Abstract
We report on molecular analyses of baseline tumor samples from the phase 3 JAVELIN Renal 101 trial (n = 886; NCT02684006), which demonstrated significantly prolonged progression-free survival (PFS) with first-line avelumab + axitinib versus sunitinib in advanced renal cell carcinoma (aRCC). We found that neither expression of the commonly assessed biomarker programmed cell death ligand 1 (PD-L1) nor tumor mutational burden differentiated PFS in either study arm. Similarly, the presence of FcɣR single nucleotide polymorphisms was unimpactful. We identified important biological features associated with differential PFS between the treatment arms, including new immunomodulatory and angiogenesis gene expression signatures (GESs), previously undescribed mutational profiles and their corresponding GESs, and several HLA types. These findings provide insight into the determinants of response to combined PD-1/PD-L1 and angiogenic pathway inhibition and may aid in the development of strategies for improved patient care in aRCC.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All relevant data are available: clinical response data (Supplementary Table 11), CD8+ summary IHC data (Supplementary Table 12), normalized RNA-seq data (Supplementary Table 13), RNA-seq deconvolution data (ImmuneNet; Supplementary Table 14), gene sets analyzed in this study (Supplementary Table 15), pathway scores (Supplementary Table 16), HLA subtypes in JAVELIN Renal 101 patients (Supplementary Table 17), WES data summary statistics (Supplementary Table 18), MATH scores (Supplementary Table 19), FCGR2A and FCGR3A mutation data (Supplementary Table 20) and gene mutation status data (Supplementary Table 21). Databases used in this analysis included TCGA (https://doi.org/10.1038/nature12222) and MSigDB (https://doi.org/10.1093/bioinformatics/btr260). In addition, subject to certain criteria, conditions and exceptions, Pfizer will also provide access to related individual anonymized participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results/ for more information.
References
Heery, C. R. et al. Avelumab for metastatic or locally advanced previously treated solid tumours (JAVELIN Solid Tumor): a phase 1a, multicohort, dose-escalation trial. Lancet Oncol. 18, 587–598 (2017).
Motzer, R. J. et al. Avelumab plus axitinib versus sunitinib for advanced renal cell carcinoma. N. Engl. J. Med. 380, 1103–1115 (2019).
McDermott, D. F. et al. Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat. Med. 24, 749–757 (2018).
The Cancer Genome Atlas Research Network. Comprehensive molecular characterization of clear-cell renal cell carcinoma. Nature 499, 43–49 (2013).
Ayers, M. et al. IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Invest. 127, 2930–2940 (2017).
Choueiri, T. K. et al. Preliminary results for avelumab plus axitinib as first-line therapy in patients with advanced clear-cell renal cell carcinoma (JAVELIN Renal 100): an open-label, dose-finding and dose-expansion, phase 1b trial. Lancet Oncol. 19, 451–460 (2018).
U.S. National Library of Medicine. Avelumab in metastatic or locally advanced solid tumors (JAVELIN Solid Tumor) (ClinicalTrials.gov, accessed 3 April 2020); https://clinicaltrials.gov/ct2/show/NCT01772004/
Chew, G.-L. et al. DUX4 suppresses MHC class I to promote cancer immune evasion and resistance to checkpoint blockade. Dev. Cell 50, 658–671 (2019).
Geng, L. N. et al. DUX4 activates germline genes, retroelements and immune mediators: implications for facioscapulohumeral dystrophy. Dev. Cell 22, 38–51 (2012).
Smith, K. G. C. & Clatworthy, M. R. FcγRIIB in autoimmunity and infection: evolutionary and therapeutic implications. Nat. Rev. Immunol. 10, 328–343 (2010).
Choueiri, T. K. et al. Biomarker analyses from JAVELIN Renal 101: avelumab + axitinib versus sunitinib in advanced renal cell carcinoma. J. Clin. Oncol. 37, 101 (2019).
Choueiri, T. K. et al. Correlation of PD-L1 tumor expression and treatment outcomes in patients with renal cell carcinoma receiving sunitinib or pazopanib: results from COMPARZ, a randomized controlled trial. Clin. Cancer Res. 21, 1071–1077 (2015).
Rini, B. I. et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal cell carcinoma. N. Engl. J. Med. 380, 1116–1127 (2019).
Motzer, R. J. et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal cell carcinoma. N. Engl. J. Med. 378, 1277–1290 (2018).
Nakano, O. et al. Proliferative activity of intratumoral CD8+ T-lymphocytes as a prognostic factor in human renal cell carcinoma: clinicopathologic demonstration of antitumor immunity. Cancer Res. 61, 5132–5136 (2001).
Barnes, T. A. & Amir, E. HYPE or HOPE: the prognostic value of infiltrating immune cells in cancer. Br. J. Cancer 117, 451–460 (2017).
Hubler, M. J. & Kennedy, A. J. Role of lipids in the metabolism and activation of immune cells. J. Nutr. Biochem. 34, 1–7 (2016).
Coates, C. J. & Decker, H. Immunological properties of oxygen-transport proteins: hemoglobin, hemocyanin and hemerythrin. Cell. Mol. Life Sci. 74, 293–317 (2017).
Masiero, M. et al. A core human primary tumor angiogenesis signature identifies the endothelial orphan receptor ELTD1 as a key regulator of angiogenesis. Cancer Cell. 24, 229–241 (2013).
Robinson, G. et al. Novel mutations target distinct subgroups of medulloblastoma. Nature 488, 43–48 (2012).
Crompton, B. D. et al. The genomic landscape of pediatric Ewing sarcoma. Cancer Discov. 4, 1326–1341 (2014).
Gröbner, S. N. et al. The landscape of genomic alterations across childhood cancers. Nature 555, 321–327 (2018).
Oberg, J. A. et al. Implementation of next generation sequencing into pediatric hematology–oncology practice: moving beyond actionable alterations. Genome Med. 8, 133 (2016).
Hugo, W. et al. Genomic and transcriptomic features of response to anti-PD-1 therapy in metastatic melanoma. Cell 165, 35–44 (2016).
Riaz, N. et al. Tumor and microenvironment evolution during immunotherapy with nivolumab. Cell 171, 934–949 (2017).
Sharma, V., Harafuji, N., Belayew, A. & Chen, Y.-W. DUX4 differentially regulates transcriptomes of human rhabdomyosarcoma and mouse C2C12 cells. PLoS ONE. 8, e64691 (2013).
Ribas, A. Adaptive immune resistance: how cancer protects from immune attack. Cancer Discov. 5, 915–919 (2015).
Szolek, A. et al. OptiType: precision HLA typing from next-generation sequencing data. Bioinformatics 30, 3310–3316 (2014).
Data4Cure (accessed 30 April 2020); https://www.data4cure.com/
Newman, A. M. et al. Robust enumeration of cell subsets from tissue expression profiles. Nat. Methods 12, 453–457 (2015).
Langfelder, P. & Horvath, S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinformatics 9, 559 (2008).
Andersen, P. K. & Gill, R. D. Cox’s regression model for counting processes: a large sample study. Ann. Stat. 10, 1100–1120 (1982).
Therneau T. M. & Grambsch P. M. Modeling Survival Data: Extending the Cox Model (Springer-Verlag, 2000) https://doi.org/10.1007/978-1-4757-3294-8
Liberzon, A. et al. The molecular signatures database hallmark gene set collection. Cell Syst. 1, 417–425 (2015).
Liberzon, A. et al. Molecular signatures database (MSigDB) 3.0. Bioinformatics 27, 1739–1740 (2011).
Roland, C. L. et al. Cytokine levels correlate with immune cell infiltration after anti-VEGF therapy in preclinical mouse models of breast cancer. PLoS ONE. 4, e7669 (2009).
Choueiri, T. K. et al. Immunomodulatory activity of nivolumab in metastatic renal cell carcinoma. Clin. Cancer Res. 22, 5461–5471 (2016).
Brauer, M. J. et al. Identification and analysis of in vivo VEGF downstream markers link VEGF pathway activity with efficacy of anti-VEGF therapies. Clin. Cancer Res. 19, 3681–3692 (2013).
Fehrenbacher, L. et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet 387, 1837–1846 (2016).
Scheller, J., Chalaris, A., Schmidt-Arras, D. & Rose-John, S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochimi. Biophys. Acta 1813, 878–888 (2011).
Russo, L. et al. Characteristics, treatment patterns and safety events from four cohorts of advanced or metastatic cancer patients based on health care claims data. J. Clin. Oncol. 36, e13603 (2018).
Ha, H., Debnath, B. & Neamati, N. Role of the CXCL8-CXCR1/2 axis in cancer and inflammatory diseases. Theranostics 7, 1543–1588 (2017).
Zelenay, S. et al. Cyclooxygenase-dependent tumor growth through evasion of immunity. Cell 162, 1257–1270 (2015).
Powles, T. et al. Immune biomarkers associated with clinical benefit from atezolizumab (MPDL3280a; anti-PD-L1) in advanced urothelial bladder cancer. J. Immunother. Cancer 3, P83 (2015).
Zou, H. & Hastie, T. Regularization and variable selection via the elastic net. J. R. Stat. Soc. Series B Stat. Methodol. 67, 301–320 (2005).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Acknowledgements
The trial was sponsored by Pfizer and is part of an alliance between Pfizer and Merck (Darmstadt, Germany), who provided the study drugs. The investigators worked with Pfizer on the trial design, collection and analysis of data and interpretation of results. Datasets were reviewed by the authors, and all authors participated fully in developing and reviewing the report for publication. Funding for a professional medical writer with access to the data was provided by the sponsors. All authors had full access to all data, and the first author had final responsibility for the decision to submit for publication. The authors vouch for the completeness and accuracy of the data and its analysis, and the fidelity of the trial to the protocol and statistical analysis plan. The authors thank the patients and their families and the investigators, coinvestigators and study teams at each of the participating centers. The authors also thank R.-Y. Tzeng, D. Eleuteri, E. Conley and J. Imus for their assistance with programming and Y. Waumans, K. Marien and D. Peeters from Histogenex. Patients treated at MSKCC were supported in part by a MSKCC Support Grant/Core Grant (P30 CA008748). Medical writing support was provided by S. Rosebeck of ClinicalThinking and funded by Pfizer and Merck (Darmstadt, Germany).
Author information
Authors and Affiliations
Contributions
Conception: R.J.M., P.B.R. and T.K.C. Data acquisition, analysis and interpretation: S.H., A.C.D., R.J.M., P.B.R., X.J.M. and K.A.C. Principal investigator: R.J.M. Biomarker analyses and interpretation: A.C.D., R.J.M., P.B.R., X.J.M. and K.A.C. Supervision of clinical data analysis: S.H., R.J.M. and P.B.R. Supervision of biomarker data analysis: R.J.M. and P.B.R. Acquisition of data and data analysis and interpretation: S.H., A.C.D., R.J.M., J.B.H., P.B.R., X.J.M. and K.A.C. Overall biomarker oversight: R.J.M., P.B.R., X.J.M. and K.A.C. Overall medical oversight: S.H. and R.J.M. R.J.M., P.B.R., T.P., L.A., J.B.H., J.L., X.J.M., K.A.C., M.U., S.K.P., B.A., G.G., M.T.C., K.P., J.L.L., S.H., X.W., W.Z., J.W., A.C., A.d.P., A.C.D. and T.K.C. contributed to the writing of the manuscript and approve its submission.
Corresponding authors
Ethics declarations
Competing interests
R.J.M. reports a consulting or advisory role for Pfizer, Novartis, Eisai, Exelixis, Merck, Genentech, Incyte, Lilly and Roche; research funding (institutional) from Pfizer, Bristol-Myers Squibb, Eisai, Novartis, Genentech and Roche; and reimbursement for travel, accommodations and expenses from Bristol-Myers Squibb. P.B.R. is an employee of Pfizer. T.P. reports personal fees from AstraZeneca, Bristol-Myers Squibb, Eisai, Roche/Genentech, Seattle Genetics, MSD, GSK, Pfizer, Astellas, Merck Serono, Novartis, Ferring and Exelixis and grants from AstraZeneca and Roche outside the submitted work. L.A. reports a consulting/advisory role (institutional) for Novartis, Amgen, Bristol-Myers Squibb, Ipsen, Roche, Pfizer, Astellas Pharma, Merck, MSD, AstraZeneca, Exelixis, Corvus Pharmaceuticals, Peloton therapeutics and research funding from Bristol-Myers Squibb. J.B.H. reports grants and institutional fees from Bristol-Myers Squibb, MSD, Novartis and Neon Therapeutics and institutional fees from Pfizer, Roche/Genentech, Bayer, Amgen, Immunocore, Sanofi, Seattle Genetics, Gadeta BV, GSK, Celsius Therapeutics and AstraZeneca/Medimmune outside the submitted work. J.L. reports personal fees from Eisai, Roche/Genentech, Secarna, Pierre Fabre, EUSA Pharma, MSD, GSK and Kymab and grants and personal fees from Bristol-Myers Squibb, Pfizer and Novartis outside the submitted work. X.J.M. and K.A.C. are employees of Pfizer. M.U. has nothing to disclose. S.P. reports a consulting/advisory role for Genentech, Aveo, Eisai, Roche, Pfizer, Novartis, Exelixis, Ipsen, Bristol-Myers Squibb and Astellas. B.A. reports personal fees from Amgen and Ferring, grants from Ipsen and grants and personal fees from Astellas, AstraZeneca, Bayer, Bristol-Myers Squibb, Janssen, MSD, Pfizer, Roche and Sanofi outside the submitted work. G.G. and K.P. have nothing to disclose. M.T.C. reports personal fees from Eisai Medical Research, EMD Serono, Apricity Health, Pfizer, Genentech and Taiho outside the submitted work. J.L.L. reports grants and personal fees from Pfizer, other fees from Eisai and personal fees from Ipsen, Janssen, Sanofi Aventis, Novartis, Astellas and Bristol-Myers Squibb outside the submitted work. S.H., X.W., W.Z., J.W., A.C., A.d.P. and A.C.D. are employees of Pfizer. T.K.C. reports grants received during the conduct of the study from Pfizer and personal fees received outside the conduct of the study from Agensys, Alexion, Alligent, American Society of Clinical Oncology, Analysis Group, AstraZeneca, Bayer, Bristol-Myers Squibb, Celldex, Cerulean, Clinical Care Options, Corvus, Dana-Farber Cancer Institute, EMD Serono, Eisai, Exelixis, Foundation Medicine, Genentech/Roche, GlaxoSmithKline, Harborside Press, Heron, Ipsen, Kidney Cancer Association, Kidney Cancer Journal, L-path, Lancet Oncology, Lilly, Merck, Michael J. Hennessy Associates, National Comprehensive Cancer Network, Navinata Health, New England Journal of Medicine, Novartis, Peloton Therapeutics, Pfizer, PlatformQ Health, Prometheus Laboratories, Sanofi/Aventis, Seattle Genetics/Astellas, and UpToDate; grants received outside the conduct of the study were from AstraZeneca, Bayer, Bristol-Myers Squibb, Calithera, Cerulean, Corvus, Eisai, Exelixis, Foundation Medicine, Genentech/Roche, GlaxoSmithKline, Ipsen, Merck, Novartis, Peloton Therapeutics, Pfizer, Prometheus Laboratories, Takeda, and Tracon; and medical writing and editorial assistance were provided by ClinicalThinking, Envision Pharma Group, Fishawack Group of Companies, Health Interactions and Parexel and funded by pharmaceutical companies.
Additional information
Peer review information Javier Carmona was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
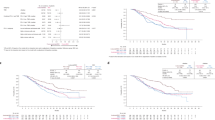
Extended Data Fig. 1 Progression-free survival (PFS) according to (a) CD8+ T cells in the invasive margin, (b) total tumor area and (c) at the tumor center.
Kaplan-Meier analysis was done to evaluate the association of PFS and the presence of CD8+ cells within regions of the tumor (Cox proportional hazards model with one-sided log-rank test). NE, not estimable.
Extended Data Fig. 2 Representative images of CD8 expression by immunohistochemistry in (a, b) CD8+ samples and (c, d) CD8− samples.
a, c, Black boxes denote magnified regions of interest displayed in b and d; scale bars = 2 mm. b, d, Scale bars = 100 μm.
Extended Data Fig. 3 Progression-free survival according to CD8+ T cells following ImmuneNet deconvolution.
Cox proportional hazards model was used and <median group was the reference group. Two-sided Wald test was used for P values.
Extended Data Fig. 4 Heatmap of correlation of WGCNA clusters vs consensus WGCNA clusters.
The heatmap depicts Pearson correlation of signature scores between the 25 original WGCNA clusters and the 23 consensus WGCNA clusters. It demonstrates that 20 of the clusters can be robustly found by both methods. These 20 clusters have been annotated by hypergeometric tests for the top enriched pathways, respectively, and they indeed have the highest correlation to the cluster with a matching annotation by the other method. Three clusters by the consensus method and five clusters by WGCNA (at the bottom right of the heatmap) do not have a matching cluster using the other method, representing contributions from multiple other clusters/biological processes. Importantly, the 26-gene JAVELIN Renal 101 Immuno signature identified by the WGCNA method is highly correlated with the immune response cluster by the consensus method (correlation=0.95, P value <2.2e-16), confirming the robustness of the WGCNA findings.
Extended Data Fig. 5 Volcano plot of association of coexpression signatures with PFS in the combination arm.
Cox proportional hazards model was used and <median (low) group is the reference group. Two-sided Wald test was used for P values. Q values were derived from multiple hypothesis adjustment using FDR.
Extended Data Fig. 6 Progression-free survival according to metabolic pathways: (a) oxygen transport, (b) lipid metabolism, (c) organic acid metabolism and (d) glucocorticoid metabolism.
Cox proportional hazards model was used and <median group was the reference group. Two-sided Wald test was used for P values. No multiple hypothesis adjustment was made.
Extended Data Fig. 7 Correlation between DUX4 signature and expression of HLA-A, -B, and -C.
The triangle symbol in the box represents the mean value. The horizontal line in the box represents the median. Upper and lower box lines represent the third and first quartiles, respectively. Two-sided P value is from Wilcoxon rank-sum test. Analysis value is converted to log2.
Extended Data Fig. 8 HLA types associated with differential progression-free survival.
Cox proportional hazards model was used, and the Other alleles group was the reference group. Two-sided Wald test was used for P values. No multiple hypothesis adjustment was made.
Extended Data Fig. 9 Effect of Fcγ receptor gene polymorphisms on progression-free survival.
*Cox proportional hazards model with wild type as the reference group was used to calculate HR and 95% CI. An HR < 1 indicates better survival in the mutant group, while an HR > 1 indicates better survival in the wild type group. †Two-sided log-rank test was performed to compare between wild type and mutant groups.
Extended Data Fig. 10 Impact of PTEN mutation in combination with other mutations of interest on progression-free survival (PFS) in the (left) avelumab + axitinib and (right) sunitinib arm.
Kaplan-Meier analysis was done to evaluate the association of PFS and the presence of PTEN mutations in combination with other mutations of interest (Cox proportional hazards model).
Supplementary information
Supplementary Information
Supplementary Figs. 1–7.
Supplementary Tables
Supplementary Tables 1–21.
Rights and permissions
About this article
Cite this article
Motzer, R.J., Robbins, P.B., Powles, T. et al. Avelumab plus axitinib versus sunitinib in advanced renal cell carcinoma: biomarker analysis of the phase 3 JAVELIN Renal 101 trial. Nat Med 26, 1733–1741 (2020). https://doi.org/10.1038/s41591-020-1044-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-1044-8
This article is cited by
-
RUNX3 pathway signature predicts clinical benefits of immune checkpoint inhibition plus tyrosine kinase inhibition in advanced renal cell carcinoma
BMC Urology (2024)
-
Tumor immune dysfunction and exclusion subtypes in bladder cancer and pan-cancer: a novel molecular subtyping strategy and immunotherapeutic prediction model
Journal of Translational Medicine (2024)
-
Crosstalk of disulfidptosis-related subtypes identifying a prognostic signature to improve prognosis and immunotherapy responses of clear cell renal cell carcinoma patients
BMC Genomics (2024)
-
New clinical trial design in precision medicine: discovery, development and direction
Signal Transduction and Targeted Therapy (2024)
-
Effect of Annexin A2 on prognosis and sensitivity to immune checkpoint plus tyrosine kinase inhibition in metastatic renal cell carcinoma
Discover Oncology (2024)