicians – Society of Critical Care Medicine consensus definition); Organic kidney disease: renal parenchymal diseases including glomerular disease and renal microvascular disease, renal vascular disease, acute interstitial nephritis, intratubular obstruction except for ATN. Acute tubular necrosis was arisen as a consequence of septic, toxic, or ischemic insult. Post-renal obstruction: bladder outlet obstruction, tumors, renal calculi, papillary necrosis, retroperitoneal fibrosis19,20,21.
Statistical analysis
The collected data were employed to establish a qualified database and were statistically analyzed using SPSS 19.0 and SAS 9.3. The data of normal distribution were presented using mean ± standard deviation. The data without abnormal distribution were shown using the median and inter-quartile range (IQR) and statistically analyzed after logarithmic transformation. The enumeration data were shown using the rate and chi-square test. The mean comparison between the two groups was conducted using the Student’s t-test. The mortality related independent risk factors were analyzed using the multivariate logistic regression analysis. The trend test was conducted using chi-square trend test. The rank sum test was used to determine the difference between groups. CMH χ2 test (Cochran mantel haeszel statistics) was used to verify the predictability of forewarning model. In addition, the Hosmer-Lemeshow goodness-of-fit test was used for calibration when evaluating the number of observed and predicted deaths in AKI patients for the entire range of death probabilities. Discrimination was assessed using the area under a receiver operating characteristic curve (AUROC), which was compared with a nonparametric approach. The AUROC analysis calculated cutoff values, sensitivity, specificity, and positive predictive value. Finally, Youden index was defined as Sensitivity + Specificity −1, and the cutoff point was chosen by the best Youden index22. A p value of less than 0.05 was considered to be statistically significant.
Results
Baseline characteristics
A total of 1169 patients were included, including 720 males and 449 females. The age ranged from 15 to 93, and the average age was 50.05. There were 731 cases in the test group, including 454 males and 277 females. The age ranged from 15 to 93 with an average age of 48.49. There were 438 patients in the validation group, including 266 males and 172 females. The age ranged from 15 to 90 with an average age of 52.66. There was no significant difference in various indexes between the two groups (P > 0.05). The results were shown in Table 1. We also found that the length of hospital stay had no correlation with death rate of hospitalized AKI patients (Table 2).
Comparison of prognostic parameters within 90 days after AKI diagnosis between survival group and death group in patients with acute kidney injury
As shown in Table 3, there was no statistical difference between the two groups in gender, baseline Scr, baseline eGFR, KDIGO staging, proteinuria, hematuresis, oliguria or anuria, CKD, diabetes mellitus, hypertension, sepsis, hepatic failure, Hb < 90 g/L, hypoalbuminemia, hospital stay, Scr peak value and replacement therapy between two groups (P > 0.05). Age, AKI types, causes of AKI, mechanical ventilation, hypotension, shock, heart failure, respiratory failure, digestive failure, central nervous system failure, BUN peak value, K+ peak value and ATN-ISI score had significantly statistical difference (P < 0.05).
All-cause mortality rate between the test group and validation group in patients with acute kidney injury
The all-cause mortality in the test group and validation group were counted in 90 days. In the test group, 101 cases occurred to the all-cause death within 90 days, showing a mortality rate of 13.8%; in the validation group, 51 cases occurred in the all-cause death within 90 days manifesting a mortality rate of 11.6%. Our results indicated that there is no significant difference between all-cause mortality of the two group (p > 0.05).
Establishment of the death independent risk factors in the test group within 90 days after AKI diagnosis in patients with acute kidney injury
The basic data of 90-day prognosis in the test group were compared between the survival group and death group. The parameters including age, AKI types, causes of AKI, mechanical ventilation, hypotension, shock, heart failure, respiratory failure, gastrointestinal failure, central nervous system failure, BUN peak value, K+ peak value and ATN-ISI score between the two groups showed statistical significance (p < 0.05). The further multivariate logistic regression analysis indicated that age, AKI types, respiratory failure, central nervous system failure, hypotension, ATN-ISI score were the independent risk factors of death (shown in Table 4). The corresponding integrals of various odds ratio (OR) values were endowed according to the principle of round.
Establishment, trend and fitting degree tests of prognostic scoring system within 90 days after AKI diagnosis in patients with acute kidney injury
Each patient’s score was calculated. As shown in Table 5, the formula was as follow: score of 90-day prognosis = the points of age + the points of AKI types + the points of respiratory failure + the points of central nervous system failure + the points of hypotension + the points of ATN-ISI score. The scoring criteria were as follow: 0 point for age 15~39, 2 points for age 40~64, 4 points for age greater than 65; 0 point for community-acquired AKI and 2 points for hospital-acquired AKI; 6 points for having respiratory failure, and 0 point for not having respiratory failure; 3 points for having central nervous system failure, and 0 point for not having central nervous system failure; 3 points for having hypotension, and 0 point for not having hypotension; 0 point for ATN-ISI score < 0.4 and 2 points for ≥0.4. The score sum of each patient and the mortality rate of each score were respectively calculated.
With the increase of the total score, the mortality rate in the test group was increased. The trend was shown in Fig. 2. The result showed that the mortality rates had statistical significance (P < 0.01). It was predicted that the area under ROC curve of 90-day mortality rate was 0.833 (95% CI: 0.788~0.879), P < 0.001, showing the predictability of the scoring system was reliable. The chi-square trend test was used in the validation group and the result showed that the mortality rates had statistical significance (P < 0.01). It was predicted that the area under ROC curve of 90-day mortality rate was 0.832 (95% CI: 0.764~0.901), P < 0.01. The mortality rates compared between the test group and validation group using rank sum test showed no statistical significance (P = 0.907), and the fitting degree was good (Table 7, Figs 3 and 4).
Establishment and preliminary application of 90-day prognosis forewarning model
The further risk stratification forewarning models were established according to the above 90 days-prognosis scoring system. The test group and validation group were divided into two risk stratification respectively according to the cut-off point: < 5 (low-risk patients), ≥5 (high-risk patients). The mortality rates of the test groups were 5.6% in low-risk patients and 38.5% in high-risk patients. The mortality rates of the validation groups were 4.6% in low-risk patients and 37.6% in high-risk patients. There were no significant differences in AKI death rate in 90-day-prognosis between the test group and validation group by CMH χ2 test (Cochran mantel haeszel Statistics). Significant difference was found between patients with low risk and high risk (all p < 0.00), and it was further demonstrated that the higher new score result in the higher cumulative AKI and mortality (Fig. 5).Our result showed that the new scoring model had good prediction ability on AKI mortality rate (Table 6).
Comparison of new scores, SOFA and ATN-ISI in predicting 90-day mortality after AKI diagnosis
As for the assessment of calibration, Table 7 lists goodness-of-fit measured by the Hosmer-Lemeshow analysis to predict hospitalized AKI mortality risk and the predictive accuracy of the new scores, SOFA and ATN-ISI in the test and validation groups. In predicting the cumulative AKI and mortality rates, as shown in Tables 7 and 8, Figs 2 and 3, Supplementary Figure S1, Supplementary Table S2 and Supplementary Table S3, new score showed a large AUROC (0.833, 0.832, and 0.830) and stable specificity (82%, 85%, and 82%) in test group, validation group and the second validating dataset, respectively, suggesting that our model showed good stability and repeatability in different datasets. To assess the values of selected cutoff points for predicting AKI mortality, the sensitivity, specificity and positive predictive value were determined (Table 8, Supplementary Table S3). Positive predictive values of new score among test group, validation group and the second validating dataset were 87%, 89% and 90%, while SOFA is 91%, 75% and 84%, ATN-ISI is 90%, 67% and 70%, indicated that all three models had good fitting degree of positive predictive value.
Discussion
Excitingly, a new prediction scoring model for 90-day mortality of hospitalized patients diagnosed with AKI was established in our study. It could help clinicians to accurately predict the prognosis of AKI patients, improve quality of life and reduce mortality of AKI patients.
Even with 35 different description of AKI listed in papers worldwide, we lacked a specific and single definition. AKI classification diagnostic criterion is also constantly updating and developing along with the change of the definition. The KDIGO put forward the new classification diagnostic criteria in 2012 on the basis of the improvements of RIFLE and AKIN8. Its diagnostic sensitivity and specificity obtained further ascension, so we chose KDIGO criteria in this research.
In our study, the 90-day mortality rate of AKI inpatients was 11.6%~13.8%. Bellomo R and Palevsky PM et al. showed that the mortality rate of critically ill patients with AKI was 40%~70%23, 24. Sara Nisula reported that mortality rate of 1141 cases of AKI inpatients was 25.6% and the mortality rate of 90-day-progonsis was 33.7%25. Other scholars reported that the mortality rate of AKI patients was 32% in 28 days26, 44.7% and 52.5% in 90 days23, 24 and 57.5% in 2 years27. The reasons of different mortality rates might be related to diagnosis standard, patients selection, the improvement of the treatment level, racial difference, basic disease, complication, cultural difference, individual economy and medical insurance difference. With the development of the treatment level and the emergence of new technology, the cure rate would change as well as the mortality.
The identification of risk factors for poor prognosis of AKI patients is required so that preventive and early diagnosis measures can be taken to reduce patients’ mortality. Our previous publication showed that age, AKI types, hypotension, multi-organ failure and ATN-ISI score and K+ concentration were the death related independent risk factors of AKI inpatients28. Other researchers reported that AKI classification, hypoalbuminemia, hypovolemia before admitting into ICU, baseline serum creatinine, ICU stay, more than four organs function failure, mechanical ventilation, sepsis and AKI attributable to nephrotoxic agents, and oliguria occurrence at AKI diagnosis, were independent significant prognostic indicators, especially preexisting CKD is the greatest known risk factor for the development of AKI29,30,31,32,33,34,35,36. Based on our previous work and parameters mentioned above, we observed the death-related risk parameters in this study. Our present results showed that age, AKI types, hypotension, respiratory failure, central nervous system failure and ATN-ISI score were the death independent risk factors in 90 days of the test patients, which suggested that death related risk factors of AKI patients may be related to diagnosis standard and following-term, patient selection, the improvement of the treatment level et al.
Also, establishment of forewarning model, identification of patients at high risk and early intervention are the keys to successful rescue and low mortality in AKI patients. The representative AKI prognosis scoring systems included APACHE II, SAPS II, MPM II, ATN-ISI, SOFA and SHARF et al. Most study index of the above scoring systems were derived from ICU, which may not suit for all hospitalized AKI patients. Moreover, in China, there has been no large-scale multi-center study and the scope of application was limited. Recently AKI morbidity model after cardiovascular surgery was published, but still has limited scope of application in other types of AKI inpatients37. In short, there were few studies on the forewarning model of the prognosis for Chinese AKI inpatients according to KDIGO criteria.
In this study, we focused on the short-term death risk assessment of hospitalized AKI patients with simple size of 1169 patients according to the latest KDIGO criterion. The forewarning model of 90 days after hospitalized patients with AKI diagnosis was built. The mortality rate of total score <5 was 5.6% while the mortality rate of total score ≥5 was 38.5%. The risk stratification forewarning model had good predictive value as observed through validation group. We found that the new scoring model, SOFA and ATN-ISI are all effective in predicting short-term mortality. Moreover, the new scoring model showed a large AUROC and stable specificity in the test group, the validation group and the second validating dataset, respectively, suggesting that our model showed good stability and repeatability in different datasets and may be developed into a potential tool for predicting short-term mortality of hospitalized AKI patients.
This new scoring model can provide some benefits for AKI patients with high risks, such as improvement of the accuracy of nursing grades; early consultation for hospital multi-disciplinary team; timely detection and correction of reversible risk factors. Our medical staff should continue to track and follow up high risk patients after discharge. This new model will help to improve life quality of AKI patients, and reduce medical disputes.
Our study still has some limitations. First, this was a retrospective study which limits the generalization of its findings; Second, it was a single-province multi-center study which may not be directly applicable to other patient populations; Third, we did not do further study on whether the change of new score has a correlation with the long-term prognosis. Therefore, multi-center prospective trials are still necessary to evaluate the accuracy of the new score in predicting 90-day mortality and long-term mortality of AKI patients.
In summary, we established a new prediction scoring model to predict mortality for hospitalized patients with AKI. The predictive mortality rate was close to the actual mortality rate. This prediction scoring model provides a portable tool for clinicians to identify high risk patients early and accurately predict the prognosis of AKI patients to reduce mortality of AKI patients.
References
Waikar, S. S., Curhan, G. C., Wald, R., McCarthy, E. P. & Chertow, G. M. Declining mortality in patients with acute renal failure, 1988 to 2002. Journal of the American Society of Nephrology: JASN 17, 1143–1150, doi:10.1681/ASN.2005091017 (2006).
Murugan, R. & Kellum, J. A. Acute kidney injury: what’s the prognosis? Nature reviews. Nephrology 7, 209–217, doi:10.1038/nrneph.2011.13 (2011).
Susantitaphong, P. et al. World incidence of AKI: a meta-analysis. Clinical journal of the American Society of Nephrology: CJASN 8, 1482–1493, doi:10.2215/CJN.00710113 (2013).
Fang, Y. et al. Acute kidney injury in a Chinese hospitalized population. Blood purification 30, 120–126, doi:10.1159/000319972 (2010).
Uchino, S. et al. Acute renal failure in critically ill patients: a multinational, multicenter study. Jama 294, 813–818, doi:10.1001/jama.294.7.813 (2005).
Hoste, E. A. & Kellum, J. A. Acute kidney injury: epidemiology and diagnostic criteria. Current opinion in critical care 12, 531–537, doi:10.1097/MCC.0b013e3280102af7 (2006).
Hoste, E. A. & Schurgers, M. Epidemiology of acute kidney injury: how big is the problem? Critical care medicine 36, S146–151, doi:10.1097/CCM.0b013e318168c590 (2008).
Pan, H. C. et al. Acute Kidney Injury Classification for Critically Ill Cirrhotic Patients: A Comparison of the KDIGO, AKIN, and RIFLE Classifications. Scientific reports 6, 23022, doi:10.1038/srep23022 (2016).
Xiong, J. et al. The RIFLE versus AKIN classification for incidence and mortality of acute kidney injury in critical ill patients: A meta-analysis. Scientific reports 5, 17917, doi:10.1038/srep17917 (2015).
Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron. Clinical practice 120, c179–184, doi:10.1159/000339789 (2012).
Li, Z. et al. Identification and predicting short-term prognosis of early cardiorenal syndrome type 1: KDIGO is superior to RIFLE or AKIN. PloS one 9, e114369, doi:10.1371/journal.pone.0114369 (2014).
Sawicka, W., Owczuk, R., Wujtewicz, M. A. & Wujtewicz, M. The effectiveness of the APACHE II, SAPS II and SOFA prognostic scoring systems in patients with haematological malignancies in the intensive care unit. Anaesthesiology intensive therapy 46, 166–170, doi:10.5603/AIT.2014.0030 (2014).
Wang, L. et al. Urinary liver-type fatty acid-binding protein predicts recovery from acute kidney injury. Clinical nephrology 84, 255–261, doi:10.5414/CN108635 (2015).
Lins, R. L. et al. Re-evaluation and modification of the Stuivenberg Hospital Acute Renal Failure (SHARF) scoring system for the prognosis of acute renal failure: an independent multicentre, prospective study. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association 19, 2282–2288, doi:10.1093/ndt/gfh364 (2004).
Xu, X. et al. Epidemiology and Clinical Correlates of AKI in Chinese Hospitalized Adults. Clinical journal of the American Society of Nephrology: CJASN 10, 1510–1518, doi:10.2215/CJN.02140215 (2015).
Wonnacott, A., Meran, S., Amphlett, B., Talabani, B. & Phillips, A. Epidemiology and outcomes in community-acquired versus hospital-acquired AKI. Clinical journal of the American Society of Nephrology: CJASN 9, 1007–1014, doi:10.2215/CJN.07920713 (2014).
Tarng, D. C. Cardiorenal anemia syndrome in chronic kidney disease. Journal of the Chinese Medical Association: JCMA 70, 424–429, doi:10.1016/S1726-4901(08)70031-5 (2007).
Ma, Y. C. et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. Journal of the American Society of Nephrology: JASN 17, 2937–2944, doi:10.1681/ASN.2006040368 (2006).
Ronco, C. et al. Cardio-renal syndromes: report from the consensus conference of the acute dialysis quality initiative. European heart journal 31, 703–711, doi:10.1093/eurheartj/ehp507 (2010).
Bone, R. C. et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101, 1644–1655 (1992).
Wu, C. L. et al. Tubular Peroxiredoxin 3 as a Predictor of Renal Recovery from Acute Tubular Necrosis in Patients with Chronic Kidney Disease. Scientific reports 7, 43589, doi:10.1038/srep43589 (2017).
Chang, C. H. et al. Acute kidney injury enhances outcome prediction ability of sequential organ failure assessment score in critically ill patients. PloS one 9, e109649, doi:10.1371/journal.pone.0109649 (2014).
Investigators, R. R. T. S. et al. Intensity of continuous renal-replacement therapy in critically ill patients. The New England journal of medicine 361, 1627–1638, doi:10.1056/NEJMoa0902413 (2009).
Network, V. N. A. R. F. T. et al. Intensity of renal support in critically ill patients with acute kidney injury. The New England journal of medicine 359, 7–20, doi:10.1056/NEJMoa0802639 (2008).
Nisula, S. et al. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive care medicine 39, 420–428, doi:10.1007/s00134-012-2796-5 (2013).
Sprung, C. L. et al. Hydrocortisone therapy for patients with septic shock. The New England journal of medicine 358, 111–124, doi:10.1056/NEJMoa071366 (2008).
Fuchs, L. et al. Severity of acute kidney injury and two-year outcomes in critically ill patients. Chest 144, 866–875, doi:10.1378/chest.12-2967 (2013).
Duan, S. et al. [RIFLE and AKIN criteria for mortality and risk factors of acute kidney injury in hospitalized patients]. Zhong nan da xue xue bao. Yi xue ban=Journal of Central South University. Medical sciences 38, 1243–1252, doi:10.3969/j.issn.1672-7347.2013.12.007 (2013).
Zhou, J., Yang, L., Zhang, K., Liu, Y. & Fu, P. Risk factors for the prognosis of acute kidney injury under the Acute Kidney Injury Network definition: a retrospective, multicenter study in critically ill patients. Nephrology 17, 330–337, doi:10.1111/j.1440-1797.2012.01577.x (2012).
Li, Q. L. et al. [Risk factors and short-term prognosis of acute kidney injury in elderly patients]. Zhonghua yi xue za zhi 93, 2715–2718 (2013).
Hsu, R. K. & Hsu, C. Y. The Role of Acute Kidney Injury in Chronic Kidney Disease. Seminars in nephrology 36, 283–292, doi:10.1016/j.semnephrol.2016.05.005 (2016).
Lafrance, J. P., Djurdjev, O. & Levin, A. Incidence and outcomes of acute kidney injury in a referred chronic kidney disease cohort. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association 25, 2203–2209, doi:10.1093/ndt/gfq011 (2010).
Ali, T. et al. Incidence and outcomes in acute kidney injury: a comprehensive population-based study. Journal of the American Society of Nephrology: JASN 18, 1292–1298, doi:10.1681/ASN.2006070756 (2007).
Cruz, D. N. & Ronco, C. Acute kidney injury in the intensive care unit: current trends in incidence and outcome. Critical care 11, 149, doi:10.1186/cc5965 (2007).
James, M. T. et al. Glomerular filtration rate, proteinuria, and the incidence and consequences of acute kidney injury: a cohort study. Lancet 376, 2096–2103, doi:10.1016/S0140-6736(10)61271-8 (2010).
Pan, H. C. et al. A nationwide survey of clinical characteristics, management, and outcomes of acute kidney injury (AKI) - patients with and without preexisting chronic kidney disease have different prognoses. Medicine 95, e4987, doi:10.1097/MD.0000000000004987 (2016).
Thakar, C. V., Arrigain, S., Worley, S., Yared, J. P. & Paganini, E. P. A clinical score to predict acute renal failure after cardiac surgery. Journal of the American Society of Nephrology: JASN 16, 162–168, doi:10.1681/ASN.2004040331 (2005).
Acknowledgements
This study was funded by National Natural Science Foundation of China (No. 81570618). Especially thanks Professor Wen-Lan Liu from University of New Mexico Health Sciences Center for his contribution on language modification.
Author information
Authors and Affiliations
Contributions
Research idea and study design: S.B.D.; data acquisition: M.L., J.X.; data analysis/interpretation: W.C., X.W.L., H.L., Y.Y.; statistical analysis: M.M.T., F.Y.L., Y.Y., supervision or mentorship: F.Y.L., H.L., S.B.D., The manuscript was prepared by M.L. and was checked or revised by S.B.D.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luo, M., Yang, Y., Xu, J. et al. A new scoring model for the prediction of mortality in patients with acute kidney injury. Sci Rep 7, 7862 (2017). https://doi.org/10.1038/s41598-017-08440-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-08440-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.