Abstract
Few studies have compared the prevalence of smoking between patients with bipolar disorder, major depressive disorder (MDD) and schizophrenia. This study examined the prevalence of smoking and its relationships with demographic and clinical characteristics, and quality of life (QOL) in patients with these psychiatric disorders. A total of 1,102 inpatients were consecutively screened. Psychopathology and QOL were measured with standardized instruments. The prevalence of current smoking in the whole sample was 16.7%; 17.5% in bipolar disorder, 10.6% in MDD and 18.5% in schizophrenia. The rates of smoking in bipolar disorder (p = 0.004, OR = 2.5, 95%CI: 1.3–4.7) and schizophrenia (p = 0.03, OR = 2.0, 95%CI: 1.06–3.8) were significantly higher than in MDD, while no difference was found between bipolar disorder and schizophrenia. Smokers had a higher mental QOL than non-smokers (p = 0.007) in MDD, but no difference was found in the other two groups. Male gender, living alone, higher personal income, older age of onset, health insurance coverage, and first episode was significantly associated with smoking in one or more diagnostic groups. Smoking appears more common in bipolar disorder and schizophrenia than in MDD in China. The figures in all disorders were lower than that reported in most of other countries.
Similar content being viewed by others
Introduction
Smoking is a major public health challenge worldwide, killing around six million people per year1. Evidence has shown that patients with major psychiatric disorders are prone to smoking2,3,4,5,6,7,8,9,10. A meta-analysis found prevalence of smoking in schizophrenia was 62%, which is 5.3 times higher than in the general population4. In Western studies, the prevalence of smoking in other psychiatric disorders seems to be lower than in schizophrenia, e.g. 31.2–66% in bipolar disorder11,12,13,14, and 34–60% in depression12, 13, 15, but these rates are still much higher than in the general population. Smoking could lead to smoking-related medical conditions, increased risk of premature death and huge economic burden16, 17. Therefore, understanding smoking patterns in major psychiatric disorders is important to develop effective interventions for smoking cessation and reduction of harmful outcomes.
Patients with major psychiatric disorders are vulnerable to smoking but the vulnerability is also influenced by the sociocultural context18,19,20,21. For example, de Leon et al.4 found lower smoking rates in psychiatric patients than in the general population in Japan and Columbia. Thus, findings on smoking reported from Western settings may not be applicable to other cultural contexts. Further, only a few Western studies have directly compared smoking rates across different major psychiatric disorders3, 22.
China has a population of 1.4 billion and the 1-month prevalence of any psychiatric disorder was estimated to be 17·5%23. To the best of our knowledge, no previous study has compared the smoking rates directly between different major psychiatric disorders in China. This study examined the prevalence of smoking in patients with bipolar disorder, major depressive disorder (MDD) and schizophrenia, and explored the relationships between smoking and demographic and clinical characteristics, and quality of life (QOL) in a large representative sample. Based on previous findings3, 22, we expected that the prevalence of smoking would be highest in schizophrenia, followed by bipolar disorder and MDD. In addition, smoking rates in each of these disorders is expected to be higher than in the general population in China.
Methods
Participants and study site
The study, conducted from February to August 2013, was part of a larger research project that examined the quality of psychiatric service models24, 25 at the China’s National Clinical Research Center for Mental Disorders. This center has 800 acute psychiatric beds and receives more than 1,500 outpatient visits daily, and provides mental health services for over 20 million people in northern China. Patients who were admitted to the hospital during the study period were consecutively screened for eligibility based on the following study entry criteria: (1) diagnosis of schizophrenia or other psychotic disorders (schizophrenia thereafter), bipolar disorder or major depressive disorder (MDD) according to DSM-IV criteria; if there were multiple diagnoses, only the principal diagnosis was recorded; (2) age 18 years or older; (3) ability to understand the contents of the protocol; (4) willingness to provide written informed consent.
Instruments and evaluation
Demographic and clinical data were collected by a review of medical records using a standardized form designed for this study and confirmed with a clinical interview with the patient and family members if available.
Smoking-related variables in this study were defined as follows: lifetime smoking referred to smoking at least 1 cigarette daily for at least one month at some time in the past7, 26; and current smoking was defined as smoking at least 1 cigarette daily during the past month7 prior to the current admission. Age of smoking onset was also recorded. In the case of any discrepancy between patients and their families, a family meeting was conducted to reach a consensus.
The validated Chinese version of the Symptom Checklist-90 (SCL-90) was used to measure psychiatric symptoms; its 90 items covers nine areas: somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Each area is rated on a 5-point scale ranging from 0 (absence of the symptom) to 4 (maximum intensity score for the symptom)27. Only the total score was used in this study. QOL was assessed with the validated Chinese version of the Medical Outcomes Study Short Form-12 (SF-12)28, 29. This is a multidimensional generic instrument with 12 items covering physical and mental component scores. A higher score on SF-12 represents better QOL.
Two psychiatric nurses with over 5 years’ experience in clinical research interviewed patients within 48 hours after admission. The study protocol was approved by the Biomedical Ethics Board of Beijing Anding Hospital, China. The protocol including the methods was performed in accordance with the Declaration of Helsinki and the relevant ethical guidelines and regulations in China. Informed consents were obtained from all patients. No identifying information/images were involved in this study.
Statistical analysis
All data were analyzed using SPSS 21.0 for Windows. Basic socio-demographic and clinical characteristics between different diagnostic groups and between smokers and non-smokers were compared using independent sample t-test, Kruskal-Wallis H test, and chi-square test, as appropriate. QOL was compared between smokers and non-smokers in each diagnostic group with analysis of covariance (ANCOVA) after controlling for the potentially confounding effects of variables that were significantly different in univariate analyses. Multiple logistic regression with the “Enter” method was performed to compare the prevalence of smoking between the three diagnostic groups after controlling for variables that differed significantly in univariate analyses. Furthermore, the independent demographic and clinical correlates of smoking were examined using multiple logistic regression with the “Enter” method separately in each diagnostic group, with smoking as the dependent variable and the socio-demographic and clinical variables that were significantly different in univariate analyses as independent variables. As the smoking rate is significantly higher in male patients in China5, 6, the independent demographic and clinical correlates of smoking in male patients were examined using multiple logistic regression with the “Enter” method. The level of significance was set at 0.05 (two-tailed).
Results
Of the 1,475 patients admitted during the study period, 1,102 met the study criteria and participated in the study. The prevalence of lifetime smoking in the whole sample was 19.6%; 20.9% in bipolar disorder, 13.2% in MDD and 20.9% in schizophrenia, while the corresponding figures of current smoking were 16.7% (male: 38.4%; female: 4.3%), 17.5% (male: 41.2%; female: 6.3%), 10.6% (male: 30.4%; female: 2.3%) and 18.5% (male: 38.6%; female: 2.8%). The prevalence of current smoking was highest in the schizophrenia group, followed by the bipolar disorder and MDD groups. There was no significant difference between the three diagnostic groups in the proportion of patients starting smoking prior to the illness, daily amount of current smoking and age of smoking onset.
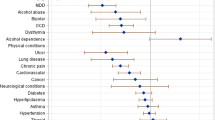
There were significant group differences in terms of age, male gender, education level, marital status, personal income, major medical conditions, family history of psychiatric disorders, age of onset, first episode of the illness, length of illness and number of admissions (Table 1). After controlling for the variates that significantly differed in univariate analyses, the prevalence of smoking in bipolar disorder (p = 0.004, OR = 2.5, 95%CI: 1.3–4.7) and schizophrenia (p = 0.03, OR = 2.0, 95%CI: 1.06–3.8) were significantly higher than in MDD, but no significant difference between bipolar disorder and schizophrenia groups was found (p = 0.33).
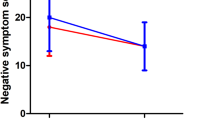
Table 2 compares demographic and clinical characteristics between smoking and non-smoking groups by diagnoses. In bipolar disorder, after controlling for male gender, living alone, personal income, having health insurance, age and age of onset, there was no significant difference between the smoking and non-smoking groups in physical (F(1,456) = 0.1, P = 0.67) and mental QOL (F(1, 456) = 0.002, P = 0.96). In MDD, after controlling for male gender, age and age of onset, there was no significant difference between the smoking and non-smoking groups in physical (F(1,184) = 0.3, P = 0.57) QOL, but smokers had a higher mental QOL than non-smokers (F(1,184) = 7.5, P = 0.007). In schizophrenia, after controlling for male gender, first episode, education level and the SCL-90 total score, there was no significant difference between the smoking and non-smoking groups in physical (F(1,400) = 1.6, P = 0.20) and mental QOL (F(1,400) = 0.001, P = 0.98).
Table 3 shows the demographic and clinical correlates independently associated with smoking by diagnoses. Smoking was independently associated with male gender and older age of onset in schizophrenia. Smoking was positively associated with male gender, living alone, higher personal income and health insurance, while negatively associated with first episode of illness and education level in bipolar disorder. Smoking was positively associated with male gender, but negatively associated with age of onset in MDD. In the pooled sample of male patients, smoking was positively associated with living alone and the number of admissions (Table 4).
Discussion
To our best knowledge, this was the first study that compared the prevalence of smoking between patients with schizophrenia, bipolar disorder and MDD in China. The prevalence of current smoking was 16.7% in the whole sample; 17.5% in bipolar disorder, 10.6% in MDD and 18.5% in schizophrenia. The prevalence in the whole sample was significantly lower than previous findings (61.3–73.5%) reported in both Chinese30,31,32,33 and Western psychiatric patient samples34, and even lower than the smoking rate (28.1%) in adult Chinese general population35. Lasser et al.7 reported that the prevalence of current smoking in persons with any lifetime psychiatric disorders was 34.8%, which is much higher than our results. Differences in types of psychiatric disorders, study settings, sample size, demographic and clinical characteristics, and sampling method may contribute to the discrepancy in the findings between studies. For example, there are usually smoking restrictions in inpatient settings19, which may contribute to the low smoking rate. Due to the gender differences, gender ratio of population samples is also a contributing factor to differences in smoking rate20. In contrast to the high ratio of males (93.8–100%) in previous studies30,31,32,33, male patients only accounted for 36.4% of the whole sample in this study.
There are several reasons for the association between severe psychiatric disorders and smoking. There is preliminary evidence that the variants in the 15q25 gene cluster may be a contributing factor to smoking in patients with schizophrenia and bipolar disorders31, 36. In addition, the abnormality of nicotine receptor (a7) may be another genetic factor making schizophrenia patients vulnerable to smoking37, 38. Furthermore, psychotic symptoms and antipsychotic-induced side effects could be mitigated through nicotinic receptors in the mesolimbic and nigrostriatal systems39, 40.
As expected, the prevalence of smoking was highest in schizophrenia, followed by bipolar disorder and MDD. However, considering that smoking rate is largely influenced by gender ratio20, we also examined the effect of gender in each diagnostic group. Surprisingly, smoking rate was highest in bipolar disorder (41.2%), followed by schizophrenia (38.6%) and MDD (30.4%) in males, with a similar pattern found in females: highest in bipolar disorder (6.3%), followed by schizophrenia (2.8%) and MDD (2.3%). This is inconsistent with previous Western findings that smoking is most common in schizophrenia3, 39, 41,42,43,44. In addition, smoking rates across each of the three disorders in this study were significantly lower than previous findings; e.g., Diaz et al.22 found smoking rate was 66%, 57% and 74% in patients with bipolar disorder, MDD and schizophrenia, respectively in a cohort of 424 psychiatric patients. Of note, the age of schizophrenia patients in our study was relatively young (34.5 years) and 19.8% had first-episode disorder. It is possible that local Chinese culture may have variable influence on smoking behavior in first-episode and chronic patients20, 45. In multivariate analyses no significant difference between bipolar disorder and schizophrenia in smoking rates was found, in line with the notion that both schizophrenia and bipolar disorder patients are vulnerable to tobacco use3, 4, 12, 46. Smoking rate was lowest in MDD in this study, which supports previous studies that found no strong cause-effect relationship between depression and smoking47,48,49.
Similar to previous studies14, 50, 51, male gender was a major risk factor for smoking in all diagnostic groups in this study. Further, smokers with bipolar disorder were more likely to have lower education and live alone compared to non-smokers, which is consistent with earlier findings20, 52. The cost of cigarette has been associated with smoking rate53. Patients with a higher income and health insurance coverage who could afford buying cigarettes were more likely to smoke. This may partly explain the higher rate of smoking in bipolar patients who had a relatively higher percentage of health insurance than the other two groups. As better education brings greater awareness of the harmful effects of smoking, patients with higher education are less likely to smoke26. In contrast, those living alone with poor family support may be more inclined to smoke as a behavioral filler54. Similar to other studies20, 55, older age of onset was positively associated with smoking in schizophrenia, but negatively associated with smoking in MDD in this study9, 56.
Demographic correlates of smoking were evident in patients with bipolar disorders. Patients living alone experience more negative feelings due to lack of family support, thus were more likely to smoke to relieve loneliness and perhaps boredom14, 54. Similar to previous findings14, smokers also had lower income. We have no explanation why smoking was associated with first episode illness, higher income and health insurance in this group only. These findings need to be confirmed in future studies.
More frequent admissions were positively associated with smoking in male patients. It is likely that patients with more frequent relapses and hospitalizations had more severe illness and higher antipsychotic dosages that are associated with increased rate of smoking. Despite the negative impact of smoking on health, patients with MDD who smoked had a higher QOL. Self-medication as a coping strategy may be a factor since smoking may alleviate cognitive deficits, lessen medication side effects, improve attention and concentration and relieve depressive and anxiety symptoms7, 57,58,59,60,61,62. All these aspects of smoking could improve QOL. However, other studies did not support the “self-medication” hypothesis8, 34, 63.
There are several limitations to this study. First, due to the cross-sectional study design, causality between smoking and other variables could not be determined. Second, some factors which influence smoking, such as lifestyle and social support, were not examined. Third, there is no substance dependence ward in this hospital, thus the association between comorbid substance dependence and smoking could not be examined. The study design focused only on the frequency of cigarettes use, and specific nicotine dependence was not examined. Fourth, smoking was self-reported, thus the possibility of recall bias cannot be excluded. Fifth, the study was only conducted in one large tertiary referral hospital hence the results cannot be generalized to other settings.
Conclusions
The prevalence of current smoking in patients with schizophrenia and bipolar disorders were significantly higher than in MDD in China. However, the figures for all three disorders were considerably lower than those reported in Western countries. The influence of psychopathological and socio-cultural factors on smoking warrants further investigations.
References
WHO. Tobacco. http://www.who.int/mediacentre/factsheets/fs339/en/ (2016).
de Leon, J., Tracy, J., McCann, E., McGrory, A. & Diaz, F. J. Schizophrenia and tobacco smoking: a replication study in another US psychiatric hospital. Schizophr. Res. 56, 55–65 (2002).
de Leon, J., Diaz, F. J., Rogers, T., Browne, D. & Dinsmore, L. Initiation of daily smoking and nicotine dependence in schizophrenia and mood disorders. Schizophr. Res. 56, 47–54 (2002).
de Leon, J. & Diaz, F. J. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr. Res. 76, 135–157 (2005).
Cao, X. L. et al. Current cigarette smoking in Chinese female patients with schizophrenia: A meta-analysis. Psychiatry Res. 235, 203–205, doi:10.1016/j.psychres.2015.11.050 (2016).
Li, Y. et al. Smoking in male patients with schizophrenia in China: A meta-analysis. Drug Alcohol Depend. 162, 146–153, doi:10.1016/j.drugalcdep.2016.02.040 (2016).
Lasser, K. et al. Smoking and mental illness: A population-based prevalence study. JAMA 284, 2606–2610 (2000).
Mendelsohn, C. Smoking and depression–a review. Aust. Fam. Physician 41, 304–307 (2012).
Holma, I. A., Holma, K. M., Melartin, T. K., Ketokivi, M. & Isometsa, E. T. Depression and smoking: a 5-year prospective study of patients with major depressive disorder. Depress. Anxiety 30, 580–588, doi:10.1002/da.22108 (2013).
Zhang, X., Chen, D., Xiu, M. & Kosten, T. Cigarette smoking in male patients with chronic schizophrenia in a chinese population: Prevalence and relationship to clinical phenotypes. International Journal of Neuropsychopharmacology 15, 140–141 (2012).
Dickerson, F. et al. Cigarette smoking among persons with schizophrenia or bipolar disorder in routine clinical settings, 1999-2011. Psychiatr. Serv. 64, 44–50, doi:10.1176/appi.ps.201200143 (2013).
Vanable, P. A., Carey, M. P., Carey, K. B. & Maisto, S. A. Smoking among psychiatric outpatients: relationship to substance use, diagnosis, and illness severity. Psychology of addictive behaviors: journal of the Society of Psychologists in Addictive Behaviors 17, 259–265, doi:10.1037/0893-164x.17.4.259 (2003).
Morris, C. D., Giese, A. A., Turnbull, J. J., Dickinson, M. & Johnson-Nagel, N. Predictors of tobacco use among persons with mental illnesses in a statewide population. Psychiatr. Serv. 57, 1035–1038, doi:10.1176/ps.2006.57.7.1035 (2006).
Waxmonsky, J. A. et al. Prevalence and correlates of tobacco use in bipolar disorder: data from the first 2000 participants in the Systematic Treatment Enhancement Program. Gen. Hosp. Psychiatry 27, 321–328, doi:10.1016/j.genhosppsych.2005.05.003 (2005).
Pratt, L. A. & Brody, D. J. Depression and smoking in the U.S. household population aged 20 and over, 2005–2008. NCHS Data Brief 1–8 (2010).
Irwin, K. E., Henderson, D. C., Knight, H. P. & Pirl, W. F. Cancer care for individuals with schizophrenia. Cancer 120, 323–334, doi:10.1002/cncr.28431 (2014).
Ruther, T. et al. EPA guidance on tobacco dependence and strategies for smoking cessation in people with mental illness. European psychiatry: the journal of the Association of European Psychiatrists 29, 65–82, doi:10.1016/j.eurpsy.2013.11.002 (2014).
Kelly, D. L. et al. Lack of beneficial galantamine effect for smoking behavior: a double-blind randomized trial in people with schizophrenia. Schizophr. Res. 103, 161–168 (2008).
Tang, Y. L., George, T. P., Mao, P. X., Cai, Z. J. & Chen, Q. Cigarette smoking in Chinese male inpatients with schizophrenia: a cross-sectional analysis. J. Psychiatr. Res. 41, 43–48 (2007).
Hou, Y. Z. et al. Cigarette smoking in community-dwelling patients with schizophrenia in China. J. Psychiatr. Res. 45, 1551–1556, doi:10.1016/j.jpsychires.2011.07.011 (2011).
Chen, D. C. et al. Association of smoking and psychiatric symptoms, clinical characteristics and cognitive function in first-episode schizophrenia inpatients. Chinese Mental Health J 23, 1–4 (in Chinese) (2009).
Diaz, F. J. et al. Tobacco smoking behaviors in bipolar disorder: a comparison of the general population, schizophrenia, and major depression. Bipolar disorders 11, 154–165 (2009).
Phillips, M. R. et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet 373, 2041–2053 (2009).
An, F. R. et al. Electroconvulsive therapy and its relationships with clinical characteristics and quality of life in Chinese psychiatric patients. Psychiatry Res. 246, 246–249, doi:10.1016/j.psychres.2016.09.046 (2016).
An, F. R. et al. Hyperprolactinemia, prolactin-related side effects and quality of life in Chinese psychiatric patients. Compr. Psychiatry 71, 71–76, doi:10.1016/j.comppsych.2016.08.009 (2016).
Ma, X. et al. Smoking and psychiatric disorders in the rural and urban regions of Beijing, China: a community-based survey. Drug Alcohol Depend. 100, 146–152 (2009).
Chen, S. L. & Li, L. J. Psychometric proporties of the SCL-90. Chin. J. Nerv. Ment. Dis 29, 327(in Chinese) (2003).
Jenkinson, C. & Layte, R. Development and testing of the UK SF-12 (short form health survey). J. Health Serv. Res. Policy 2, 14–18 (1997).
Zhang, S. et al. Reliability and validity of SF-12 among floating population (in Chinese). Chin. J. Public Health 27, 226–227 (2011).
Ruan, J. H., WANG, K. & PAN, K. P. Clinical investigation and analysis of smoking status of hospitalized psychiatric patients. Medical Journal of Chinese People’s Health 25, 17 + 27(in Chinese) (2013).
Li, X. J. Investigation and analysis of smoking status of hospitalized psychiatric patients. Medical Information 19, 694–695(in Chinese) (2006).
Pan, W. Y. et al. Investigation and analysis of smoking status of hospitalized psychiatric patients. Chinese Journal of Drug Abuse Prevention and Treatment, 31–32 (2000).
Chen, R. D., Luo, M., Chen, X. & Xiong, H. The outcome of investigation on smoking status of hospitalized psychiatric patients. Sichuan Mental Health 17, 225–227 (2004).
Ziedonis, D. et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco 10, 1691–1715, doi:10.1080/14622200802443569 (2008).
WHO. Global Adult Tobacco Survey (GATS) China 2010, Country Report. http://www.notc.org.cn/newjcpg/201304/W020121108628365808856.pdf (2015).
Jackson, K. J., Fanous, A. H., Chen, J., Kendler, K. S. & Chen, X. Variants in the 15q25 gene cluster are associated with risk for schizophrenia and bipolar disorder. Psychiatr. Genet. 23, 20–28, doi:10.1097/YPG.0b013e32835bd5f1 (2013).
Leonard, S. et al. Association of promoter variants in the alpha7 nicotinic acetylcholine receptor subunit gene with an inhibitory deficit found in schizophrenia. Arch. Gen. Psychiatry 59, 1085–1096 (2002).
Freedman, R. et al. Linkage of a neurophysiological deficit in schizophrenia to a chromosome 15 locus. Proc. Natl. Acad. Sci. USA 94, 587–592 (1997).
Lohr, J. B. & Flynn, K. Smoking and schizophrenia. Schizophr. Res. 8, 93–102 (1992).
Kumari, V. & Postma, P. Nicotine use in schizophrenia: the self medication hypotheses. Neurosci. Biobehav. Rev. 29, 1021–1034 (2005).
Hughes, J. R., Hatsukami, D. K., Mitchell, J. E. & Dahlgren, L. A. Prevalence of smoking among psychiatric outpatients. A. J. Psychiatry 143, 993–997 (1986).
de Leon, J. et al. Schizophrenia and smoking: an epidemiological survey in a state hospital. A. J. Psychiatry 152, 453–455 (1995).
Diwan, A., Castine, M., Pomerleau, C. S., Meador-Woodruff, J. H. & Dalack, G. W. Differential prevalence of cigarette smoking in patients with schizophrenic vs mood disorders. Schizophr. Res. 33, 113–118 (1998).
Jackson, J. G., Diaz, F. J., Lopez, L. & de Leon, J. A combined analysis of worldwide studies demonstrates an association between bipolar disorder and tobacco smoking behaviors in adults. Bipolar Disord 17, 575–597, doi:10.1111/bdi.12319 (2015).
Li, Y. et al. Smoking and its associations with sociodemographic and clinical characteristics and quality of life in patients with schizophrenia treated in primary care in China. Gen. Hosp. Psychiatry 38, 79–83, doi:10.1016/j.genhosppsych.2015.10.003 (2016).
Diaz, F. J., Velasquez, D. M., Susce, M. T. & de Leon, J. The association between schizophrenia and smoking: Unexplained by either the illness or the prodromal period. Schizophr. Res. 104, 214–219 (2008).
Kendler, K. S. et al. Smoking and major depression. A causal analysis. Arch. Gen. Psychiatry 50, 36–43 (1993).
Hitsman, B., Borrelli, B., McChargue, D. E., Spring, B. & Niaura, R. History of depression and smoking cessation outcome: a meta-analysis. J. Consult. Clin. Psychol. 71, 657–663 (2003).
Hitsman, B. et al. Past major depression and smoking cessation outcome: a systematic review and meta-analysis update. Addiction 108, 294–306, doi:10.1111/add.12009 (2013).
Escobedo, L. G., Anda, R. F., Smith, P. F., Remington, P. L. & Mast, E. E. Sociodemographic characteristics of cigarette smoking initiation in the United States. Implications for smoking prevention policy. JAMA 264, 1550–1555 (1990).
Tang, Y. L. et al. Gender differences in 542 Chinese inpatients with schizophrenia. Schizophr. Res. 97, 88–96 (2007).
Li, W. et al. Characterization of brain blood flow and the amplitude of low-frequency fluctuations in major depressive disorder: A multimodal meta-analysis. J. Affect. Disord. 210, 303–311, doi:10.1016/j.jad.2016.12.032 (2016).
Hyland, A. et al. Cigarette purchase patterns in four countries and the relationship with cessation: findings from the International Tobacco Control (ITC) Four Country Survey. Tob. Control 15(Suppl 3), iii59–64, doi:10.1136/tc.2005.012203 (2006).
Roick, C. et al. Health habits of patients with schizophrenia. Soc. Psychiatry Psychiatr. Epidemiol. 42, 268–276 (2007).
Zhang, X. Y. et al. Sex difference in the prevalence of smoking in Chinese schizophrenia. J. Psychiatr. Res. 44, 986–988, doi:10.1016/j.jpsychires.2010.02.015 (2010).
Khaled, S. M., Bulloch, A., Exner, D. V. & Patten, S. B. Cigarette smoking, stages of change, and major depression in the Canadian population. Can. J. Psychiatry. 54, 204–208, doi:10.1177/070674370905400309 (2009).
Gonzalez-Pinto, A. et al. Tobacco smoking and bipolar disorder. J. Clin. Psychiatry 59, 225–228 (1998).
Zammit, S. et al. Investigating the association between cigarette smoking and schizophrenia in a cohort study. A. J. Psychiatry 160, 2216–2221 (2003).
Pomerleau, O. F., Downey, K. K., Stelson, F. W. & Pomerleau, C. S. Cigarette smoking in adult patients diagnosed with attention deficit hyperactivity disorder. J. Subst. Abuse 7, 373–378 (1995).
John, U., Meyer, C., Rumpf, H. J. & Hapke, U. Smoking, nicotine dependence and psychiatric comorbidity–a population-based study including smoking cessation after three years. Drug Alcohol Depend. 76, 287–295 (2004).
Dalack, G. W., Healy, D. J. & Meador-Woodruff, J. H. Nicotine dependence in schizophrenia: clinical phenomena and laboratory findings. A. J. Psychiatry 155, 1490–1501 (1998).
Glassman, A. H., Covey, L. S., Stetner, F. & Rivelli, S. Smoking cessation and the course of major depression: a follow-up study. Lancet 357, 1929–1932 (2001).
Wu, L. T. & Anthony, J. C. Tobacco smoking and depressed mood in late childhood and early adolescence. Am. J. Public Health 89, 1837–1840 (1999).
Acknowledgements
The study was supported by the Capital City Clinical Practice and Research Funding of Beijing Municipal Science & Technology Commission (Z141107002514033; Z151100004015042), the Clinical Medicine Development Funding of Beijing Municipal Administration of Hospitals (ZYLX201403; ZYLX201607), Beijing Municipal Administration of Hospital’s Ascent Plan (DFL20151801) and the University of Macau (SRG2014-00019-FHS; MYRG2015-00230-FHS; MYRG2016-00005-FHS). The University of Macau had no role in the study design, generating or interpreting the results and publication of the study.
Author information
Authors and Affiliations
Contributions
Study Design: Yu-Tao Xiang. Data collection: Feng-Rong An, Ping-Ping Wu, Xin Jin. Analysis and interpretation of data: Xiao-Hong Li, Yu-Tao Xiang. Drafting of the manuscript: Xiao-Hong Li, Yu-Tao Xiang. Critical revision of the manuscript: Gabor S. Ungvari, Chee H. Ng, Helen F. K. Chiu. Approval of the final version for publication: All the authors.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, XH., An, FR., Ungvari, G.S. et al. Prevalence of smoking in patients with bipolar disorder, major depressive disorder and schizophrenia and their relationships with quality of life. Sci Rep 7, 8430 (2017). https://doi.org/10.1038/s41598-017-07928-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-07928-9
This article is cited by
-
Demographic, biochemical, clinical, and cognitive symptom differences between smokers and non-smokers in Chinese older male patients with chronic schizophrenia
European Archives of Psychiatry and Clinical Neuroscience (2024)
-
Health behaviours of patients with affective disorders: a cross-sectional study
BMC Psychiatry (2023)
-
Associations between adverse childhood experiences and overweight, obese, smoking and binge drinking among adult patients with depression in China
Current Psychology (2023)
-
The impact of pharmacological and non-pharmacological interventions on physical health outcomes in people with mood disorders across the lifespan: An umbrella review of the evidence from randomised controlled trials
Molecular Psychiatry (2023)
-
An observational study of system-level changes to improve the recording of very brief advice for smoking cessation in an inpatient mental health setting
BMC Public Health (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.