Abstract
Durvalumab is a programmed death-ligand 1 (PD-L1) inhibitor with clinical activity in advanced urothelial cancer (AUC)1. AUC is characterized by several recurrent targetable genomic alterations2,3,4,5. This study (NCT02546661, BISCAY) combined durvalumab with relevant targeted therapies in biomarker-selected chemotherapy-refractory AUC populations including: (1) fibroblast growth factor receptor (FGFR) inhibitors in tumors with FGFR DNA alterations (FGFRm); (2) pharmacological inhibitor of the enzyme poly-ADP ribose polymerase (PARP) in tumors with and without DNA homologous recombination repair deficiency (HRRm); and (3) TORC1/2 inhibitors in tumors with DNA alteration to the mTOR/PI3K pathway3,4,5.This trial adopted a new, biomarker-driven, multiarm adaptive design. Safety, efficacy and relevant biomarkers were evaluated. Overall, 391 patients were screened of whom 135 were allocated to one of six study arms. Response rates (RRs) ranged 9–36% across the study arms, which did not meet efficacy criteria for further development. Overall survival (OS) and progression-free survival (PFS) were similar in the combination arms and durvalumab monotherapy arm. Biomarker analysis showed a correlation between circulating plasma-based DNA (ctDNA) and tissue for FGFRm. Sequential circulating tumor DNA analysis showed that changes to FGFRm correlated with clinical outcome. Our data support the clinical activity of FGFR inhibition and durvalumab monotherapy but do not show increased activity for any of the combinations. These findings question the targeted/immune therapy approach in AUC.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The authors declare that access to the clinical and biomarker data analyzed here may be obtained in accordance with AstraZeneca’s data-sharing policy as part of an external collaborative request (https://astrazenecagroup-dt.pharmacm.com//DT/Home/Index/) or an external data access request (https://vivli.org/ourmember/astrazeneca/)
References
Powles, T. et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma: updated results from a phase 1/2 open-label study. JAMA Oncol. 3, e172411 (2017).
Grivas, P. & Yu, E. Y. Role of targeted therapies in management of metastatic urothelial cancer in the era of immunotherapy. Curr. Treat. Options Oncol. 20, 67 (2019).
Robertson, A. G. et al. Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 171, 540–556 (2017).
Garcia, J. A. & Danielpour, D. Mammalian target of rapamycin inhibition as a therapeutic strategy in the management of urologic malignancies. Mol. Cancer Ther. 7, 1347–1354 (2008).
Teo, M. Y. et al. DNA damage response and repair gene alterations are associated with improved survival in patients with platinum-treated advanced urothelial carcinoma. Clin. Cancer Res. 23, 3610–3618 (2017).
von der Maase, H. et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J. Clin. Oncol. 18, 3068–3077 (2000).
Bellmunt, J. et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N. Engl. J. Med. 376, 1015–1026 (2017).
Jones, R. J. et al. Randomized phase II study investigating pazopanib versus weekly paclitaxel in relapsed or progressive urothelial cancer. J. Clin. Oncol. 35, 1770–1777 (2017).
Loriot, Y. et al. Erdafitinib in locally advanced or metastatic urothelial carcinoma. N. Engl. J. Med. 381, 338–348 (2019).
Wagle, N. et al. Activating mTOR mutations in a patient with an extraordinary response on a phase I trial of everolimus and pazopanib. Cancer Discov. 4, 546–553 (2014).
Necchi, A. et al. Exceptional response to olaparib in BRCA2-altered urothelial carcinoma after PD-L1 inhibitor and chemotherapy failure. Eur. J. Cancer 96, 128–130 (2018).
Friedlander, M. et al. Pamiparib in combination with tislelizumab in patients with advanced solid tumours: results from the dose-escalation stage of a multicentre, open-label, phase 1a/b trial. Lancet Oncol. 20, 1306–1315 (2019).
Bellmunt, J. et al. Prognostic factors in patients with advanced transitional cell carcinoma of the urothelial tract experiencing treatment failure with platinum-containing regimens. J. Clin. Oncol. 28, 1850–1855 (2010).
Massard, C. et al. Safety and efficacy of durvalumab (MEDI4736), an anti-programmed cell death ligand-1 immune checkpoint inhibitor, in patients with advanced urothelial bladder cancer. J. Clin. Oncol. 34, 3119–3125 (2016).
Bellmunt, J., Powles, T. & Vogelzang, N. J. A review on the evolution of PD-1/PD-L1 immunotherapy for bladder cancer: the future is now. Cancer Treat. Rev. 54, 58–67 (2017).
Zhang, Q. et al. Prognostic and predictive impact of circulating tumor DNA in patients with advanced cancers treated with immune checkpoint blockade. Cancer Discov. 10, 1842–1853 (2020).
Christensen, E. et al. Early detection of metastatic relapse and monitoring of therapeutic efficacy by ultra-deep sequencing of plasma cell-free DNA in patients with urothelial bladder carcinoma. J. Clin. Oncol. 37, 1547–1557 (2019).
Mariathasan, S. et al. TGFbeta attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554, 544–548 (2018).
Taber, A. et al. Molecular correlates of cisplatin-based chemotherapy response in muscle invasive bladder cancer by integrated multi-omics analysis. Nat. Commun. 11, 4858 (2020).
Choi, W. et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 25, 152–165 (2014).
Kamoun, A. et al. A consensus molecular classification of muscle-invasive bladder cancer. Eur. Urol. 77, 420–433 (2020).
Rosenberg, J. E. et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387, 1909–1920 (2016).
Grivas, P. et al. Rucaparib for recurrent, locally advanced, or metastatic urothelial carcinoma (mUC): results from ATLAS, a phase II open-label trial. J. Clin. Oncol. 38, 440–440 (2020).
Update on the Phase III NEPTUNE Trial of Imfinzi Plus Tremelimumab in Stage IV Non-small Cell Lung Cancer (AstraZeneca, 2019); https://www.astrazeneca.com/media-centre/press-releases/2019/update-on-the-phase-iii-neptune-trial-of-imfinzi-plus-tremelimumab-in-stage-iv-non-small-cell-lung-cancer-21082019.html
Powles, T. et al. Atezolizumab versus chemotherapy in patients with platinum-treated locally advanced or metastatic urothelial carcinoma (IMvigor211): a multicentre, open-label, phase 3 randomised controlled trial. Lancet 391, 748–757 (2018).
Powles, T. et al. Clinical efficacy and biomarker analysis of neoadjuvant atezolizumab in operable urothelial carcinoma in the ABACUS trial. Nat. Med. 25, 1706–1714 (2019).
Pairawan, S. et al. Cell-free circulating tumor DNA variant allele frequency associates with survival in metastatic cancer. Clin. Cancer Res. 26, 1924–1931 (2020).
Vandekerkhove, G. et al. Plasma ctDNA is a tumor tissue surrogate and enables clinical-genomic stratification of metastatic bladder cancer. Nat. Commun. 12, 184 (2021).
Xing, P. et al. Co-mutational assessment of circulating tumour DNA (ctDNA) during osimertinib treatment for T790M mutant lung cancer. J. Cell Mol. Med. 23, 6812–6821 (2019).
Leonetti, A. et al. Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer. Br. J. Cancer 121, 725–737 (2019).
Antonescu, C. R. et al. Acquired resistance to imatinib in gastrointestinal stromal tumor occurs through secondary gene mutation. Clin. Cancer Res. 11, 4182–4190 (2005).
Acknowledgements
We thank the patients and their families who gave their time and commitment to participate in this study; the CRUK Experimental Cancer Medicine Centre; and staff and investigators at participating sites, including the following. Canada: M. Sawyer, University of Alberta—Cross Cancer Institute; S. S. Sridhar, Princess Margaret Cancer Centre, Toronto; C. Ferrario, Jewish General Hospital, Montreal. France: A. Fléchon, Centre Léon Bérard, Lyon; G. Gravis, Institute Paoli-Calmettes, Marseille; F. Joly, Centre Francois Baclesse, Caen; L. Mourey, Institut Claudius Regaud, Toulouse; A. Ravaud, Bordeaux University Hospital; F. Rolland, Institut de Cancerologie de l’Ouest, Saint-Herblain. Spain: J. Carles, Vall D’Hebron Institute of Oncology, Barcelona; J. P. Maroto, Hospital de la Santa Creu i San Pau, Barcelona; J. P. Vásquez, Hospital Clinico San Carlos, Madrid; A. Rodriquez-Vida, IMIM Hospital del Mar Medical Research Instutute, Barcelona. UK: H.-T. Arkenau, Sarah Cannon Research Institute, London; S. Chowdhury, Guys and St Thomas’ Medical School, London; N. Cook, The Christie NHS Foundation Trust, Manchester (Research at the Christie NHS Foundation Trust was supported by the NIHR Manchester Clinical Research Facility and Manchester Experimental Cancer Medicine Centre award); S. Crabb, University of Southampton; R. Jones, University of Glasgow, Beatson West of Scotland Cancer Centre, Glasgow; T. Powles, Barts Cancer Institute, London. USA: A. V. Balar, Perlmutter Cancer Center, NYU Langone Health, New York; J. Bendell, Tennessee Oncology, Nashville; A. Drakaki, Ronald Reagan UCLA Medical Center, Hematology Oncology, Santa Monica; P. Grivas, University of Washington, Seattle; M. Galsky, Icahn School of Medicine at Mount Sinai, New York; N. Hahn, Johns Hopkins University School of Medicine, Baltimore; E. Lim, New York Presbyterian, Columbia University Irving Medical Centre, New York; D. Petrylak, Yale School of Medicine, New Haven; J. Reeves Jr., Florida Cancer Specialists and Research Institute; B. Rini and P. Grivas, Cleveland Clinic, Cleveland; P. Van Veldhuizen, HCA Midwest, Kansas City. We thank the staff at Sarah Cannon Development Innovations and AstraZeneca who supported this clinical study. Medical writing support was provided by S. Hurrell (Bioscript Medical) and was funded by AstraZeneca. We thank A. Reddy (AstraZeneca) for support with data analysis.
Author information
Authors and Affiliations
Contributions
T.P., S.C., D.P., A.J.B., P.G., D.H., R. Mather, R. McEwen and D.L. contributed to the conception and design of the study. T.P., A.F., D.P., S.S.S., M.D.G., R.J., I.K. and R. Mather acquired the data. T.P., S.C., D.P., A.J.B. S.S.S., M.G., P.G., R.J., D.H., I.K., R. Mather, R. McEwen, F.M. and D.L. contributed to data analysis and interpretation. T.P., S.C., J. Carles, A.F., P.M., D.P., G.G., F.R., N.C., A.J.B., S.S.S., M.G., P.G., A.R., R.J., J. Cosaert and R. Mather contributed to clinical management, patient recruitment and data collection. T.P., A.F., D.P., D.H. and R. Mather contributed administrative, technical or material support. T.P., S.C., D.P., R. Mather, R. McEwen and F.M. contributed to the drafting of the manuscript. T.P., S.C., J. Carles, A.F, P.M., D.P., N.C., A.J.B., S.S.S., M.G., P.G., A.R., R.J., J. Cosaert, D.H., I.K. and D.L. critically revised the manuscript for intellectual content. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
T.P. has received research funding from AstraZeneca, Astellas, Bristol-Myers Squibb, Roche and Merck; and received honoraria for lectures or advisory boards from AstraZeneca, Astellas, Bristol-Myers Squibb, Roche, Merck, Johnson & Johnson, Ipsen, Exelixis, Pfizer, Novartis and Seattle Genetics. D.C. is a full-time employee at AstraZeneca and owns stocks/shares in AstraZeneca. S.C. has held advisory roles for Astellas Pharma, Bayer, Beigene, Clovis Oncology, Janssen-Cilag, and Pfizer; participated in speakers’ bureaux for Pfizer; received honoraria from Clovis Oncology and Novartis; received research funding from Clovis Oncology and Sanofi/Aventis; and received travel expenses from Beigene and Clovis Oncology. G.G. has received travel expenses for symposia from Bristol-Myers Squibb, Sanofi, Astellas, Ipsen, Janssen and Pfizer. F.J. has provided consultancy for Roche, Ipsen, AstraZeneca, Janssen, Tesaro, Bristol-Myers Squibb, Pfizer, Novartis and Sanofi, Astellas. F.J. has received travel/accommodation expenses from Roche, Ipsen, AstraZeneca, Janssen, Tesaro and Bristol-Myers Squibb and has received funding (institution) from Astellas. J. Carles has received research funding from AB Science, Aragon Pharmaceuticals, Arog Pharmaceuticals, Inc., Astellas Pharma, AstraZeneca AB, Aveo Pharmaceuticals, Bayer AG, Blueprint Medicines, BN Immunotherapeutics, Boehringer Ingelheim España, Bristol-Myers Squibb, Clovis Oncology, Cougar Biotechnology, Deciphera Pharmaceuticlas, Exelixis, Hoffmann-La Roche, Genentech, GlaxoSmithKline, Incyte Corporations, Janssen-Cilag, Karyopharm Therapeutics, Laboratoires Leurquin Mediolanum, Lilly, MedImmune, Millennium Pharmaceuticals, Nanobiotix, Novartis Farmaceutica, Pfizer, Puma Biotechnology, Sanofi-Aventis, SFJ Pharma and Teva; has participated in advisory boards for Bayer, Johnson & Johnson, Bristol-Myers Squibb, Astellas, Pfizer, Sanofi, MSD Oncology, Roche and AstraZeneca; has participated in speakers’ bureaux for Bayer, Johnson & Johnson, Asofarma and Astellas; and received travel expenses from Bristol-Myers Squibb, Ipsen, Roche and AstraZeneca. A.F. has received honoraria and travel expenses from AstraZeneca, MSD, Roche, Janssen and Astellas. P.M. declares no competing interests. D.P. consults for Ada Cap (Advanced Accelerator Applications), Amgen, Astellas, AstraZeneca, Bayer, Bicycle Therapeutics, Boehringer Ingelheim, Bristol-Myers Squibb, Clovis Oncology, Eli Lilly, Exelixis, Incyte, Janssen, Mirati, Monopteros, Pfizer, Pharmacyclics, Roche, Seattle Genetics and Urogen; has received research funding from Ada Cap, Agensys, Astellas, AstraZeneca, Bayer, BioXcel Therapeutics, Bristol-Myers Squibb, Clovis Oncology, Eisai, Eli Lilly, Endocyte, Genentech, Innocrin, MedImmune, Medivation, Merck, Mirati, Novartis, Pfizer, Progenics and Replimune; and is a stockholder in Bellicum. F.R. has received honoraria from Merck KGaA and MSD. N.C. has received research funding from RedX Pharmaceuticals, Tarveda, AstraZeneca, Roche, Novartis, Eisai, Boehringer Ingelheim and Taiho; has participated in advisory boards for RedX Pharmaceuticals; and has been an advisor (unpaid) to Roche Pharmaceuticals. Research at the Christie NHS Foundation Trust was supported by the NIHR Manchester Clinical Research Facility and Manchester Experimental Cancer Medicine Centre award. A.B. has received research funding from Genentech, Merck, AstraZeneca, MedImmune, Nektar, Seattle Genetics and Immunomedics; has held a consultancy or advisory role for Genentech, Incyte, Merck, Pfizer, AstraZeneca, MedImmune, Nektar and Seattle Genetics; has had speaker engagements for Genentech, Merck, AstraZeneca and MedImmune; and has participated in steering groups and advisory boards for Merck. S.S.S. has consulted for or served on advisory boards for AstraZeneca, Pfizer, Roche, Merck, Bristol-Myers Squibb, Astellas, Janssen and Bayer. M.G. has held a consultancy or advisory role for Aileron Therapeutics and is a stockholder in Rappta Therapeutics. P.G. has consulted for AstraZeneca, Bayer, Biocept, Bristol-Myers Squibb, Clovis Oncology, Driver, EMD Serono, Exelixis, Foundation Medicine, Genentech/Roche, Genzyme, Heron Therapeutics, Janssen, Merck, Mirati Therapeutics, Pfizer, Seattle Genetics, QED Therapeutics and GlaxoSmithKline; has delivered educational programs to GlaxoSmithKline; and has received research funding from AstraZeneca, Bayer, Genentech/Roche, Merck, Mirati Therapeutics, Oncogenex, Pfizer, Clovis Oncology, Bavarian Nordic, Immunomedics, Debiopharm and Bristol-Myers Squibb. A.R. has received research funding from Pfizer and Merck GA; and has received honoraria and participated in advisory boards for Pfizer, Merck GA, Bristol-Myers Squibb, AstraZeneca, Roche, Novartis, MSD and Ipsen. R.J. has received research funding from AstraZeneca, MSD, Merck Serono, Pfizer, Bristol-Myers Squibb, Roche, Janssen and Astellas; has received honoraria for speaking and advisory boards from AstraZeneca, MSD, Merck Serono, Pfizer, Bristol-Myers Squibb, Janssen and Astellas; and has written for the educational company Mirrors of Medicine (noncompensated). J. Cosaert is an AstraZeneca employee. D.H., I.K., R. Mather and R. McEwen are AstraZeneca employees and stockholders. F.M. is a contract employee of AstraZeneca and shareholder in StatProcess and Health Data Process. D.L. is a former employee of AstraZeneca (as Senior Director Physician on this study), consults for AstraZeneca and has received research funding from Decision Science.
Additional information
Peer review information Nature Medicine thanks David McConkey, Sumanta Pal and the other, anonymous reviewers for their contribution to the peer review of this work. Javier Carmona was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Consort diagram for screened and enrolled participants.
Consort diagram for screened and enrolled participants. Enrolment periods: AZD4547 monotherapy and AZD4547 + durvalumab, Oct 2016 to Jun 2018; olaparib + durvalumab (selected), Feb 2017 to April 2018; olaparib + durvalumab (unselected), Aug 2018 to Mar 2019; vistusertib + durvalumab, Apr 2017 to Jan 2018; durvalumab monotherapy, Oct 2016 to May 2017. R, randomized.
Extended Data Fig. 2 Most frequent DNA alterations from archived tissue.
Common alterations: Mutations: 65% TERT promoter, 59% TP53, 36% KMT2D, 27% KDM6A and 23% KMT2C. Copy number alterations: 31% CDKN2A loss, 31% CDKN2B loss, 12% MDM2 amplification, 12% FRS2 amplification, 11% CCND1 amplification.
Extended Data Fig. 3
Molecular classification of tumours derived from RNA sequencing data.
Extended Data Fig. 4 TGE signature (IFNG, CXCL9, CD274) comparison (n = 22 and n = 18 subjects in AZD4547 and durvalumab arms, respectively).
Each boxplot displays the median, first and third quartiles (lower and upper hinges), the largest value smaller and the smallest value larger than 1.5 interquartile (upper and lower whiskers).
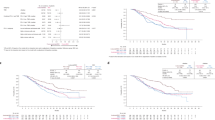
Extended Data Fig. 5 OS according to tumor TMB.
TMB < 10 mutations/Mb was associated with numerically shorter OS when combining the arms irrespective of treatment (HR 1.924 [0.953; 3.884] from Cox model) Logrank test, P = 0.063. HR, hazard ratio; OS, overall survival; TMB, tumor mutational burden.
Extended Data Fig. 6 PFS according to tumor TMB.
TMB < 10 mutations/Mb was associated with shorter PFS when combining the arms irrespective of treatment (HR 1.904 [1.178; 3.078]) Logrank test, P = 0.007. Analysis performed: Kaplan Meier analysis according to the TMB at baseline and Cox model for HR. HR, hazard ratio; PFS, progression-free survival; TMB, tumor mutational burden.
Extended Data Fig. 7 OS according to blood TMB.
TMB ≤ 16 mutations/Mb was associated with similar OS when combining the arms irrespective of treatment (HR 1.21 [0.69–2.13] from Cox model) Logrank test: p = 0.50. HR, hazard ratio; OS, overall survival; TMB, tumor mutational burden.
Extended Data Fig. 8 PFS according to blood TMB.
TMB ≤ 16 mutations/Mb was associated with shorter PFS when combining the arms irrespective of treatment (HR 1.60 [1.05; 2.42]) Logrank test, p = 0.0025. Analysis performed: Kaplan Meier analysis according to the TMB at baseline and Cox model for HR. HR, hazard ratio; PFS, progression-free survival; TMB, tumor mutational burden.
Extended Data Fig. 9 Oncoprint for ctDNA (Guardant Health) n = 111 from baseline samples (patients receiving treatment).
bTMB, blood-derived tumor mutational burden; ctDNA, circulating tumor deoxyribonucleic acid; DDRm, DNA damage repair mutation.
Extended Data Fig. 10 Correlation between expression of mutations and radiological response.
ctDNA, circulating tumor deoxyribonucleic acid; PD, progressive disease; PR, partial response; SD, stable disease.
Supplementary information
Supplementary Information
Supplementary Figs. 1 and 2 and Supplementary Tables 1–4.
Rights and permissions
About this article
Cite this article
Powles, T., Carroll, D., Chowdhury, S. et al. An adaptive, biomarker-directed platform study of durvalumab in combination with targeted therapies in advanced urothelial cancer. Nat Med 27, 793–801 (2021). https://doi.org/10.1038/s41591-021-01317-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-021-01317-6
This article is cited by
-
Progress in systemic therapy for advanced-stage urothelial carcinoma
Nature Reviews Clinical Oncology (2024)
-
Circulating and urinary tumour DNA in urothelial carcinoma — upper tract, lower tract and metastatic disease
Nature Reviews Urology (2023)
-
TALASUR trial: a single arm phase II trial assessing efficacy and safety of TALazoparib and Avelumab as maintenance therapy in platinum-Sensitive metastatic or locally advanced URothelial carcinoma
BMC Cancer (2022)
-
Serial ctDNA analysis predicts clinical progression in patients with advanced urothelial carcinoma
British Journal of Cancer (2022)
-
Personalisierte Therapie beim metastasierten Urothelkarzinom – Vision oder Wirklichkeit?
Die Onkologie (2022)