Abstract
Although it is believed that implementation of the functional generated path (FGP) technique can facilitate occlusal surface design for restorations, it has not been objectively compared in situ with the conventional fabrication yet. Therefore, in the present study, a single-blind crossover clinical trial was conducted using T-scan to compare changes in occlusion time (OT) and disocclusion time (DT) of single posterior artificial crowns designed differently using FGP technique (FGP), average-value FGP technique (AVR) and conventional fabrication (CON). Each of the 10 participants took part in the study tried three artificial crowns in different sequences according to a computer generated randomization list. The results objectively revealed that changes in OT and DT were significantly smaller for FGP than CON (P < 0.05) and considerably smaller for AVR than CON, respectively. The subjective feedback and the occlusal adjusting time were better and shorter for FGP and AVR than CON (P < 0.05). No harm to the participants occurred. Overall, FGP is an efficient technique showing more physiological harmonious relationship with the articulating system.
Similar content being viewed by others
Introduction
Occlusion and occlusal surface are important subjects in daily dental practice1. When performing single crown restoration in patients, it is important that the crown contributes to harmonious function2, 3. Traditionally, crown occlusal surface is designed based on static relationship4. However, when patient’s dynamic occlusion was introduced on try-in visit, occlusal interference usually occurs5,6,7. To solve the problem, using articulator for accurate measurement and registration of jaw movements and temporomandibular joint (TMJ) parameters is essential. Nonetheless, the procedure could be time-consuming. Besides, how much individual registration is actually needed in order to keep occlusal interference within acceptable tolerance limits is still under debate8, 9.
Undoubtedly, the most accurate articulator is the patient him/herself. Meyer et al. first proposed the concept of functional generated path (FGP) in 1959 by recording the occlusal path of the teeth during movement directly in the patient’s mouth10. Thereafter, different materials and methods had been applied in FGP fixed prosthodontics5, 6, 11,12,13,14,15,16,17,18,19. Some researchers even tried to integrate the concept into CAD/CAM manufacturing5,6,7, 12,13,14,15,16,17,18. For single unit crowns, Mehl3 reviewed several related studies and deduced that FGP could be simulated by average-setting articulator in most cases, saving a great deal of time and devices in crown fabrication.
Numerous reports have illustrated that FGP has drawn more and more attentions and is useful for fixed prosthodontics. However, very few reports compared FGP technique and conventional fabrication6, 11, and none of them was an objective comparison in situ. T-scan system is among one of the most frequently used computerized analyzing systems to objectively assess occlusal equilibration20,21,22,23,24. The system records relative force values and objectively quantifies occlusal balance by displaying numerical values for occlusion and disocclusion times. Occlusion time (OT) is defined as the time from the first contact of occluding teeth to maximum intercuspation, whereas disocclusion time (DT) is defined as the time from maximum intercuspation to complete disocclusion during lateral movement25, 26. OT and DT are helpful in occlusal adjustment and linking the occlusion with other elements of the articulatory system21, 22, 27.
The purpose of this study was to compare OT and DT changes of the crown designed using FGP and conventional fabrication. Our null hypothesis was there were no significant differences between OT and DT of the crown designed using FGP technique and those using conventional fabrication.
Materials and Methods
A single-blind crossover clinical trial was adopted. The evaluation was carried out among single crowns designed differently using FGP technique (FGP), average-value FGP technique (AVR) and conventional fabrication (CON) in a sequence determined by a computer-generated list of random numbers. The study sample included 10 participants (5 men and 5 women, aged from 19 to 65 years old, with an average of 44.2 years old) selected from the Department of Prosthodontics at Stomatological Hospital of Fourth Military Medical University from December 2015 to March 2016. Power analysis was conducted using software G*Power, v. 3.1.9.2 (University of Kiel). Use of an alpha value of 0.05, a sample size of 10 was found to yield a power of 0.8. All participants were given detailed information about the study and singed written informed consent. The study protocol was reviewed and approved by the Institutional Review Board of Stomatological Hospital of Fourth Military Medical University (approval number: IRB-REV-2015039; Supplementary Fig. 1). It was further registered under protocol ID ClinicalTrials.gov NCT02609178 (date of registration:05/11/2015) according to the CONSORT 2010 statement. The methods employed were performed in accordance with the approved guidelines.
All participants had Angle class I jaw relationship with a single tooth needs crown restoration in the posterior quadrant (3 premolars and 7 molars). The tooth’s antagonist was purely natural or had received minimum restorations that would not significantly change the occlusal morphology. In other words, the antagonist could have received restorations on the surfaces other than the occlusal surface. If the restorations were on the occlusal surface, they should not cover the cusps28, 29. Exclusion criteria were the presence of missing tooth, moderate or severe periodontitis, temporomandibular joint disease, parafunctional movements or orthodontic treatment history.
All the teeth were prepared by 1 of 3 experienced practitioners (S.J.Z, F.W and L.L) under standard recommended preparation guidelines of 1.5 to 2.0 mm occlusal reduction, and 1.0 to 1.5 mm axial reduction with a deep chamfer margin circumferentially. Margin placement was designated at no more than 0.5 mm subgingivally. The impressions were made of A-silicones using two-phase impression technique (Silagum, DMG, Germany). The interim of the prepared teeth was fabricated in the laboratory using CAD/CAM (Dental system, 3Shape, Denmark; D710, Wieland, Germany) with 1 mm occlusal clearance. Participants were recalled for the first visit to perform general FGP technique. Light-cured resin (Clip F, VOCO, Germany) was applied onto the occlusal surface until the interim was properly fit with 1 mm occlusal clearance. Afterwards, the participants were instructed to close in maximum intercuspation position and then to perform right lateral, left lateral and protrusive movements in succession ending at maximum intercuspation position. After excess resin was trimmed off, the resin was fully polymerized under the manufacturer's instruction. The ICP contacts were marked using a 40 μm articulating paper (Arti-Check BK09, Bausch, Germany). Then a 12 μm shimstock (Arti-Fol BK31, Bausch, Germany) was used while instructing the participants to perform the eccentric movements. All eccentric interferences were eliminated and care was taken not to grind the ICP contacts registered in blue. The interim was then sent back to the laboratory to make the final restoration by duplicating its occlusal scheme (marked as FGP) (Dental System, 3Shape, Denmark; D710, Wieland, Germany). Meanwhile, two more final restorations of the same prepared tooth were made using average-value FGP technique (marked as AVR) and conventional fabrication (marked as CON), respectively (Dental system, 3Shape, Denmark; D710, Wieland, Germany). AVR was designed with the help of the virtual articulator to set the average values, as Mehl5 described. The average values adopted in the study were 30° for the angles of the sagittal condyle, 15° for the lateral Bennett angle, and 30° for the incisal path, respectively6. CON was designed purely from the technician’s experience. To avoid error, all the zirconia crowns were designed by the same technician and fabricated in fully anatomical form using Upcera blocks (Upcera, Upcera Dental, China) without using veneering porcelain (Fig. 1).
Example of the crowns designed differently in the study. (a) The ceramic crown designed by FGP technique (FGP). The crown was a copy of the interim made in the participant’s mouth by the FGP technique. (b) The ceramic crown designed with the average-value virtual articulator (AVR). (c) The ceramic crown designed by conventional fabrication (CON), which was fabricated by the technician from his own experience in the CAD/CAM software.
Each participant’s 3 crowns were packed separately with notes illustrating their try-in order following simple randomization procedures (computerized random numbers) in advance. On the try-in visit, each participant tried in the three crowns in corresponding order. First, OT and DT were recorded before try-in of any crowns as the baseline. Then the same participant started to try in each of the 3 crowns, and OT and DT were recorded again when the crown was seated before occlusal adjustments. The participant was at the same time inquired to grade their feeling towards the occlusal interference of the crown using Likert’s 3-point scale11 (Table 1). Adjustments were done by the same clinician (P. T. L) to remove premature occlusal contacts and occlusal interference, and the adjusting time for occlusal surface was recorded. A 5-minute interval was given to each participant between try-in of each crown. At last, the best fitting crown was chosen by the participant and cemented using glass ionomer cement (Fuji 1, GC, Japan).
In the study, OT and DT examinations were carried out using T-scan system (T-scan III, Teckscan, USA) by the same examiner (P. T. L). The size of the 100-μm-thick sensor (large or small) was chosen to suit the participant’s dental arch. Prior to any occlusal data acquisition, a proper sensitivity range was established25, 30 according to the manufacturer’s recommendation, and the sensor conditioning procedures of 2 to 4 test closures27, 31 were performed for each participant.
For all scanning procedures, participants were asked to sit in a relaxed upright position in the dental chair. The sensor was held consistently at the same position with respect to the teeth and aligned parallel to the occlusal plane and centered on the midline between the central incisors31. The same sensor was used for each participant throughout the try-in visit.
When recording OT and DT, participants were asked to 1) occlude on the sensor in centric occlusion with normal pressure until maximum intercuspation, 2) hold their teeth together for a period of 1 to 3 seconds, 3) start a protrusion from that completely intercuspated position, and 4) disocclude31. This procedure was repeated 3 times. Changes in OT and DT (ΔOT and ΔDT) were calculated by the following formulas:
The mean OT, DT, ΔOT and ΔDT of all the participants were calculated and statistically analyzed using SPSS 19.0 for Windows. All data were expressed as mean ± standard deviation. ΔOT and ΔDT were first tested by the Kolmogorov-Smirnov test of normality and then by the test for the homogeneity of variance. The results showed most of the data were normally distributed, thus one-way ANOVA (α = 0.05) was conducted to compared ΔOT and ΔDT among the 3 different crown designs – FGP, AVR and CON. The Kruskal-Wallis test (α = 0.05) was used to compare Likert’s 3-point scale and adjusting time among the 3 different crown designs.
Results
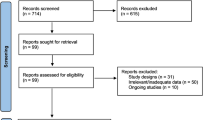
A CONSORT flow diagram illustrating subject flow during the clinical trial is presented in Fig. 2. All the experimental teeth had received root canal treatment before preparation. At last, 9 participants chose to take FGP and the other one chose AVR. No adverse events were reported. OT was 0.47 ± 0.57 s, 0.52 ± 0.58 s, 0.58 ± 0.55 s and 0.67 ± 0.56 s for baseline, FGP, AVR and CON, respectively, and DT was 0.89 ± 1.30 s, 0.98 ± 1.11 s, 1.38 ± 1.82 s and 1.91 ± 1.79 s for baseline, FGP, AVR and CON, respectively. Changes in OT were calculated as 0.07 ± 0.09 s, 0.13 ± 0.06 s and 0.22 ± 0.10 s for FGP, AVR and CON, respectively, and changes in DT were 0.09 ± 0.51 s, 0.49 ± 0.58 s and 1.02 ± 0.69 s for FGP, AVR and CON, respectively. Statistical analysis revealed significant smaller changes in OT and DT in FGP than in CON (P = 0.002 for OT; P = 0.005 for DT). Although AVR showed smaller OT and DT changes than CON, the difference was not statistically significant (Fig. 3). In addition, the average time needed for adjustment was 5.4 ± 3.8 min, 6.1 ± 4.8 min and 12.6 ± 5.3 min for FGP, AVR and CON, respectively. From the participants’ perspective, a significant better feedback was received from both FGP (P = 0.001) and AVR (P = 0.002) in try-in procedure (Fig. 4a). Statistical analysis showed both FGP (P = 0.01) and AVR (P = 0.029) crowns could significantly save time in occlusal adjustment, compared with CON (Fig. 4b).
T-scan measurements of the study. (a–d) Example of the 2-D and 3-D results of the T-scan measurement. The movie was advanced to the MA frame in which maximum intercuspation occurred. (a) The baseline image. (b) Try-in of FGP. The force loaded on tooth 26 at baseline distributed equally on tooth 26 and 27 while maintaining almost the same occlusal balance to the baseline. (c) Try-in of AVR. Tooth 27 shared part of the force loaded on tooth 26 at baseline. Occlusal balance was maintained. (d) Try-in of CON. Occlusal balance was broke. Force concentration area was detected on tooth 27. (e) Result of the difference among FGP, AVR and CON in ∆OT. Significant smaller changes were observed between FGP and CON. (f) Result of the difference among FGP, AVR and CON in ∆DT. Significant smaller changes were observed between FGP and CON.
Discussion
Concept of FGP has long been adopted in fixed prosthodontic practice. In traditional lost-wax technique, FGP could be employed with double-casting technique. Previous studies have confirmed the efficiency and a better patients’ satisfaction of double-casted FGP crown in adjusting occlusal surface11. In the digital process, FGP has been integrated into the workflow of virtual articulator with the help of individual registrations of centric and eccentric jaw position12,13,14,15,16,17,18. Some researchers even developed scanning devices to aid in recording the occlusal movement path directly in patients’ mouth6, 7. However, these devices still need time to popularize. A simulation study on dental models compared the morphological difference of crowns designed using FGP, AVR and CON and found that crowns prepared using FGP and AVR had more stabilized occlusion than those prepared using CON6. However, no clinical study compared objectively between FGP technique and conventional fabrication in situ so far.
Occlusion is hard to be evaluated due to lack of available gold standard. For simple restorations such as single unit crown, a successful occlusal surface design should not significantly change the patients’ occlusion32. Stated by the guidance for occlusal adjustment of simple restoration, occlusal adjustment should apply to rectify the contact points of the adjacent teeth back to the state when no crown has been worn32, 33.
However, conventional ways of assessing occlusal contacts encounter their own limits in practical application. Although articulating paper has been most commonly used, its marks would be affected by its width, and the salivary impregnation can diffuse the paper ink, leading to false positives34,35,36. Transillumination of silicon bite registration can overcome the problems of articulating paper, but the result depends much on the orientation of the light resource and would be affected by the filler in the bite registration material37, 38.
The T-scan was adopted in the present study to detect occlusal contacts because it could not only locate premature contacts and occlusal interference more clearly31, 39, but also relate occlusion to other elements of articulatory system simply through OT and DT. OT is directly related with patients’ occlusal contact pattern21 and has been considered as a capable description of occlusion22, 40, whereas, DT could relate tooth contacts to muscle activity26. Abnormalities in DT would result in change of muscle activity, thus facilitating the occurrence of TMD23. According to the manufacturer, OT is recommended as less than 0.2 s, and DT less than 0.4 s25, 26. However, in a survey conducted by Haralur et al.20, the average OT and DT in normal dentate subjects with healthy TMJs were 0.69 s and 0.79 s respectively. Another survey performed by Ma et al.41 in Chinese population with Angle class I relationship and healthy TMJs showed an average of 0.34 s for OT and 1.00 s for DT. Also, in the present study, the average OT and DT at baseline were 0.47 s and 0.89 s, respectively, which were between the results obtained by Haralur et al. and Ma et al., but still much longer than the recommended values. These discrepancies may be probably explained by individual difference. Therefore, in the study we calculated ΔOT and ΔDT as the main indexes. On the other hand, among other 3 pairs of OT and DT recorded before adjustments were made, the average OT values of all groups fell within the range between Haralur et al. and Ma et al., but only the average DT values of FGP group fell within the range between Haralur et al. and Ma et al. The phenomenon indicated that more physiologic harmonious function might be achieved by FGP than other two kinds of crowns. The results of ΔOT and ΔDT rejected the null hypothesis and revealed that ΔOT and ΔDT were significantly smaller in FGP than CON, but the difference between AVR and CON was not significant. Moreover, the results of subjective evaluation of patients’ feedback and adjusting time exhibited more comfortable feeling and less chair-side time in FGP and AVR, compared with CON, which was consistent with the result of a previous study carried out by Memon11. Moreover, in another study performed by Olthoff et al.6, larger interocclusal distance was found in FGP and AVR than CON. These results similarly indicated easier occlusal adjustment of FGP and AVR.
To ensure valid and reliable results, several measures were considered. First, the present study was designed as a crossover clinical trial to exclude individual variations and 5-minute washout time was provided to eliminate the effect between each crown. Second, the occlusal adjustment and the recording of T-scan were carried out by the same examiner (P. T. L) to exclude interexaminer variations because no study has investigated the influence of operator on the values recorded by T-scan42. Furthermore, considering an increasingly significant relationship was reported between the sagittal plan head-neck posture and initial occlusal contacts for patients over the age of 3043, all the occlusal adjustment procedures were done with participants sitting in a relaxed upright position. As instructed by the manufacturer, the sensors of T-scan can be used up to 15 to 25 times44. Therefore, for each participant, the same sensor was used throughout the try-in visit to exclude intersensor variability.
The authors acknowledged that the present study did not cover all cohorts who needed single unit crown restoration. Although FGP technique generally showed good results, FGP crowns were not easy to fabricate and needed to be further examined in more follow-ups. Therefore, it is necessary to further simplify the technique.
Conclusions
Within the limitations of the present study, FGP single crown showed significantly smaller changes in OT and DT than those from conventional single crowns, thus significantly improving patients’ satisfaction and reducing time for adjusting occlusion.
References
Zarb, G. The interface of occlusion revisited. The International journal of prosthodontics 18, 270–271 (2005).
Bryant, S. R. The rationale for management of morphologic variations and nonphysiologic occlusion in the young dentition. The International journal of prosthodontics 18, 284–287 (2005).
Mehl, A., Blanz, V. & Hickel, R. Biogeneric tooth: a new mathematical representation for tooth morphology in lower first molars. European journal of oral sciences 113, 333–340, doi:10.1111/j.1600-0722.2005.00224.x (2005).
Paulus, D., Wolf, M., Meller, S. & Niemann, H. Three-dimensional computer vision for tooth restoration. Medical image analysis 3, 1–19 (1999).
Mehl, A. A new concept for the integration of dynamic occlusion in the digital construction process. International journal of computerized dentistry 15, 109–123 (2012).
Olthoff, L. W., Van Der Zel, J. M., De Ruiter, W. J., Vlaar, S. T. & Bosman, F. Computer modeling of occlusal surfaces of posterior teeth with the CICERO CAD/CAM system. The Journal of prosthetic dentistry 84, 154–162 (2000).
Fang, J.-J. & Kuo, T.-H. Tracked motion-based dental occlusion surface estimation for crown restoration. Computer-Aided Design 41, 315–323, doi:10.1016/j.cad.2008.10.006 (2009).
Bowley, J. F., Michaels, G. C., Lai, T. W. & Lin, P. P. Reliability of a facebow transfer procedure. The Journal of prosthetic dentistry 67, 491–498 (1992).
Proschel, P. A., Maul, T. & Morneburg, T. Predicted incidence of excursive occlusal errors in common modes of articulator adjustment. The International journal of prosthodontics 13, 303–310 (2000).
Meyer, F. S. The generated path technique in reconstruction dentistry: Part II. Fixed partial dentures. The Journal of prosthetic dentistry 9, 432–440, doi:10.1016/0022-3913(59)90075-7 (1959).
Memon, S. A Comparative Evaluation of the Effect of Double Casting Technique Using Functionally Generated Path and Conventional Single Casting with Respect to Functional Articulation, Patient Satisfaction and Chair Side Time, in Single Unit Molar Teeth: An In Vivo Study. J Indian Prosthodont Soc 14, 119–125, doi:10.1007/s13191-014-0379-6 (2014).
Sohmura, T. & Takahashi, J. CAD/CAM system to fabricate dental prostheses-CAD for bridge restoration. Dental materials journal 16, 10–20 (1997).
Curtis, S. R. Functionally generated paths for ceramometal restorations. The Journal of prosthetic dentistry 81, 33–36 (1999).
Sohmura, T. & Takahashi, J. Improvement of CAD to produce crown by considering occlusion. Dental materials journal 12, 190–195 (1993).
Kimura, H., Sohmura, T. & Takahashi, J. Three dimensional shape measurement of teeth (2). CAD to produce crown considering occlusion. Dental materials journal 11, 38–44 (1992).
Rohrle, O., Waddell, J. N., Foster, K. D., Saini, H. & Pullan, A. J. Using a motion-capture system to record dynamic articulation for application in CAD/CAM software. Journal of prosthodontics: official journal of the American College of Prosthodontists 18, 703–710, doi:10.1111/j.1532-849X.2009.00510.x (2009).
Zou, B., Lu, P. J., Ye, S. Y. & Wang, Y. [Application of functionally generated path technique in computer-aided-design modeling of occlusal surface of full crown]. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi = Chinese journal of stomatology 41, 631–633 (2006).
Zou, B., Pei-Jun, L. U. & Wang, Y. Preliminary Study on Computer-Aided Design of Full Crown. Journal of Sun Yat-sen University (Medical Sciences) (2005).
DuVall, N. B. & Rogers, P. M. Application of the functionally generated path technique to restore mandibular molars in bilateral group function occlusion. Journal of prosthodontics: official journal of the American College of Prosthodontists 22, 226–232, doi:10.1111/j.1532-849X.2012.00944.x (2013).
Haralur, S. B. Digital Evaluation of Functional Occlusion Parameters and their Association with Temporomandibular Disorders. Journal of clinical and diagnostic research: JCDR 7, 1772–1775, doi:10.7860/JCDR/2013/5602.3307 (2013).
Wang, C. & Yin, X. Occlusal risk factors associated with temporomandibular disorders in young adults with normal occlusions. Oral surgery, oral medicine, oral pathology and oral radiology 114, 419–423, doi:10.1016/j.oooo.2011.10.039 (2012).
Baldini, A., Nota, A. & Cozza, P. The association between Occlusion Time and Temporomandibular Disorders. Journal of electromyography and kinesiology: official journal of the International Society of Electrophysiological Kinesiology 25, 151–154, doi:10.1016/j.jelekin.2014.08.007 (2015).
Thumati, P., Manwani, R. & Mahantshetty, M. The effect of reduced disclusion time in the treatment of myofascial pain dysfunction syndrome using immediate complete anterior guidance development protocol monitored by digital analysis of occlusion. Cranio: the journal of craniomandibular practice 32, 289–299, doi:10.1179/2151090314Y.0000000004 (2014).
Asazuma, Y., Isogai, Y., Watanabe, K. & Hara, K. Changes in gnathosonic and tooth contact characteristics induced by experimental occlusal interferences created using a full-cast double crown. Journal of oral rehabilitation 22, 203–211 (1995).
Kerstein, R. B. Obtaining measurable bilateral simultaneous occlusal contacts with computer-analyzed and guided occlusal adjustments. Quintessence international 32, 7–18 (2001).
Kerstein, R. B. & Wright, N. R. Electromyographic and computer analyses of patients suffering from chronic myofascial pain-dysfunction syndrome: before and after treatment with immediate complete anterior guidance development. The Journal of prosthetic dentistry 66, 677–686 (1991).
Kerstein, R. B. & Radke, J. The effect of disclusion time reduction on maximal clench muscle activity levels. Cranio: the journal of craniomandibular practice 24, 156–165, doi:10.1179/crn.2006.026 (2006).
Al-Omiri, M. K. et al. Quantification of tooth wear: conventional vs new method using toolmakers microscope and a three-dimensional measuring technique. Journal of dentistry 38, 560–568, doi:10.1016/j.jdent.2010.03.016 (2010).
Al-Hiyasat, A. S. & Abu-Alhaija, E. S. J. The relationship between static and dynamic occlusion in 14–17-year-old school children. Journal of Oral Rehabilitation 31, 628–633 (2004).
Kerstein, R. B. Combining technologies: a computerized occlusal analysis system synchronized with a computerized electromyography system. Cranio: the journal of craniomandibular practice 22, 96–109, doi:10.1179/crn.2004.013 (2004).
da Silva Martins, M. J., Caramelo, F. J., Ramalho da Fonseca, J. A. & Gomes Nicolau, P. M. In vitro study on the sensibility and reproducibility of the new T-Scan®III HD system. Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial 55, 14–22, doi:10.1016/j.rpemd.2014.01.001 (2014).
Davies, S. J., Gray, R. M. & Smith, P. W. Good occlusal practice in simple restorative dentistry. British dental journal 191, 365-368, 371–364, 377–381, doi:10.1038/sj.bdj.4801185a (2001).
Kimmel, S. S. Rationale and technique for achieving occlusal harmony. The New York state dental journal 75, 39–43 (2009).
Halperin, G. C., Halperin, A. R. & Norling, B. K. Thickness, strength, and plastic deformation of occlusal registration strips. The Journal of prosthetic dentistry 48, 575–578 (1982).
Gazit, E., Fitzig, S. & Lieberman, M. A. Reproducibility of occlusal marking techniques. The Journal of prosthetic dentistry 55, 505–509 (1986).
Millstein, P. & Maya, A. An evaluation of occlusal contact marking indicators. A descriptive quantitative method. Journal of the American Dental Association 132, 1280–1286; quiz 1319 (2001).
Kihara, T. et al. Influence of filler on bite impression material in transillumination method for occlusal examination. Dental materials journal 32, 144–149 (2013).
Gurdsapsri, W., Ai, M., Baba, K. & Fueki, K. Influence of clenching level on intercuspal contact area in various regions of the dental arch. Journal of oral rehabilitation 27, 239–244 (2000).
Kerstein, R. B., Thumati, P. & Padmaja, S. Force Finishing and Centering to Balance a Removable Complete Denture Prosthesis Using the T-Scan III Computerized Occlusal Analysis System. Journal of Indian Prosthodontic Society 13, 184–188, doi:10.1007/s13191-013-0287-1 (2013).
Cheng, H. J., Geng, Y. & Zhang, F. Q. [The evaluation of intercuspal occlusion of healthy people with T-Scan II system]. Shanghai kou qiang yi xue = Shanghai journal of stomatology 21, 62–65 (2012).
Ma, F. F., Hu, X. L., Li, J. H. & Lin, Y. [Normal occlusion study: using T-Scan III occlusal analysis system]. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi = Chinese journal of stomatology 48, 363–367 (2013).
Abdelnabi, M. H., Swelem, A. A. & Al-Dharrab, A. A. Influence of denture adhesives on occlusion and disocclusion times. The Journal of prosthetic dentistry 115, 306–312, doi:10.1016/j.prosdent.2015.07.014 (2016).
Makofsky, H. W., Sexton, T. R., Diamond, D. Z. & Sexton, M. T. The effect of head posture on muscle contact position using the T-Scan system of occlusal analysis. Cranio: the journal of craniomandibular practice 9, 316–321 (1991).
Kerstein, R. B. Disclusion time measurement studies: A comparison of disclusion time between chronic myofascial pain dyfunction patients and nonpatients: A population analysis. Journal of Prosthetic Dentistry 72, 473–480 (1994).
Acknowledgements
Supported by grant 81130078, 81470773 from National Natural Science Foundation of China and Program for Changjiang Scholars and Innovative Research Team in University (No. IRT13051).
Author information
Authors and Affiliations
Contributions
J.H.C., P.T.L., S.J.Z. and F.W. designed the clinical trial. P.T.L. and Y.J. performed the experiments, wrote and revised the manuscript. S.J.Z., F.W. and L.L. prepared the abutment teeth in the study. F.Y., M.T., H.H.Y. and Y.J. generated the allocation sequence and performed the statistical analysis. J.H.C. supervised the project and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lin, Pt., Jiao, Y., Zhao, Sj. et al. Occlusion and Disocclusion Time Changes in Single Unit Crowns Designed by Functional Generated Path Technique: A Randomised Clinical Trial. Sci Rep 7, 388 (2017). https://doi.org/10.1038/s41598-017-00408-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-00408-0
This article is cited by
-
Computerized dynamic occlusal analysis and its correlation with static characters in post-orthodontic patients using the T-Scan system and the ABO objective grading system
BMC Oral Health (2023)
-
Intraoral occlusal adjustment time and volume required for CAD/CAM crowns fabricated with different virtual mounting methods (A randomized crossover trial)
BDJ Open (2023)
-
Evaluation of occlusal function during orthognathic therapy
Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie (2023)
-
Occlusion time analysis in military pilots affected by bruxism
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.