Abstract
The TILES-2019 data set consists of behavioral and physiological data gathered from 57 medical residents (i.e., trainees) working in an intensive care unit (ICU) in the United States. The data set allows for the exploration of longitudinal changes in well-being, teamwork, and job performance in a demanding environment, as residents worked in the ICU for three weeks. Residents wore a Fitbit, a Bluetooth-based proximity sensor, and an audio-feature recorder. They completed daily surveys and interviews at the beginning and end of their rotation. In addition, we collected data from environmental sensors (i.e., Internet-of-Things Bluetooth data hubs) and obtained hospital records (e.g., patient census) and residents’ job evaluations. This data set may be may be of interest to researchers interested in workplace stress, group dynamics, social support, the physical and psychological effects of witnessing patient deaths, predicting survey data from sensors, and privacy-aware and privacy-preserving machine learning. Notably, a small subset of the data was collected during the first wave of the COVID-19 pandemic.
Measurement(s) | Stress • Burnout • Affect • Depression • Sleep • Physical Activity Measurement • Alcohol Use History • Frequency Any Tobacco Use • Personality • Social Support • Intragroup Conflict • Challenge and Hindrance Stressors • Demographics • Context and Atypical Events • Daily Stressors • Most Stressful Event • Work Context • Job Performance • Job Satisfaction • Stressors at Work • Charting at Home • Coworker Trust • Social Networks at Work • Socialization Outside of Work • Use of Wellness Resources • Heart Rate • Step Count • Acoustic Features • Team Interactions • Proximity to Key Objects • Cell Phone Use • Hospital Contextual Data • Coping with Stress • Productivity at Work • Pride at Work • Teamwork • Support System |
Technology Type(s) | Perceived Stress Scale - 14 Questionnaire • Survey • Patient Health Questionnaire - 9 Item • Pittsburgh Sleep Quality Index • FitBit • International Physical Activity Questionnaire (August 2002) Short Last 7 Days Self-Administered Format • Unihertz Atom Phone • Minew E8- TILES Interaction Sensors • Minew E8- Eddystone Beach • Rescuetime • Evaluations • Patient Census • Interview |
Sample Characteristic - Organism | Homo sapiens |
Sample Characteristic - Location | Los Angeles County and University of Southern California Medical Center |
Similar content being viewed by others
Background & Summary
The Intensive Care Unit (ICU), which provides care for critically ill patients, is an unpredictable and demanding environment. Physicians frequently engage in high-stakes tasks and encounter patient death and ethical issues surrounding end-of-life care1. The ICU may be especially challenging for physicians-in-training, as patient deaths can be traumatic for those with less experience2. Our first goal, therefore, was to identify how working in the ICU impacts the well-being of physicians-in-training, specifically residents (i.e., physicians who completed medical school but practice under supervision). Understanding factors that contribute to resident well-being is critical, as residents report higher levels of depression and burnout than the general population3. Poor well-being may also have significant consequences for patient care, as burnout is linked with lower quality care and more medical errors4.
Our second goal was to examine team functioning in a demanding workplace. Several studies suggest that working under extreme circumstances may lead to decreased cooperation and communication quality5,6. Conversely, working under extreme circumstances may create solidarity7. In the ICU, residents are supervised by an attending physician and a fellow (i.e., physicians who completed residency and are receiving critical care medicine training). Junior residents work closely with more senior residents and all residents coordinate care with nurses. Our study sought to shed light on how team interactions fluctuated in conjunction with workplace demands. Understanding whether demanding situations can affect team functioning is vital, as some studies have found a link between teamwork quality and patient outcomes8.
Most studies on individual and team functioning among physicians are cross-sectional (e.g.6,9,10,11), with a notable exception being a study that examined real-time, within-subject associations between work activities and stress12. A limitation of cross-sectional designs is that they assume that these factors are stable across time, when in fact, they may be dynamic. For example, work hours may fluctuate daily depending on the patient census. Intensive longitudinal designs, which can be used to model how individuals and teams respond to day-to-day changes, are thus needed.
Most studies on individual and team functioning among physicians also rely on self-report (e.g.6,9,13,14). Recent advances in bio-behavioral sensing enable continuous and unobtrusive measurement of heart rate and sleep quality15. Advances in the Internet-of-Things (IoT) and cloud computing enable interactions to be studied using off-the-shelf devices. Raw audio can also be processed in-device so that information regarding the quality of interactions can be extracted while preserving privacy. We leveraged these bio-behavioral sensing opportunities together with self-report measures.
This study extended our prior work which also used an intensive longitudinal design and a combination of bio-behavioral sensing and self-report measures to examine well-being and job performance among healthcare professionals16. Our current study is unique because participants worked in the same unit, enabling us to observe team-level interactions, and because participants were still in training, which may give greater insight into how individuals acclimate to a demanding workplace.
We observed 57 residents during their three-week ICU rotation at the Los Angeles County and University of Southern California Medical Center (LAC + USC). Residents completed baseline measures of mental and physical health, social support, and personality, and were interviewed. They also completed daily surveys that assessed stress, sleep, job performance and satisfaction, and weekly surveys that assessed exercise, substance use, and relationships with teammates. They wore sensors such as a Fitbit, a smartphone that captured audio features, and a Minew sensor (referred to as the TILES Interaction Sensor or TIS) that detected when they were in proximity to others wearing the sensor, as a proxy for team interactions. Uniquely, we recruited full-time employees who worked with the residents (e.g., nurses) to wear the TIS device, so that a more complete picture of residents’ interactions could be obtained. Lastly, we obtained job performance evaluations and hospital contextual data (e.g., patient census).
Our data set has applications in health psychology, industrial-occupational psychology, medical education, signal processing, and machine learning/AI. Our data set also presents opportunities to model changes due to the COVID-19 pandemic, as a small subsample of residents were participating when the first cases arrived at the hospital on March 23, 2020.
The data are available at: https://tiles-data.isi.edu/17.
Methods
Location and Setup
The study took place in the ICU of the Los Angeles County and University of Southern California Medical Center (LAC + USC). The ICU, which had a capacity of fifty beds, was divided into two units. Each team consisted of an attending physician, a Pulmonary, Critical Care, and Sleep Medicine fellow, and six to seven residents. Most residents rotated through the ICU for three weeks.
Residents’ shifts generally followed the schedule outlined in Table 1, which consisted of both individual and team management of patients. From 6:30 to 7:00 AM, residents received updates from the night team (i.e., sign out), reviewed charts, and divided up the work for the day (i.e., pre-rounds). Led by the fellow, the residents on the team then saw all the patients in the unit from 7:00 to 8:30 AM in order to develop a management plan (i.e., fellow rounds). After fellow rounds, residents continued seeing patients (i.e., work rounds) until the attending arrived at 10:00 AM. From 10:00 AM to 12:00 PM, the attending led the residents and fellow in seeing all the patients in the unit. The attending reviewed new admissions, residents’ work on patient charts, and identified plans for patient care and discharges. From noon to 1:00 PM, residents took their lunch break and on occasion, attended lectures at the hospital. After lunch, they provided care, updated patients’ charts, admitted new patients and discharged patients from the ICU. They may also attend lectures. At the end of their shift, residents briefed the night team on what occurred during the day.
Residents will be referred to as focal participants here while non-resident participants, who only wore the TIS and did not complete surveys or interviews will be referred to as minimally involved participants.
Materials
Baseline Survey
The baseline survey is comprised of the following scales:
-
Perceived Stress. Stress in the past month was measured using the Perceived Stress Scale (PSS)18. The PSS consisted of ten items that were rated on a five-point Likert scale ranging from never (0) to very often (4). Some items were reverse coded as required and the ratings for the ten items were averaged to create a composite score (possible range: 0–4).
-
Burnout. Burnout was measured using the Oldenburg Burnout Inventory (OBI)19. The OBI was comprised of 2 eight-item subscales: disengagement and exhaustion. Items were rated on a four-point scale ranging from strongly agree (1) to strongly disagree (4). Some items were reverse coded and the items for each subscale were averaged (possible range for each subscale: 1–4).
-
Affect. Affect in the past week was measured using the Positive And Negative Affect Schedule (PANAS)20. The PANAS consisted of two subscales: positive and negative affect. Each contained 10 items that were rated on a five-point scale from very slightly or not at all (1) to extremely (5). The items for each subscale were summed to create an aggregate score (possible range for each subscale: 10–50).
-
Depression. The nine-item Patient Health Questionnaire (PHQ-9) was used to assess depressive symptoms in the past two weeks21. The items were rated on a four-point scale from not at all (0) to nearly every day (3) and then aggregated (possible range: 0–27).
-
Anxiety. The trait subscale (denoted STAI-T) of the State and Trait Anxiety Inventory (STAI) was used to assess symptoms of anxiety22. The trait subscale of the STAI consisted of 20 items, which were rated on a four-point scale from almost never (1) to almost always (4). Some of the items were reverse coded as requred. The items were then aggregated (possible range: 20–80).
-
Sleep. The 12-item Medical Outcomes Study (MOS) Sleep Scale was used to measure sleep quantity and quality in the past four weeks23,24. Participants reported the number of hours slept and a dichotomous optimal sleep score was computed (i.e., whether participants slept between 7–8 hrs per night). The sleep quality subscales that were computed were sleep disturbance (mean of 4 items), snoring (1 item), awakening with short of breath or headache (1 item), sleep adequacy (mean of 2 items), sleep somnolence (mean of 3 items), and sleep problems (mean of 9 items). The possible range for these subscales was 0 to 100.
-
Physical Activity. An abbreviated version of the International Physical Activity Questionnaire (IPAQ) was used to assess physical activity25. Participants reported the total amount of time engaging in vigorous and moderate activities across all domains (e.g., at work, for leisure) and the amount of time walking. Their responses were then converted into total MET-minutes, which is a measure of the intensity and duration of physical activity where higher scores indicate greater physical activity. Participants also reported the amount of time spent sitting in the past seven days.
-
Alcohol Use. The Habitual Alcohol Use (HAU) scale was used26. Items included the number of alcoholic drinks consumed in a typical week, their drinking rate (i.e., number of drinks consumed per hour), and the tendency to get drunk while drinking. The items were weighted and summed.
-
Tobacco Use. An abbreviated version of the Global Adult Tobacco Use Scale (GATS) was administered27. Participants reported whether they used tobacco and the total units of tobacco smoked in a typical week.
-
Personality. The Big Five Inventory 2 (BFI-2) was used to assess five dimensions of personality: extraversion, agreeableness, conscientiousness, negative emotionality (formerly known as neuroticism), and openness to experience28. Each subscale consisted of twelve items that were rated on a five-point scale from disagree strongly (1) to agree strongly (5). The mean of each subscale was then computed (possible range: 1–5).
-
Social Support. The Multidimensional Scale of Perceived Social Support (MSPSS) was used to assess perceived support from romantic partners, family, and friends29. Each of these three subscales were comprised of four items. These items were rated on a seven-point scale from very strongly disagree (1) to very strongly agree (7). The mean of each subscale was computed (possible range: 1–7).
-
Intragroup Conflict. The Intragroup Conflict Scale consisted of two subscales: conflict due to tasks, and conflict due to interpersonal relations30. These subscales contained four items each and were rated on a five-point scale from none (1) to a lot (5). The mean of each subscale was computed (possible range: 1–5).
-
Challenge and Hindrance Stressors. The Challenge and Hindrance Stressors Scale (CHSS) was a 16-item scale consisting of two eight-item subscales: challenge stressors (i.e., job demands that create opportunities for personal growth) and hindrance stressors (i.e., job demands that hinder opportunities for growth)31. Items were rated on a five-point scale ranging from strongly disagree (1) to strongly agree (5) and the mean of each subscale was generated (possible range: 1–5).
-
Demographics. Participants reported their gender, relationship status, number of children in household, housing situation (e.g., renting a private apartment, townhouse, condo, or house), people with whom they lived, mode of transportation to work, commute time, and household income in 2019. Household income was dichotomized as $74,000 or below, which is the range in which participants’ salaries fall, or $75,000 and above. Participants’ year in training and the unit in which they worked were obtained from the residency programs. Age, ethnicity, country of birth, and whether English is their native language, have been excluded from the shared data set so that participants cannot be easily re-identified.
Ecological Momentary Assessment
Participants received two surveys daily (including non-work days): a one-item survey on current stress levels in the middle of the workday (hereafter named the midday survey) and a survey on daily stressors, work behaviors, and sleep at the end of the workday (hereafter named the end of day survey). Participants received the midday survey at 12:15 pm during their lunch break and the end of day survey at 6:15 pm. The midday survey stayed open for four hours and the end of day survey stayed open for six hours.
At the end of the week, participants received an end of week survey (hereafter named the end of week survey) in addition to the end of day survey. The end of week survey contained questions on substance use, exercise, work stressors, relationships with co-workers, and the utilization of wellness resources offered by the school of medicine and was administered in conjunction with the end of day survey. These items were only asked weekly in order to minimize participant burden and maximize response rates. As participants’ ICU rotations began on a Tuesday, participants received the end of week survey on Mondays.
-
Midday Survey. Participants indicated how stressed they were that morning on a scale from not at all stressed (1) to a great deal of stress (7).
-
End of Day Survey
-
Context and Atypical Events. Participants indicated what they were doing (e.g., work, leisure, household activities) and where they were (e.g., home, work, outdoors) immediately before taking the survey. They also listed any atypical events that had occurred or were expected to occur that day.
-
Stress. Participants indicated how stressed they were that afternoon on a scale from not at all stressed (1) to a great deal of stress (7) (same as the midday survey).
-
Daily Stressors. Participants indicated whether they had experienced stress that day from any of the following: Tension or arguments with spouse/partner; tension or arguments with family members; an item breaking; not having enough money to pay bills, loans, or something else that is needed; finding time for self-care; own health problems; someone else’s health problems; doing or needing to do household tasks; caring or arranging care for child; and experiencing discrimination. Participant selected all that applied.
-
Most Stressful Event. Participants were asked to report the most stressful event that occurred that day and the time at which it occurred (e.g., morning, midday, afternoon). Participants’ responses were coded and to protect participants’ privacy, the codes are presented in the data set, rather than the open-ended responses. Codes include patient coded (e.g., when the participant experienced cardiac arrest), many patients, goals of care/family discussions, and ran late/tried to be on time.
-
Work Context. Participants indicated whether they participated in half-day non-clinical activities (e.g., didactics), and therefore were not in the ICU, or were out sick. They also indicated when they started and ended work.
-
Job Performance. Perceived job performance was a single-item scale (i.e., “How would you rate your overall work performance today?”). Participants responded on a six-point scale ranging from poor (1) to excellent (6). This was followed by an open-ended question on the aspect of work that participants felt they had performed the best that day. Again, responses were coded in order to protect sensitive information. Codes include provided good care/managed patients well, rapport with patient/compassionate care, end of life/goals of care, and helped team.
-
Job Satisfaction. Job satisfaction was also a single-item scale (i.e., “Select the face that best describes how you feel about your job today.”). Participants selected from one of five emojis32.
-
Sleep. Two items from the Pittsburgh Sleep Quality Index (PSQI) were used33. Specifically, participants reported the number of hours that they slept last night and rated the overall quality of their sleep on a four-point scale ranging from very bad (1) to very good (4).
-
-
End of Week Survey. The following questions were included on the end of week survey:
-
Alcohol Use. Participants indicated whether they consumed alcohol that week and the number of beverages they consumed.
-
Tobacco Use. Participants indicated whether they used tobacco products that week and the number of tobacco products they used.
-
Physical Activity. Participants indicated whether they exercised that week and the number of hours they spent exercising. The intensity of the activity was not documented.
-
Stressors at Work. Participants indicated the degree to which they felt stressed by the following work events: difficulty finding a computer, difficult patient interactions, conflict with co-workers, too many patients to care for, had to stay late to care for patients, was paged into work to provide emergency medical care, had to supervise more junior residents or staff, clinical and administrative responsibilities, difficult patient cases, and patient death. These items were developed by the research team following an exploratory focus group interview with six residents prior to the full study. The scale ranged from not at all stressful (1) to very stressful (7) and a “not applicable” option was also available. These items were not summed or averaged.
-
Charting at Home. Participants were asked whether they brought work-related tasks home. Specifically, they indicated whether they spent time charting at home (i.e., documenting patient care) that week and the number of hours spent doing so.
-
Coworker Trust. Coworker trust was measured using four items that were rated on a five-point scale ranging from strongly disagree (1) to strongly agree (5)34. The mean of these items was computed.
-
Social Networks at Work. Participants listed the names of up to three team members for the following four categories:1) team members with whom they asked work-related questions in-person, 2) team members with whom they asked work-related questions digitally, 3) team members with whom they shared positive (joys, successes) or negative (frustrations, challenges) experiences from work in-person, and 4) team members with whom they shared positive or negative experiences from work digitally.
-
Socialization Outside of Work. Participants indicated whether they attended social events organized by the residency program and whether they spent time with other residents informally that week.
-
Use of Wellness Resources. Participants indicated whether they utilized the school of medicine’s wellness resources that week.
-
Sensing Devices
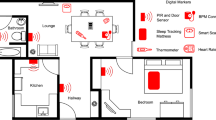
Sensing devices consisted of wearable sensors and environmental sensors (see Table 2). Wearable sensors were given to focal participants. Minimally involved participants received a passive version of the TILES Interaction Sensor (TIS) described below. Environmental sensors were used for the localization of participants within the ICU.
-
Fitbit Charge 3 (Wearable). Participants were given this smart wristband with instructions to wear it continuously during the study and to recharge it while showering. Collected data included heart rate, step count, and sleep quantity and quality.
-
Unihertz Atom Phone (Wearable). Focal participants wore this small Android smartphone at work by clipping it to their clothing near the neckline or by placing it in their shirt pockets. The Atom phone ran custom software and served as a social-sensing, environment-sensing badge, and audio collection device using Bluetooth and its built-in microphone. The audio collection capability was handled by the TILES Audio Recorder (TAR), which immediately processed recorded audio samples by storing anonymized features and discarding the recording35. Participants charged their phones when they were not at work.
-
Minew E8 - TILES Interaction Sensor (TIS) Device (Wearable). This Minew E8 was programmed with one of two possible custom-designed firmwares: active mode and passive mode. Its compact size (36.5 × 23.7 × 5 mm) enabled it to be temporarily affixed on the participants’ work badge. Both firmwares acted as beacons, regularly broadcasting custom designed Bluetooth advertisement packets (to be received by active Atom phones, active TIS sensors and Owl-in-Ones). Focal participants wore the active TIS variant which, on top of acting as beacons, also recorded Received Signal Strength Indicators (RSSI) from nearby Eddystone beacons and other TIS devices. The passive TIS variant was given to minimally involved participants.
-
Minew E8 - Eddystone Beacon (Environmental). These Bluetooth implemented the Eddystone BLE advertisement protocol and were attached to key objects in the ICU (e.g., computer monitors, patient beds) to facilitate proximity-based detection of focal and minimally involved participants.
-
reelyActive Owl-in-One (Environmental). These Bluetooth hubs were positioned within the ICU, the resident lounge, and the conference rooms. They collected Bluetooth information from Eddystone beacons and TIS devices described above and from other Owl-in-One hubs.
Phone Apps
We used three smartphone applications
-
TILES app. The TILES application, which was a modified version of the application used in our previous study16, was used for consenting participants, administering the surveys, and retrieving Fitbit data. It was installed on participants’ personal smartphone (iOS or Android).
-
RescueTime. This third party application was installed on participants’ personal smartphone and was used to monitor cell phone usage.
-
TILES Audio Recorder (TAR). The TILES Audio Recorder (TAR) was installed on the Atom phone and was used for audio and Bluetooth proximity recording and processing. It collected fewer features than the TAR used in our previous study16 but it still captured the same amount of information from audio modality.
Interviews
Interviews were used to obtain rich descriptions of participants’ experiences working in the ICU and their sources of support. Participants were interviewed at the beginning of their rotation (i.e., pre-study interview) and after their rotation ended (i.e., post-study interview). For the pre-study interview, participants were asked about their work experiences and sources of support in the month prior to their ICU rotation. For the post-study interview, participants responded to these questions in the context of their ICU rotation. Conducting interviews at the beginning, as well as, the end of the rotation, allowed for greater insights into the experiences that are unique to working in the ICU. We asked:
-
1.
How stressed do you feel this week in comparison to last week? Why do you feel more stressed/less stressed/about the same?
-
2.
Can you give me an example of how you dealt with a stressful situation at work in the last month/in the ICU?
-
3.
Can you describe a time when you felt productive or efficient at work in the last month/in the ICU?
-
4.
Can you describe a time when you felt proud at work in the last month/in the ICU?
-
5.
What did you enjoy about working with your team in the last month/in the ICU? What did you find challenging about working with your team in the last month/in the ICU?
-
6.
Can you name people (maximum of five) who were in your support network during the last month/during your ICU rotation (you can name your relationship to them, rather than their name). How did they support you?
Job Performance Evaluations
At the end of every rotation, job performance evaluations are given by the attending(s) that supervised them and their teammates. Over the course of residency, the job performance evaluations are tracked and assessed to ensure that residents hit the necessary training milestones to become eligible for initial certification and are ready for independent practice. The residency directors review the evaluations on a monthly basis.
These evaluations that were used in this study were designed by the residency program and based on the developmental milestones set by the American Board of Internal Medicine. Participants were given the option on the consent form to decline having employee data, such as job evaluations, accessed by researchers.The anonymized evaluations are available in the data set as a measure of job performance. Refer to Table 3 for the items.
-
Attending Evaluations. Forty-seven participants granted the research team permission to access their job evaluations. The number of evaluations participants received varied, as not all of the attendings completed their evaluations. Moreover, attendings rotated through different services and their schedules were not aligned with residents; thus, some participants were evaluated by multiple attendings. Nonetheless, all but one participant received at least one evaluation (43% 1 evaluation, 47% 2 evaluations, 9% 3 evaluations). Participants were rated on their patient care and procedural skills, medical knowledge, system-based practices, practice-based learning and improvement, professionalism, and interpersonal and communication skills on a scale from 1 to 5 (1.0 = at the level of an intern (i.e., first-year resident), 1.5 = between intern and PGY2 (i.e., postgraduate year 2, second-year resident), 2.0 = at the level of a PGY2, 3.0 = between PGY2 and PGY3 (i.e., postgraduate year 3, third-year resident), 3.5 = at the level of PGY3, 4.0 = above the level of a PGY3, 5.0 = aspirational).
-
Peer Evaluations. Peer evaluations were optional; thus, only half of participants (n = 23) received a peer evaluation. Fifteen percent of participants received 1–3 evaluations, 28% received 4–6 evaluations, and 6% received 7–9 evaluations. Participants were rated on their interpersonal and communication skills, patient and procedural skills, and professionalism on a scale from 1 to 5 (1 = unsatisfactory, 2 = marginal, 3 = average, 4 = good, 5 = outstanding).
Hospital contextual data
We obtained patient census and death records from the hospital to contextualize participants’ daily work demands.
-
Patient Census. A list of patients that were in the ICU during the study period was obtained. For each patient, we received the date and time when they were admitted to the ICU, the unit they were in, and the date and time they were discharged from the ICU.
-
Patient Deaths. A list of deaths that occurred during the study period was also obtained (no names were given). For each patient death, we received the corresponding date, time, unit, and room number.
Study Procedures
All these steps were conducted in accordance with University of Southern California’s Institutional Review Board (IRB) approval (study ID HS-19-00606).
Requirements for Eligibility
Residents were invited to participate as focal participants if they rotated through the ICU between November 2019 and April 2020. In addition, they needed to be proficient in speaking and reading English and have access to an Internet and Bluetooth-enabled personal smart phone (not used by anyone else) running Android 4.3 or iOS 8 or newer, a personal email account, and WiFi at home.
Full-time employees who worked with the residents in the ICU were invited to participate as minimally involved participants. These included attending physicians, fellows, nurses, and a small number of residents whose rotation only partially overlapped with the study.
Recruitment
Residents who were rotating through the ICU between November 2019 and April 2020 were contacted by their program coordinators. Those who expressed interest were asked to complete a screening survey to determine their eligibility. Eligible residents were then scheduled for an enrollment session. They also received a text with the link and directions to download the TILES study app.
Research team members approached minimally involved participants at the start or end of their shifts to inform them about the study. Minimally involved participants were also informed about the study through email and flyers posted in the ICU.
Participant Enrollment Session
Residents who indicated their interest were invited to a one-hour enrollment session prior to the start of their rotation. However, due to scheduling conflicts, 11 participants (19%) were enrolled on their first day of their ICU rotation. During the enrollment session, residents who had not done so downloaded the TILES study app and indicated their consent via the app. They received their sensors (i.e., a TIS device, a Fitbit, and an Atom phone) and instructions on when and how to wear them. They were shown how to sync their Fitbit and Rescuetime accounts and received information on the survey and interview schedules and the environmental sensors that were placed in the ICU. They were also informed about the compensation scheme and were given their gift card, which was loaded weekly.
Minimally involved participants who consented to participate were shown how to wear their TIS devices and were informed about their compensation.
Baseline Survey
After the enrollment session, participants received a link to the baseline survey. They were instructed to complete the survey prior to the start of data collection or for those who were enrolled on the first day of their ICU rotation, as soon as possible. The survey was administered through Qualtrics and could be completed on a computer or mobile device. The median time to complete the survey was 31 minutes (Q1-Q3 = 18 minutes-98 minutes).
Data Collection
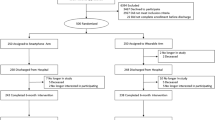
All residents were invited to participate in the study for four weeks, as some residents (n = 7) were scheduled to work in the ICU for four weeks. The remaining residents worked in the clinics, other units in the hospital, or were on the night shift in the ICU during the fourth week. For consistency across participants, we have made data from participants’ ICU rotation (day shift only) available. For participants who were scheduled to be in the ICU for four weeks, data from the first three weeks is available. Figure 1 shows the number of focal participants over the weeks of the study.
Interviews
Participants were scheduled to be interviewed by the graduate medical wellness clinician during the first two weeks of their data collection period (pre-study interview) and again after they completed data collection (post-study interview). However, due to scheduling difficulties, a subset of participants did not complete the pre-study interview (n = 8) and more than a third of participants completed their pre-study interviews after the second week (n = 24). All participants completed the post-study interview. Interviews were 15–20 minutes and detailed notes were taken by the wellness clinician. Interviews conducted on or after March 18, 2020 were conducted over the phone due to social distancing guidelines.
Job Performance Evaluations and Hospital Contextual Data
Job performance evaluations were obtained from the residency programs and patient census and death data were obtained from the hospital.
Off-boarding Session
At the end of the data collection period, participants were off-boarded by a research assistant. The off-boarding sessions lasted ten minutes and participants returned their Atom phones and TIS devices. Research assistants also confirmed that participants’ Rescuetime accounts were synced to the TILES app.
Off-boarding sessions for the minimally involved participants were also faciliated by a research assistant and consisted of participants returning their TIS devices and receiving their gift cards.
Incentives Structure
Focal participants were compensated with a gift card and were allowed to keep the Fitbit. To encourage engagement in the study, participants were paid weekly and the amount they received was commensurate with the number of tasks they completed (see Table 5). Participants also earned points each day, which were then translated into monetary amounts (see Table 4). Depending on the number of points they accrued, participants earned up to $25 at the end of the week (see Table 5). At the end of the study, the number of points that participants earned were summed and participants were awarded bonus points for downloading and installing the TILES app, for authorizing Fitbit access, for weeks where they earned at least 205 points, and for weeks where they earned more points than they did the previous week. The top three-point earners also received bonuses of $150, $100, and $75 respectively.
Minimally involved participants were compensated with a $125 gift card.
Data Acquisition and Flow
Figure 2 depicts the architecture for the data collection from sensors where information flows from left to right. The left column contains the wearable and environmental sensors providing the data (except for Owl-in-Ones, which serve a double purpose of sensing and processing/sending data). The Fitbit wristband connected to participants’ personal smartphones using Bluetooth. The data was uploaded to a third-party server using an available wireless internet connection (WiFi or LTE) through participants’ smartphones.
The Atom phones stored the data in the device, and data was uploaded manually using the computer through a USB connection. Acquired data included anonymized audio features derived from vocal audio recordings collected by the phone’s internal microphone, and timestamped proximity data obtained throughout the study by detecting Bluetooth pings from broadcasting devices (Eddystone beacons, TIS devices, and Owl-in-Ones) with timestamps.
The Owl-in-Ones received data from the Eddystone beacons and TIS devices. Data was sent through LAC + USC Internet connection (ethernet) using User Datagram Protocol (UDP) to an Amazon Elastic Compute Cloud (AWS EC2) instance which performed filtering against a white list of devices in the study and forwarded (through a RESTful API) the data to an ElasticSearch cluster provided by Elastic.co. Daily dumps of this data were stored securely in the research server.
Data was also collected directly through the participants’ personal smartphones through the TILES app, the RescueTime app, and the Fitbit servers. The TILES app uploaded data directly to the research server while the RescueTime app uploaded data to the RescueTime server and this data was later pulled by the research server. The research server36 included a RESTful API hosting a series of endpoints to collect push-type data streams (i.e., TILES app) in addition to a suite of tasks to fetch pull-type data streams (i.e., Fitbit, RescueTime).
Data Preprocessing
Survey Data
The surveys were scored using SPSS37. In a few rare cases, participants completed the baseline survey more than once. In those instances, the most complete response that was submitted before or during the first week of data collection was kept. One participant submitted their response after the first week of data collection. Their response was excluded, as the data would no longer represent how the participant felt at the beginning of the rotation. In three of the cases, participants had submitted a response previously; thus, baseline data was only missing for one of the participants.
Fitbit Data
Preprocessing of the Fitbit data was very close to that of our previous study16. Fitbit data retrieved using the Fitbit API contained separate time series for measured heart rate and step count, in addition to a daily summary of physical activity and sleep. Heart rate data was reported on non-uniform intervals anywhere between approximately 5 s and 15 min depending on the participants’ physical activity. Occasionally, long strings of repeated identical heart rate values (usually 70bpm) were reported in the raw data. These strings were typically under 15 minutes but a few were as long as 20 hours. These strings were interpreted as artifacts because of consumer observations that Fitbit technology sometimes incorrectly reported exactly 70 bpm38 and because repeated measures of the same heart rate over several minutes is highly unlikely. Thus, sequences of at least 50 repeated identical heart rate values were replaced with NaN (Not a Number, equivalent to missing values). The step count, daily summary, and sleep data did not contain these long string artifacts and, therefore, were not pre-processed.
Finally, as the Fitbit stores local time only and does not record when time offset changes occurred, we included Fibit sync data with the Fitbit server to indicate the time offset (namely the time offset of the participant’s phone and fitbit sync times). This is a known limitation of Fitbit devices.
Owl-in-One Data
Bluetooth packets were binary encoded as raddecs39 by the Owl-in-Ones, transmitted over the network, and decoded into a JSON structure. Owl-in-ones aggregated Bluetooth packets received from individual devices over a fixed time window. Each raddec contains (i) the timestamp of the first data received from the device, (ii) the number of received packets (called the number of decoding), (iii) the average RSSI, (iv) the MAC addresses of the Bluetooth device and the Owl-in-One, and (v) the received packets. We compiled this data based on the unique identifier from each device.
Atom Phone Proximity Data
The Atom audio badge sensor captured packets from all Bluetooth devices broadcasting Bluetooth advertisements installed at the study location. The application running on the Atom audio badge filtered the Bluetooth packets received against a white list and kept the packets from the Eddystone beacons, TIS devices, and Owl-in-Ones. The RSSI information was pre-processed separately for the Eddystone beacons, TIS devices, and Owl-in-Ones, and stored locally. The MAC addresses associated with TIS sensors were translated into the unique participant identifiers.
The MAC addresses received alongside Bluetooth transmissions from Owl-in-One and Eddystone beacons were mapped to hospital rooms or locations and formatted into a directory name. We hashed the actual directory names, such as the floor number, unit, and room numbers, to keep the hospital’s floor plans private16. We used the following format:
[building name]:[floor#]:[wing/area]:[room type][room #].
Atom Phone Audio Data
Features were extracted on device using a suite of 69 low-level descriptors that are a combination of filterbank data and prosodic features. The Atom phones ran the OpenSMILE toolkit40 to extract features from 25 ms windows every 10 ms. Custom feature configuration file was created specifically for this data collection41. Given the sensitive nature of the data, the computed features were stored on device and the raw audio collected was discarded. To be mindful of participant privacy, only prosodic features were included in this data set release. We plan to release the filterbank features in the future after we ensure the speech content is obfuscated using privacy preservation methods.
For data cleanup and pre-processing, wWe removed all empty files and removed duplicated columns that occur in some files. For each audio sample containing non-empty feature data, the likelihood that audio sample was produced by the participant carrying the Atom device was estimated, which we called the “foreground audio” probability. We reused the approach outlined in our previous study16 to produce this estimate, with a small modification to the dimension of several CNN layers in the VGG-slim42 neural network to accommodate the larger number of mel-frequency cepstral coefficients (MFCCs) collected in this study (40 opposed to 13). The foreground audio probability estimate ranged from 0 (highly unlikely) to 1 (highly likely).
Interviews
The interviews were coded using descriptive codes. Discrepancies in the coding were identified and discussed until agreement was reached. These codes (e.g., teammates were fun, teammates were supportive) were then coded into broader themes (e.g., positive environment). Both the initial codes and the themes were provided in the data set. The original responses were not provided in order to protect participants’ privacy.
Job Performance Evaluations
As some participants were evaluated by multiple attendings or peers, the mean score for each item (e.g., attending evaluation- medical knowledge, peer evaluation- professionalism item 1) was computed.
Hospital Contextual Data
We created two versions of the census data that differ in their granularity. Data users may select the version that best suits their research questions. In the first version, the data were divided into 1-hour time windows. For each of the two units in the ICU, we calculated the following: 1) the number of admissions in each time window, 2) the number of discharges during the time window, 3) the number of patients at the end of the time window, and 4) the maximum number of patients during the time window. In the second version, the data was segmented into 30-minute time windows. The names of the units were anonymized in both versions.
Limitations
One limitation was that we were not able to deploy a follow-up survey due to participants’ limited availability. The onset of the COVID-19 pandemic also prevented longer-term follow up. Nevertheless, the post-study interview at the end of the rotation offered the opportunity for participants to reflect on their experiences as a whole after their rotation ended. A second limitation is that the social interaction data is not complete as some residents, attendings, fellows, and nurses chose not to participate. Participation rates, however, were still high: 70% of residents, 80% of attendings, and 90% of fellows.
Data Records
The TILES-2019 dataset is hosted by the USC Information Sciences Institute17. See Table 7 for a summary of the data folders.
TILES-2019 Main Data Record
Participant Summary
We targeted for recruitment all the residents who were rotating through the ICU during the study period (i.e., between November 2019 and April 2020) and 57 (70%) agreed to participate.There were no differences in program (χ2(2, N = 82) = 1.87, p = 0.393) or in years of experience (Fisher’s exact, p = 0.564) between residents who participated and those who did not. Differences in demographics between residents who participated and those who did not cannot be assessed, as demographic data was not collected for residents who did not participate.
60% of the participants were male (n = 34). Most participants identified as Asian American (n = 32, 56%) or White (n = 16, 28%). A smaller percentage of participants identified as Latino/a (n = 3, 5%), African American (n = 1, 2%), multi-ethnic (n = 1, 2%), other (n = 1, 2%), or preferred not to answer/did not answer n = 3, 5%). Participants were primarily in the Internal Medicine program (n = 45, 79%) and the remaining residents were in the Emergency Medicine (n = 10, 18%) and Internal Medicine-Pediatrics (n = 2, 3%) programs. We did not include participants’ program in this data set in order to prevent re-identification. Our sample was evenly split across years of experience; there were 19 residents in their first year of training (33%), 22 residents in their second year of training (39%), and 16 residents in their third year of training (28%). Participants were given the option to decline providing audio data. Forty-five participants (79%) consented to providing audio data and 12 participants (21%) declined.
The majority of minimally involved participants who were rotating through the ICU during the study agreed to participate (80% of attendings, 92% of fellows). We did not collect data on minimally involved participants, so differences between those who participated and those who did not cannot be determined.
Surveys (surveys folder)
This folder contains the baseline survey file and two EMA files. The “daily-ema.csv.gz” file contains surveys responses from midday surveys and end of day surveys, and “weekly-ema.csv.gz” includes information of weekly survey answers. On the baseline survey file, each row represents the responses from one participant. The EMA file is in tall array format so that each row represents the responses from one participant at a particular timepoint. Missing responses were left blank.
Fitbit (fitbit folder)
We followed the same folder structure for the Fitbit data as in TILES-201816.
daily-summary folder
Each file contains rows with a date and time and a set of daily summaries including resting heart rate, total calories burned, total number of steps, sleep report, and heart rate zone durations. The sleep reports provide information about sleep duration, sleep efficiency, the duration of four sleep stages (awake sleep, light sleep, deep sleep, REM sleep), as well as the timestamp of the start and end of the sleep. There are up to four sleep records per day. Moreover, calorie consumption and duration of four heart rate zones are available in Fitbit daily summaries.
heart-rate folder
Each file has rows with a timestamp and PPG-based heart rate values (beats per minute). The heart rate samples made available by the Fitbit Charge 3 sensors were aggregated over intervals of less than 1, but the time differences between two consecutive samples were non-uniform.
sleep-data folder
Each file has rows containing a timestamp, the sleep phase with its total duration (in), and a sleepId corresponding to a sleep metadata entry in the sleep-metadata folder. Sleep phase is either in the sleep states set (one of asleep, restless, or awake) or in the sleep stages set (one of deep, light, rem, or wake). The timestamp marks the beginning of the sleeping phase.
sleep-metadata folder
Each file has rows for each period of sleep, and metadata for that sleep, including beginning and end, a sleep type (main vs. nap), type of inferred sleep phases (sleep states or sleep stages), duration, and various metrics.
step-count folder
Each file has rows with a timestamp and step count value. In contrast to heart rate values, step count data were sampled with an interval of 1; thus, we report the number of steps taken each minute.
Interviews (interviews folder)
The file “p2-preinterviews-data-public-5.21.csv.gz” contains the coded pre-study interviews, and the file “p2-postinterviews-data-public-5.21.csv.gz” contains the coded post-study interviews. A value of “1” indicates that a code was applied to a participant’s interview while a value of “0” indicates that the code was not applied. The descriptions of the codes can be found in the codebook: “p2-interviews-codebook-public-5.21.csv.gz”
Hospital Contextual Data (hospital-census folder)
In the file “p2-census-1 hr-public-7.2021.csv.gz,” the data are segmented into 1-hour time windows. In the file, “p2-census-30 min-public-7.2021.csv.gz”, the data are segmented into 30-minute time windows. Each line corresponds to the data from each unit at a particular time window.
Job Performance Evaluations (job-performance folder)
The file “p2-evals-data-public-4.2.22.csv.gz” contains the attending and peer evaluations of each participant. Each row represents the evaluation scores for each participant. The file “p2-evals-codebook-public-5.21.csv.gz” contains the codebook.
Metadata (metadata folder)
This folder contains a file with hash-based residents participant IDs, working unit(s) (if available, using the same hashing as for the atom-proximity directories), and year in the program (1st, 2nd or 3rd year). A file indicating the dates when each participant was in the ICU is also available. Most participants (n = 53) were working in the ICU for three consecutive weeks and the exceptions are noted in the document. The schedule document also indicates the unit, which has been anonymized, in which participants were working. Furthermore, this folder includes a file with hash-based minimally involved participant IDs and their positions (N: nurse; F: fellow; A: attending).
Owl-in-Ones (owlinone folder)
Owl-in-One data contains information from other Owl-in-Ones (RSSIs). The Owl-in-One files are organized by Unix time days (meaning that the cutoff is midnight UTC). These files each contain the signals sent and received by the Owl-in-Ones. The sending and receiving MAC addresses and the sender and receivers’ associated directories are included.
Atom Proximity (atomproximity folder)
Atom-based proximity data includes information from three different sources: TIS phones (RSSIs from the TIS sensors of participants), Owl-in-Ones (RSSIs), and Eddystone beacons (RSSIs).
-
tis folder. The tis subfolder is organized by participant ID. Each file contains rows with a timestamp, a participant ID of the TIS device, and the corresponding RSSI values. There are multiple files for each participant.
-
eddystone folder. This folder has one file per participant. Each file contains rows with a timestamp (sorted), the hashed directory of the receiving Eddystone beacon, and the corresponding RSSI value. There is one file per participant.
-
owlinone folder. The owlinone subfolder folder is organized by participant IDs. Each file includes rows with a timestamp, the hashed directory of the receiving Owl-In-One hub, and the corresponding RSSI value. There are multiple files per participant.
Phone timestamps (phone folder)
The files in this folder list the timestamps and the associated time zone offset. The events triggering those records are independent from the time zone offsets changes of the phone and those changes are most likely in between the events.
TILES-2019 Audio Data Record
In this section, we describe the folder structure and contents of the TILES-2019 Audio Data Record. See Table 8.
Folder Structure
raw-features folder
Data from each participant is organized in separate subfolders. The name of each data snippet in the participant subfolder is the unix time at which the recording started.
fg-predictions folder
Similarly, this folder has subfolders for each participant. This folder contains foreground audio predictions for the files in raw-features folder. These files are in NumPy (.npy) format and they store an array with the probability that the corresponding frame in raw-features folder contains foreground speech (as opposed to background speech).
Features
As mentioned in the Data Preprocessing section, we collected both filterbank and prosodic features, of which we are currently releasing only the prosodic features. Filterbank features consist of 40 dimensional MFCCs. The prosodic features collected are: features related to pitch/voicing like fundamental frequency, jitter, shimmer, fundamental frequency after Viterbi smoothing, energy features like: Root Mean Square energy, zero crossing rate, intensity, loudness, average energy in the spectral bands ([250Hz-650Hz], [1000Hz-4000Hz]), spectral rolloffs at 25, 50, 75 and 90 percentiles, various measures/descriptors of spectral domain like flux, centroid, entropy, variance, skewness, curtosis, slope and psychoacoustic sharpness, logarithm of harmonics to noise ratio (HNR) and harmonicity. Jitter (defined as a measure of the cycle-to-cycle variation of fundamental frequency43) is collected with (jitterDDP_sma) and without dithering (jitterLocal_sma) whereas shimmer (defined as a measure of the cycle-to-cycle variation of amplitude43) is only collected without dithering.
Technical Validation
Sensor Validation
Fitbit
There are many studies validating the data from Fitbit devices. For a list of publications, please refer to https://healthsolutions.fitbit.com/research-library/.
TILES Audio Recorder
We presented an analysis of the audio recorder in35 and followed the same procedure as16. TAR primarily extracted the audio features using openSMILE40. OpenSMILE is a widely used tool for extracting a wide range of features from audio signals. To test the feature distortion from the recording device, a recording setup was proposed in35 to allow TAR to record speech amplified through a speaker. In this feature degradation experiment, 1000 gender-balanced utterances from the TIMIT44 database were randomly sampled and concatenated into one file. The audio files were then played through a loud-speaker. Multiple TARs set at distances 15 cm, 20 cm, 25 cm, and 30 cm from the speaker extracted the audio features simultaneously. This experiment quantified the feature distortion by measuring the root-mean-squared error (RMSE) and cosine distance between the features extracted from the source file and recorded features. The results showed that energy-related features were sensitive to recording distance, but pitch and spectral features yield consistent patterns with different recording distances. The results also showed that errors of pitch, MFCC, and LSP were reasonably low (e.g. pitch errors were under 10 Hz when compared with the groundtruth label), which confirmed the robustness of the feature recorded by TAR.
Data Integrity
The compliance rates observed in this data set were similar to those found in our previous TILES-2018 data set16. Table 8 includes a summary of the compliance rates for Fitbit sensor, Atom sensor, and RescueTime App. Table 9 shows a measure of sensor compliance in one-week interval. The decrease in compliance in the last week of the study was not significant.
Sensor Data
Fitbit
Table 10 shows the number of Fitbit recordings across all participants. The recordings were divided by length (i.e., under 4 hours, 4–8 hours, or over 8 hours). Approximately 82.5% of the recordings were over 8 hours while close to 16% of the recordings were under 4 hours.
Owl-in-One, TIS Devices, and Eddystone Beacons
These devices were subjected to a controlled experiment to verify that they ran continuously and to validate the data collection pipeline up to the daily dumps (see section Data acquisition and Flow). In addition, battery life experiments were run in a worst case controlled scenario and a 15 days autonomy was observed (increased to about 3 weeks in a real life setting due to a low power mode).
Atom
Tables 8 and 10 presents the information regarding the total number of hours recorded through the Atom phones, and the number of participants from which these recordings were obtained. The compliance rate was 52% and over 85% of the Atom recordings were over 4 hours. The decrease in compliance rate between the first, second, and third weeks of the study was not significant (Table 9).
Survey Data
Most of the scales used in the baseline scale had α values that were above the threshold of 0.70, which is commonly accepted as “good,” and that were comparable to those reported in the literature (see Table 6)45. Although the α values for agreeableness and open-mindedness scales were below those found in the literature, they were still above 0.70. The sleep disturbance and sleep somnolence scales, however, were below the threshold of 0.70. This may be due to the relatively small number of items in these scales (i.e., 4 and 3 items respectively). The coworker trust scale in the end of week survey was reliable (α = 0.76).
Table 11 demonstrates the opt-in rate for the EMAs, the percentage of completed EMAs, and the total number of completed EMAs by each type (i.e., midday, end of day, end of week). Most participants (>90%) answered at least one of the midday survey and one of the end of day surveys, while 80% of subjects attempted at least one end of week survey. The compliance rates for those subjects who opt-in to answer the midday survey and the end of day survey were 77.2% and 69.7% respectively. The compliance rate for the end of week surveys was 77.2%.
On average, the midday survey took under half a minute to complete (M = 0.41 mins, SD = 1.74) to complete. The end of day survey took, on average, 3.5 minutes to complete (M = 3.49 mins, SD = 7.13 mins) and the end of week survey took 7 minutes to complete (M = 6.90 mins, SD = 12.46 mins).
Works using the Data Set
There are currently no works published using this data set.
Usage Notes
Data Access
Due to privacy concerns, we request a signed Data Usage Agreement (DUA) to grant access to all data records. A user signing this DUA agrees not to de-anonymize the data, identify language content, or share the data with individuals who have not signed a DUA. The document and the form to submit the signed document can be found here: https://tiles-data.isi.edu/download_tiles_2019. Once validated, the user will receive an email with the information on how to download each data record. The same account may be used for both TILES-2018 and TILES-2019 data sets, but different DUAs will be requested to access each data set.
Main Record
The main data record has a total size of 25GB. To be mindful of the use of resources, we ask users to download this record only once.
Audio Record
The audio record has a total size of 151GB. We provide the raw features collected and also the foreground masks that were inferred.
Reading the Files
All files were compressed Comma Separated Values (CSV) files (.csv .gz), except for the foreground predictions which were stored as NumPy (.npy) files46. We recommend directly reading the compressed files. All files can be easily read in Python and R (using the Pandas library in Python47, or data.table48 or tidyverse49 in R). Note that .csv.gz files can also be opened directly in LibreOffice Calc50 (free software alternative to Microsoft Excel) without decompression. If the files need to be decompressed, we recommend using the command line utility gzip.
Data Records: Use Cases
This data set was developed to study the well-being and team functioning of residents using a multi-modal approach. We envision several use cases for this data set.
Signal processing
There are several opportunities for data quality enrichment in time series and graphs over time, including time series of Fitbit data or audio features, and graph-structured data corresponding to interactions. Like the TILES-201816 data set, there are opportunities for the processing of longitudinal survey information, as well as for finding general representations of behavioral multimodal data.
Workplace interactions
Researchers can examine interactions between residents and other members of their team (i.e., other residents, attendings, fellows, nurses) using social network analyses. Interaction data can be studied in conjunction with physiological data and with observed job performance data (i.e., attending and peer evaluations).
Medical training
Researchers can also explore physiological and behavioral differences between residents who have worked in the ICU previously (i.e., second and third year residents) and those who have not (i.e., first year residents). Researchers may also be interested in the effects of witnessing patient deaths.
Code availability
The code is available at https://github.com/usc-sail/tiles-2019-dataset/.
References
Moss, M., Good, V. S., Gozal, D., Kleinpell, R. & Sessler, C. N. An official critical care societies collaborative statement: Burnout syndrome in critical care health-care professionals: A call for action. Chest 150, 17–26 (2016).
Sorensen, R. & Iedema, R. Emotional labour: Clinicians’ attitudes to death and dying. J Health Organ Manag 53, 5–22 (2009).
Dyrbye, L. N. et al. Burnout among u.s. medical students, residents, and early career physicians relative to the general u.s. population. Acad Med 89, 443–451 (2014).
West, C. P., Dyrbye, L. N. & Shanafelt, T. D. Physician burnout: Contributors, consequences and solutions. J Intern Med 283, 516–529 (2018).
Dietz, A. S. et al. in The Wiley Blackwell Handbook of the Psychology of Team Working and Collaborative Processes (eds. Salas, E., Rico, R. & Passmore, J.) Ch. 13 (Wiley Blackwell, 2017).
Flowerdew, L., Brown, R., Russ, S., Vincent, C. & Woloshynowych, M. Teams under pressure in the emergency department: An interview study. Emerg Med J 29, e2 (2012).
Bartone, P. T., Johnsen, B. H., Eid, J., Brun, W. & Laberg, J. C. Factors influencing small-unit cohesion in norwegian navy officer cadets. Mil Psychol 14, 1–22 (2002).
Havyer, R. D. A. et al. Teamwork assessment in internal medicine: A systematic review of validity evidence and outcomes. J Gen Intern Med 29, 894–910 (2014).
Meth, N. D., Lawless, B. & Hawryluck, L. Conflicts in the icu: Perspectives of administrators and clinicians. Intensive Care Med 35, 2068–2077 (2009).
del Carmen, M. G. et al. Trends and factors associated with physician burnout at a multispecialty academic faculty practice organization. JAMA Netw Open 2, e190554 (2019).
Wallace, J. E. & Lemaire, J. On physician well-being- you’ll get by with a little help from your friends. Soc Sci Med 64, 2565–2577 (2007).
Rutledge, T. et al. A real-time assessment of work stress in physicians and nurses. Health Psychol 28, 194–200 (2009).
Estryn-Behar, M. et al. Emergency physicians accumulate more stress factors than other physicians-results from the french sesmat study. Emerg Med J 28, 397–410 (2011).
Shanafelt, T. D. et al. Burnout and satisfaction with work-life balance among us physicians relative to the general us population. JAMA Intern Med 172, 1377–1385 (2012).
Bell, C. L., Allan, J. L., Ross, S., Powell, D. J. H. & Johnston, D. W. How can we better prepare new doctors for the tasks and challenges of ward rounds?: An observational study of junior doctors’ experiences. Med Teach 35, 2068–2077 (2021).
Mundnich, K. et al. TILES-2018, a longitudinal physiologic and behavioral data set of hospital workers. Sci Data 7 (2020).
Yau, J. C. et al. TILES-2019: A longitudinal physiologic and behavioral data set of medical residents in an intensive care unit. University of Southern California (USC), Information Sciences Institute (ISI) https://doi.org/10.25549/md28-dw83 (2022).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J Health Soc Behav 385–396 (1983).
Demerouti, E., Mostert, K. & Bakker, A. B. Burnout and work engagement: A thorough investigation of the independency of both constructs. J Occup Health Psychol 15, 209–222 (2010).
Watson, D., Clark, L. A. & Tellegen, A. Development and validation of brief measures of positive and negative affect: The panas scales. J Pers Soc Psychol 54, 1063–1070 (1988).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The phq-9: Validity of a brief depression severity measure. J Gen Intern Med 16, 606–613 (2001).
Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. R. & Jacobs, G. A. Manual for the State-Trait Anxiety Inventory. (Consulting Psychologists Press, 1983).
Hays, R. D. & Stewart, A. L. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach (eds. Stewart, A. L. & Ware, J. E.) Ch. 14 (Duke University Press, 1992).
Spritzer, K. L. & Hays, R. D. MOS sleep scale: A manual for use and scoring. 1st edn (Rand Corporation, 2003).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35, 1381–1395 (2003).
Mehrabian, A. & Russell, J. A. A questionnaire measure of habitual alcohol use. Psychol Rep 43, 803–806 (1978).
Global Adult Tobacco Survey Collaborative Group. Tobacco questions for surveys: A subset of key questions from the Global Adult Tobacco Survey. 2nd edn (Centers for Disease Control and Prevention, 2011).
Soto, C. J. & John, O. P. The next big five inventory (bfi-2): Developing and assessing a hierarchical model with 15 facets to enhance bandwith, fidelity, and predictive power. J Pers Soc Psychol 113, 117–143 (2017).
Zimet, G. D., Dahlem, N. W., Zimet, S. G. & Farley, G. K. The multidimensional scale of perceived social support. J Pers Assess 52, 30–41 (1988).
Jehn, K. A. A multimethod examination of the benefits and detriments of intragroup conflict. Adm Sci Q 40, 256–282 (1995).
Rodell, J. B. & Judge, T. A. Can “good” stressors spark “bad” behaviors? the mediating role of emotions in links of challenge and hindrance stressors with citizenship and counterproductive behaviors. J Appl Psychol 94, 1438–1451 (2009).
Phan, W. M. J., Amrhein, R., Rounds, J. & Lewis, P. Contextualizing interest scales with emojis: Implications for measurement and validity. J Career Assess 27, 114–133 (2019).
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R. & Kupfer, D. J. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res 28, 193–213 (1989).
Parker, S. K., Williams, H. M. & Turner, N. Modeling the antecedents of proactive behavior at work. J Appl Psychol 91, 636–652 (2006).
Feng, T., Nadarajan, A., Vaz, C., Booth, B. & Narayanan, S. Tiles audio recorder: an unobtrusive wearable solution to track audio activity. In Proceedings of the 4th ACM Workshop on Wearable Systems and Applications, 33–38 (2018).
USC SAIL. Data collection pipeline. https://github.com/usc-sail/tiles-data-collection-pipeline/.
IBM. Spss statistics. https://www.ibm.com/products/spss-statistics.
Fitbit Community. Heart Rate Stuck on 70 bpm. https://community.fitbit.com/t5/Blaze/Blaze-s-Heart-Rate-Stuck-on-70-bpm/td-p/2727738.
reelyActive. Raddec. https://github.com/reelyactive/raddec (2018–2020).
Eyben, F., Wöllmer, M. & Schuller, B. Opensmile: the munich versatile and fast open-source audio feature extractor. In Proceedings of the 18th ACM international conference on Multimedia, 1459–1462 (2010).
USC SAIL. Audio collection config file. https://github.com/usc-sail/tiles-audio-feature-extraction/blob/master/tiles_offline_config/TILES_phase2_core_lld.conf.
Nadarajan, A., Somandepalli, K. & Narayanan, S. S. Speaker agnostic foreground speech detection from audio recordings in workplace settings from wearable recorders. In ICASSP 2019-2019 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), 6765–6769 (IEEE, 2019).
Farrús, M., Hernando, J. & Ejarque, P. Jitter and shimmer measurements for speaker recognition. In Eighth annual conference of the international speech communication association (2007).
Garofolo, J. et al. Darpa timit acoustic-phonetic continuous speech corpus cd-rom TIMIT. NIST Interagency/Internal Report (NISTIR), National Institute of Standards and Technology, Gaithersburg, MD (1993).
Bland, J. M. & Altman, D. G. Statistics notes: Cronbach’s alpha. BMJ 314, 572 (1997).
Numpy documentation. https://numpy.org/doc/.
Pandas documentation. https://pandas.pydata.org/docs/.
R project. https://cran.r-project.org/web/packages/data.table/data.table.pdf.
Tidyverse. https://www.rdocumentation.org/packages/tidyverse.
Libre Office Calc. https://libreoffice.org.
Hays, R. D., Martin, S. A., Sesti, A. M. & Spritzer, K. L. Psychometric properties of the medical outcomes study sleep measure. Sleep Med 6, 41–44 (2005).
Acknowledgements
The research is based upon work supported by the Office of the Director of National Intelligence (ODNI), Intelligence Advanced Research Projects Activity (IARPA), via IARPA Contract No 2017-17042800005. The views and conclusions contained herein are those of the authors and should not be interpreted as necessarily representing the official policies or endorsements, either expressed or implied, of the ODNI, IARPA, or the U.S. Government. The U.S. Government is authorized to reproduce and distribute reprints for Governmental purposes notwithstanding any copyright annotation thereon. We would like to thank Krystle Santos from USC Keck School of Medicine and our research assistants. The study would not have been possible without their contributions. We also thank Evidation Health for their help with data collection and Jeffrey Dungen from reelyActive for his amazing support. Finally, we would like to thank all the volunteers who decided to be a part of the study.
Author information
Authors and Affiliations
Contributions
Joanna C. Yau was responsible for study design and implementation, recruitment, data curation, and manuscript preparation. Focus: Surveys, interviews, and job performance evaluations. Benjamin Girault was responsible for study design and study implementation, data management, data curation, and manuscript preparation. Focus: TILES Bluetooth data collection pipeline design and TILES interaction sensor. Currently at École Nationale de la Statistique et de l’Analyse de l’Information (ENSAI). Tiantian Feng was responsible for study design and implementation, data management, data curation, and manuscript preparation. Focus: TILES audio recorder, Fitbit, Owl-in-One, TILES interaction sensor, RescueTime, and TILES website. Karel Mundnich was responsible for study design and implementation, data management, data curation, manuscript preparation, and TILES website development. Focus: TILES Bluetooth data collection pipeline design, Owl-in-One, TILES interaction sensor, survey, hospital contextual data, and TILES website. Currently at Amazon. Amrutha Nadarajan was responsible for study design, data curation, and manuscript preparation. Focus: Audio data. Brandon M. Booth was responsible for data management, data curation, manuscript preparation, and TILES website development. Focus: TILES Bluetooth data collection pipeline. Currently at University of Colorado Boulder. Emilio Ferrara was responsible for study design and implementation. Kristina Lerman was responsible for study design and implementation. Eric Hsieh was responsible for study design and implementation, recruitment. Focus: Job performance evaluations and hospital contextual data. Shrikanth Narayanan was responsible for study design and implementation, manuscript preparation, and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yau, J.C., Girault, B., Feng, T. et al. TILES-2019: A longitudinal physiologic and behavioral data set of medical residents in an intensive care unit. Sci Data 9, 536 (2022). https://doi.org/10.1038/s41597-022-01636-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41597-022-01636-4