Abstract
The role of the prostatic middle lobe in the presentation and management of benign prostatic hyperplasia (BPH) is under-appreciated. Middle lobe enlargement is associated with intravesical prostatic protrusion (IPP), which causes a unique type of bladder outlet obstruction (BOO) via a ‘ball-valve’ mechanism. IPP is a reliable predictor of BOO and the strongest independent factor for failure of medical therapy necessitating conversion to surgical intervention. Men with middle lobe enlargement tend to exhibit mixed symptoms of both the storage and the voiding types, but symptomatology will vary depending on the degree of IPP present. Initial assessments such as uroflowmetry and post-void residual volumes are inadequate to detect IPP and could confound the clinical picture. Radiological evaluation of prostate morphology is key to assessment as it provides important prognostic information and can help with operative planning. Treatment strategies employed for BPH should consider the shape and morphology of prostate adenomata, specifically the presence of middle lobe enlargement and the degree of associated IPP.
Key points
-
Various subcategories of benign prostatic hyperplasia exist, specifically, middle lobe enlargement is associated with intravesical prostatic protrusion (IPP), which causes a unique type of bladder outlet obstruction (BOO) via a ball-valve mechanism.
-
IPP is a reliable clinical parameter that positively correlates strongly with the urodynamic evidence of BOO.
-
Measurement of IPP using transabdominal or transrectal ultrasonography is a discriminative evaluation that can help inform the decision to use invasive urodynamic studies.
-
Low-grade IPP can be managed conservatively with α-adrenoceptor antagonists and/or 5α-reductase inhibitors; 5α-reductase inhibitors might reduce total prostate volume but are unlikely to alter the degree of IPP.
-
High-grade IPP is the strongest predictor of failed medical therapy and conversion to surgical intervention. Patients with high-grade IPP should be offered surgery from the outset to reduce the risk of clinical progression.
-
The extent, shape and morphology of IPP might help inform the optimal surgical approach; however, more studies are needed to examine their effects on the success of bladder outlet procedures.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Platz, E. A., Smit, E., Curhan, G. C., Nyberg, L. M. & Giovannucci, E. Prevalence of and racial/ethnic variation in lower urinary tract symptoms and noncancer prostate surgery in US men. Urology 59, 877–883 (2002).
Foo, K. T. Solving the benign prostatic hyperplasia puzzle. Asian J. Urol. 3, 6–9 (2016).
Goddard, J. C. History of the prostate, part two: the cause of urinary symptoms. Trends Urol. Men. Health 10, 31–34 (2019).
Hunter, J. A Treatise on the Venereal Disease (1788).
Oesterling, J. E. Benign prostatic hyperplasia: a review of its histogenesis and natural history. Prostate 29, 67–73 (1996).
Chia, S. J., Heng, C. T., Chan, S. P. & Foo, K. T. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int. 91, 371–374 (2003).
Gandhi, J. et al. Clinical considerations for intravesical prostatic protrusion in the evalutation and management of bladder outlet obstruction secondary to benign prostatic hyperplasia. Curr. Urol. 12, 6–12 (2018).
Lee, A. et al. Can intravesical prostatic protrusion predict bladder outlet obstruction even in men with good flow? Asian J. Urol. 3, 39–43 (2016).
Sigdel, G. & Belokar, W. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic hyperplasia. J. Univ. Coll. Med. Sci. 3, 6–10 (2015).
Luo, G. C., Foo, K. T., Kuo, T. & Tan, G. Diagnosis of prostate adenoma and the relationship between the site of prostate adenoma and bladder outlet obstruction. Singap. Med. J. 54, 482–486 (2013).
Randall, A. Surgical pathology of prostatic obstructions (Williams & Wilkins, 1931).
Guneyli, S. et al. Magnetic resonance imaging of benign prostatic hyperplasia. Diagn. Interv. Radiol. 22, 215–219 (2016).
Lee, H. J., Lee, A., Huang, H. H., Sundaram, P. & Foo, K. T. Patients with small prostates and low-grade intravesical prostatic protrusion – a urodynamic evaluation. Asian J. Urol. 4, 247–252 (2017).
Wasserman, N. F. Benign prostatic hyperplasia: a review and ultrasound classification. Radiol. Clin. North. Am. 44, 689–710 (2006).
Wesson, M. B. The prostatic median bar. J. Urol. 22, 397–406 (1929).
Wang, D., Huang, H., Law, Y. M. & Foo, K. T. Relationships between prostatic volume and intravesical prostatic protrusion on transabdominal ultrasound and benign prostatic obstruction in patients with lower urinary tract symptoms. Ann. Acad. Med. Singap. 44, 60–65 (2015).
Tan, Y. G. et al. A systematic review and meta-analysis of transabdominal intravesical prostatic protrusion assessment in determining bladder outlet obstruction and unsuccessful trial without catheter. Eur. Urol. Focus. 8, 1003–1014 (2022). This systematic review provides evidence that IPP is a reliable clinical parameter that correlates strongly with underlying BOO and unsuccessful trial without catheter.
Doo, C. K. & Uh, H. S. Anatomic configuration of prostate obtained by noninvasive ultrasonography can predict clinical voiding parameters for determining BOO in men with LUTS. Urology 73, 232–236 (2009).
Roehrborn, C. G. et al. Five year results of the prospective randomized controlled prostatic urethral LIFT study. Can. J. Urol. 24, 8802–8813 (2017).
McVary, K. T. et al. Minimally invasive prostate convective water vapor energy ablation: a multicenter, randomized, controlled study for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J. Urol. 195, 1529–1538 (2016).
Zorn, K. C. et al. Aquablation therapy in large prostates (80–150 cc) for lower urinary tract symptoms due to benign prostatic hyperplasia: WATER II 3‐year trial results. BJUI Compass 3, 130–138 (2021).
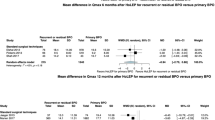
Eure, G., Rukstalis, D. & Roehrborn, C. Prostatic urethral lift for obstructive median lobes: consistent results across controlled trial and real-world settings. J. Endourol. 37, 50–59 (2023).
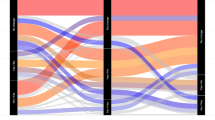
Lee, S. W., Cho, J. M., Kang, J. Y. & Yoo, T. K. Clinical and urodynamic significance of morphological differences in intravesical prostatic protrusion. Korean J. Urol. 51, 694–699 (2010). IPP has two morphological types of trilobar and bilobar enlargement; bladder contractility and BOO indexes were significantly increased in the trilobar adenoma group compared with the bilobar adenoma group.
D’Ancona, C. et al. The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol. Urodyn. 38, 433–477 (2019).
Stravodimos, K. G. et al. TRUS versus transabdominal ultrasound as a predictor of enucleated adenoma weight in patients with BPH: a tool for standard preoperative workup? Int. Urol. Nephrol. 41, 767–771 (2009).
Kuo, T. L., Teo, J. S. & Foo, K. T. The role of intravesical prostatic protrusion (IPP) in the evaluation and treatment of bladder outlet obstruction (BOO). Neurourol. Urodyn. 35, 535–537 (2016).
Lieber, M. M. et al. Intravesical prostatic protrusion in men in Olmsted County, Minnesota. J. Urol. 182, 2819–2824 (2009).
Kwon, S. Y., Ryu, J. W., Choi, D. H. & Lee, K. S. Clinical significance of the resistive index of prostatic blood flow according to prostate size in benign prostatic hyperplasia. Int. Neurourol. J. 20, 75–80 (2016).
Shin, S. H., Kim, J. W., Oh, M. M. & Moon, D. G. Defining the degree of intravesical prostatic protrusion in association with bladder outlet obstruction. Korean J. Urol. 54, 369–372 (2013).
Reis, L. O., Barreiro, G. C., Baracat, J., Prudente, A. & D’Ancona, C. A. Intravesical protrusion of the prostate as a predictive method of bladder outlet obstruction. Int. Braz. J. Urol. 34, 627–637 (2008).
Rieken, M., Presicce, F., Autorino, R. & DE Nuzio, C. Clinical significance of intravesical prostatic protrusion in the management of benign prostatic enlargement: a systematic review and critical analysis of current evidence. Min. Urol. Nefrol. 69, 548–555 (2017).
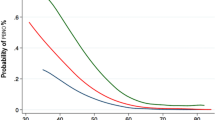
Yoshida, T. et al. Intravesical prostatic protrusion as a predicting factor for the adverse clinical outcome in patients with symptomatic benign prostatic enlargement treated with dutasteride. Urology 91, 154–157 (2016). The 3-year cumulative incidence of AUR or BPH-related surgery in the low IPP group was 9.9% compared with 71.5% in the high IPP group.
Zheng, J. et al. Role for intravesical prostatic protrusion in lower urinary tract symptom: a fluid structural interaction analysis study. BMC Urol. 15, 86 (2015). This fluid structural interaction analysis study demonstrated how high grades of IPP cause increasing distortion and deformation of the prostatic urethra leading to deterioration of flow efficiency and compromise of BOO alleviation treatment.
Kim, J. H. et al. Terminal dribbling in male patients with lower urinary tract symptoms: relationship with International Prostate Symptom Score and with intravesical prostatic protrusion. BMC Urol. 15, 89 (2015).
Abrams, P. et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol. Urodyn. 21, 167–178 (2002).
Bates, C. P., Whiteside, C. G. & Turner‐Warwick, R. Synchronous cine/pressure/flow/cysto‐urethrography with special reference to stress and urge incontinence. Br. J. Urol. 42, 714–723 (1970).
Shafik, A., El-Sibai, O. & Ahmed, I. Effect of urethral dilation on vesical motor activity: identification of the urethrovesical reflex and its role in voiding. J. Urol. 169, 1017–1019 (2003).
Lu, S. Y., Yang, C.-M., Fan, Y.-H., Long Lin, A. T. & Chen, K.-K. Intravesical prostatic protrusion correlates well with storage symptoms in elderly male patients with non-neurogenic overactive bladder. Urol. Sci. 27, 17–20 (2016).
Steers, W. D. Pathophysiology of overactive bladder and urge urinary incontinence. Rev. Urol. 4, S7–S18 (2002).
Keqin, Z. et al. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology 70, 1096–1109 (2007).
Hur, W. S. et al. Predictors of urgency improvement after holmium laser enucleation of the prostate in men with benign prostatic hyperplasia. Investig. Clin. Urol. 57, 431–436 (2016).
Kim, J. W. et al. Intravesical prostatic protrusion is a risk factor for bladder stone in patients with benign prostatic hyperplasia. Urology 84, 1026–1029 (2014).
Huang, W. et al. Risk factors for bladder calculi in patients with benign prostatic hyperplasia. Medicine 96, e7728 (2017).
Roehrborn, C. G. Accurate determination of prostate size via digital rectal examination and transrectal ultrasound. Urology 51, 19–22 (1998).
Dujin, M., Hovius, M. C. & Boeve, L. M. S. Intravesical protrusion of giant median prostatic lobe: a case report. Urol. Case Rep. 44, 102152 (2022).
Park, H. K. et al. Effect of intravesical prostatic protrusion on the characteristics of lower urinary tract symptom change after 12-week drug medication: a prospective analysis. Low. Urin. Tract. Symptoms 5, 1–4 (2013).
Cumpanas, A. A., Botoca, M., Minciu, R. & Bucuras, V. Intravesical prostatic protrusion can be a predicting factor for the treatment outcome in patients with lower urinary tract symptoms due to benign prostatic obstruction treated with tamsulosin. Urology 81, 859–863 (2013).
Kalkanli, A. et al. Intravesical prostatic protrusion: a potential marker of alpha-blocker treatment success in patients with benign prostatic enlargement. Urology 88, 161–165 (2016).
Topazio, L. et al. Intravescical prostatic protrusion is a predictor of alpha blockers response: results from an observational study. BMC Urol. 18, 6 (2018).
Liu, Q., Zhu, Y., Liu, J., Qi, J. & Kang, J. Ultrasound image features of intravesical prostatic protrusion indicated failure of medication therapy of finasteride and doxazosin in patients with benign prostatic hyperplasia (LUTS/BPH). Int. Urol. Nephrol. 49, 399–404 (2017).
Hirayama, K. et al. Evaluation of intravesical prostatic protrusion as a predictor of dutasteride-resistant lower urinary tract symptoms/benign prostatic enlargement with a high likelihood of surgical intervention. Urology 86, 565–569 (2015). In patients with BPH and severe IPP, combination therapy with dutasteride might have insufficient efficacy owing to a low proportion of stromal components, necessitating conversion to surgical intervention.
Dantas, L. P. et al. Treatment of bladder dysfunction with solifenacin: is there a risk of dementia or cognitive impairment? Braz. J. Med. Biol. Res. 55, e11721 (2022).
McVary, K. T., Rogers, T. & Roehrborn, C. G. Rezūm water vapor thermal therapy for lower urinary tract symptoms associated with benign prostatic hyperplasia: 4-year results from randomized controlled study. Urology 126, 171–179 (2019).
McVary, K. T. & Roehrborn, C. G. Three-year outcomes of the prospective, randomized controlled Rezūm system study: convective radiofrequency thermal therapy for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Urology 111, 1–9 (2018).
Rukstalis, D. et al. Prostatic urethral lift (PUL) for obstructive median lobes: 12 month results of the MedLift Study. Prostate Cancer Prostatic Dis. 22, 411–419 (2019).
Gravas, S. et al. EAU guidelines on non-neurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO) (European Association of Urology, 2020).
Parsons, J. K., Dahm, P., Kohler, T. S., Lerner, L. B. & Wilt, T. J. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2020. J. Urol. 204, 799–804 (2020).
Eure, G. et al. Real-world evidence of prostatic urethral lift confirms pivotal clinical study results: 2-year outcomes of a retrospective multicentre study. J. Endourol. 33, 576–584 (2019).
Naidu, S. G. et al. Prostate artery embolization–review of indications, patient selection, techniques and results. J. Clin. Med. 10, 5139 (2021).
Bilhim, T. Prostatic artery embolization and the median lobe: stuck in the middle with you? J. Vasc. Interv. Radiol. 30, 1817–1819 (2019).
Yu, S. C. H. et al. Thickness-to-height ratio of intravesical prostatic protrusion predicts the clinical outcome and morbidity of prostatic artery embolization for benign prostatic hyperplasia. J. Vasc. Interv. Radiol. 30, 1807–1816 (2019). IPP with a thickness to height ratio of ≤1.3 predicts the occurrence of post-procedure complications with urinary obstruction in patients undergoing PAE for the treatment of LUTS.
Maron, S. Z. et al. Effect of median lobe enlargement on early prostatic artery embolization outcomes. J. Vasc. Interv. Radiol. 31, 370–377 (2020).
Meira, M. et al. Intravesical prostatic protrusion does not influence the efficacy of prostatic artery embolization. J. Vasc. Interv. Radiol. 32, 106–112 (2019).
Gilling, P., Anderson, P. & Tan, A. Aquablation of the prostate for symptomatic benign prostatic hyperplasia: 1-year results. J. Urol. 197, 1565–1572 (2017).
Roehrborn, C. G., Teplitsky, S. & Das, A. K. Aquablation of the prostate: a review and update. Can. J. Urol. 26, 20–24 (2019).
Gilling, P. et al. WATER: a double-blind, randomized, controlled trial of Aquablation® vs transurethral resection of the prostate in benign prostatic hyperplasia. J. Urol. 199, 1252–1261 (2018).
Young, M. J., Elmussareh, M., Morrison, T. & Wilson, J. R. The changing practice of transurethral resection of the prostate. Ann. R. Coll. Surg. Engl. 100, 326–329 (2018).
DeLay, K. J., Nutt, M. & McVary, K. T. Ejaculatory dysfunction in the treatment of lower urinary tract symptoms. Transl. Androl. Urol. 5, 450–459 (2016).
Favilla, V. et al. Risk factors of sexual dysfunction after transurethral resection of the prostate (TURP): a 12 months follow-up. J. Endocrinol. Invest. 36, 1094–1098 (2013).
Gul, Z., Chughtai, B., Te, A. E., Thomas, D. & Kaplan, S. A. Ejaculatory preserving middle lobe only-transurethral resection and vaporization of the prostate: 12-year experience. Urology 134, 199–202 (2019).
Gilling, P. J., Kennett, K., Das, A. K., Thompson, D. & Fraundorfer, M. R. Holmium laser enucleation of the prostate (HOLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J. Endourol. 12, 457–459 (1998).
Tamalunas, A. et al. Holmium laser enucleation of the prostate: a truly size-independent method? Low. Urin. Tract. Symptoms 14, 17–26 (2022).
Rücker, F. et al. A call for HoLEP: en-bloc vs. two-lobe vs. three-lobe. World J. Urol. 39, 2337–2345 (2021).
Ito, K. et al. Intravesical prostatic protrusion is not always the same shape: evaluation by preoperative cystoscopy and outcome in HoLEP. Neurourol. Urodyn. 37, 2160–2166 (2018). Patients with middle lobe protrusion had greater IPSS improvement after HoLEP than those with comparable-length IPP but without middle lobe protrusion.
Wisenbaugh, E. S., Nunez-Nateras, R., Mmeje, C. O., Warner, J. N. & Humphreys, M. R. Does prostate morphology affect outcomes after holmium laser enucleation? Urology 81, 844–848 (2013).
Humphreys, M. R. et al. Holmium laser enucleation of the prostate–outcomes independent of prostate size? J. Urol. 180, 2431–2435 (2008).
Oh, S. J. Current surgical techniques of enucleation in holmium laser enucleation of the prostate. Investig. Clin. Urol. 60, 333–342 (2019).
Author information
Authors and Affiliations
Contributions
S.G. researched data for the article. S.G. and B.C. contributed substantially to discussion of the content. S.G. and F.R. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no completing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Jonathan Goddard, Giuseppe Magistro and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gharbieh, S., Reeves, F. & Challacombe, B. The prostatic middle lobe: clinical significance, presentation and management. Nat Rev Urol 20, 645–653 (2023). https://doi.org/10.1038/s41585-023-00774-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-023-00774-7
This article is cited by
-
Exploring the Enigma of 5-ARIs Resistance in Benign Prostatic Hyperplasia: Paving the Path for Personalized Medicine
Current Urology Reports (2023)