Abstract
Body-mass index (BMI) has increased steadily in most countries in parallel with a rise in the proportion of the population who live in cities1,2. This has led to a widely reported view that urbanization is one of the most important drivers of the global rise in obesity3,4,5,6. Here we use 2,009 population-based studies, with measurements of height and weight in more than 112 million adults, to report national, regional and global trends in mean BMI segregated by place of residence (a rural or urban area) from 1985 to 2017. We show that, contrary to the dominant paradigm, more than 55% of the global rise in mean BMI from 1985 to 2017—and more than 80% in some low- and middle-income regions—was due to increases in BMI in rural areas. This large contribution stems from the fact that, with the exception of women in sub-Saharan Africa, BMI is increasing at the same rate or faster in rural areas than in cities in low- and middle-income regions. These trends have in turn resulted in a closing—and in some countries reversal—of the gap in BMI between urban and rural areas in low- and middle-income countries, especially for women. In high-income and industrialized countries, we noted a persistently higher rural BMI, especially for women. There is an urgent need for an integrated approach to rural nutrition that enhances financial and physical access to healthy foods, to avoid replacing the rural undernutrition disadvantage in poor countries with a more general malnutrition disadvantage that entails excessive consumption of low-quality calories.
Similar content being viewed by others
Main
Being underweight or overweight can lead to adverse health outcomes. BMI—a measure of underweight and overweight—is rising in most countries2. It is commonly stated that urbanization is one of the most important drivers of the worldwide rise in BMI because diet and lifestyle in cities lead to adiposity3,4,5,6. However, such statements are typically based on cross-sectional comparisons in one or a small number of countries. Only a few studies have analysed how BMI is changing over time in rural and urban areas. The majority have been in one country, over short durations, and/or in one sex and narrow age groups. The few studies that covered more than one country7,8,9,10,11,12 used at most a few dozen data sources and hence could not systematically estimate trends, and focused primarily on women of child-bearing age.
Data on how BMI in rural and urban populations is changing are needed to plan interventions that address underweight and overweight. Here, we report on mean BMI in rural and urban areas of 200 countries and territories from 1985 to 2017. We used 2,009 population-based studies of human anthropometry conducted in 190 countries (Extended Data Fig. 1), with measurements of height and weight in more than 112 million adults aged 18 years and older. We excluded data based on self-reported height and weight because they are subject to bias. For each sex, we used a Bayesian hierarchical model to estimate mean BMI by year, country and rural or urban place of residence. As described in the Methods, the estimated trends in population mean BMI represent a combination of (1) the change in the health of individuals due to change in their economic status and environment, and (2) the change in the composition of individuals that make up the population (and their economic status and environment).
From 1985 to 2017, the proportion of the world’s population who lived in urban areas1 increased from 41% to 55%. Over the same period, global age-standardized mean BMI increased from 22.6 kg m−2 (95% credible interval 22.4–22.9) to 24.7 kg m−2 (24.5–24.9) in women, and from 22.2 kg m−2 (22.0–22.4) to 24.4 kg m−2 (24.2–24.5) in men. The increase in mean BMI was 2.09 kg m−2 (1.73–2.44) and 2.10 kg m−2 (1.79–2.41) among rural women and men, respectively, compared to 1.35 kg m−2 (1.05–1.65) and 1.59 kg m−2 (1.33–1.84) in urban women and men. Nationally, change in mean BMI ranged from small decreases among women in 12 countries in Europe and Asia Pacific, to a rise of >5 kg m−2 among women in Egypt and Honduras. The lowest observed sex-specific mean BMI over these 33 years was that of rural women in Bangladesh of 17.7 kg m−2 (16.3–19.2) and rural men in Ethiopia of 18.4 kg m−2 (17.0–19.9), both in 1985; the highest were 35.4 kg m−2 (33.7–37.1) for urban women and 34.6 kg m−2 (33.1–35.9) for rural men in American Samoa in 2017 (Extended Data Figs. 2, 3), representing a twofold difference.
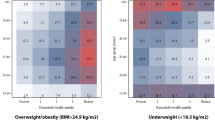
In 1985, urban men and women in every country in east, south and southeast Asia, Oceania, Latin America and the Caribbean and a region that comprises central Asia, the Middle East and north Africa had a higher mean BMI than their rural peers (Figs. 1, 2). The urban–rural gap was as large as 3.25 kg m−2 (2.57–3.96) in women and 3.05 kg m−2 (2.44–3.68) in men in India. Over time, the BMI gap between rural and urban women shrank in all of these regions by at least 40%, as BMI rose faster in rural areas than in cities (Fig. 3). In 14 countries in these regions, including Armenia, Chile, Jamaica, Jordan, Malaysia, Taiwan and Turkey, the ordering of rural and urban female BMI reversed over time and rural women had higher BMI than their urban peers in 2017 (Fig. 1 and Extended Data Fig. 4).
a, Difference in age-standardized mean BMI in 1985. b, Difference in age-standardized mean BMI in 2017. We did not estimate the difference between rural and urban areas for countries and territories in which the entire population live in areas classified as urban (Singapore, Hong Kong, Bermuda and Nauru) or rural (Tokelau)—shown in grey. See Extended Data Fig. 2 for mean BMI at the national level and in rural and urban populations in 1985 and 2017. See Extended Data Fig. 6 for comparisons of the results between women and men.
a, Difference in age-standardized mean BMI in 1985. b, Difference in age-standardized mean BMI in 2017. We did not estimate the difference between rural and urban areas for countries and territories in which the entire population live in areas classified as urban (Singapore, Hong Kong, Bermuda and Nauru) or rural (Tokelau)—shown in grey. See Extended Data Fig. 3 for mean BMI at the national level and in rural and urban populations in 1985 and 2017. See Extended Data Fig. 6 for comparison of results between women and men.
The mean BMI of rural men also increased more than the mean BMI of urban men in south Asia and Oceania, shrinking the urban–rural BMI gap by more than half (Figs. 2, 3). In east and southeast Asia, Latin America and the Caribbean, and central Asia, the Middle East and north Africa, men in both rural and urban areas experienced a similar BMI increase and, therefore, the urban excess BMI did not change substantially over time.
In contrast to emerging economies, excess BMI among urban women became larger in sub-Saharan Africa (Fig. 3): from 2.59 kg m−2 (2.21–2.98) in 1985 to 3.17 kg m−2 (2.93–3.42) in 2017 (posterior probability of the observed increase being a true increase >0.999). This occurred because female BMI rose faster in cities than in rural areas in sub-Saharan Africa. This led to women in sub-Saharan African countries, especially those in west Africa, having the largest urban excess BMI of any country in 2017—for example, more than 3.35 kg m−2 in Niger, Burkina Faso, Togo and Ghana (Fig. 1 and Extended Data Fig. 4). BMI increased at a similar rate in rural and urban men in sub-Saharan Africa, with the difference in 2017 (1.66 kg m−2; 1.37–1.94) being similar to 1985 (1.60 kg m−2; 1.13–2.07) (Fig. 2 and Extended Data Fig. 4).
BMI was previously lower in rural areas of low- and middle-income countries than in cities, both because rural residents had higher energy expenditure in their daily work—especially agriculture—and domestic activities, such as fuelwood and water collection13,14, and because lower incomes in rural areas restricted food consumption15. In middle-income countries, agriculture is increasingly mechanized, cars are used for rural transport as income increases and road infrastructure improves, service and administrative jobs have become more common in rural areas, and some household tasks are no longer needed—for example, because homes have a water connection and use commercial fuels16. Furthermore, higher incomes as a result of economic growth allow more spending on food and hence higher caloric intake, disproportionately more in rural areas, where a substantial share of income was previously spent on food. Additionally, the consumption of processed carbohydrates may have increased disproportionately in rural areas where such foods have become more readily available through national and transnational companies9,17,18,19,20,21. These changes, referred to as ‘urbanization of rural life’ by some researchers6, have contributed to a larger increase in rural BMI22,23.
In contrast to other regions, urbanization in sub-Saharan Africa preceded significant economic growth24. Subsistence farming remains common in Africa, and agriculture remains mostly manual; fuelwood—usually collected by women—is still the dominant fuel in rural Africa; and the use of cars for transportation is limited by poor infrastructure and poverty. In African cities, many people have service and office jobs, and mobility has become less energy-intensive owing to shorter travel distances and the use of cars and buses. Furthermore, urban markets where fresh produce is sold are increasingly replaced by commercially prepared and processed foods from transnational and local industries and street vendors25,26,27. These effects are exacerbated by limited time and space for cooking healthy meals and possibly perceptions of large weight as a sign of affluence28,29.
In contrast to low- and middle-income regions, urban women in high-income western and Asia Pacific regions, and in central and eastern Europe, had slightly lower mean BMI than their rural peers in 2017 (Fig. 3). The rural excess BMI for women in these regions changed little from 1985 to 2017. Nationally, the excess BMI of rural women was largest in central and eastern European countries (for example, around 1 kg m−2 or more in Belarus, Latvia and Czech Republic; Fig. 1 and Extended Data Fig. 4). Rural men in high-income western countries also had an excess BMI compared to urban men throughout the analysis period. The largest rural excess BMI for men in 2017 was seen in Sweden, Czech Republic, Ireland, Australia, Austria and the United States, which all had an excess BMI of 0.35 kg m−2 or larger. In the high-income Asia Pacific region and in central and eastern Europe, rural and urban men had almost identical BMI throughout these three decades (Fig. 2 and Extended Data Fig. 4).
The lower urban BMI in high-income and industrialized countries reflects a growing rural economic and social disadvantage, including lower education and income, lower availability and higher price of healthy and fresh foods30,31, less access to, and use of, public transport and walking than in cities32,33, and limited availability of facilities for sports and recreational activity34, which account for a significant share of overall physical activity in high-income and industrialized countries.
We also estimated how much of the overall rise in mean BMI since 1985 has been due to increases in BMI of rural and urban populations versus those attributable to urbanization (defined as an increase in the proportion of the population who live in urban areas), in each region and in the world as a whole. At the global level, 60% (56–64) of the rise in mean BMI from 1985 to 2017 in women and 57% (53–60) in men was due to increases in the BMI of rural populations; 28% (24–31) in women and 30% (27–32) in men due to the rise in BMI in urban populations; and 13% (11–15) and 14% (12–16) due to urbanization (Table 1). The contribution of the rise in rural BMI ranged from around 60% to 90% in the mostly rural regions of sub-Saharan Africa, east, south and southeast Asia and Oceania. The contribution of urbanization was small in all regions of the world, with maximum values of 19% (15–25) among women and 14% (10–21) among men in sub-Saharan Africa.
Our results show that, contrary to the prevailing view3,4,5,6, BMI is rising at the same rate or faster in rural areas compared to cities, particularly in low- and middle-income countries except among women in sub-Saharan Africa. These trends have resulted in a rural–urban convergence in BMI in most low- and middle-income countries, especially for women. This convergence mirrors the experience of high-income and industrialized countries, where we found a persistently higher BMI in rural areas. The rising rural BMI is the largest contributor to the BMI rise in low- and middle-income regions and in the world as a whole over the last 33 years, which challenges the current paradigm of urban living and urbanization as the key driver of the global epidemic of obesity.
In poor societies, urban areas historically had lower levels of undernutrition35,36, possibly because infrastructure such as roads and electricity facilitate food trade, transport and storage in cities, which can in turn reduce the impacts of agricultural shocks and seasonality. As economic growth and rural nutrition programmes reduce rural caloric deficiency, the rural undernutrition disadvantage may be replaced with a more general and complex malnutrition that entails excessive consumption of low-quality calories. To avoid such an unhealthy transition, the fragmented national and international responses to undernutrition and obesity should be integrated, and the narrow focus of international aid on undernutrition should be broadened, to enhance access to healthier foods in poor rural and urban communities.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this paper.
Methods
Our aim was to estimate trends in mean BMI from 1985 to 2017 by rural and urban place of residence for 200 countries and territories (Supplementary Table 2). To achieve this aim, we pooled cross-sectional population-based data on height and weight in adults aged 18 years and older. Therefore, by design, our results measure total change in BMI in each country’s rural and urban populations, which consists of (1) change in the BMI of individuals due to change in their economic status and environment, and (2) change in the composition of individuals that make up the population (and their economic status and environment). Change in population composition occurs naturally owing to fertility and mortality, as well as owing to migration. Therefore, our results should not be interpreted as solely a change in the BMI of individuals. Both components of change are relevant for policy formulation because policies should address the environment and nutrition of the contemporary population.
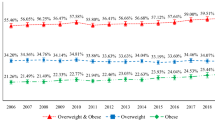
We used mean BMI as the primary outcome, rather than prevalence of overweight or obesity, because the relationship between BMI and disease risk is continuous, with each unit lower BMI being associated with a constant proportional reduction in disease risk until a BMI of around 21–23 kg m−2, which is below the cut-offs used to define overweight and obesity37,38,39. Therefore, the largest health benefits of weight management are achieved by lowering the population distribution of BMI. Mean BMI is the simplest summary statistic of the population distribution. Nonetheless, mean BMI and prevalence of overweight and obesity are closely associated (Extended Data Fig. 5).
Data sources
We used a database on cardiometabolic risk factors collated by the Non-Communicable Disease Risk Factor Collaboration (NCD-RisC). NCD-RisC is a worldwide network of health researchers and practitioners, that systematically documents the worldwide trends and variations in risk factors for non-communicable diseases. The database was collated through multiple routes for identifying and accessing data. We accessed publicly available population-based measurement surveys—for example, Demographic and Health Surveys, Global School-based Student Health Surveys, the European Health Interview and Health Examination Surveys and those available via the Inter-University Consortium for Political and Social Research. We requested, through the World Health Organization (WHO) and its regional and country offices, help with identification and access to population-based surveys from ministries of health and other national health and statistical agencies. Requests were also sent by the World Heart Federation to its national partners. We made similar requests to the co-authors of an earlier pooled analysis of cardiometabolic risk factors40,41,42,43 and invited them to reanalyse data from their studies and join NCD-RisC. Finally, to identify major sources not accessed through the above routes, we searched and reviewed published studies as described previously44 and invited all eligible studies to join NCD-RisC.
Anonymized individual record data from sources included in NCD-RisC were reanalysed according to a common protocol. Within each survey, we included participants aged 18 years and older who were not pregnant. We dropped participants with implausible BMI levels (defined as BMI < 10 kg m−2 or BMI > 80 kg m−2) or with implausible height or weight values (defined as height < 100 cm, height > 250 cm, weight < 12 kg or weight > 300 kg; <0.2% of all subjects). We also dropped participants whose urban and rural status was unknown in surveys that had recorded place of residence (0.05% of all participants). We calculated mean BMI and its standard error by sex, age group (18 years, 19 years, 10-year age groups from 20–29 years to 70–79 years and 80+ years) and rural or urban place of residence. All analyses incorporated appropriate sample weights and complex survey design, when applicable, in calculating summary statistics. Countries typically use the rural and urban classification of communities designated by their statistical offices at any given time both for survey design and for reporting of population to the United Nations Population Division. The classification can change, for example as previously rural areas grow and industrialize and hence become, and are (re)designated as, de novo cities. To the extent that the reclassifications keep up with changes in the real status of each community, survey and population data reflect the status of each community at the time of measurement. For surveys without information on place of residence, we calculated age- and sex-stratified summary statistics for the entire sample, which represented the population-weighted sum of rural and urban means.
To ensure summaries were prepared according to the study protocol, computer code was provided to NCD-RisC members who requested assistance. All submitted data were checked by at least two independent reviewers. Questions and clarifications were discussed with NCD-RisC members and resolved before data were incorporated into the database.
Finally, we incorporated all nationally representative data from sources that were identified but not accessed through the above routes, by extracting summary statistics from published reports. Data were also extracted for nine WHO STEPwise approach to Surveillance (STEPS) surveys, one Countrywide Integrated Non-communicable Diseases Intervention (CINDI) survey, and five sites of the WHO Multinational MONItoring of trends and determinants in CArdiovascular disease (MONICA) project that were not deposited in the MONICA Data Centre. Data were extracted from published reports only when reported by sex and in age groups no wider than 20 years. We also used data from a previous global data pooling study43 when such data had not been accessed through the routes described.
All NCD-RisC members are asked periodically to review the list of sources from their country, to suggest additional sources not in the database, and to verify that the included data meet the inclusion criteria listed below and are not duplicates. The NCD-RisC database is continuously updated through this contact with NCD-RisC members. For this paper, we used data from the NCD-RisC database for years 1985 to 2017 and ages 18 years and older. A list of the data sources that we used in this analysis and their characteristics is provided in Supplementary Table 1.
Data inclusion and exclusion
Data sources were included in the NCD-RisC database if: (1) measured data on height, weight, waist circumference or hip circumference were available; (2) study participants were 5 years of age and older; (3) data were collected using a probabilistic sampling method with a defined sampling frame; (4) data were from population samples at the national, sub-national (that is, covering one or more sub-national regions, more than three urban communities or more than five rural communities) or community level; and (5) data were from the countries and territories listed in Supplementary Table 2.
We excluded all data sources that were based solely on self-reported weight and height without a measurement component, because these data are subject to biases that vary by geography, time, age, sex and socioeconomic characteristics45,46,47. Owing to these variations, approaches to correcting self-reported data leave residual bias. We also excluded data sources on population subgroups whose anthropometric status may differ systematically from the general population, including: (1) studies that included or excluded people based on their health status or cardiovascular risk; (2) studies whose participants were only ethnic minorities; (3) specific educational, occupational, or socioeconomic subgroups, with the exception noted below; (4) those recruited through health facilities, with the exception noted below; and (5) women aged 15–19 years in surveys which sampled only ever-married women or measured height and weight only among mothers.
We used school-based data in countries, and in age–sex groups, with school enrolment of 70% or higher. We used data for which the sampling frame was health insurance schemes in countries in which at least 80% of the population were insured. Finally, we used data collected through general practice and primary care systems in high-income and central European countries with universal insurance, because contact with the primary care systems tends to be as good as or better than response rates for population-based surveys.
Conversion of BMI prevalence metrics to mean BMI
In 2% of our data points—mostly extracted from published reports or from a previous pooling analysis43—mean BMI was not reported, but data were available for the prevalence of one or more BMI categories, for example, BMI ≥ 30 kg m−2. In order to use these data, we used previously validated conversion regressions2 to estimate the missing primary outcome from the available BMI prevalence metric(s). All sources of uncertainty in the conversion—including the sampling uncertainty of the original data, the uncertainty of the regression coefficients and random effects, and the regression residuals—were carried forward by using repeated draws from their joint posterior distribution, accounting for the correlations among the uncertainties of regression coefficients and random effects.
Statistical analysis of BMI trends by rural and urban place of residence
We used a Bayesian hierarchical model to estimate mean BMI by country, year, sex, age and place of residence. The statistical model is described in detail in a statistical paper and related substantive papers2,35,40,41,42,43,44,48,49,50,51, and in the Supplementary Information. In summary, we organized countries into 21 regions (Supplementary Table 2), mostly based on geography and national income. The exception was high-income English-speaking countries (Australia, Canada, Ireland, New Zealand, the United Kingdom and the United States), grouped together in one region because BMI and other cardiometabolic risk factors have similar trends in these countries, which can be distinct from other countries in their geographical regions2,49,50,52. Regions were in turn organized into nine super-regions.
The model had a hierarchical structure in which estimates for each country and year were informed by their own data, if available, and by data from other years in the same country and from other countries, especially those in the same region with data for similar time periods. The extent to which estimates for each country-year were influenced by data from other years and other countries depended on whether the country had data, the sample size of the data, whether they were national, and the within-country and within-region variability of the available data. The model incorporated nonlinear time trends comprising linear terms and a second-order random walk, all modelled hierarchically. The age association of BMI was modelled using a cubic spline to allow nonlinear age patterns, which could vary across countries. The model accounted for the possibility that BMI in sub-national and community samples might differ systematically from nationally representative ones and have larger variation than in national studies. These features were implemented by including data-driven fixed-effect and random-effect terms for sub-national and community data. The fixed effects adjusted for systematic differences between sub-national or community studies and national studies. The random effects allowed national data to have larger influence on the estimates than sub-national or community data with similar sample sizes.
Here, we extended the model to make estimates for rural and urban populations following a previously published approach35,51. This model includes a parameter representing the urban–rural BMI difference, which is estimated empirically and allowed to vary by country and year. The model uses all of the data—those stratified by rural and urban place of residence as well as those reported for the entire population. If data for a country-year were not stratified by place of residence, the estimated urban–rural BMI difference was informed by stratified data from other years and countries, especially those in the same region with data from similar time periods.
We fitted the statistical model with the Markov chain Monte Carlo (MCMC) algorithm and following burn-in obtained 5,000 samples (or draws) from the posterior distribution of model parameters, which were in turn used to obtain the posterior distributions of our primary outcomes—mean urban BMI, mean rural BMI and mean urban–rural BMI difference. Posterior estimates were made in 1-year age groups for ages 18 and 19 and 5-year age groups for those aged 20 years and older. We generated age-standardized estimates by taking weighted means of age-specific estimates, using age weights from the WHO standard population. Regional and global rural and urban mean BMI estimates were calculated as population-weighted averages of rural and urban mean for the constituent country estimates by age group and sex. National mean BMI was calculated as population-weighted averages of the rural and urban means. All analyses were done separately by sex because geographical and temporal patterns of BMI differ between men and women2.
The reported credible intervals represent the 2.5th and the 97.5th percentiles of the posterior distributions. We report the posterior probability that the estimated urban–rural BMI difference is a true difference in the same direction as the posterior mean estimate. We also report the posterior probability that the estimated change in the rural–urban BMI difference over time represents a true increase or decrease.
Validation of statistical model
We calculated the difference between the posterior estimates from the model and data from national studies. Median errors were very close to zero (0.03 kg m−2 for women and −0.02 kg m−2 for men) and median absolute errors were 0.32 kg m−2 for women and 0.26 kg m−2 for men, indicating that the estimates were unbiased and had small deviations relative to national studies. The differences were indistinguishable from zero at the 5% level of statistical significance.
We also tested how well our statistical model predicts missing data, known as external predictive validity or cross-validation, in two different tests. In the first test, we held out all data from 10% of countries with data (that is, created the appearance of countries with no data for which we actually had data). The countries for which the data were withheld were selected randomly from the following three groups: data rich (8 or more data sources for women and 7 or more data sources for men), data poor (1–3 data sources for women and 1–2 for men) and average data availability (4–7 data sources for women and 3–6 for men). All data-rich countries had at least one data source after 2000 and at least one source with data stratified on rural and urban place of residence. We fitted the model to the data from the remaining 90% of countries and made estimates of the held-out observations. In the second test, we assessed other patterns of missing data by holding out 10% of our data sources, again from a mix of data-rich, data-poor and average-data countries, as defined above. For a given country, we either held out a random one third of the country’s data or all of the country’s 2000–2017 data to determine, respectively, how well we filled in the gaps for countries with intermittent data and how well we estimated in countries without recent data. We fitted the model to the remaining 90% of the dataset and made estimates of the held-out observations. We repeated each test five times, holding out a different subset of data in each repetition. In both tests, we calculated the differences between the held-out data and the estimates. We also calculated the 95% credible intervals of the estimates; in a model with good external predictive validity, 95% of held-out values would be included in the 95% credible intervals.
Our statistical model performed very well in the external validation tests, that is, in estimating mean BMI when data were missing. The estimates of mean BMI were unbiased, as evidenced with median errors that were zero or close to zero globally (0.03 and −0.03 kg m−2 for women and –0.15 and 0.00 kg m−2 for men in the first and second tests, respectively), and less than ±0.20 kg m−2 in every subset of withheld data except 1985–1999 data in the first test for men, for which the median error was −0.24 kg m−2 (Extended Data Table 2). Most of the median errors were indistinguishable from zero at the 5% level of statistical significance. The 95% credible intervals of estimated mean BMI covered 94–98% of true data globally; coverage was >93% in all but one subset of withheld data. Median absolute errors ranged from 0.52 to 1.09 kg m−2 globally and were at most 1.29 kg m−2 in all subsets of withheld data. Median absolute errors were smaller in the second test, in which subsets of data sources from some countries were withheld, than in the first test, in which all data from some countries were withheld. Given that we had data for 190 out of 200 countries for women and 183 out of 200 countries for men, the second test is a better reflection of data availability in our analysis. For comparison, median absolute differences for mean BMI between pairs of nationally representative surveys done in the same country and in the same year was 0.46 kg m−2, indicating that our estimates perform almost as well as running two parallel surveys in the same country and year.
Contributions of urbanization and rural and urban BMI change to changes in population mean BMI
We calculated the contributions of the following components to change in population mean BMI from 1985 to 2017: the contribution of change in BMI in rural areas, the contribution of change in BMI in urban areas, and the contribution of urbanization (that is, increase in the proportion of people living in urban areas). The first two parts were calculated by fixing the proportion of people living in rural and urban areas to 1985 levels and allowing BMI to change as it did in the respective population. The contribution of urbanization was calculated by fixing BMI in rural and urban areas to 2017 levels and allowing the proportion of people living in cities to change as it did. Percentage contributions were calculated using posterior draws, with reported credible intervals representing the 2.5th and the 97.5th percentiles of their posterior distributions. The change in mean BMI from 1985 to 2017 was then calculated as (contribution of change in rural BMI + contribution of change in urban BMI + contribution of change in the proportion of the population living in urban areas) = ((change in BMIrural1985–2017)(percentage living in rural areas1985) + (change in BMIurban1985–2017)(percentage living in urban areas1985) +(change in percentage living in urban areas1985–2017)(BMIurban2017 − BMIrural2017)).
Strengths and limitations
Urbanization is regarded as one of the most important contributors to the global obesity epidemic, but this perspective is based on limited data. We present the first comparable estimates of mean BMI for rural and urban populations worldwide over three decades using, to our knowledge, the largest and most comprehensive global database of human anthropometry with information on urban or rural place of residence. We used population-based measurement data from almost all countries, with information on participants’ urban or rural place of residence for the majority of data sources. We maintained a high level of data quality through repeated checks of study characteristics against our inclusion and exclusion criteria, which were verified by NCD-RisC members, and did not use any self-reported data to avoid bias in height and weight. Data were analysed according to a common protocol to obtain mean BMI by age, sex and place of residence. We used a statistical model that used all available data, while giving more weight to national data than sub-national and community studies and took into account the epidemiological features of BMI by using nonlinear time trends and age associations. The model used information on the urban–rural difference in BMI where available and estimated this difference hierarchically and temporally in the absence of stratified data.
Despite our large-scale data collation effort, some countries and regions had fewer data sources, particularly the Caribbean, and Polynesia and Micronesia. There were also fewer data sources before 2000. This temporal and geographical sparsity of data led to wider uncertainty intervals for these countries, regions and years. Although health surveys commonly use the rural and urban classification of national statistical offices, cities and rural areas in different countries vary in their demographic characteristics (for example, population size or density), economic activity, administrative structures, infrastructure and environment. These differences appropriately exist because countries themselves differ in terms of their demography, geography and economy. For example, a country with a smaller population may use a lower threshold for urban designation than one with a larger population, because its cities are naturally smaller even if they serve the same functions. Official rural and urban classifications are used for resource allocation and planning for nutrition and health53,54,55,56,57,58, which makes them the appropriate unit for tracking outcomes. Nonetheless, understanding the causes of change in rural and urban areas can be enriched with use of more complex and multi-dimensional measures of urbanicity involving size, density, economic and commercial activities and infrastructures59,60. Finally, urbanization could arise from a variety of mechanisms: (1) natural increase due to excess births over deaths in cities compared to rural areas, (2) rural to urban migration (often related to opportunities for work and education) and (3) reclassification of previously rural areas as they grow and industrialize and hence become, and are (re)designated as, de novo cities. The contributions of these mechanisms to urbanization vary across countries. The use of time-varying rural versus urban classification of communities ensures that in any year, the rural and urban strata represent the actual status of each community. However, each of these mechanisms may have different implications for changes in nutrition and physical activity and, therefore, BMI.
Data availability
Estimates of mean BMI by country, year, sex and urban and rural place of residence are available from http://www.ncdrisc.org/. Input data from publicly available sources can also be downloaded from http://www.ncdrisc.org/. For other data sources, contact information for data providers can be obtained from http://www.ncdrisc.org/.
Code availability
The computer code for the Bayesian hierarchical model used in this work is available at http://www.ncdrisc.org/.
References
United Nations Department of Economic and Social Affairs, Population Division. World Urbanization Prospects: the 2014 Revision. https://esa.un.org/unpd/wup/publications/files/wup2014-report.pdf (United Nations, 2015).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
WHO. Global Report on Urban Health: Equitable Healthier Cities for Sustainable Development. Report No. 9241565276. https://apps.who.int/iris/handle/10665/204715 (World Health Organization, 2016).
Yusuf, S., Reddy, S., Ôunpuu, S. & Anand, S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 104, 2746–2753 (2001).
Wagner, K. H. & Brath, H. A global view on the development of non communicable diseases. Prev. Med. 54, S38–S41 (2012).
Popkin, B. M. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am. J. Clin. Nutr. 84, 289–298 (2006).
Abubakari, A. R. et al. Prevalence and time trends in obesity among adult West African populations: a meta-analysis. Obes. Rev. 9, 297–311 (2008).
Filozof, C., Gonzalez, C., Sereday, M., Mazza, C. & Braguinsky, J. Obesity prevalence and trends in Latin-American countries. Obes. Rev. 2, 99–106 (2001).
Jaacks, L. M., Slining, M. M. & Popkin, B. M. Recent underweight and overweight trends by rural–urban residence among women in low- and middle-income countries. J. Nutr. 145, 352–357 (2015).
Mamun, A. A. & Finlay, J. E. Shifting of undernutrition to overnutrition and its determinants among women of reproductive ages in the 36 low to medium income countries. Obes. Res. Clin. Pract. 9, 75–86 (2015).
Neuman, M., Kawachi, I., Gortmaker, S. & Subramanian, S. V. Urban–rural differences in BMI in low- and middle-income countries: the role of socioeconomic status. Am. J. Clin. Nutr. 97, 428–436 (2013).
Popkin, B. M., Adair, L. S. & Ng, S. W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 70, 3–21 (2012).
Assah, F. K., Ekelund, U., Brage, S., Mbanya, J. C. & Wareham, N. J. Urbanization, physical activity, and metabolic health in sub-Saharan Africa. Diabetes Care 34, 491–496 (2011).
Levine, J. A. et al. The work burden of women. Science 294, 812 (2001).
Subramanian, S. & Deaton, A. The demand for food and calories. J. Polit. Econ. 104, 133–162 (1996).
Ng, S. W. & Popkin, B. M. Time use and physical activity: a shift away from movement across the globe. Obes. Rev. 13, 659–680 (2012).
Popkin, B. M. Nutrition, agriculture and the global food system in low and middle income countries. Food Policy 47, 91–96 (2014).
Reardon, T., Timmer, C. P. & Minten, B. Supermarket revolution in Asia and emerging development strategies to include small farmers. Proc. Natl Acad. Sci. USA 109, 12332–12337 (2012).
Mahajan, V. How Unilever reaches rural consumers in emerging markets. Harv. Bus. Rev. https://hbr.org/2016/12/how-unilever-reaches-rural-consumers-in-emerging-markets (2016).
Jacobs, A. & Richtel, M. How big business got Brazil hooked on junk food. The New York Times. https://www.nytimes.com/interactive/2017/09/16/health/brazil-obesity-nestle.html (2017).
Reardon, T., Timmer, C., Barrett, C. & Berdegué, J. The rise of supermarkets in Africa, Asia and Latin America. Am. J. Agric. Econ. 85, 1140–1146 (2003).
Ng, S. W., Norton, E. C. & Popkin, B. M. Why have physical activity levels declined among Chinese adults? Findings from the 1991–2006 China Health and Nutrition Surveys. Soc. Sci. Med. 68, 1305–1314 (2009).
Monda, K. L., Adair, L. S., Zhai, F. & Popkin, B. M. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur. J. Clin. Nutr. 62, 1318–1325 (2008).
Fay, M. & Opal, C. Urbanization without Growth: A Not-So-Uncommon Phenomenon. Policy Research Working Paper No. 241. https://openknowledge.worldbank.org/bitstream/handle/10986/21373/wps2412.pdf?sequence=1&isAllowed=y (World Bank, 2000).
FAO. Street Food in Urban Ghana. http://www.fao.org/3/a-i5804e.pdf (Food and Agriculture Organization of the United Nations, 2016).
Chilanga, E., Riley, L., Ngwira, J., Chalinda, C. & Masitala, L. Food Insecurity in Informal Settlements in Lilongwe, Malawi. https://www.afsun.org/wp-content/uploads/2017/09/AFSUN25.pdf (African Food Security Network, 2017).
Tschirley, D., Reardon, T., Dolislager, M. & Snyder, J. The rise of a middle class in east and southern Africa: implications for food system transformation. J. Int. Dev. 27, 628–646 (2015).
Holdsworth, M., Gartner, A., Landais, E., Maire, B. & Delpeuch, F. Perceptions of healthy and desirable body size in urban Senegalese women. Int. J. Obes. 28, 1561–1568 (2004).
Ettarh, R., Van de Vijver, S., Oti, S. & Kyobutungi, C. Overweight, obesity, and perception of body image among slum residents in Nairobi, Kenya, 2008–2009. Prev. Chronic Dis. 10, 130198 (2013).
Liese, A. D., Weis, K. E., Pluto, D., Smith, E. & Lawson, A. Food store types, availability, and cost of foods in a rural environment. J. Am. Diet. Assoc. 107, 1916–1923 (2007).
Lenardson, J. D., Hansen, A. Y. & Hartley, D. Rural and remote food environments and obesity. Curr. Obes. Rep. 4, 46–53 (2015).
Ihara, M. et al. A cross-sectional study of the association between city scale and daily steps in Japan: Data from the National Health and Nutrition Survey Japan (NHNS-J) 2006–2010 (in Japanese). Nippon Koshu Eisei Zasshi 63, 549–559 (2016).
Scheiner, J. A century of motorisation in urban and rural contexts: paths of motorisation in German cities. Erdkunde 66, 313–328 (2012).
Seguin, R., Connor, L., Nelson, M., LaCroix, A. & Eldridge, G. Understanding barriers and facilitators to healthy eating and active living in rural communities. J. Nutr. Metab. 2014, 146502 (2014).
Paciorek, C. J., Stevens, G. A., Finucane, M. M. & Ezzati, M. Children’s height and weight in rural and urban populations in low-income and middle-income countries: a systematic analysis of population-representative data. Lancet Glob. Health 1, e300–e309 (2013).
Krumdiek, C. L. The rural-to-urban malnutrition gradient. A key factor in the pathogenesis of urban slums. J. Am. Med. Assoc. 215, 1652–1654 (1971).
Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 373, 1083–1096 (2009).
The Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388, 776–786 (2016).
Singh, G. M. et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS ONE 8, e65174 (2013).
Danaei, G. et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet 377, 568–577 (2011).
Danaei, G. et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet 378, 31–40 (2011).
Farzadfar, F. et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. Lancet 377, 578–586 (2011).
Finucane, M. M. et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 377, 557–567 (2011).
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 387, 1377–1396 (2016).
Hayes, A. J., Clarke, P. M. & Lung, T. W. C. Change in bias in self-reported body mass index in Australia between 1995 and 2008 and the evaluation of correction equations. Popul. Health Metr. 9, 53 (2011).
Gorber, S. C., Tremblay, M., Moher, D. & Gorber, B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes. Rev. 8, 307–326 (2007).
Ezzati, M., Martin, H., Skjold, S., Vander Hoorn, S. & Murray, C. J. L. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J. R. Soc. Med. 99, 250–257 (2006).
Finucane, M. M., Paciorek, C. J., Danaei, G. & Ezzati, M. Bayesian estimation of population-level trends in measures of health status. Stat. Sci. 29, 18–25 (2014).
NCD Risk Factor Collaboration (NCD-RisC). A century of trends in adult human height. eLife 5, e13410 (2016).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 389, 37–55 (2017).
Finucane, M. M., Paciorek, C. J., Stevens, G. A. & Ezzati, M. Semiparametric Bayesian density estimation with disparate data sources: a meta-analysis of global childhood undernutrition. J. Am. Stat. Assoc. 110, 889–901 (2015).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387, 1513–1530 (2016).
The World Bank. An Overview of Links Between Obesity and Food Systems: Implications for the Food and Agriculture Global Practice Agenda. http://documents.worldbank.org/curated/en/222101499437276873/pdf/117200-REVISED-WP-Obesity-Overview-Web-PUBLIC-002.pdf (World Bank, 2017).
FAO. Ending Poverty and Hunger by Investing in Agriculture and Rural Areas. http://www.fao.org/3/a-i7556e.pdf (Food and Agriculture Organization of the United Nations, 2017).
WHO & Global Health Workforce Alliance. Global Experience of Community Health Workers for Delivery of Health Related Millenium Development Goals: a Systematic Review, Country Case Studies, and Recommendations for Integration into National Health Systems. https://www.who.int/workforcealliance/knowledge/publications/CHW_FullReport_2010.pdf?ua=1 (World Health Organization, 2010).
Bhutta, Z. A. et al. Rethinking community based strategies to tackle health inequities in South Asia. Br. Med. J. 363, k4884 (2018).
IFAD. Rural Development Report 2016: Fostering Inclusive Rural Transformation. https://www.ifad.org/documents/38714170/39155702/Rural+development+report+2016.pdf/347402dd-a37f-41b7-9990-aa745dc113b9 (International Fund for Agricultural Development, 2016).
FAO, IFAD & WFP. The State of Food Insecurity in the World 2015. Meeting the 2015 International Hunger Targets: Taking Stock of Uneven Progress. http://www.fao.org/3/a-i4646e.pdf (Food and Agriculture Organization of the United Nations, 2015).
Dahly, D. L. & Adair, L. S. Quantifying the urban environment: a scale measure of urbanicity outperforms the urban–rural dichotomy. Soc. Sci. Med. 64, 1407–1419 (2007).
Jones-Smith, J. C. & Popkin, B. M. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc. Sci. Med. 71, 1436–1446 (2010).
Acknowledgements
This study was funded by the Wellcome Trust. H.B. was supported by a Medical Research Council Doctoral Training Partnership Studentship, J.B. by a Royal Society Research Grant, and M.D.C. by an Academy of Medical Sciences Springboard Award. We thank L. Jaacks, B. Popkin, S. Sundberg and W. Willett for recommendations of relevant citations. The authors are responsible for the views expressed in this Letter and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Reviewer information
Nature thanks Miguel A. Martinez Beneito, Barry M. Popkin and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Consortia
Contributions
M.E. designed the study and oversaw research. H.B. led the data collection and statistical analysis, and prepared results. The other authors contributed to study design; collected, reanalysed, pooled and checked data; analysed pooled data; and prepared results. M.E. and H.B. wrote the first draft of the manuscript with input from the other authors.
Corresponding author
Ethics declarations
Competing interests
M.E. reports a charitable grant from the AstraZeneca Young Health Programme, and personal fees from Prudential, Scor and Third Bridge, outside the submitted work. The other authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Number of data sources by country.
The colour indicates the number of population-based data sources used in the analysis for each country. Countries and territories not included in the analysis are coloured in grey.
Extended Data Fig. 2 Age-standardized national, rural and urban mean BMI in women aged 18 years and older in 1985 and 2017 by country.
The numerical values are provided in Supplementary Table 3 and can be downloaded from http://www.ncdrisc.org.
Extended Data Fig. 3 Age-standardized national, rural and urban mean BMI in men aged 18 years and older in 1985 and 2017 by country.
The numerical values are provided in Supplementary Table 3 and can be downloaded from http://www.ncdrisc.org.
Extended Data Fig. 4 The difference between rural and urban age-standardized mean BMI in 1985 compared to 2017.
Each point shows one country and colours indicate region. A positive number indicates a higher urban mean BMI and a negative number indicates a higher rural mean BMI. Different sections labelled A–F indicate the following categories of countries. A, countries with an urban excess BMI that increased from 1985 to 2017. B, countries with an urban excess BMI that decreased from 1985 to 2017. C, countries with an urban excess BMI in 1985 that changed to a rural excess BMI in 2017. D, countries with a rural excess BMI that increased from 1985 to 2017. E, countries with a rural excess BMI that decreased from 1985 to 2017. F, countries with a rural excess BMI in 1985 that changed to an urban excess BMI in 2017.
Extended Data Fig. 5 The relationship between mean BMI and prevalence of overweight.
Overweight is defined as BMI ≥ 25 kg m−2. Prevalence is plotted on a probit scale, which changes in an approximately linear manner as the mean changes. Each point represents an age group- and sex-specific mean, stratified by place of residence as described in the Methods and with more than 25 participants, from data sources in the NCD-RisC database.
Extended Data Fig. 6 Comparison of the difference between rural and urban age-standardized mean BMI in women and men aged 18 years and older in 1985 and 2017.
Each point shows one country and colours indicate region.
Supplementary information
Supplementary Information
This file contains the statistical model for estimating BMI trends by rural and urban place of residence, Supplementary Tables 1-3 and Supplementary References.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
NCD Risk Factor Collaboration (NCD-RisC). Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 569, 260–264 (2019). https://doi.org/10.1038/s41586-019-1171-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-019-1171-x
This article is cited by
-
Differences in nutritional status and level of physical activity among adolescents living in urban and rural areas of Montenegro - national study
BMC Public Health (2024)
-
Impact of home quarantine on physical fitness of school-aged children in Xi’an during COVID-19 lockdown: a cross-sectional study
BMC Public Health (2024)
-
Relationship satisfaction and metabolic health parameters: a cross-sectional study in Burkinabe population of older adults
BMC Public Health (2024)
-
Intestinal IL-22RA1 signaling regulates intrinsic and systemic lipid and glucose metabolism to alleviate obesity-associated disorders
Nature Communications (2024)
-
Western diets and chronic diseases
Nature Medicine (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.