Abstract
Proximal femoral fractures are a major public health concern with estimated annual direct and social costs amounting to £2 billion and average 30-day mortality risk of 7.5%. In response to the recent debate over out-of-hours hospital provision we investigated the ‘weekend effect’ at a major trauma centre, caring for acute injuries. A single centre, multi-surgeon review of 2060 patients performed. The distribution of patient and treatment variables compared in patients admitted on a weekday or the weekend. Fewer patients met performance indicators during weekend admission, time to surgery (63 vs. 71%) and time to geriatric review (86 vs. 91%). Weekend admission 30-day mortality was marginally lower than weekday (9.7% vs. 10.2%, OR 0.94, 95% CI 0.67 to 1.32, p = 0.7383). Increasing age, female gender, co-morbidities and confusion increased mortality risk. Binary regression analysis including these variables found no significant ‘weekend effect’. Despite the unit observing an increasing workload in the last five years, with meticulous workforce planning, senior doctor provisions and careful use of resources, it is possible to provide a seven-day fracture neck of femur service with no variation in thirty-day mortality by the day of admission.
Similar content being viewed by others
Introduction
Proximal femoral fractures affect geriatric patients with multiple comorbidities and poor physiological reserve. This renders patients vulnerable and a third will die within the anniversary of their injury1. In 2014, the national hip fracture database reported an overall 30-day mortality (TDM) of 7.5% in England, Wales and Northern Ireland for patients with acute proximal femoral fracture (PFF)1. It is not uncommon for individual hospitals to report higher TDM in the region of 10 to 12%2. In other medical specialities, patients presenting with acute perforated appendix, bacteraemic community acquired pneumonia or ruptured abdominal aortic aneurysm, have TDM rates of 0.5%, 30% and 37% respectively3,4,5. There is also evidence to support inferior outcomes with weekend admission and surgery in these pathologies6. Freemantle et al. report a ‘weekend effect’ with higher relative risk of 30-day mortality (10 vs 15%)7. The findings of this study are widely debated, with newer evidence emerging to tackle criticisms of causality and staffing levels8, 9. Meacock et al. found no difference with emergency department admissions but did observe lower admission rates at the weekend and when subgrouping by diagnosis, higher weekend mortality was attributed to severity of illness10. There is evidence to suggest higher weekend mortality differentiated by diagnosis in emergency attendances and neonatal admissions11, 12.
Mortality risk is elevated for two decades following a PFF, predominantly from cardiovascular events or pneumonia13, 14. As our population ages PFF have become a public health concern with projected U.K. annual incidence of 101,000 in 2020 and yearly healthcare costs of £2 billion15. In recognition of treatment needs and frailty of patients we have seen the implementation of a national hip fracture registry, management guidelines and financial incentives for healthcare trusts that comply with efficiency targets16, 17. The policies have imparted an ethos of multi-disciplinary care, early surgery and targeted rehabilitation, with a notable reduction in TDM14. However, we do not know whether the day of admission influences patient outcomes and overall survival18, 19.
Proximal femoral fracture patients offer a valid and relevant population to evaluate the ‘weekend effect’, using short-term survival as proxy outcome to compare weekday and weekend service provision. In light of recent debate concerning out of hours’ emergency provision we investigate the mortality rates of patients admitted with acute PFF managed at a major trauma centre.
Methods
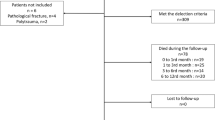
All patients with a newly diagnosed PFF were identified from a single institutions prospectively maintained database between 2010 and 2015. The study includes 2061 patients with acute fractures. For purpose of analysis the following data were extracted: patient’s age and sex; date of admission; fracture classification; co-morbidity; mental capacity; treatment modality; time to surgery and geriatric assessment; date of death if applicable.
Day of admission was calculated from the date and time of admission to the emergency department. Weekend was defined from midnight Friday to midnight Sunday. Fractures were classified by appearance on plain radiographs into extra or intracapsular20. The American Society of Anaesthesiologists (ASA) physical status classification system, routinely recorded for all patients undergoing operative treatment, was used as a surrogate measure of co-morbidities and anaesthetic risk. A ten-point abbreviated mental test (AMT) assessment was performed at the time of admission to assess cognitive function. Time of emergency department attendance defined the starting point for the continuous variables, time to surgery (hours) and geriatric assessment (hours). Pre-operative mobility was sub-classified into independent or use of one walking aid, use of two walking aids/frame or some indoor mobility but never goes outside without help and wheelchair bound or bed bound with no functional mobility. Patient’s outcome and mortality was verified by the office of national statistics to ensure all patients with TDM are identified irrespective of discharge destination or location at the time of death.
Our unit is a tertiary referral centre serving nearly 800,000 patients every year, for civilian patients with additional military provisions. The trust has a treatment pathway directing prompt haemodynamic resuscitation and analgesia, early clinical assessment and radiological diagnosis and definitive management within 36 hours of attendance. Patients are offered an ilio-fasical block in the emergency department following diagnostic radiographs.
Care is co-ordinated by trauma nurse practitioners who work every day, a trauma foundation one doctor, core surgical doctor, orthopaedic registrar and nominated consultant. Patients are admitted to a dedicated trauma ward for pre-operative optimisation, surgical and geriatric assessment. On weekdays, consultant led morning hip fracture operating lists run in addition to a designated trauma list. At weekends a consultant led two-session trauma list will prioritise hip fracture surgery providing there are no trauma patients requiring time critical intervention due to life or limb threatening injuries.
Ward patients are assessed daily by an orthopaedic registrar who leads a multidisciplinary team, including weekends. Ortho-geriatric services are provided by two consultants who review patients on weekdays. On the weekends attending medical registrars and consultant anaesthetists will review patients. Surgery is performed in line with national guidance preferring cemented modular stemmed hemiarthroplasty for intracapsular fractures, or total hip arthroplasty for patients fitting NICE criteria. We take a pragmatic approach to extracapsular fractures using dynamic hip screw fixation or cephalo-medullary devices in most cases. The ethos of our anaesthetic department is to augment general anaesthesia with a spinal or regional block, thus enhancing recovery and early mobilisation. Patients routinely have peri-operative antibiotics. Discharge destination post-surgery varies from rehabilitation wards within the trust, intermediate care centres to home with a safe package of care.
For the power analysis we identified a 3% increase in mortality risk to be significant using outlier evidence from the hip fracture registry1, 2. The parameters used were; dichotomous endpoint; two independent sample groups; alpha 0.05 and power of 80%. To detect a statistical difference we need to recruit 1745 weekday and 524 weekend admissions.
For analysis, we used IBM SPSS Statistics Version 20(Armonk, New York) software with a pre-determined significance level of 0.05. Continuous variables underwent tests for normality. A Shapiro-Wilkes test (p > 0.05), visual inspection of histograms and box plots showed that age was not normally distributed, with a skewness of −0.944 (SE 0.63) and kurtosis of 1.009 (SE 0.125) for patients who survived and a skewness of −0.667 (SE 0.187) and kurtosis of −0.761 (SE 0.371) for patients who died. Time to surgery and time to geriatric review also had skewed distributions.
In the first instance, we investigated the credibility of each candidate feature by performing univariate tests. A Chi-square test was used for categorical data. To compare median distributions we used Mann Witney U-tests with a predetermined significance level (p < 0.05). By accepting the null hypothesis (p > 0.05) we can assume no difference in distribution between the candidate feature and day of admission, Table 1. These variables were nominated to assess the effect on 30-day mortality risk (dependant variable), comparing the prevalence of factors (independent variables) in patients dying within thirty days to those surviving using a binomial logistic regression model. The model will assess the effect of changing weekday to weekend admission on 30-day mortality whilst keeping other candidate features constant and generate odd ratios.
Study approval was gained via the local institutional review board (University hospital Birmingham audit committee). Anonymised patient and treatment information from the trust’s neck of femur database was made available for a service evaluation study. The trusts audit policies were adhered to for this study and no patients were directly contacted.
Results
The study included 2061 patients with mean age of 82.4 years (S.D. 9.84) and 71% of female sex. On average, 412 patients were treated each year and we observed an average annual increase of 22 cases. The mean 30-day mortality was 10.1%, during 2013 we observed the lowest mortality risk where the hospital treated 426 patients with 46 deaths (7%).
A quarter of patients attended on the weekend (505). Table 1 describes the prevalence of variables and patient characteristics for patients admitted on a weekday or weekend. There was no significant difference in distribution of gender, age, anaesthetic risk and location of fracture relative to hip capsule, thus we can assume the two groups were comparable in these demographics.
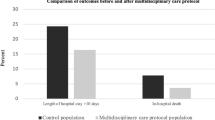
Over the entire study period weekend mortality was marginally lower than weekday (9.7% vs. 10.2%, OR 0.94, 95% CI 0.67 to 1.32 and P = 0.7383). The mean difference over five years was 0.3% (SD 1.7). Only in 2012 did weekend admission have a higher mortality risk, Fig. 1.
Over the study period the highest number of patients were admitted on a Monday (324 patients) whilst Saturday had the lowest attendance (226 patients, 10.18%). Figure 2 charts the mortality rates by day of admission, with range of 5% change in risk by day of admission (12.96 vs 8.06%).
The average time to surgery was longer at weekends (38.1 vs 34.8 hours) and only 63% met the 36-hour target for surgery compared to 71% on a weekday. There was no difference in mean time to geriatric assessment (44.6 vs 44.5 hours), however weekend admissions were less likely to adhere to the 72-hour target for review (90.9 vs 86.1%). Across the two groups AMT completion was comparable (76%). Uni-variate analysis of AMT suggested a higher risk of mortality with cognitive decline, AMT <7, OR 2.6 (1.82 to 3.71, p = 0.001).
Patients who mobilised with a wheelchair were twice as likely to die compared to those independently mobile or with aids, OR 2.036 (1.48 to 2.80, P = 0.001).
Multivariate analysis tests the effect of changing one independent variable, whilst keeping the other independent variables static, Table 2. In the final multivariate analysis 970 cases were included as patients with missing data were excluded. In the final data set weekend mortality was 7.5% (23 patients) compared to weekday 7.2% (60 patients), observing 83 deaths in total. Gender and ASA paralleled the original dataset. Age was similar, averaging 83 years and weekend admission had 4 hours delay in time to surgery and a two hour delay for geriatric reviews. The final test set matched the original data set well.
The output suggests that patients have a significantly greater risk of dying for a one-year increase in age, with a 5.7% increase in odds for every year. We categorised AMT and found that the odds ratio of dying within 30 days of injury is double with cognitive impairment when adjusted for other risk factors. Multivariate analysis suggested that being female (OR 1.76) and having pre-existing co-morbidities (OR 2.23) was associated with higher mortality risk. Increased time to surgery was significantly associated with raised mortality risk, although there was a trend for earlier geriatric assessment to be beneficial this was not significant.
Discussion
Out of hours emergency cover to admit acute proximal femoral fracture (PFF) patients is necessary twenty-four hours a day. Hospitals, knowing the frailty of these patients, prioritise early investigation and treatment. Our findings suggest that care for acute PFF is similar for patients admitted on a weekday and weekend. The study illustrates the successful implementation of consultant led multi-disciplinary treatment that neutralises any potential ‘weekend effect’. We also identified independent prognostic factors that correlate with short-term survival: increasing age; female gender; co-morbidities and cognitive decline. These can be used to risk assess patients on admission.
The crude mortality estimates over five years were comparable (9.7 vs 10.2). The small reduction in mortality when admitted at the weekend was not statistically significant and clinically this amounts to two fewer deaths a year. Larger studies across multiple sites would be required to provide a generalisable output. Our study lacked power with the final model only recruiting 970 patients. Hence the discriminatory power of the final model was average, with area under the curve (AUROC) of 0.737 (95% CI 0.682–0.792). However, relevant studies have similar accuracy when generating mortality predictors for PFF2. Looking at the binary regression output, the model generates two predicted deaths, whilst we observed 83 deaths in the final data set. This suggests there are influential factors not accounted for by the variables in this model and we are missing predictive ability.
There has been an expanse of evidence in 2016 across a range of specialities refuting the weekend effect. To date, evidence for PFF patients has found variability in mortality by day of admission, being higher on the weekend21,22,23. Thomas et al.21 attributes this to junior anaesthetic cover and no ortho-geriatrician provision on weekends. The study did not control for pre-morbid function or cognitive impairment, which have previously been reported as independent prognostic factors24. Research investigating hip fracture outcomes that omit independent variables, such as mobility assessment, are prone to confounding22. Being a major trauma centre we staff a dedicated weekday morning hip fracture theatre list supervised by consultants. The department has dedicated trauma nurses to coordinate care and we also prioritise neck of femur patients on weekend trauma lists. This minimises surgical delays and ensures perioperative multi-disciplinary care targets are met. In our study, on weekends, we observed a greater proportion of patients receiving dynamic hip screws for extra-capsular fractures which are considered a lesser surgical insult than cemented hemi-arthroplasty for intra-capsular fractures. We also noted more patients admitted on the weekend had total hip replacements, which are reserved for younger, active individuals according to NICE guidance in 2012.
The factors we found to be associated with poor outcomes in patients with acute PFF are similar to those reported in existing literature: increasing age; female gender; presence of co-morbidities increasing anaesthetic risk and cognitive impairment2, 25, 26. Altered biochemistry such as low albumin or low 25-hydroxyvitamin D are also poor prognostic indicators25. Impaired pre-operative mobility, diabetes and residing in social care also raises mortality risk27. Frost et al.2 found congestive cardiac and liver disease to moderate survival the most, RR of 3.02 and 4.75 respectively. For every 10 years increase in age, mortality risk doubled (RR 1.92)2. The Nottingham hip fracture score encompasses seven variables with the largest magnitude of effect on the outcome of interest, 30-day mortality28. Validation studies found a difference of 10.2% in TDM between low and high risk patients29. Future studies can use the scoring system to risk profile.
By adjusting for co-morbidities Grimes et al.30 failed to demonstrate a difference in mortality with delayed surgery (>96 hours)30. Moran et al.31 found no harmful effect when surgery was performed within 4 days. However, any delay secondary to medical co-morbidities elevated mortality risk (17% TDM risk, HR 2.3)31. One can conclude from previous studies that outcomes are linked to the overall health of individual patients. The presence of co-morbidities often correlates to age and cognitive function and requires optimisation from senior physicians, with potential to delay surgery. A comprehensive orthogeriatic service reduces mortality and length of stay32. Our results suggest that the TDM odds increase for every extra hour taken until the patient has surgery and decrease for every extra hour taken before a geriatric assessment is made. This proposes that patients with increased risk are identified and reviewed sooner by medical physicians and subsequently may have a delay to surgery in order to resuscitate physiological parameters.
We believe the “weekend effect” is complex and speciality dependant. Acute conditions requiring time critical diagnosis or intervention may be hampered by deficient resources and staffing at weekends18, 33. Generic studies may not account for the heterogeneity of emergency provisions across specialities and may explain the equipoise in evidence. Care pathways for PFF patients are not time critical34. Although a less fragile group, patients with biliary colic have many similarities to PFF patients. Early diagnosis and prompt biliary drainage improves outcomes, but these are not time critical. Other factors were found to have a greater impact on survival (development of cholangitis and dehydration), perhaps why the authors also failed to demonstrate a weekend effect35.
Our findings must be considered in light of the studies limitations as a retrospective observational study and the associated discrepancies with data collection, missing data and irregularities in documentation, despite meticulous effort to analyse reliable data fields with consistent definitions. Due to missing data fields the final statistical analysis comprised 970 cases, less than half of the original study sample and was underpowered. This has influenced the predictive ability and accuracy of our analysis. No attempt was made to synthesise missing data.
As described in the methodology, the studied population was treated at a major trauma centre with seven day working rotas, involving consultant led care in orthopaedics, anaesthesia and geriatrics. This may not be achievable in lesser hospital tiers and limits the generalisability of our conclusions. We also recognise the limitations of grading systems, such as ASA. The classification is known to have inter-observer variability. We used it as a proxy for co-morbidities as these were not reliably recorded on the hip fracture database. A prospective study would facilitate the capture of data such as co-morbidities, cardiovascular health and liver disease, reducing bias. We selected thirty-day mortality as it is reliably recorded as we do not routinely follow-up PFF patients, however it is an arbitrary time point and we cannot comment on the weekend effect on longer-term survival.
Conclusion
With an aging population and increasing prevalence of proximal femoral fractures, it is important that we allocate appropriate resource and staffing to accommodate needs. The unit investigated provides seven-day consultant led multi-disciplinary care for complex injuries involving frail and vulnerable elderly patients. The study failed to demonstrate a weekend effect. A larger multi-centre study is required to generate a generalisable outcome. We successfully identified independent prognostic factors that increase short-term mortality; Increasing age, female gender, higher ASA grade and cognitive decline. With meticulous service provision and robust care pathways we can provide effective seven-day care.
References
Johansen, A. National Hip Fracture Database (NHFD) An analysis of 30-day mortality in 2014. 1–15 (2016).
Frost, S. A., Nguyen, N. D., Black, D. A., Eisman, J. A. & Nguyen, T. V. Risk factors for in-hospital post-hip fracture mortality. Bone 49, 553–558, doi:10.1016/j.bone.2011.06.002 (2011).
Blomqvist, P. G., Andersson, R. E., Granath, F., Lambe, M. P. & Ekbom, A. R. Mortality after appendectomy in Sweden, 1987–1996. Annals of Surgery 233, 455–460, doi:10.1097/00000658-200104000-00001 (2001).
Melzer, M. & Welch, C. 30-day mortality in UK patients with bacteraemic community-acquired pneumonia. Infection 41, 1005–1011, doi:10.1007/s15010-013-0462-7 (2013).
Powell, J. T., Sweeting, M. J. & Thompson, M. M. Endovascular or open repair strategy for ruptured abdominal aortic aneurysm: 30 day outcomes from IMPROVE randomised trial. BMJ 348, f7661, doi:10.1136/bmj.f7661 (2014).
Al-Qurayshi, Z., Kadi, A., Srivastav, S. & Kandil, E. Risk and outcomes of 24-h delayed and weekend appendectomies. J. Surg. Res. 203(1), 246–252 (2016).
Freemantle, N. et al. Increased mortality associated with weekend hospital admission: a case for expanded seven day services? BMJ 351, h4596, doi:10.1136/bmj.h4596 (2015).
Godlee, F. What to do about the ‘weekend effect’. BMJ 351, h4840, doi:10.1136/bmj.h4840 (2015).
Aldridge, C. et al. Weekend specialist intensity and admission mortality in acute hospital trusts in England: a cross-sectional study. Lancet 0 (2016).
Meacock, R., Anselmi, L., Kristensen, S. R., Doran, T. & Sutton, M. Higher mortality rates amongst emergency patients admitted to hospital at weekends reflect a lower probability of admission. J Health Serv Res Policy 1355819616649630 doi:10.1177/1355819616649630 (2016).
Aylin, P., Yunus, A., Bottle, A., Majeed, A. & Bell, D. Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 19, 213–217, doi:10.1136/qshc.2008.028639 (2010).
Palmer, W. L., Bottle, A. & Aylin, P. Association between day of delivery and obstetric outcomes: observational study. BMJ 351, h5774, doi:10.1136/bmj.h5774 (2015).
Friesendorff, von M. et al. Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int 1–9, doi:10.1007/s00198-016-3616-5 (2016).
Chatterton, B. D., Moores, T. S., Ahmad, S., Cattell, A. & Roberts, P. J. Cause of death and factors associated with early in-hospital mortality after hip fracture. The Bone & Joint Journal 97-B, 246–251, doi:10.1302/0301-620X.97B2.35248 (2015).
NICE. National Costing Report Hip Fractures. nice.org.uk (2011).
British Orthopaedic Association. The Care of Patients with Fragility Fracture. http://www.fractures.com/pdf/BOA-BGS-Blue-Book.pdf (date last accessed 6th June 2016).
No authors listed. Payment by Results Guidance for 2011–12. http://webarchive.nationalarchives.gov.uk/20130507170152/https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/151911/dh_126157.pdf.pdf (date last accessed 6th June 2016).
Glance, L. G. et al. Outcomes are Worse in US Patients Undergoing Surgery on Weekends Compared With Weekdays. Med Care 54, 608–615, doi:10.1097/MLR.0000000000000532 (2016).
Hamada, T. et al. No weekend effect on outcomes of severe acute pancreatitis in Japan: data from the diagnosis procedure combination database. J. Gastroenterol., doi:10.1007/s00535-016-1179-z (2016).
Garden, R. S. Low-angle fixation in fractures of the femoral neck. Bone Joint J 43-B, 647–663 (1961).
Thomas, C. J., Smith, R. P., Uzoigwe, C. E. & Braybrooke, J. R. The weekend effect: short-term mortality following admission with a hip fracture. The Bone & Joint Journal 96-B, 373–378, doi:10.1302/0301-620X.96B3.33118 (2014).
Foss, N. B. & Kehlet, H. Short-term mortality in hip fracture patients admitted during weekends and holidays. Br. J. Anaesth. 96, 450–454, doi:10.1093/bja/ael012 (2006).
Kristiansen, N. S., Kristensen, P. K., Nørgård, B. M., Mainz, J. & Johnsen, S. P. Off-hours admission and quality of hip fracture care: a nationwide cohort study of performance measures and 30-day mortality. Int J Qual Health Care, doi:10.1093/intqhc/mzw037 (2016).
Seitz, D. P. et al. Effects of impairment in activities of daily living on predicting mortality following hip fracture surgery in studies using administrative healthcare databases. BMC Geriatr 14, 9, doi:10.1186/1471-2318-14-9 (2014).
Pioli, G. et al. Modifiable and non-modifiable risk factors affecting walking recovery after hip fracture. - PubMed - NCBI. Osteoporos Int, doi:10.1007/s00198-016-3485-y (2016).
Pioli, G. et al. Predictors of mortality after hip fracture: results from 1-year follow-up. Aging Clin Exp Res 18, 381–387, doi:10.1007/BF03324834 (2006).
Hu, F., Jiang, C., Shen, J., Tang, P. & Wang, Y. Preoperative predictors for mortality following hip fracture surgery: A systematic review and meta-analysis. Injury 43, 676–685, doi:10.1016/j.injury.2011.05.017 (2012).
Maxwell, M. J., Moran, C. G. & Moppett, I. K. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br. J. Anaesth. 101, 511–517, doi:10.1093/bja/aen236 (2008).
Wiles, M. D., Moran, C. G., Sahota, O. & Moppett, I. K. Nottingham Hip Fracture Score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br. J. Anaesth. 106, 501–504, doi:10.1093/bja/aeq405 (2011).
Grimes, J. P., Gregory, P. M., Noveck, H., Butler, M. S. & Carson, J. L. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am. J. Med. 112, 702–709, doi:10.1016/S0002-9343(02)01119-1 (2002).
Moran, C. G., Wenn, R. T., Sikand, M. & Taylor, A. M. Early Mortality After Hip Fracture: Is Delay Before Surgery Important? 87, 483–489 (2005).
Henderson, C. Y. et al. Dedicated orthogeriatric service reduces hip fracture mortality. Ir J Med Sci 1–6, doi:10.1007/s11845-016-1453-3 (2016).
Deshmukh, H., Hinkley, M., Dulhanty, L., Patel, H. C. & Galea, J. P. Effect of weekend admission on in-hospital mortality and functional outcomes for patients with acute subarachnoid haemorrhage (SAH). Acta Neurochir (Wien) 158, 829–835, doi:10.1007/s00701-016-2746-z (2016).
Novack, V., Jotkowitz, A., Etzion, O. & Porath, A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. International Journal for Quality in Health Care 19, 170–176, doi:10.1093/intqhc/mzm003 (2007).
Inamdar, S., Sejpal, D. V., Ullah, M. & Trindade, A. J. Weekend vs. Weekday Admissions for Cholangitis Requiring an ERCP: Comparison of Outcomes in a National Cohort. Am. J. Gastroenterol. 111, 405–410, doi:10.1038/ajg.2015.425 (2016).
Author information
Authors and Affiliations
Contributions
Rajpal Nandra was involved in study design, data collection, analysis and manuscript preparation. Jack Pullen was involved with study design, data collection and analysis. Jon Bishop provided statistical input, interpreting findings and performing data analysis. Khalid Baloch was involved in the treatment of patients, study design, interpretation of findings and proof on final manuscript. Liam Grover was involved with study design, interpretation of findings and proof of manuscript. Keith Porter is head of department and helped form the service provided. He contributed to interpretation of findings, manuscript preparation and proof of manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nandra, R., Pullan, J., Bishop, J. et al. Comparing mortality risk of patients with acute hip fractures admitted to a major trauma centre on a weekday or weekend. Sci Rep 7, 1233 (2017). https://doi.org/10.1038/s41598-017-01308-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01308-z
This article is cited by
-
Frailty and comorbidity predict 30 day postoperative outcomes, independent of anatomical site of fracture
Archives of Orthopaedic and Trauma Surgery (2023)
-
Hip fracture patients admitted to hospital on weekends are not at increased risk of 30-day mortality as compared with weekdays
Journal of Orthopaedics and Traumatology (2020)
-
Weekend effect on mortality by medical specialty in six secondary hospitals in the Helsinki metropolitan area over a 14-year period
BMC Health Services Research (2020)
-
Weekend admissions and mortality for major acute disorders across England and Wales: record linkage cohort studies
BMC Health Services Research (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.