Abstract
The Omicron (B.1.1.529) variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was initially identified in November 2021 in South Africa and Botswana, as well as in a sample from a traveller from South Africa in Hong Kong1,2. Since then, Omicron has been detected globally. This variant appears to be at least as infectious as Delta (B.1.617.2), has already caused superspreader events3, and has outcompeted Delta within weeks in several countries and metropolitan areas. Omicron hosts an unprecedented number of mutations in its spike gene and early reports have provided evidence for extensive immune escape and reduced vaccine effectiveness2,4,5,6. Here we investigated the virus-neutralizing and spike protein-binding activity of sera from convalescent, double mRNA-vaccinated, mRNA-boosted, convalescent double-vaccinated and convalescent boosted individuals against wild-type, Beta (B.1.351) and Omicron SARS-CoV-2 isolates and spike proteins. Neutralizing activity of sera from convalescent and double-vaccinated participants was undetectable or very low against Omicron compared with the wild-type virus, whereas neutralizing activity of sera from individuals who had been exposed to spike three or four times through infection and vaccination was maintained, although at significantly reduced levels. Binding to the receptor-binding and N-terminal domains of the Omicron spike protein was reduced compared with binding to the wild type in convalescent unvaccinated individuals, but was mostly retained in vaccinated individuals.
Similar content being viewed by others
Main
SARS-CoV-2 was first detected in Wuhan, China, in late 2019 and has since caused the coronavirus disease 2019 (COVID-19) pandemic. Although SARS-CoV-2 was antigenically relatively stable during its first few months of circulation, the first antigenically distinct variants—Alpha (B.1.1.7), Beta and Gamma (P.1)—emerged in late 2020. Other variants of interest and variants of concern followed. So far, Beta has shown the most antigenic drift in terms of reduction of in vitro neutralization, rivalled only by Mu7 (B.1.621). Delta, which emerged in early 2021, has been the most consequential variant, since it is more infectious than the viruses circulating in the beginning of the pandemic and also partially escapes neutralization in vitro8. Omicron was first detected in South Africa, Botswana and in a traveller from South Africa in Hong Kong1,2. The variant hosts a large number of mutations in its spike protein including at least 15 amino acid changes in the receptor-binding domain (RBD) and extensive changes in the N-terminal domain (NTD). These mutations are predicted to affect most neutralizing antibody epitopes. In addition, Omicron seems to be fit and highly transmissible3 and has spread rapidly across the globe, outcompeting Delta within weeks to become the dominant circulating variant in several countries and urban areas.
Immunity to SARS-CoV-2 in human populations is highly variable and probably differs in individuals with infection induced immunity, double vaccinated individuals, boosted individuals, and individuals with hybrid immunity owing to the combination of infection followed by vaccination. Understanding residual neutralizing and binding activity against highly antigenically distinct viral variants such as Omicron in these distinct groups is essential to gauge the level of protection that a specific community has against infection and mild or severe COVID-19.
Neutralization of Omicron
To address these questions, we determined differences in in vitro neutralizing and binding activity for Omicron (Pango lineage BA.1) compared with other variants in sera from individuals with different levels of immunity. We included samples from individuals who had recovered from SARS-CoV-2 infection (convalescent individuals) (n = 15), individuals vaccinated twice with BNT162b2 (Pfizer–BioNTech mRNA vaccine; n = 10), individuals vaccinated twice with mRNA-1273 (Moderna mRNA vaccine; n = 10), individuals vaccinated three times (boosted) with BNT162b2 (boosted individuals) (n = 10), individuals vaccinated three times with mRNA-1273 (n = 10), convalescent individuals who had received two doses of BNT162b2 (n = 10), convalescent individuals who had received two doses of mRNA-1273 (n = 10), and convalescent individuals who had received three doses of BNT162b2 (n = 10) (Fig. 1a, Extended Data Tables 1, 2). First, we tested the in vitro neutralizing activity of the sera against wild type SARS-CoV-2 (USA-WA1/2020; as a reference for ancestral strains), Beta (as a reference for the most pronounced in vitro escape phenotype) and Omicron (isolated from one of the first cases identified in New York City in late November 2021) (Extended Data Table 3). The neutralization assay that we used is performed with authentic SARS-CoV-2 in a multicycle replication setting in which serum and antibody are present at all times, similar to the situation in a seropositive individual. Across all 85 samples, the reduction in neutralization of Omicron compared with wild type was greater than 14.5-fold (the actual fold reduction could not be calculated since many samples were below the limit of detection) (Fig. 1b). By comparison, there was a fourfold reduction of Beta neutralization compared with wild type in the same sample set. Indeed, 16.5% of samples did not show neutralizing activity against Omicron. Comparing the different groups, we noted that convalescent individuals had lower neutralizing antibody titres against wild-type and Beta, with the majority (73.3%) of samples exhibiting no measurable neutralizing activity for Omicron (Fig. 1c). Sera from individuals double vaccinated with either BNT162b2 or mRNA-1273 showed a reduction in neutralization of Omicron compared with wild-type of more than 23-fold or 42-fold, respectively (Fig. 1d, e). However, most individuals showed low but detectable neutralizing activity against Omicron. Boosted individuals showed smaller differences in neutralizing activity with a 7.5-fold reduction in neutralization of Omicron compared with wild type for BNT162b2-boosted individuals and a 16.7-fold reduction in mRNA-1273-boosted individuals (Fig. 1f, g). Of note, the smaller fold change and higher initial neutralization titres against wild-type virus led to substantial neutralizing activity against Omicron in sera from boosted individuals. Convalescent individuals who received 2 BNT162b2, 2 mRNA-1272 or 3 BNT162b2 vaccine doses showed reductions in Omicron neutralization compared with wild type of 14-fold, 11-fold and 13-fold, respectively (Fig. 1h–j). However, all individuals in these groups maintained relatively robust neutralization activity against Omicron. These data indicate that convalescent individuals greatly benefit from vaccination, an observation that is of considerable importance to public health.
a, Overview of different exposure groups from whom samples were obtained. Further details are provided in Supplementary Tables 1, 2. b, Absolute titres (left) and fold reduction (right) for neutralization by all serum samples of wild-type (WA1 (WT)), Beta and Omicron SARS-CoV-2 variants. c–j, Neutralization of wild-type (WA1 (WT)), Beta and Omicron SARS-CoV-2 variants by sera from convalescent individuals (c), after two BNT162b2 vaccinations (d), after two mRNA-1273 vaccinations (e), after three BNT162b2 vaccinations (f), after three mRNA-1273 vaccinations (g), from convalescent individuals after two BNT162b2 vaccinations (h), from convalescent individuals after two mRNA-1273 vaccinations (i) and from convalescent individuals after three BNT162b2 vaccinations (j). One-way ANOVA with Tukey’s multiple comparisons test was used to compare the neutralization titres; P < 0.05 indicated. n = 85 (b), 15 (c), or 10 (d–j) samples. The dotted line represents the limit of detection (10); negative samples were assigned half the limit of detection (5). Each dot represents a biological replicate and the assays were performed once. Fold change is defined as the geometric mean fold change.
Binding to RBD, NTD and spike
In vitro neutralization is a key function of the antibody response; however, antibody binding—even in the absence of detectable neutralizing activity—can also provide protection through Fc-mediated effector functions. This type of protection has been described in detail for influenza virus9,10,11, but binding antibody titres also represent a correlate of protection from SARS-CoV-212,13. Furthermore, retention of binding to a highly mutated RBD or NTD, even if it is reduced, indicates that cognate B cells are present. These B cells could probably be rapidly recalled during infection with variants or by variant-specific vaccination, producing a strong plasmablast response leading to rapid control of viral spread. In addition, B cells with low-affinity binding to antigenically drifted variant proteins may enter lymph nodes and engage in germinal centre reactions, leading to production of antibodies that may regain neutralizing activity through affinity maturation.
To investigate the reduction in binding, we expressed a recombinant Omicron RBD and compared binding of sera to this RBD with binding to wild-type (Wuhan-1) and Beta RBD (Fig. 2a). Overall, the reduction in binding to Omicron RBD compared with wild-type was much less pronounced than the reduction in neutralization (Fig. 2b). However, this reduction in binding to Omicron RBD was significantly greater than the reduction in binding to Beta RBD observed here and previously8. This reduced binding to Omicron RBD was most pronounced for convalescent individuals (Fig. 2c), with a difference of more than 7.5-fold compared with wild-type RBD and undetectable reactivity by enzyme-linked immunosorbent assay (ELISA) in two-thirds of the convalescent individuals who were infected early in the pandemic before the circulation of viral variants of concern. In all other groups, there was a smaller difference in binding to Omicron RBD compared with wild type, with reductions ranging from 2.9-fold in individuals who had received two vaccinations with mRNA-1273 to 1.5-fold in individuals boosted with BNT162b2 (Fig. 2d–j).
a, A model of the Omicron spike protein in complex with the angiotensin converting enzyme 2 (ACE2) receptor with Omicron-specific mutations indicated. The model is based on Protein Data Bank 6M0J25 and 7C2L15 and the figure was made in PyMOL. b, Absolute titres (left) and fold reduction (right) in binding to wild-type, Beta and Omicron spike RBDs for all serum samples. c–j, Binding to wild-type, Beta and Omicron RBDs by sera from convalescent individuals (c), after two BNT162b2 vaccinations (d), after two mRNA-1273 vaccinations (e), after three BNT162b2 vaccinations (f), after three mRNA-1273 vaccinations (g), from convalescent individuals after two BNT162b2 vaccinations (h), from convalescent individuals after two mRNA-1273 vaccinations (i) and from convalescent individuals after three BNT162b2 vaccinations (j). One-way ANOVA with Tukey’s multiple comparisons test was used to compare the binding, except in b, d, where a mixed-effects model was used owing to a missing data point; P < 0.05 indicated. n = 85 (b), 15 (c), or 10 (d–j) samples, except in d, where one data point for Beta is missing. The dotted line represents the limit of detection (10), negative samples were assigned half the limit of detection (5). Each dot represents a biological replicate and the assays were performed twice. Fold change is defined as the geometric mean fold change.
In addition to the RBD, the spike NTD is a prime target for B cells following COVID-19 mRNA vaccination14. The NTD also hosts neutralizing epitopes inside and outside of the immunodominant ‘super site’15,16,17,18. The NTD of Omicron spike carries a large number of amino acid substitutions, three deletions and one three-amino-acid-long insertion (Fig. 2a, Extended Data Table 4); collectively, these mutations are predicted to substantially change the neutralizing epitopes inside and outside the super site. To determine whether infection-induced and vaccine-induced antibodies retain binding to the Omicron NTD, we expressed both wild-type and variant NTDs and probed them by ELISA using the same 85 samples tested for neutralization. Surprisingly, the sera retained binding to the Omicron NTD, with relatively minor reductions (maximum 1.9-fold) compared with the wild type, suggesting that binding to the super site was retained (for example, at lower affinity), or the presence of a large number of unchanged epitopes within this domain but outside the super site (Fig. 3).
a, Absolute titres (left) and fold reduction (right) in binding to wild-type and Omicron NTDs for all serum samples. b–i, Binding to wild-type and Omicron spike NTDs by sera from convalescent individuals (b), after two BNT162b2 vaccinations (c), after two mRNA-1273 vaccinations (d), after three BNT162b2 vaccinations (e), after three mRNA-1273 vaccinations (f), from convalescent individuals after two BNT162b2 vaccinations (g), from convalescent individuals after two mRNA-1273 vaccinations (h) and from convalescent individuals after three BNT162b2 vaccinations (i). Student’s t-test was used to compare the binding; P < 0.05 indicated. n = 85 (a), 15 (b), or 10 (c–i) samples. The dotted line represents the limit of detection (10), negative samples were assigned half the limit of detection (5). Each dot represents a biological replicate and the assays were performed once. Fold change is defined as the geometric mean fold change.
Finally, we also measured antibody binding to the wild-type (Wuhan-1), Beta and Omicron spike protein ectodomains. Overall, there was a 5.2-fold decrease in the binding to Omicron spike and a 2.7-fold decrease in binding to Beta spike, compared with wild-type spike (Fig. 4a). Sera from all convalescent individuals bound to Omicron spike and there was no significant difference in binding between Beta and Omicron spike, with some low-titre sera showing better binding to Omicron spike than to Beta spike (Fig. 4b). However, in sera from vaccinated individuals and from convalescent plus vaccinated individuals, which typically showed strong binding to spike protein, the difference in binding to Omicron spike compared with wild type (ranging from 4.4- to 8.3-fold) was consistently larger than for Beta (ranging from 2- to 3.8-fold) (Fig. 4c–i). Of note, all proteins used were histidine-tagged, to enable control of the coating concentration. Probing with an anti-His antibody showed that the variant spike proteins exhibited similar binding to the ELISA plates (Extended Data Fig. 1).
a, Absolute titres (left) and fold reduction (right) in binding to wild-type and Omicron spike protein ectodomain for all serum samples. b–i, Binding to wild-type and Omicron spike protein ectodomain by sera from convalescent individuals (b), after two BNT162b2 vaccinations (c), after two mRNA-1273 vaccinations (d), after three BNT162b2 vaccinations (e), after three mRNA-1273 vaccinations (f), from convalescent individuals after two BNT162b2 vaccinations (g), from convalescent individuals after two mRNA-1273 vaccinations (h) and from convalescent individuals after three BNT162b2 vaccinations (i). One-way ANOVA with Tukey’s multiple comparisons test was used to compare the binding; P < 0.05 indicated. n = 85 (a), 15 (b), or 10 (c–i) samples. The dotted line represents the limit of detection (10), negative samples were assigned half the limit of detection (5). Each dot represents a biological replicate and the assays were performed once. Fold change is defined as the geometric mean fold change.
Discussion
The data presented here align well with initial reports on the impact of Omicron on in vitro neutralizing activity of serum from convalescent and vaccinated individuals and expand on these initial reports by including subcohorts with divergent histories of SARS-CoV-2 exposure, including infection-induced, primary vaccination-induced, booster vaccination-induced and hybrid immunity2,5,6. We found that neutralizing activity against Omicron is weakest in unvaccinated, convalescent individuals and in naive individuals who acquired immunity through two mRNA COVID-19 vaccine doses. Our findings support recent reports describing significantly reduced protection from reinfection19 and almost non-existent vaccine effectiveness against symptomatic disease after two BNT162b2 vaccinations4. However, boosted individuals have shown—at least within a short time after a booster dose—significant protection against symptomatic disease4 in the range of 75%. Although it is unclear how long this protection lasts, we observed neutralizing titres similar to those in boosted individuals in convalescent vaccinated individuals, suggesting that those individuals may experience significant protection. With regard to neutralization, we made some interesting additional observations. It has been reported that in some vaccine effectiveness studies protection from infection is better maintained after mRNA-1273 vaccination as compared with BNT162b2 vaccination20. We did not observe obvious differences in residual Omicron-neutralizing activity between the two vaccines in naive individuals who were vaccinated two or three times, but there was a trend towards higher titres in convalescent individuals after mRNA-1273 vaccination compared with BNT162b2 vaccination. However, the failure to observe differences may be owing to the small sample size per group, which is a major limitation of our study. Further, individuals with low neutralizing activity against wild-type SARS-CoV-2 often showed neutralization against Omicron only at the highest tested concentration, resulting in titres just above the limit of detection. Whether this was an artefact of the assay or bona fide neutralization is unclear. It is currently unclear which epitopes are targeted by the antibodies responsible for the residual neutralizing activity against Omicron. On the basis of recent reports with data for monoclonal antibodies, it is likely that most of the residual activity comes from antibodies binding to epitopes outside the receptor binding motif (sites IV and V), but rare antibodies binding to sites I and II (which completely or partially overlap with the RBD) may also contribute21,22.
This study also provides insights into Omicron RBD-, NTD- and spike-specific binding changes. Compared with the changes in neutralizing activities, binding was relatively well preserved, especially against the NTD in general and against the RBD in vaccinated, boosted and convalescent vaccinated individuals. Notably, reductions in binding to the full Omicron spike ectodomain were somewhat larger than against the RBD and the NTD, despite there being fewer mutations outside of these two domains. A possible explanation for this finding could be that more epitopes—and more conserved epitopes—are accessible in recombinant RBD and NTD, whereas it is mostly the mutated epitopes that are accessible in the full-length ectodomain. Conversely, in some instances, sera from convalescent individuals with low titres exhibited greater reactivity to Omicron spike than to Beta spike. Although differences at such low levels of binding should not be over-interpreted, this phenomenon could be driven by slight differences in spike conformation, which could lead to exposure of additional epitopes owing either to differences in sequence or differences in the spike preparations. However, no such phenomenon was seen in the other groups that had higher titres against wild-type spike. Based on conservation, we assume that most of the cross-reactive anti-spike antibodies do in fact bind to the S2 subunit14.
It is conceivable that these binding antibodies—which frequently have non-neutralizing phenotypes in cell culture—contribute to protection from disease, as has been seen for other viral infections9,10,11. In concert with T cell-based immunity23, these non-neutralizing but binding antibodies—which frequently target S2 but also the RBD and NTD14—could be responsible for the protection from severe disease that has been observed against Omicron in individuals with pre-existing immunity. In addition, the presence of strong binding antibodies suggests that, although some antibodies may have lost affinity for the drifted epitopes, B cells may be recalled when encountering Omicron spike through infection or vaccination. This could lead to a strong anamnestic response, which could have a positive effect against COVID-19 progression. It could also lead to the recruitment of these B cells into germinal centres for further affinity maturation resulting in potent, high-affinity neutralizing antibodies against Omicron24. Our data add to the growing body of evidence suggesting that Omicron-specific vaccines are urgently needed.
Methods
Human serum samples
Convalescent and post-vaccine sera were collected from participants in the longitudinal observational PARIS (Protection Associated with Rapid Immunity to SARS-CoV-2) study8,26. This cohort follows health care workers longitudinally since April 2020. The study was reviewed and approved by the Mount Sinai Hospital Institutional Review Board (IRB-20-03374). All participants signed written consent forms prior to sample and data collection. All participants provided permission for sample banking and sharing. Serum samples from the PARIS cohort are unique to this study and are not publicly available.
For the antigenic characterization of the Omicron variant, we selected 85 serum samples from 54 participants. Twenty out of 54 participants were seronegative prior to vaccination while 34/54 had COVID-19 prior to vaccination (see Supplementary Tables 1, 2 for demographics and vaccine information). All participants with pre-vaccination immunity were infected in 2020 when only ancestral SARS-CoV-2 strains circulated in the New York metropolitan area. Convalescent samples (n = 15) were obtained within three months of SARS-CoV-2 infection (average: 58 days, range: 23–87 days) whereas the post-vaccination samples were collected on average 23 days (range: 14–39 days) after the second dose (n = 40, 20 Pfizer 2× and 20 Moderna 2×) or 19 days (range: 14–33 days) after the third booster (n = 30, 20 Pfizer 3× and 10 Moderna 3×) vaccine dose.
Cells
Vero.E6 cells expressing TMPRSS2 (BPS Biosciences, catalogue (cat.) no. 78081) were cultured in Dulbecco’s modified Eagles medium (DMEM; Corning, cat. no. 10-013-CV) containing 10% heat-inactivated fetal bovine serum (FBS; GeminiBio, cat. no. 100–106) and 1% minimum essential medium (MEM) amino acids solution (Gibco, cat. no. 11130051), supplemented with 100 U ml−1 penicillin and 100 μg ml−1 streptomycin (Gibco, cat. no. 15140122), 100 μg ml−1 normocin (InvivoGen, cat. no. ant-nr), and 3 μg ml−1 puromycin (InvivoGen, cat. no. ant-pr). FreeStyle 293-F cells (Gibco, cat. no. R79007) were cultured in ESF-SFM medium (Expression Systems, cat. no. 98-001) supplemented with 100 U ml−1 penicillin and 100 μg ml−1 streptomycin (Gibco, cat. no. 15140122). Expi293F cells (Gibco, cat. no. A14527) were cultured in Expi293 Expression Medium (Gibco, cat. no. A1435102) supplemented with 100 U ml−1 penicillin and 100 μg ml−1 streptomycin (Gibco, cat. no. 15140122). Cell lines were authenticated by supplier. No other authentication at the laboratory level was performed. Cell lines are tested on a regular basis for mycoplasma and are mycoplasma-free.
Selection and culture of replication competent SARS-CoV-2 isolates
The Mount Sinai Pathogen Surveillance program (IRB approved, HS no. 13-00981) actively screens nasopharyngeal swab specimens from patients seeking care at the Mount Sinai Health System for emerging viral variants. After completion of the diagnostics, de-identified biospecimen were sequenced either using an established complete virus genome sequencing approach27 (for example, Beta isolate USA/NY-MSHSPSP-PV27007/2021, EPI_ISL_1708926) or based on the spike S1 mutational profile determined by Spike-ID (Omicron, manuscript in preparation). The B.1.1.529 isolate USA/NY-MSHSPSP-PV44488/2021 (BA.1, EPI_ISL_7908059) represents one of the first cases diagnosed in New York State (female, age bracket: 30–40 years, mild COVID-19 symptoms, vaccinated and boosted) in late November 2021. The SARS-CoV-2 isolate USA-WA1/2020 was used as wild-type reference (BEI Resources, NR‐52281). Supplementary Table 3 summarizes the amino acid substitutions, insertions and deletions in the spike region of each of the three viral isolates.
Viruses were grown by adding 200 μl of viral transport media from the nasopharyngeal swabs to Vero.E6-TMPRSS2 cells in culture media supplemented with 0.5 μg ml−1 amphotericin B (Gibco, cat. no. 15290-018). Cytopathic effects appeared within 4–6 days at which point the culture supernatants were clarified by centrifugation at 4,000g for 5 min. Expanded viral stocks used were sequence-verified and titred by the 50% tissue culture infectious dose (TCID50) method on Vero.E6-TMPRSS2 cells before use in microneutralization assays.
Generation of recombinant variant RBD, NTD and spike proteins
The recombinant RBD proteins were produced using Expi293F cells (Life Technologies). The coding sequences for the proteins were cloned into a mammalian expression vector, pCAGGS as described earlier28,29 and purified after transient transfections with each respective plasmid. Six-hundred-million Expi293F cells were transfected using the ExpiFectamine 293 Transfection Kit and purified DNA. Supernatants were collected on day four post transfection, centrifuged at 4,000g for 20 min and finally filtered using a 0.22-µm filter. Ni-nitrilotriacetic acid (Ni-NTA) agarose (Qiagen) was used to purify the proteins via gravity flow and proteins were eluted as previously described28,29. The buffer was exchanged using Amicon centrifugal units (EMD Millipore) and all recombinant proteins were finally re-suspended in phosphate buffered saline (PBS). Proteins were also run on a sodium dodecyl sulphate (SDS) polyacrylamide gels (5–20% gradient; Bio-Rad) to check for purity30,31. The NTD protein constructs (residues 1–306) were cloned into pVRC8400 expression vector between SalI and NotI endonuclease restriction sites yielding an NTD with a human rhinovirus (HRV) 3C protease-cleavable C-terminal hexahistidine and streptavidin-binding protein tags. The NTDs were transiently expressed in FreeStyle 293-F cells. Four days after transfection, supernatants were collected by centrifugation and further purified using immobilized metal affinity chromatography (IMAC) with cobalt-TALON resin (Takara) followed by a Superdex 200 Increase 10/300 GL size exclusion column (GE Healthcare). Spike proteins were expressed as described before8.
Enzyme-linked immunosorbent assay
Antibody titres in sera from convalescent individuals and vaccinees were measured by a research-grade ELISA using recombinant versions of the RBD, NTD and spike of wild-type SARS-CoV-2 as well as B.1.351 (Beta) and B.1.1.529 (Omicron) (see Supplementary Table 4 for specific substitutions in each variant). All samples were analysed in a blinded manner. In brief, 96-well microtitre plates (Corning, cat. no. 353227) were coated with 50 μl per well of recombinant protein (2 μg ml−1) overnight at 4 °C. Plates were washed 3 times with phosphate-buffered saline (PBS; Gibco, cat. no. 10010-031) supplemented with 0.1% Tween-20 (PBS-T; Fisher Scientific ref. 202666) using an automatic plate washer (BioTek 405TS microplate washer). For blocking, PBS-T containing 3% milk powder (American Bio, cat. no. AB1010901000) was used. After 1 h of incubation at room temperature, blocking solution was removed and initial dilutions (1:100) of heat-inactivated sera (in PBS-T 1%-milk powder) were added to the plates, followed by twofold serial dilutions. After 2 h of incubation, plates were washed three times with PBS-T and 50 μl per well of the pre-diluted secondary anti-human IgG (Fab-specific) horseradish peroxidase (HRP) antibody (produced in goat; Sigma-Aldrich, cat. no. A0293, RRID: AB_257875) diluted 1:3,000 in PBS-T containing 1% milk powder were added. After 1 h of incubation at room temperature, plates were washed three times with PBS-T and SigmaFast O-phenylenediamine dihydrochloride (Sigmafast OPD; Sigma-Aldrich, Ref. P9187-50SET) was added (100 μl per well) for 10 min, followed by addition of 50 μl per well of 3 M hydrochloric acid (Thermo Fisher, Ref. S25856) to stop the reaction. Optical density was measured at a wavelength of 490 nm using a plate reader (BioTek, SYNERGY H1 microplate reader). The area under the curve (AUC) values were calculated and plotted using Prism 9 software (GraphPad).
SARS-CoV-2 multi-cycle microneutralization assay
Sera from vaccinees were used to assess the neutralization of wild type (WA1), B.1.351 (Beta) and B.1.1.529 (Omicron) SARS-CoV-2 isolates (Supplementary Table 3). All procedures were performed in a biosafety level 3 (BSL-3) facility at the Icahn School of Medicine at Mount Sinai following standard safety guidelines. Vero.E6-TMPRSS2 cells were seeded in 96-well high binding cell culture plates (Costar, cat. no. 07620009) at a density of 20,000 cells per well in complete Dulbecco’s modified Eagle medium (cDMEM) one day before the infection. Heat inactivated serum samples (56 °C for 1 h) were serially diluted (threefold) in minimum essential media (MEM; Gibco, cat. no. 11430-030) supplemented with 2 mM l-glutamine (Gibco, cat. no. 25030081), 0.1% sodium bicarbonate (w/v) (HyClone, cat. no. SH30033.01), 10 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES; Gibco, cat. no. 15630080), 100 U ml−1 penicillin, 100 μg ml−1 streptomycin (Gibco, cat. no. 15140122) and 0.2% bovine serum albumin (BSA) (MP Biomedicals, cat. no. 810063) starting at 1:10. Remdesivir (Medkoo Bioscience inc., cat. no. 329511) was included as a control to monitor assay variation. Serially diluted sera were incubated with 10,000 TCID50 of WT USA-WA1/2020 SARS-CoV-2, MSHSPSP-PV27007/2021 (B.1.351, Beta) or USA/NY-MSHSPSP-PV44488/2021 (B.1.1.529, Omicron) for one hour at room temperature, followed by the transfer of 120 μl of the virus–serum mix to Vero.E6-TMPRSS2 plates. Infection proceeded for 1 h at 37 °C and inoculum was removed. One-hundred microlitres per well of the corresponding antibody dilutions plus 100 μl per well of infection media supplemented with 2% fetal bovine serum (FBS; Gibco, cat. no. 10082-147) were added to the cells. Plates were incubated for 48 h at 37 °C followed by fixation overnight at 4 °C in 200 μl per well of a 10% formaldehyde solution. For staining of the nucleoprotein, formaldehyde solution was removed, and cells were washed with PBS (pH 7.4) (Gibco, cat. no. 10010-031) and permeabilized by adding 150 μl per well of PBS with 0.1% Triton X-100 (Fisher Bioreagents, cat. no. BP151-100) for 15 min at room temperature. Permeabilization solution was removed, plates were washed with 200 μl per well of PBS (Gibco, cat. no. 10010-031) twice and blocked with PBS, 3% BSA for 1 h at room temperature. Blocking solution was removed and 100 μl per well of biotinylated monoclonal antibody 1C7C732, a mouse anti-SARS nucleoprotein monoclonal antibody generated at the Center for Therapeutic Antibody Development at The Icahn School of Medicine at Mount Sinai ISMMS (Millipore Sigma, cat. no. ZMS1075) at a concentration of 1μg ml−1 in PBS, 1% BSA was added for 1 h at room temperature. Cells were washed with 200 μl per well of PBS twice and 100 μl per well of HRP-conjugated streptavidin (Thermo Fisher Scientific) diluted in PBS, 1% BSA were added at a 1:2,000 dilution for 1 h at room temperature. Cells were washed twice with PBS, and 100 μl per well of O-phenylenediamine dihydrochloride (Sigmafast OPD; Sigma-Aldrich) were added for 10 min at room temperature, followed by addition of 50 μl per well of a 3 M HCl solution (Thermo Fisher Scientific). Optical density (OD) was measured (490 nm) using a microplate reader (Synergy H1; Biotek). Analysis was performed using Prism 7 software (GraphPad). After subtraction of background and calculation of the percentage of neutralization with respect to the ‘virus-only’ control, a nonlinear regression curve fit analysis was performed to calculate the 50% inhibitory dilution (ID50), with top and bottom constraints set to 100% and 0% respectively. All samples were analysed in a blinded manner.
Statistics
A one-way ANOVA with Tukey’s multiple comparisons test was used to compare the neutralization and RBD-binding antibody titres. The exception is the 2× BNT162b2 RBD ELISA group, where a mixed-effects model had to be used owing to a missing data point. A Student’s t-test was used for comparing wild-type and Omicron NTD-binding data. Statistical analyses were performed using Prism 9 software (GraphPad).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this paper.
Data availability
Complete genome sequences for the viral isolates cultured from nasal swabs (B.1.351 and B.1.1.529) were deposited to GISAID. Source data are provided with this paper.
References
Gu, H. et al. Probable transmission of SARS-CoV-2 Omicron variant in quarantine hotel, Hong Kong, China, November 2021. Emerg. Infect. Dis. 28, 460–462 (2021).
Cele, S. et al. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature https://doi.org/10.1038/s41586-021-04387-1 (2021).
Brandal, L. T. et al. Outbreak caused by the SARS-CoV-2 Omicron variant in Norway, November to December 2021. Eurosurveillance 26, 2101147 (2021).
Andrews, N. et al. Effectiveness of COVID-19 vaccines against the Omicron (B.1.1.529) variant of concern. Preprint at https://doi.org/10.1101/2021.12.14.21267615 (2021).
Wilhelm, A. et al. Reduced neutralization of SARS-CoV-2 Omicron variant by vaccine sera and monoclonal antibodies. Preprint at https://doi.org/10.1101/2021.12.07.21267432 (2021).
Rössler, A., Riepler, L., Bante, D., Laer, D. V. & Kimpel, J. SARS-CoV-2 Omicron variant neutralization in serum from vaccinated and convalescent persons. N. Eng. J. Med. https://doi.org/10.1056/NEJMc2119236 (2022).
Uriu, K. et al. Neutralization of the SARS-CoV-2 Mu variant by convalescent and vaccine serum. N. Engl. J. Med. 385, 2397–2399 (2021).
Carreño, J. M. et al. Evidence for retained spike-binding and neutralizing activity against emerging SARS-CoV-2 variants in serum of COVID-19 mRNA vaccine recipients. eBioMedicine 73, 103626 (2021).
Dilillo, D. J., Tan, G. S., Palese, P. & Ravetch, J. V. Broadly neutralizing hemagglutinin stalk-specific antibodies require FcγR interactions for protection against influenza virus in vivo. Nat. Med. 20, 143–151 (2014).
Asthagiri Arunkumar, G. et al. Broadly cross-reactive, nonneutralizing antibodies against influenza B virus hemagglutinin demonstrate effector function-dependent protection against lethal viral challenge in mice. J. Virol. 93, e01696–18 (2019).
Ng, S. et al. Novel correlates of protection against pandemic H1N1 influenza A virus infection. Nat. Med. 25, 962–967 (2019).
Gilbert, P. B. et al. Immune correlates analysis of the mRNA-1273 COVID-19 vaccine efficacy clinical trial. Science eab3435 (2021).
Earle, K. A. et al. Evidence for antibody as a protective correlate for COVID-19 vaccines. Vaccine 39, 4423–4428 (2021).
Amanat, F. et al. SARS-CoV-2 mRNA vaccination induces functionally diverse antibodies to NTD, RBD, and S2. Cell 184, 3936–3948.e10 (2021).
Chi, X. et al. A neutralizing human antibody binds to the N-terminal domain of the spike protein of SARS-CoV-2. Science 369, 650–655 (2020).
Voss, W. N. et al. Prevalent, protective, and convergent IgG recognition of SARS-CoV-2 non-RBD spike epitopes. Science 372, 1108–1112 (2021).
Cerutti, G. et al. Potent SARS-CoV-2 neutralizing antibodies directed against spike N-terminal domain target a single supersite. Cell Host Microbe 29, 819–833.e817 (2021).
Rosa, A. et al. SARS-CoV-2 can recruit a heme metabolite to evade antibody immunity. Sci. Adv. 7, eabg7607 (2021).
Pulliam, J. R. C. et al. Increased risk of SARS-CoV-2 reinfection associated with emergence of the Omicron variant in South Africa. Preprint at https://doi.org/10.1101/2021.11.11.21266068 (2021).
Rosenberg, E. S. et al. Covid-19 vaccine effectiveness in New York state. N. Engl. J. Med. 386, 116–127 (2021).
Cameroni, E. et al. Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shift. Nature https://doi.org/10.1038/s41586-021-04386-2 (2021).
Liu, L. et al. Striking antibody evasion manifested by the Omicron variant of SARS-CoV-2. Nature https://doi.org/10.1038/s41586-021-04388-0 (2021).
GeurtsvanKessel, C. H. et al. Divergent SARS CoV-2 Omicron-specific T- and B-cell responses in COVID-19 vaccine recipients. Preprint at https://doi.org/10.1101/2021.12.27.21268416 (2021).
Turner, J. S. et al. SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses. Nature 596, 109–113 (2021).
Lan, J. et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature 581, 215–220 (2020).
Krammer, F. et al. Antibody responses in seropositive persons after a single dose of SARS-CoV-2 mRNA vaccine. N. Engl. J. Med. 384, 1372–1374 (2021).
Gonzalez-Reiche, A. S. et al. Introductions and early spread of SARS-CoV-2 in the New York City area. Science 369, 297–301 (2020).
Amanat, F. et al. A serological assay to detect SARS-CoV-2 seroconversion in humans. Nat. Med. 26, 1033–1036 (2020).
Stadlbauer, D. et al. SARS-CoV-2 seroconversion in humans: a detailed protocol for a serological assay, antigen production, and test setup. Curr. Protoc. Microbiol. 57, e100 (2020).
Margine, I., Palese, P. & Krammer, F. Expression of functional recombinant hemagglutinin and neuraminidase proteins from the novel H7N9 influenza virus using the baculovirus expression system. J. Vis. Exp. 81, e51112 (2013).
Amanat, F. et al. Antibodies to the glycoprotein GP2 subunit cross-react between old and new world arenaviruses. mSphere 3, e00189–18 (2018).
Amanat, F. et al. An in vitro microneutralization assay for SARS-CoV-2 serology and drug screening. Curr. Protoc. Microbiol. 58, e108 (2020).
Acknowledgements
We thank the study participants for their generosity and willingness to participate in longitudinal COVID-19 research studies. We thank the Rapid Response Laboratories and the Molecular Microbiology Laboratory of the Mount Sinai Health System for their assistance in the expeditious transfer of SARS-CoV-2 positive diagnostic specimen; R. A. Albrecht for oversight of the conventional BSL3 biocontainment facility; J. Kimpel and D. von Laer for sharing B.1.1.529 virus isolates (even though they could not be included in this work); P. Palese, C. Cordon-Cardo, D. Charney, D. Reich and K. Davis for their leadership and support throughout the COVID-19 pandemic; and D. Caughey for expert administrative assistance. This work is part of the PARIS/SPARTA studies funded by the NIAID Collaborative Influenza Vaccine Innovation Centers (CIVIC) contract 75N93019C00051. In addition, this work was also partially funded by the NIAID Centers of Excellence for Influenza Research and Response (CEIRR) contract and 75N93021C00014 by anonymous donors. The Mount Sinai Pathogen Surveillance Program is supported by institutional School of Medicine and Hospital funds. This work is part of the NIAID SARS-CoV-2 Assessment of Viral Evolution (SAVE) program.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: J.M.C., H.A., E.M.S., G.B., H.v.B., V.S. and F.K. Methodology: J.M.C., H.A., D.C.A. and A.S.G.-R. Investigation: J.M.C., H.A., J.T., G.S., A.J.R., H.K., L.A.S., J.J.C., D.C.A., D.A.B., A.S.G.-R., N.D. and V.V. and the PSP-PARIS Study Group. Visualization: G.B. and F.K. Funding acquisition: V.S., H.v.B. and F.K. Project administration: K.S., D.N.S., E.M.S., G.B., H.v.B., V.S. and F.K. Supervision: J.M.C., D.N.S., E.M.S., G.B., H.v.B., V.S. and F.K. Writing, first draft: F.K. Writing, review and editing: J.M.C., H.A., J.T., G.S., A.J.R., H.K., L.A.S., J.J.C., D.C.A., D.A.B., A.S.G.-R., N.D., V.V., PSP-PARIS Study Group, K.S., D.N.S., E.M.S., G.B., H.v.B., V.S. and F.K.
Corresponding authors
Ethics declarations
Competing interests
The Icahn School of Medicine at Mount Sinai has filed patent applications relating to SARS-CoV-2 serological assays (US provisional application numbers: 62/994,252, 63/018,457, 63/020,503 and 63/024,436) and NDV-based SARS-CoV-2 vaccines (US provisional application number: 63/251,020) which list F.K. as co-inventor. V.S. is also listed on the serological assay patent application as co-inventor. Patent applications were submitted by the Icahn School of Medicine at Mount Sinai. Mount Sinai has spun out a company, Kantaro, to market serological tests for SARS-CoV-2. F.K. has consulted for Merck and Pfizer (before 2020), and is currently consulting for Pfizer, Third Rock Ventures, Seqirus and Avimex. The F.K. laboratory is also collaborating with Pfizer on animal models of SARS-CoV-2.
Peer review
Peer review information
Nature thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
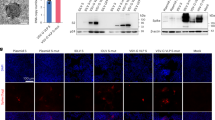
Extended Data Fig. 1 ELISA coating control data.
All recombinant proteins used were his tagged which allows to control for coating efficiency by using an anti-his antibody. A shows endpoint titers of an anti-his mouse antibody to wild type, B.1.351 and B.1.1.529 spike. B shows the same for RBD. C shows binding of the anti-his antibody to NTDs from wild type and B.1.1529. D–F shows the same graphed as AUC. The assays were performed once. Data shown is based on three technical replicates.
Supplementary information
Rights and permissions
About this article
Cite this article
Carreño, J.M., Alshammary, H., Tcheou, J. et al. Activity of convalescent and vaccine serum against SARS-CoV-2 Omicron. Nature 602, 682–688 (2022). https://doi.org/10.1038/s41586-022-04399-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-022-04399-5
This article is cited by
-
Immunogenicity and protective efficacy of a co-formulated two-in-one inactivated whole virus particle COVID-19/influenza vaccine
Scientific Reports (2024)
-
A sustainable approach to universal metabolic cancer diagnosis
Nature Sustainability (2024)
-
Aptamers targeting SARS-CoV-2 nucleocapsid protein exhibit potential anti pan-coronavirus activity
Signal Transduction and Targeted Therapy (2024)
-
An ancestral SARS-CoV-2 vaccine induces anti-Omicron variants antibodies by hypermutation
Nature Communications (2024)
-
Modelling optimal lockdowns with waning immunity
Economic Theory (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.