Abstract
Precision oncology presumes an accurate prediction of drug response on the basis of the molecular profile of tumors. However, the extent to which patient-derived tumor organoids recapitulate the response of in vivo tumors to a given drug remains obscure. To gain insights into the pharmacobiology of human colorectal cancer (CRC), we here created a robust drug screening platform for patient-derived colorectal organoids. Application of suspension culture increased organoid scalability, and a refinement of the culture condition enabled incorporation of normal and precursor organoids to high-throughput drug screening. Drug screening identified bromodomain and extra-terminal (BET) bromodomain protein inhibitor as a cancer-selective growth suppressor that targets genes aberrantly activated in CRC. A multi-omics analysis identified an association between checkpoint with forkhead and ring finger domaines (CHFR) silencing and paclitaxel sensitivity, which was further validated by gene engineering of organoids and in xenografts. Our findings highlight the utility of multiparametric validation in enhancing the biological and clinical fidelity of a drug screening system.

This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data relevant to this study are available from the corresponding author upon reasonable request. Of the gene expression data used in the study, the data on 37 and 2 organoid lines can be accessed via our previous datasets GSE74843 (ref. 21) and GSE137336 (ref. 19). The expression microarray data of the remaining three lines are available in Gene Expression Omnibus under the accession ID GSE184732. The RNA sequencing and ChIP sequencing data are available in the National Bioscience Database Centre (NBDC) under the accession ID JGAS000378. The ethical protocol approved for this study requires the raw sequencing data to be deposited to the NBDC (https://biosciencedbc.jp/en/) and be available under controlled access for protection of patients’ privacy. Data users need to fulfill the NBDC Guidelines for Human Data Sharing (https://humandbs.biosciencedbc.jp/en/guidelines/data-sharing-guidelines) and the NBDC Security Guidelines for Human Data (for Data Users) (https://humandbs.biosciencedbc.jp/en/guidelines/security-guidelines-for-users). In detail, those who wish to use the data need to conform to the following requirements. First, indicate that the head of the institution to which the data users belong has given permission to implement the research plan that includes the dataset the data users plan to use. Second, provide evidence that the data users have engaged in research related to the dataset the data users plan to use. Third, indicate that the data users have implemented security measures appropriate to the access level of the dataset the data user plans to use. Fourth, obtain approval from the NBDC Human Data Review Board (details on how to apply can be found at https://humandbs.biosciencedbc.jp/en/data-use). Source data are provided with this paper.
References
Stratton, M. R., Campbell, P. J. & Futreal, P. A. The cancer genome. Nature 458, 719–724 (2009).
Holohan, C., Schaeybroeck, S. V., Longley, D. B. & Johnston, P. G. Cancer drug resistance: an evolving paradigm. Nat. Rev. Cancer 13, 714–726 (2013).
Druker, B. J. et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N. Engl. J. Med. 355, 2408–2417 (2006).
Slamon, D. J. et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N. Engl. J. Med. 344, 783–792 (2001).
Bang, Y.-J. et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376, 687–697 (2010).
Chapman, P. B. et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 364, 2507–2516 (2011).
Ramzy, G. M. et al. Patient-derived in vitro models for drug discovery in colorectal carcinoma. Cancers 12, 1423 (2020).
Wilson, T. R. et al. Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors. Nature 487, 505–509 (2012).
Barretina, J. et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 483, 603–607 (2012).
Garnett, M. J. et al. Systematic identification of genomic markers of drug sensitivity in cancer cells. Nature 483, 570–575 (2012).
Basu, A. et al. An interactive resource to identify cancer genetic and lineage dependencies targeted by small molecules. Cell 154, 1151–1161 (2013).
Iorio, F. et al. A landscape of pharmacogenomic interactions in cancer. Cell 166, 740–754 (2016).
Ghandi, M. et al. Next-generation characterization of the Cancer Cell Line Encyclopedia. Nature 569, 503–508 (2019).
Kodack, D. P. et al. Primary patient-derived cancer cells and their potential for personalized cancer patient care. Cell Rep. 21, 3298–3309 (2017).
Dangles-Marie, V. et al. Establishment of human colon cancer cell lines from fresh tumors versus xenografts: comparison of success rate and cell line features. Cancer Res. 67, 398–407 (2007).
Gao, H. et al. High-throughput screening using patient-derived tumor xenografts to predict clinical trial drug response. Nat. Med. 21, 1318–1325 (2015).
Bruna, A. et al. A biobank of breast cancer explants with preserved intra-tumor heterogeneity to screen anticancer compounds. Cell 167, 260–274.e222 (2016).
Sato, T. et al. Long-term expansion of epithelial organoids from human colon, adenoma, adenocarcinoma, and Barrett’s epithelium. Gastroenterology 141, 1762–1772 (2011).
Kawasaki, K. et al. Chromosome engineering of human colon-derived organoids to develop a model of traditional serrated adenoma. Gastroenterology 158, 638–651 (2020).
van de Wetering, M. et al. Prospective derivation of a living organoid biobank of colorectal cancer patients. Cell 161, 933–945 (2015).
Fujii, M. et al. A colorectal tumor organoid library demonstrates progressive loss of niche factor requirements during tumorigenesis. Cell Stem Cell 18, 827–838 (2016).
Drost, J. & Clevers, H. Organoids in cancer research. Nat. Rev. Cancer 18, 407–418 (2018).
Vlachogiannis, G. et al. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science 359, 920–926 (2018).
Ooft, S. N. et al. Patient-derived organoids can predict response to chemotherapy in metastatic colorectal cancer patients. Sci. Transl. Med. 11, eaay2574 (2019).
Yao, Y. et al. Patient-derived organoids predict chemoradiation responses of locally advanced rectal cancer. Cell Stem Cell 26, 17–26 (2020).
Verissimo, C. S. et al. Targeting mutant RAS in patient-derived colorectal cancer organoids by combinatorial drug screening. eLife 5, e18489 (2016).
Boehnke, K. et al. Assay establishment and validation of a high-throughput screening platform for three-dimensional patient-derived colon cancer organoid cultures. J. Biomol. Screen. 21, 931–941 (2016).
Schütte, M. et al. Molecular dissection of colorectal cancer in pre-clinical models identifies biomarkers predicting sensitivity to EGFR inhibitors. Nat. Commun. 8, 14262 (2017).
Fujii, M. et al. Human intestinal organoids maintain self-renewal capacity and cellular diversity in niche-inspired culture condition. Cell Stem Cell 23, 787–793.e786 (2018).
Liu, Y. et al. Comparative molecular analysis of gastrointestinal adenocarcinomas. Cancer Cell 33, 721–735 (2018).
Vassilev, L. T. et al. In vivo activation of the p53 pathway by small-molecule antagonists of MDM2. Science 303, 844–848 (2004).
Pahuja, K. B. et al. Actionable activating oncogenic ERBB2/HER2 transmembrane and juxtamembrane domain mutations. Cancer Cell 34, 792–806.e795 (2018).
Poulin, E. J. et al. Tissue-specific oncogenic activity of KRASA146T. Cancer Discov. 9, 738–755 (2019).
Kopetz, S. et al. Phase II pilot study of vemurafenib in patients with metastatic BRAF-mutated colorectal cancer. J. Clin. Oncol. 33, 4032–4038 (2015).
Hyman, D. M. et al. Vemurafenib in multiple nonmelanoma cancers with BRAF V600 mutations. N. Engl. J. Med. 373, 726–736 (2015).
Prahallad, A. et al. Unresponsiveness of colon cancer to BRAF(V600E) inhibition through feedback activation of EGFR. Nature 483, 100–103 (2012).
Kopetz, S. et al. Encorafenib, binimetinib, and cetuximab in BRAF V600E-mutated colorectal cancer. N. Engl. J. Med. 381, 1632–1643 (2019).
Matano, M. et al. Modeling colorectal cancer using CRISPR–Cas9-mediated engineering of human intestinal organoids. Nat. Med. 21, 256–262 (2015).
Shi, J. & Vakoc, C. R. The mechanisms behind the therapeutic activity of BET bromodomain inhibition. Mol. Cell 54, 728–736 (2014).
Donati, B., Lorenzini, E. & Ciarrocchi, A. BRD4 and cancer: going beyond transcriptional regulation. Mol. Cancer 17, 164 (2018).
Guinney, J. et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 21, 1350–1356 (2015).
Bradner, J. E., Hnisz, D. & Young, R. A. Transcriptional addiction in cancer. Cell 168, 629–643 (2017).
Bolden, J. E. et al. Inducible in vivo silencing of Brd4 identifies potential toxicities of sustained BET protein inhibition. Cell Rep. 8, 1919–1929 (2014).
Roerink, S. F. et al. Intra-tumour diversification in colorectal cancer at the single-cell level. Nature 556, 457–462 (2018).
Overman, M. et al. Phase II study of nab-paclitaxel in refractory small bowel adenocarcinoma and CpG island methylator phenotype (CIMP)-high colorectal cancer. Ann. Oncol. 29, 139–144 (2018).
Le, D. T. et al. PD-1 blockade in tumors with mismatch-repair deficiency. N. Engl. J. Med. 372, 2509–2520 (2015).
Sugimoto, S. et al. Reconstruction of the human colon epithelium in vivo. Cell Stem Cell 22, 171–176 (2018).
Mihara, E. et al. Active and water-soluble form of lipidated Wnt protein is maintained by a serum glycoprotein afamin/α-albumin. eLife 5, e11621 (2016).
Ootani, A. et al. Sustained in vitro intestinal epithelial culture within a Wnt-dependent stem cell niche. Nat. Med. 15, 701–706 (2009).
Fujii, M., Matano, M., Nanki, K. & Sato, T. Efficient genetic engineering of human intestinal organoids using electroporation. Nat. Protoc. 10, 1474–1485 (2015).
Schmidl, C., Rendeiro, A. F., Sheffield, N. C. & Bock, C. ChIPmentation: fast, robust, low-input ChIP-seq for histones and transcription factors. Nat. Methods 12, 963–965 (2015).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet.journal 17, https://doi.org/10.14806/ej.17.1.200 (2011).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Zhang, Y. et al. Model-based analysis of ChIP-Seq (MACS). Genome Biol. 9, R137 (2008).
Whyte, W. A. et al. Master transcription factors and mediator establish super-enhancers at key cell identity genes. Cell 153, 307–319 (2013).
Cong, L. et al. Multiplex genome engineering using CRISPR/Cas systems. Science 339, 819–823 (2013).
Guo, Q. et al. ‘Cold shock’ increases the frequency of homology directed repair gene editing in induced pluripotent stem cells. Sci. Rep. 8, 2080 (2018).
Randolph, L. N., Bao, X., Zhou, C. & Lian, X. An all-in-one, Tet-On 3G inducible PiggyBac system for human pluripotent stem cells and derivatives. Sci. Rep. 7, 1549 (2017).
Acknowledgements
This work was supported by the Project for Cancer Research and Therapeutic Evolution (P-CREATE) from the Japan Agency for Medical Research and Development (AMED) (Grant Number 20cm0106206), JSPS KAKENHI (Grant Numbers JP18J21346, JP17K09395 and JP17H06176) and JST Moonshot R&D (Grant Number JPMJMS2022). K.Toshimitsu was supported by the Japan Society for the Promotion of Science Research Fellowships for Young Scientists. We thank the Screening Committee of Anticancer Drugs supported by Grant-in-Aid for Scientific Research on Innovative Areas, Scientific Support Programs for Cancer Research, from The Ministry of Education, Culture, Sports, Science and Technology, Japan, for providing the SCADS Inhibitor Kit. We also thank the Collaborative Research Resources at the School of Medicine, Keio University for providing technical assistance.
Author information
Authors and Affiliations
Contributions
K. Toshimitsu, A.T. and T.S. conceived the project and designed experiments. A.T., M.M. and M.F. performed organoid experiments. A.T. performed animal experiments. S.T. performed immunostaining experiments. K. Toshimitsu and K. Togasaki performed data analysis. M.F. and T.K. provided resources. K. Toshimitsu, M.F., A.T. and T.S. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
T.S. is an inventor on several patents related to organoid culture.
Peer review
Peer review information
Nature Chemical Biology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Metrics of the modified organoid HTS system.
a, The growth of organoids in Matrigel-embedded culture, static floating culture and floating culture in a rotating vessel. The number of cells in each culture condition was counted on day 0, 2, 5, 7 and 9. n = 3 technical replicates for each condition. b, Doubling time of organoids in the indicated culture conditions. The doubling time was calculated by linear regression of the day of harvesting and logarithmic average cell numbers from day 0 to day 7. c, Comparison of organoid growth metrics measured using confocal fluorescence imaging, ATP abundance and bright-field imaging. Each dot indicates one well. Organoid viability is shown as the relative to the mean of vehicle-treated control. Note that the viability of organoids treated with mTOR inhibitors appear lower in the fluorescence measurement than in the ATP-based assay. d, Comparison of the Z’-factors in conventional and refined culture conditions.
Extended Data Fig. 2 Drug sensitivity of organoids based on drug targets.
a, Biological (left) and pathway (right) targets of the 56 drugs used for screening. b, log2IC50 values and their standard deviation (SD) in replicate experiments using a normal colonic organoids line (NLCRC15). Each dot represents one assay. c, The response of 6 normal and 20 cancer organoids to the drugs that share the same targets. The Z-scores of logIC50 values are shown. Samples are sorted by the average Z-score. NA; not available.
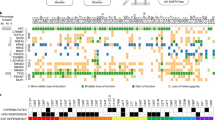
Extended Data Fig. 3 Genetic alterations of CRC organoids.
Genetic mutations in CRC organoids used for HTS (top). Mutations in recurrently mutated genes in CRC (MutSigCV FDR < 0.2 in Pan-Cancer Atlas30) are shown. Chromosomal copy number variations in CRC organoids (bottom). Chromosome states are shown as the log2 ratio of the copy number between the sample and euploid genome.
Extended Data Fig. 4 Gene-drug correlation in organoids.
a, A volcano plot representation of MANOVA incorporating drug sensitivity and genetic mutations. Each dot indicates a genetic mutation-drug pair. Statistically significant pairs (TP53 mutation/nutlin-3 and TP53 mutation/paclitaxel pairs, FDR < 0.25) are highlighted in blue. b, The response of CRC18a (TP53-mutant) and CRC18b (TP53-wild type) to nutlin-3. The organoids are subclones that were derived from the same tumor. Data are shown as mean ± SD. n = 3 c, Capillary-based immunodetection of p53 in CRC18a and CRC18b with or without nutlin-3 treatment. d, IC50 values of EGFR inhibitors and RTK/MAPK pathway mutations in a refined screening condition. The organoids were treated with the indicated drugs from day 1 after plating and cultured without IGF-1 and FGF-2. e, IC50 values of vemurafenib. Each dot represents one organoid line. Samples were sorted by the IC50 value.
Extended Data Fig. 5 Sensitivity of patient-derived organoids to JQ1.
a, Response of normal and cancer organoids to JQ1. Representative images from three technical replicates with similar results. Scale bar, 500 μm. b, Response of organoids derived from tubular adenoma and serrated lesion to JQ1. Representative images from three technical replicates with similar results. Scale bar, 500 μm. c, Response of genetically engineered normal organoids with single (APC) and quadruple (APC, KRAS, TP53 and SMAD4) mutations to JQ1. Representative images from three technical replicates with similar results. Scale bar, 500 μm.
Extended Data Fig. 6 Relationship between drug sensitivity and CIMP.
a, Hierarchical clustering of CRC organoids based using variably methylated probes (probes in CpG island and with an SD of M-value > 3). The CRC organoids were assigned to either CIMP+ or CIMP– based on the cluster membership. b, Association between methylation clusters and consensus molecular subtypes (CMS). The integers indicate the number of samples assigned to each subtype. c, Principal component analysis of the organoid transcriptomes. Each dot represents one organoid line. d, The relationship between the expression levels of the 50 CIMP genes and the responses to the 56 drugs. The expression of the CIMP genes were ranked based on the Spearman’s correlation between the gene expression value and the IC50 value of the drugs, and were summarized as the normalized enrichment score by gene set enrichment analysis. The drugs of which the resistance or sensitivity was significantly associated with the expression of the CIMP genes are highlighted in red (positive NES, FDR < 0.01) or blue (negative NES, FDR < 0.01), respectively. NES, normalized enrichment score. e, Response of normal, CIMP– CRC and CIMP+ CRC organoids treated to paclitaxel. Representative images from three technical replicates with similar results. Scale bar, 500 μm. f, Response of tubular adenoma (Ad3) and serrated lesion (SL3) organoids treated to paclitaxel. Representative images from three technical replicates with similar results. Scale bar, 500 μm.
Extended Data Fig. 8 Response of CRC organoid xenografts to nab-paclitaxel or cetuximab treatment.
a, The growth curves of cetuximab- and vehicle-treated xenografts. Each dot and line indicates one mouse. b, Schedule for treating CRC organoid xenografts with cetuximab (top). Sensitivity of CRC organoid xenografts to cetuximab (bottom). Each dot and line indicates one organoid line. c, The relationship between the sensitivity to cetuximab in vitro and in vivo. Each dot shows one organoid line, and the organoids were colored according to the possession of KRAS or BRAF mutation. d, The growth curves of nab-paclitaxel- and vehicle-treated CRC organoid xenografts. Each dot and line indicates one mouse.
Supplementary information
Source data
Source Data Fig. 1
Statistical source data for Fig. 1.
Source Data Fig. 2
Statistical Source Data for Fig. 2.
Source Data Fig. 3
Uncropped pseudo-gel images for Fig. 3.
Source Data Fig. 3
Statistical source data for Fig. 3.
Source Data Fig. 4
Statistical source data for Fig. 4.
Source Data Fig. 5
Statistical source data for Fig. 5.
Source Data Fig. 5
Uncropped pseudo-gel images for Fig. 5.
Source Data Fig. 6
Statistical source data for Fig. 6.
Source Data Extended Data Fig. 1
Statistical Source Data for Extended Data Fig. 1.
Source Data Extended Data Fig. 2
Statistical source data for Extended Data Fig. 2.
Source Data Extended Data Fig. 3
Statistical source data for Extended Data Fig. 3.
Source Data Extended Data Fig. 4
Statistical source data for Extended Data Fig. 4.
Source Data Extended Data Fig. 4
Uncropped pseudo-gel images for Extended Data Fig. 4c.
Source Data Extended Data Fig. 8
Statistical source data for Extended Data Fig. 8.
Rights and permissions
About this article
Cite this article
Toshimitsu, K., Takano, A., Fujii, M. et al. Organoid screening reveals epigenetic vulnerabilities in human colorectal cancer. Nat Chem Biol 18, 605–614 (2022). https://doi.org/10.1038/s41589-022-00984-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41589-022-00984-x
This article is cited by
-
Gene expression in organoids: an expanding horizon
Biology Direct (2023)
-
Neuroendocrine neoplasms of the lung and gastrointestinal system: convergent biology and a path to better therapies
Nature Reviews Clinical Oncology (2023)
-
Organoids and organs-on-chips: insights into predicting the efficacy of systemic treatment in colorectal cancer
Cell Death Discovery (2023)
-
Combining Endometrial Assembloids and Blastoids to Delineate the Molecular Roadmap of Implantation
Stem Cell Reviews and Reports (2023)
-
Cell–matrix interface regulates dormancy in human colon cancer stem cells
Nature (2022)