Abstract
We develop soft and stretchable fatigue-resistant hydrogel optical fibers that enable optogenetic modulation of peripheral nerves in naturally behaving animals during persistent locomotion. The formation of polymeric nanocrystalline domains within the hydrogels yields fibers with low optical losses of 1.07 dB cm−1, Young’s modulus of 1.6 MPa, stretchability of 200% and fatigue strength of 1.4 MPa against 30,000 stretch cycles. The hydrogel fibers permitted light delivery to the sciatic nerve, optogenetically activating hindlimb muscles in Thy1::ChR2 mice during 6-week voluntary wheel running assays while experiencing repeated deformation. The fibers additionally enabled optical inhibition of pain hypersensitivity in an inflammatory model in TRPV1::NpHR mice over an 8-week period. Our hydrogel fibers offer a motion-adaptable and robust solution to peripheral nerve optogenetics, facilitating the investigation of somatosensation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data associated with this study are available in the article and the Supplementary Information. Source data are provided with this paper. In addition, the original data for the material characterization, optogenetic stimulation, biocompatibility test, behavior test and pain inhibition have been deposited in the public repository figshare (https://figshare.com) and are accessible at https://doi.org/10.6084/m9.figshare.c.6703152.v3.
Code availability
The codes for EMG data extraction, running cycle counting and horizontal walk scoring used in this work are available at https://doi.org/10.6084/m9.figshare.c.6703152.v3 under an MIT license.
References
Deisseroth, K. Optogenetics. Nat. Methods 8, 26–29 (2011).
Kim, C. K., Adhikari, A. & Deisseroth, K. Integration of optogenetics with complementary methodologies in systems neuroscience. Nat. Rev. Neurosci. 18, 222–235 (2017).
Montgomery, K. L., Iyer, S. M., Christensen, A. J., Deisseroth, K. & Delp, S. L. Beyond the brain: optogenetic control in the spinal cord and peripheral nervous system. Sci. Transl. Med. 8, 337rv335–337rv335 (2016).
Nam, S. & Mooney, D. Polymeric tissue adhesives. Chem. Rev. 121, 11336–11384 (2021).
Chen, R., Canales, A. & Anikeeva, P. Neural recording and modulation technologies. Nat. Rev. Mater. 2, 1–16 (2017).
Liu, X., Liu, J., Lin, S. & Zhao, X. Hydrogel machines. Mater. Today 36, 102–124 (2020).
Park, S. I. et al. Soft, stretchable, fully implantable miniaturized optoelectronic systems for wireless optogenetics. Nat. Biotechnol. 33, 1280–1286 (2015).
Kathe, C. et al. Wireless closed-loop optogenetics across the entire dorsoventral spinal cord in mice. Nat. Biotechnol. 40, 198–208 (2021).
Michoud, F. et al. Epineural optogenetic activation of nociceptors initiates and amplifies inflammation. Nat. Biotechnol. 39, 179–185 (2021).
Zhang, Y. et al. Battery-free, fully implantable optofluidic cuff system for wireless optogenetic and pharmacological neuromodulation of peripheral nerves. Sci. Adv. 5, eaaw5296 (2019).
Brooks, S. P. & Dunnett, S. B. Tests to assess motor phenotype in mice: a user’s guide. Nat. Rev. Neurosci. 10, 519–529 (2009).
Canales, A. et al. Multifunctional fibers for simultaneous optical, electrical and chemical interrogation of neural circuits in vivo. Nat. Biotechnol. 33, 277–284 (2015).
Park, S. et al. Adaptive and multifunctional hydrogel hybrid probes for long-term sensing and modulation of neural activity. Nat. Commun. 12, 3435 (2021).
Lu, C. et al. Flexible and stretchable nanowire-coated fibers for optoelectronic probing of spinal cord circuits. Sci. Adv. 3, e1600955 (2017).
Buchanan, K. L. et al. The preference for sugar over sweetener depends on a gut sensor cell. Nat. Neurosci. 25, 191–200 (2022).
Sparta, D. R. et al. Construction of implantable optical fibers for long-term optogenetic manipulation of neural circuits. Nat. Protoc. 7, 12–23 (2012).
Liu, Y. et al. Soft and elastic hydrogel-based microelectronics for localized low-voltage neuromodulation. Nat. Biomed. Eng. 3, 58–68 (2019).
Tringides, C. M. et al. Viscoelastic surface electrode arrays to interface with viscoelastic tissues. Nat. Nanotechnol. 16, 1019–1029 (2021).
Yuk, H., Wu, J. & Zhao, X. Hydrogel interfaces for merging humans and machines. Nat. Rev. Mater. 7, 935–952 (2022).
Guo, J. et al. Highly stretchable, strain sensing hydrogel optical fibers. Adv. Mater. 28, 10244–10249 (2016).
Choi, M. et al. Light-guiding hydrogels for cell-based sensing and optogenetic synthesis in vivo. Nat. Photonics 7, 987–994 (2013).
Bai, R., Yang, J. & Suo, Z. Fatigue of hydrogels. Eur. J. Mech. A Solids 74, 337–370 (2019).
Liu, J. et al. Fatigue-resistant adhesion of hydrogels. Nat. Commun. 11, 1071 (2020).
Kashyap, S., Pratihar, S. K. & Behera, S. K. Strong and ductile graphene oxide reinforced PVA nanocomposites. J. Alloys Compd. 684, 254–260 (2016).
Oster, G. The scattering of light and its applications to chemistry. Chem. Rev. 43, 319–365 (1948).
Rinawati, M., Triastuti, J. & Pursetyo, K. T. Characterization of elasticity and hydration of composite hydrogel based on collagen-iota carrageenan as a corneal tissue engineering. IOP Conf. Ser. Earth Environ. Sci. 137, 012042 (2018).
Zheng, H. et al. A shape-memory and spiral light-emitting device for precise multisite stimulation of nerve bundles. Nat. Commun. 10, 2790 (2019).
Liske, H., Qian, X., Anikeeva, P., Deisseroth, K. & Delp, S. Optical control of neuronal excitation and inhibition using a single opsin protein, ChR2. Sci. Rep. 3, 3110 (2013).
Iyer, S. M. et al. Virally mediated optogenetic excitation and inhibition of pain in freely moving nontransgenic mice. Nat. Biotechnol. 32, 274–278 (2014).
Antunes, P., Domingues, F., Granada, M. & André, P. Mechanical Properties of Optical Fibers (INTECH Open Access Publisher, 2012).
Guimarães, C. F., Gasperini, L., Marques, A. P. & Reis, R. L. The stiffness of living tissues and its implications for tissue engineering. Nat. Rev. Mater. 5, 351–370 (2020).
Kuthe, C. D., Uddanwadiker, R. V. & Ramteke, A. Experimental evaluation of fiber orientation based material properties of skeletal muscle in tension. Mol. Cell. Biomech. 11, 113–128 (2014).
Zwirner, J., Ondruschka, B., Scholze, M. & Hammer, N. Passive load-deformation properties of human temporal muscle. J. Biomech. 106, 109829 (2020).
Kuthe, C. D. & Uddanwadiker, R. V. Investigation of effect of fiber orientation on mechanical behavior of skeletal muscle. J. Appl. Biomater. Funct. Mater. 14, 154–162 (2016).
Layton, B. & Sastry, A. A mechanical model for collagen fibril load sharing in peripheral nerve of diabetic and nondiabetic rats. J. Biomech. Eng. 126, 803–814 (2004).
Wang, Z. et al. Stretchable materials of high toughness and low hysteresis. Proc. Natl Acad. Sci. USA 116, 5967–5972 (2019).
Griffith, A. A. VI. The phenomena of rupture and flow in solids. Philos. Trans. R. Soc. Lond. A 221, 163–198 (1921).
Park, S., Loke, G., Fink, Y. & Anikeeva, P. Flexible fiber-based optoelectronics for neural interfaces. Chem. Soc. Rev. 48, 1826–1852 (2019).
Nath, T. et al. Using DeepLabCut for 3D markerless pose estimation across species and behaviors. Nat. Protoc. 14, 2152–2176 (2019).
Chiu, I. M. et al. Activation of innate and humoral immunity in the peripheral nervous system of ALS transgenic mice. Proc. Natl Acad. Sci. USA 106, 20960–20965 (2009).
Kalinski, A. L. et al. Analysis of the immune response to sciatic nerve injury identifies efferocytosis as a key mechanism of nerve debridement. eLife 9, e60223 (2020).
Liu, Y. et al. Touch and tactile neuropathic pain sensitivity are set by corticospinal projections. Nature 561, 547–550 (2018).
Boettger, M. K. et al. Differences in inflammatory pain in nNOS-, iNOS- and eNOS-deficient mice. Eur. J. Pain 11, 810–818 (2007).
Basbaum, A. I., Bautista, D. M., Scherrer, G. & Julius, D. Cellular and molecular mechanisms of pain. Cell 139, 267–284 (2009).
Hsueh, B. et al. Cardiogenic control of affective behavioural state. Nature 615, 292–299 (2023).
Sahasrabudhe, A. et al. Multifunctional microelectronic fibers enable wireless modulation of gut and brain neural circuits. Nat. Biotechnol. https://doi.org/10.1038/s41587-023-01833-5 (2023).
Gunaydin, L. A. et al. Natural neural projection dynamics underlying social behavior. Cell 157, 1535–1551 (2014).
Acknowledgements
This work is supported in part by the National Institutes of Health (grant no. 1R01HL153857-01, grant no. 1R01HL167947-01, X.Z.), the National Science Foundation (grant no. EFMA-1935291, X.Z.), the US Army Research Office through the Institute for Soldier Nanotechnologies at MIT (grant no. W911NF-13-D-0001, X.Z.), Department of Defense Congressionally Directed Medical Research Programs (grant no. PR200524P1, X.Z.), the National Institutes of Health (grant no. K99-MH120279, grant no. R00-MH120279, S.R.), the Brain and Behavior Research Foundation (grant no. 29878, S.R.), UMass Amherst Faculty Research Grant (grant no. P1FRG0000000295, S.R.), the National Institute of Neurological Disorders and Stroke (grant no. R01-NS086804 and grant no. R01-NS115025, P.A.), the McGovern Institute for Brain Research (P.A.), the Hock E. Tan and K. Lisa Yang Center for Autism Research (P.A.) and the K. Lisa Yang Brain-Body Center (P.A.). A.S. was supported by the Lore Harp McGovern Fellowship.
Author information
Authors and Affiliations
Contributions
These authors contributed equally: P.A., X.Z., X.L. and S.R. P.A. and X.Z. discussed the initial concept of the hydrogel optical fibers. X.L., S.R., S.L. and S.H. designed the materials and fabrication methods for the hydrogel optical fibers. X.L., J.N. and S.L. designed and conducted the characterization of materials and devices and data analysis. X.L., S.R., W.C., A.S., Q.W. and E.H. conducted the in vivo and ex vivo experiments and data analysis. X.L., S.R., K.F., W.C., J.X., Y.L., Z.H., J.X. and T.Y. designed the behavior assays and conducted the behavioral analysis. X.L., S.R., P.A. and X.Z. wrote the manuscript with input from all authors.
Corresponding authors
Ethics declarations
Competing interests
P.A. has a financial interest in NeuroBionics Inc., a biotechnology company focused on the development of multifunctional fibers for research and clinical applications. X.Z. has a financial interest in SanaHeal, a biotechnology company focused on the development of medical devices for surgical sealing and repair. Z.H. is an advisor for Myro Therapeutics, Axonis and Rugen Therapeutics. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Methods thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editor: Nina Vogt, in collaboration with the Nature Methods team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
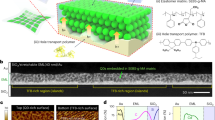
Extended Data Fig. 1 Mechanical design principles for peripheral nerve optogenetics.
a, Light delivery to peripheral nerves under persistent deformation faces challenges including repeated stretching of the bulk fiber and at the fiber-silica and the tissue-fiber interfaces. b, Using a silica fiber with high stiffness and high brittleness leads to fatigue failure under repeated stretching and localized mechanical stress at the silica fiber terminal. c, Using an amorphous hydrogel fiber with high compliance but high brittleness leads to fatigue failure under repeated stretching and no tissue integration at the hydrogel fiber terminal. d, Using a nanocrystalline hydrogel fiber with polymeric nanocrystalline domains leads to fatigue-resistance under repeated stretching and motion-adaptable integration between a hydrogel cuff and a target tissue.
Extended Data Fig. 2 Fabrication procedures of hydrogel optical fibers.
a, Fabrication of polyvinyl alcohol (PVA)-coated short silica fibers. The silica fiber in a ceramic optic ferrule was dip-coated within a PVA solution, and then the PVA solution was allowed to dry and annealed to form the PVA hydrogel coating (50-μm-thick in the swollen state). b, Fabrication of hydrogel cores. The hydrogel core was fabricated by chemical crosslinking of the PVA solution in a silicone mold, together with the PVA-coated optic ferrule at one end and a disk-shaped compartment (3 mm in diameter) at the other end. The chemically crosslinked hydrogel core was then demolded, washed, dried, annealed, and swollen. By hole punching, the hydrogel cuff at the other end of the hydrogel core has the dimensions of 1500 μm in outer diameter and 900 μm in inner diameter in the dry state. c, Fabrication of hydrogel claddings. After inserting the hydrogel core into another silicone mold, the graphene oxide (GO)-PVA hydrogel was chemically crosslinked on the surface of the hydrogel core. After crosslinking and demolding, it was then reduced to reduced graphene oxide (rGO)-PVA hydrogel cladding. The resulting hydrogel core is 600 μm in diameter and the hydrogel cladding is 200 μm thick. The inset is an image of a hydrogel fiber connected to a light source.
Extended Data Fig. 3 Engineered optical performances of hydrogel fibers.
a, Wide-angle X-ray scattering profiles for hydrogel core materials (dry state) with varied annealing times. b-e, Nanocrystalline domain size (b), refractive index (c), normalized absorbance at 473 nm (d), and normalized absorbance at 589 nm (e) for hydrogel core materials with varied annealing times. The dashed lines represent the values of PBS. AU: absorbance units. f, Attenuation coefficient at 473 nm for hydrogel fibers, in which the hydrogel core materials have varied annealing times. g, h, Crystallinity (g) and refractive index (h) for hydrogel core materials with varied glutaraldehyde (GA) amounts. The dashed line represents the refractive index of PBS. i, Attenuation coefficient at 473 nm for hydrogel fibers, in which the hydrogel core materials have varied GA amounts. j, k, Schematic (j) and ray tracing simulation (k) of hydrogel fibers, in which the hydrogel core materials have varied refractive indices. l-m, Representative plots of light intensity delivered through hydrogel fibers in PBS vs. tensile strain, in which the hydrogel core materials have varied annealing time. The right images show the hydrogel fibers (no cladding) at different tensile strains with two ends connected to a light source and a photodetector, respectively. Scale bars: 5 mm. n, Transmittance spectra for hydrogel cladding materials with varied reduction times and the hydrogel core material. o-q, Refractive index (o), normalized absorbance at 473 nm (p), and normalized absorbance at 589 nm (q) for hydrogel cladding materials with varied reduction times and the hydrogel core material. The dashed lines represent the values of PBS. AU: absorbance units. r, Attenuation coefficient at 473 nm for hydrogel fibers over time when incubated in the PBS at 37 °C. One-way ANOVA with Tukey’s multiple comparison test. ns: not significant.
Extended Data Fig. 4 Engineered mechanical performances of hydrogel fibers.
a, Representative plot of nominal stress vs. strain of the hydrogel fiber (without silica) under single-cycle tensile test. The measured tensile strength is 4.6 MPa and Young’s modulus is 1.8 MPa. b, Plot of crack extension rate vs. energy release rate of the hydrogel core material (without silica) under cyclic tensile test. The measured fatigue threshold is 1,400 J m−2. c, Plot of nominal stress vs. strain of the hydrogel fiber (with silica) under cyclic tensile test. The applied stress amplitude in the cyclic tensile test is 1.4 MPa and the cycle number is 10,000 and 30,000. The hysteresis for both stress-strain curves are 0%. d, Plot of strain vs. cycle number of the hydrogel fiber under cyclic tensile test. The applied stress amplitude in the cyclic tensile test is 1.8 MPa and the total cycle number (Nc) is 3,347. e, Microscopic images of the hydrogel fiber at different tensile stresses of 0 MPa and 1.8 MPa under cyclic tensile test. Cavitation happens at the hydrogel-silica interface when the applied stress amplitude is 1.8 MPa. Scale bars: 0.5 mm. f, Plot of applied stress amplitude vs. stretch cycle number to break of the hydrogel fiber (with silica), or the stress-life curve. The measured fatigue strength is 1.4 MPa. g-h, Tensile strength (g) and strain energy density (h) for hydrogel fibers over time when incubated in the PBS at 37 °C. i, Representative plot of normalized light intensity vs. bending radius of the silica, PDMS, and hydrogel fibers in PBS. j, k, Schematic and image of a hydrogel cuff (j) and a hydrogel membrane (k) at the optical fiber terminal attached to artificial tissues (nerve and heart). The inset is an image of the hydrogel cuff in the dark field with light on. One-way ANOVA with Tukey’s multiple comparison test for g,h. ns: not significant.
Extended Data Fig. 5 Gait analysis of mice implanted with hydrogel fibers.
a, Image of a mouse implanted with a hydrogel fiber moving on a running wheel. The mouse is labeled with nodes for the ferrule, neck, back, iliac crest, hip, knee, ankle, and toe. b, c, Frequency of gait cycle (that is, fiber stretch cycle, b) and strain amplitude of hydrogel fibers (c) during mice movement on a running wheel from week 0 to week 6. d, Images of a mouse rearing and grooming when implanted with a hydrogel fiber. The mouse is labeled with nodes for the ferrule, neck, back, iliac crest, hip, knee, ankle, and toe. The fiber length, highlighted in blue, is calculated by the total length of the segments starting from the ferrule to the middle point between the hip and knee. e, Quantified strain amplitude of hydrogel fibers during mice running, rearing, and grooming. f-j, Kinematic stick diagram of mouse hindlimb movement on a running wheel on week 0 (f) before implantation, and week 1 (g), week 2 (h), week 4 (i) and week 6 (j) after implantation. A gait cycle is composed of a stance phase (left) and a swing phase (right) in the kinematic stick diagram. The nodes represent the iliac crest, hip, knee, ankle, and toe from top to bottom. k, Representative plot of distance between the fore toe to hind toe over time during mice movement on a running wheel. The total time period is divided into a few gait cycles, and each cycle is discomposed to a swing phase and a stance phase according to the positive or negative slope. l, Representative plots of knee angle variation during mice hindlimb movement on a running wheel from week 0 to week 6. m, Quantified maximum knee angle during mice hindlimb movement on a running wheel from week 0 to week 6. n, Representative plots of ankle angle variation during mice hindlimb movement on a running wheel from week 0 to week 6. o, Quantified maximum ankle angle during mice hindlimb movement on a running wheel from week 0 to week 6. One-way ANOVA with Tukey’s multiple comparison test for b,c,e,m,o. ns: not significant.
Extended Data Fig. 6 Optogenetic stimulation measured by EMG signals.
a, Overlay plot of EMG signals recorded on the GN muscle when the frequency of optical pulses is 1 Hz (ON: 10 ms, OFF: 990 ms) and the irradiance is 35.4 mW mm−2. b, Plots of EMG signals recorded on the GN muscle (left) and TA muscle (right) when the frequency of optical pulses is 1 Hz and the irradiance is 35.4 mW mm−2. c, Plots of EMG signals recorded on the GN muscle when the frequency of optical pulses is 1 Hz and the irradiance is 35.4 mW mm−2 (left) or 145.0 mW mm−2 (right). d, Plots of EMG signals recorded on the GN muscle when the frequency of optical pulses is 1 Hz (left) or 40 Hz (right), and the irradiance is 35.4 mW mm−2. Blue bars indicate optical pulses from a 473-nm light source.
Extended Data Fig. 7 Behavior and biocompatibility tests of mice implanted with hydrogel fibers.
a, Schematic showing a Thy1::ChR2-EYFP mouse with a hydrogel fiber during von Frey tests. b, c, Nociceptive thresholds of ipsilateral (b) and contralateral (c) hind paw flinch in von Frey tests for Thy1::ChR2-EYFP mice over time after implantation. d, Schematic showing a Thy1::ChR2-EYFP mouse with a hydrogel fiber during horizontal ladder tests. e, Steps are counted and classified as either a normal walk (score 2), a slight slip (score 1), and a fall (score 0). f, Skilled locomotor score of ipsilateral hind paws for Thy1::ChR2-EYFP mice over time after implantation. g-h, Representative histological images of TRPV1::NpHR-EYFP mice’s ipsilateral (g) and contralateral (h) sciatic nerves. Sciatic nerves were harvested 8 weeks after implantation, and stained using hematoxylin and eosin (H&E). Blue: cell nuclei by hematoxylin; pink: extracellular matrix and cytoplasm by eosin. Scale bars: 100 μm. i, j, Representative immunohistochemistry images of Thy1::ChR2-EYFP mice’s ipsilateral (i) and contralateral (j) sciatic nerves. Sciatic nerves were harvested 8 weeks after implantation, and stained using anti-Iba1 antibodies for macrophages. Red: Iba1; blue: DAPI. Scale bars: 100 μm. k, Iba1 relative densities in both ipsilateral and contralateral sciatic nerves. ns: not significant.
Extended Data Fig. 8 Evaluation of optical illumination through implanted hydrogel fibers.
a, Schematic of the temperature measurement through a resistance temperature detector (RTD) at the hydrogel cuff in air. The light source delivers 473-nm optical pulses with an irradiance of 35.4 mW mm−2. b, Plots of temperature variation in air when the optical pulses exhibit different duty cycles (DCs). Blue bars indicate optical pulses. c, Temperature increase in air under optical pulses with different DCs. d, Schematic of the temperature measurement through an RTD at the hydrogel cuff in mice. The light source delivers 473-nm optical pulses with an irradiance of 35.4 mW mm−2. e, Plots of temperature variation in mice when the optical pulses exhibit different DCs. Blue bars indicate optical pulses. f, Temperature increase in mice under optical pulses with different DCs. g, Ray tracing simulation of hydrogel fibers with the hydrogel cladding. h, Images of a mouse implanted with a hydrogel fiber with the hydrogel cladding, showing on-target illumination. i, Ray tracing simulation of hydrogel fibers without the hydrogel cladding. j, Images of a mouse implanted with a hydrogel fiber without the hydrogel cladding, showing off-target illumination. k-l, Darkfield (DF) and brightfield (BF) images of a mouse implanted with a hydrogel fiber (no cladding) when the fiber is relaxed (k) and stretched (l). Contours of the hydrogel fiber without cladding are visible in the darkfield. The skin on top of the sciatic nerve is labeled with a green sticker to identify the original sciatic nerve position. m, Change of fiber length and nerve dislocation over fiber stretch cycles. n, Images of the hydrogel cuff before and after 8-week implantation in mice.
Extended Data Fig. 9 Optogenetic inhibition of nociception in naturally behaving mice enabled by hydrogel fibers (control and contralateral).
a, Image of the experimental setup for hot plate tests, during which animal hind paw flinches were observed. b, Schematic of TRPV1::NpHR-EYFP mice (test group) and TRPV1::Cre mice (control group) with ipsilateral and contralateral hind paws. Yellow optical pulses were applied with a pulse width of 25 ms and irradiance of 8.5 mW mm−2. c, Latency of first-time contralateral hind paw flinch in hot plate tests for TRPV1::NpHR-EYFP mice over time after implantation. d, Latency of first-time ipsilateral hind paw flinch in thermal nociception tests for TRPV1::Cre mice over time after implantation. e, Latency of first-time contralateral hind paw flinch in thermal nociception tests for TRPV1::Cre mice over time after implantation. f, Image of the experimental setup for von Frey tests, during which animal hind paw flinch were observed. g, Schematic of TRPV1::NpHR-EYFP mice (test group) and TRPV1::Cre mice (control group) with ipsilateral and contralateral hind paws. Yellow optical pulses were applied with a pulse width of 25 ms and irradiance of 8.5 mW mm−2. h, Nociceptive threshold of contralateral hind paw flinch in von Frey tests for TRPV1::NpHR-EYFP mice over time after implantation. i, Nociceptive threshold of ipsilateral hind paw flinch in von Frey tests for TRPV1::Cre mice over time after implantation. j, Nociceptive threshold of contralateral hind paw flinch in von Frey tests for TRPV1::Cre mice over time after implantation. ns: not significant.
Supplementary information
Supplementary Information
Supplementary Tables 1–21 and Figs. 1 and 2.
Supplementary Video 1
Measurement of normalized light intensity during repeated stretching of a hydrogel optical fiber. The strain amplitude of repeated stretching is 25%. Two ends of the hydrogel optical fiber are connected to a light source and a photodetector, respectively. The normalized light intensity is higher than 87%.
Supplementary Video 2
Deformation of a porcine artery with no fiber showing free deformation, an artery with a silica fiber attached showing constrained deformation and an artery with a hydrogel optical fiber attached showing free deformation. Scale bars, 10 mm.
Supplementary Video 3
Movement of a mouse on a running wheel before and after implantation with a hydrogel optical fiber. The mouse skeleton features are labeled with a series of nodes using DeepLabCut, including the ferrule, neck, back, iliac crest, hip, knee, ankle and toe.
Supplementary Video 4
Analysis of the mechanical strain of a hydrogel optical fiber in a mouse during its movement on a running wheel. The mouse skeleton features are labeled with a series of nodes using DeepLabCut, including the ferrule, neck, back, iliac crest, hip, hind and front knee, hind and front ankle, and hind and front toe.
Source data
Source Data Figs. 1, 2, 3, 4 and Extended Data Figs. 3, 4, 5, 6, 7, 8, 9
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, X., Rao, S., Chen, W. et al. Fatigue-resistant hydrogel optical fibers enable peripheral nerve optogenetics during locomotion. Nat Methods 20, 1802–1809 (2023). https://doi.org/10.1038/s41592-023-02020-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41592-023-02020-9