Abstract
The use of prostate-specific membrane antigen (PSMA)-directed applications in modern prostate cancer management has evolved rapidly over the past few years, helping to establish new treatment pathways and provide further insights into prostate cancer biology. However, the prognostic implications of PSMA–PET have not been studied systematically, owing to rapid clinical implementation without long follow-up periods to determine intermediate-term and long-term oncological outcomes. Currently available data suggest that traditional prognostic factors and survival outcomes are associated with high PSMA expression (both according to immunohistochemistry and PET uptake) in men with localized and biochemically recurrent disease. Treatment with curative intent (primary and/or salvage) often fails when PSMA-positive metastases are present; however, the sensitivity of PSMA–PET in detecting all metastases is poor. Low PSMA–PET uptake in recurrent disease is a favourable prognostic factor; however, it can be associated with poor prognosis in conjunction with high 18F-fluorodeoxyglucose uptake in metastatic castration-resistant prostate cancer. Clinical trials embedding PSMA–PET for guiding management with reliable oncological outcomes are needed to support ongoing clinical use.
Key points
-
Prostate-specific membrane antigen (PSMA)–PET–CT is increasingly being used in clinical practice for prostate cancer staging and re-staging owing to improved accuracy and potential to change management. Improved oncological outcomes from improved accuracy are assumed, but yet to be conclusively proven.
-
PSMA is biologically associated with high-grade prostate cancer and advanced disease, and is altered by the use of systemic hormonal therapies. Higher PSMA expression according to immunohistochemistry has been associated with worse survival outcomes than patients with low PSMA expression.
-
Primary tumour PSMA ligand uptake on PET–CT has been associated with traditional prognostic factors, such as high Gleason scores or International Society of Uro-Pathology (ISUP) Grade Group and reduced progression-free survival after radical prostatectomy. PSMA–PET detection of index tumours also serves to improve accuracy of prostate biopsy and possibly enable safe omission of biopsy for men with suspected prostate cancer.
-
Detection of PSMA-positive lymph nodal metastases is associated with biochemical persistence and biochemical recurrence after surgery, as well as after salvage therapies (surgery and radiotherapy). However, small-sized lymph node metastases will be missed by PSMA–PET; thus, clinical factors remain an important consideration.
-
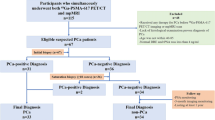
Biochemical recurrence prognostic factors, such as high Gleason score, high PSA levels and short PSA doubling time, are predictive of positive PSMA–PET results. Conversely, patients with post-prostatectomy biochemical recurrence and negative PSMA–PET might be a group of patients with the best oncological outcomes after salvage radiotherapy.
-
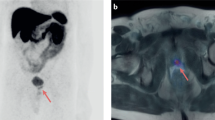
PSMA–PET has a high detection rate for metastasis in men with non-metastatic castration-resistant prostate cancer according to conventional imaging, enabling image-guided treatments (such as radiotherapy and radioligand therapy) in this context. High PSMA–PET radioligand uptake in men with castration-resistant prostate cancer does not necessarily confer a poor prognosis, with emerging data suggesting that low PSMA uptake with concurrent high 18F-fluorodeoxyglucose uptake might be the subgroup with a very poor prognosis, and least likely to benefit from radioligand therapy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Mottet, N. et al. EAU-EANM-ESTRO-ESUR-ISUP-SIOG guidelines on prostate cancer. EAU https://uroweb.org/guidelines/prostate-cancer (2020).
Wallitt, K. L. et al. Clinical PET imaging in prostate cancer. RadioGraphics 37, 1512–1536 (2017).
Jadvar, H. Molecular imaging of prostate cancer with 18F-fluorodeoxyglucose PET. Nat. Rev. Urol. 6, 317–323 (2009).
Jadvar, H. Is there use for FDG-PET in prostate cancer? Semin. Nucl. Med. 46, 502–506 (2016).
Horoszewicz, J. S. et al. The LNCaP cell line — a new model for studies on human prostatic carcinoma. Prog. Clin. Biol. Res. 37, 115–132 (1980).
Horoszewicz, J. S., Kawinski, E. & Murphy, G. P. Monoclonal antibodies to a new antigenic marker in epithelial prostatic cells and serum of prostatic cancer patients. Anticancer Res. 7, 927–935 (1987).
Wynant, G. E. et al. Immunoscintigraphy of prostatic cancer: preliminary results with 111In-labeled monoclonal antibody 7E11-C5.3 (CYT-356). Prostate 18, 229–241 (1991).
Robinson, M. B., Blakely, R. D., Couto, R. & Coyle, J. T. Hydrolysis of the brain dipeptide N-acetyl-L-aspartyl-L-glutamate. Identification and characterization of a novel N-acetylated alpha-linked acidic dipeptidase activity from rat brain. J. Biol. Chem. 262, 14498–14506 (1987).
Kozikowski, A. P. et al. Design of remarkably simple, yet potent urea-based inhibitors of glutamate carboxypeptidase II (NAALADase). J. Med. Chem. 44, 298–301 (2001).
Maurer, T., Eiber, M., Schwaiger, M. & Gschwend, J. E. Current use of PSMA-PET in prostate cancer management. Nat. Rev. Urol. 13, 226–235 (2016).
Lawhn-Heath, C. et al. Prostate-specific membrane antigen PET in prostate cancer. Radiology 299, 248–260 (2021).
Siva, S. et al. Expanding the role of small-molecule PSMA ligands beyond PET staging of prostate cancer. Nat. Rev. Urol. 17, 107–118 (2020).
van Leeuwen, F. W. B. et al. Technologies for image-guided surgery for managing lymphatic metastases in prostate cancer. Nat. Rev. Urol. 16, 159–171 (2019).
Wright, G. L. Jr, Haley, C., Beckett, M. L. & Schellhammer, P. F. Expression of prostate-specific membrane antigen in normal, benign, and malignant prostate tissues. Urol. Oncol. 1, 18–28 (1995).
O’Keefe, D. S. et al. Mapping, genomic organization and promoter analysis of the human prostate-specific membrane antigen gene. Biochim. Biophys. Acta 1443, 113–127 (1998).
DeMarzo, A. M., Nelson, W. G., Isaacs, W. B. & Epstein, J. I. Pathological and molecular aspects of prostate cancer. Lancet 361, 955–964 (2003).
Kinoshita, Y. et al. Expression of prostate-specific membrane antigen in normal and malignant human tissues. World J. Surg. 30, 628–636 (2006).
Silver, D. A., Pellicer, I., Fair, W. R., Heston, W. D. & Cordon-Cardo, C. Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin. Cancer Res. 3, 81–85 (1997).
Ferreira, G., Iravani, A., Hofman, M. S. & Hicks, R. J. Intra-individual comparison of 68Ga-PSMA-11 and 18F-DCFPyL normal-organ biodistribution. Cancer Imaging 19, 23 (2019).
Israeli, R. S., Powell, C. T., Fair, W. R. & Heston, W. D. Molecular cloning of a complementary DNA encoding a prostate-specific membrane antigen. Cancer Res. 53, 227–230 (1993).
Barinka, C. et al. Selection and characterization of Anticalins targeting human prostate-specific membrane antigen (PSMA). Protein Eng. Des. Sel. 29, 105–115 (2016).
Pinto, J. T. et al. Prostate-specific membrane antigen: a novel folate hydrolase in human prostatic carcinoma cells. Clin. Cancer Res. 2, 1445–1451 (1996).
Paschalis, A. et al. Prostate-specific membrane antigen heterogeneity and DNA repair defects in prostate cancer. Eur. Urol. 76, 469–478 (2019).
Bostwick, D. G., Pacelli, A., Blute, M., Roche, P. & Murphy, G. P. Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: a study of 184 cases. Cancer 82, 2256–2261 (1998).
Mannweiler, S. et al. Heterogeneity of prostate-specific membrane antigen (PSMA) expression in prostate carcinoma with distant metastasis. Pathol. Oncol. Res. 15, 167–172 (2009).
Kaittanis, C. et al. Prostate-specific membrane antigen cleavage of vitamin B9 stimulates oncogenic signaling through metabotropic glutamate receptors. J. Exp. Med. 215, 159–175 (2018).
Caromile, L. A. & Shapiro, L. H. PSMA redirects MAPK to PI3K-AKT signaling to promote prostate cancer progression. Mol. Cell. Oncol. 4, e1321168 (2017).
Shorning, B. Y., Dass, M. S., Smalley, M. J. & Pearson, H. B. The PI3K-AKT-mTOR pathway and prostate cancer: at the crossroads of AR, MAPK, and WNT signaling. Int. J. Mol. Sci. 21, 4507 (2020).
Xu, L. et al. Screening and identification of significant genes related to tumor metastasis and PSMA in prostate cancer using microarray analysis. Oncol. Rep. 30, 1920–1928 (2013).
Wu, J. et al. A novel fully human antibody targeting extracellular domain of PSMA inhibits tumor growth in prostate cancer. Mol. Cancer Ther. 18, 1289–1301 (2019).
Su, Y. et al. PSMA specific single chain antibody-mediated targeted knockdown of Notch1 inhibits human prostate cancer cell proliferation and tumor growth. Cancer Lett. 338, 282–291 (2013).
Kuroda, K. & Liu, H. The proteasome inhibitor, bortezomib, induces prostate cancer cell death by suppressing the expression of prostate-specific membrane antigen, as well as androgen receptor. Int. J. Oncol. 54, 1357–1366 (2019).
Weidle, U. H., Epp, A., Birzele, F. & Brinkmann, U. The functional role of prostate cancer metastasis-related Micro-RNAs. Cancer Genomics Proteom. 16, 1–19 (2019).
Vummidi Giridhar, P., Williams, K., VonHandorf, A. P., Deford, P. L. & Kasper, S. Constant degradation of the androgen receptor by MDM2 conserves prostate cancer stem cell integrity. Cancer Res. 79, 1124–1137 (2019).
Zhou, Y., Bolton, E. C. & Jones, J. O. Androgens and androgen receptor signaling in prostate tumorigenesis. J. Mol. Endocrinol. 54, R15–R29 (2015).
Shore, N. D., Abrahamsson, P. A., Anderson, J., Crawford, E. D. & Lange, P. New considerations for ADT in advanced prostate cancer and the emerging role of GnRH antagonists. Prostate Cancer Prostatic Dis. 16, 7–15 (2013).
Bakht, M. K. et al. Influence of androgen deprivation therapy on the uptake of PSMA-targeted agents: emerging opportunities and challenges. Nucl. Med. Mol. Imaging 51, 202–211 (2017).
Vaz, S. et al. Influence of androgen deprivation therapy on PSMA expression and PSMA-ligand PET imaging of prostate cancer patients. Eur. J. Nucl. Med. Mol. Imaging 47, 9–15 (2020).
Roy, J. et al. Monitoring PSMA responses to ADT in prostate cancer patient-derived xenograft mouse models using [18F]DCFPyL PET imaging. Mol. Imaging Biol. 23, 745–755 (2021).
Hope, T. A. et al. 68Ga-PSMA-11 PET imaging of response to androgen receptor inhibition: first human experience. J. Nucl. Med. 58, 81–84 (2017).
Mei, R. et al. Androgen deprivation therapy and its modulation of PSMA expression in prostate cancer: mini review and case series of patients studied with sequential [68Ga]-Ga-PSMA-11 PET/CT. Clin. Transl. Imaging 9, 215–220 (2021).
Leitsmann, C. et al. Enhancing PSMA-uptake with androgen deprivation therapy — a new way to detect prostate cancer metastases? Int. Braz. J. Urol. 45, 459–467 (2019).
Ettala, O. et al. Prospective study on the effect of short-term androgen deprivation therapy on PSMA uptake evaluated with 68Ga-PSMA-11 PET/MRI in men with treatment-naïve prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 47, 665–673 (2020).
Liu, T., Wu, L. Y., Fulton, M. D., Johnson, J. M. & Berkman, C. E. Prolonged androgen deprivation leads to downregulation of androgen receptor and prostate-specific membrane antigen in prostate cancer cells. Int. J. Oncol. 41, 2087–2092 (2012).
Afshar-Oromieh, A. et al. Impact of long-term androgen deprivation therapy on PSMA ligand PET/CT in patients with castration-sensitive prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 45, 2045–2054 (2018).
Hoberück, S. et al. [68Ga]Ga-PSMA-11 PET before and after initial long-term androgen deprivation in patients with newly diagnosed prostate cancer: a retrospective single-center study. EJNMMI Res. 10, 135 (2020).
Wright, G. L. Jr et al. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urology 48, 326–334 (1996).
Chen, M. et al. Can 68Ga-PSMA-11 positron emission tomography/computerized tomography predict pathological response of primary prostate cancer to neoadjuvant androgen deprivation therapy? A pilot study. J. Urol. 205, 1082–1089 (2021).
Murga, J. D. et al. Synergistic co-targeting of prostate-specific membrane antigen and androgen receptor in prostate cancer. Prostate 75, 242–254 (2015).
Evans, M. J. et al. Noninvasive measurement of androgen receptor signaling with a positron-emitting radiopharmaceutical that targets prostate-specific membrane antigen. Proc. Natl Acad. Sci. USA 108, 9578–9582 (2011).
Emmett, L. et al. Rapid modulation of PSMA expression by androgen deprivation: serial 68Ga-PSMA-11 PET in men with hormone-sensitive and castrate-resistant prostate cancer commencing androgen blockade. J. Nucl. Med. 60, 950–954 (2019).
Minner, S. et al. High level PSMA expression is associated with early PSA recurrence in surgically treated prostate cancer. Prostate 71, 281–288 (2011).
Bakht, M. K. et al. Neuroendocrine differentiation of prostate cancer leads to PSMA suppression. Endocr. Relat. Cancer 26, 131–146 (2018).
Ross, J. S. et al. Correlation of primary tumor prostate-specific membrane antigen expression with disease recurrence in prostate cancer. Clin. Cancer Res. 9, 6357–6362 (2003).
Marchal, C. et al. Expression of prostate specific membrane antigen (PSMA) in prostatic adenocarcinoma and prostatic intraepithelial neoplasia. Histol. Histopathol. 19, 715–718 (2004).
Kasperzyk, J. L. et al. Prostate-specific membrane antigen protein expression in tumor tissue and risk of lethal prostate cancer. Cancer Epidemiol. Biomark. Prev. 22, 2354–2363 (2013).
McEwan, L. M., Wong, D. & Yaxley, J. Fluorodeoxyglucose positron emission tomography scan may be helpful in the case of ductal variant prostate cancer when prostate specific membrane antigen ligand positron emission tomography scan is negative. J. Med. Imaging Radiat. Oncol. 61, 503–505 (2017).
Shetty, D. et al. Non-prostate-specific membrane antigen-avid metastatic lung nodule from primary prostatic adenocarcinoma. Clin. Nucl. Med. 41, 776–778 (2016).
Hupe, M. C. et al. Expression of prostate-specific membrane antigen (PSMA) on biopsies is an independent risk stratifier of prostate cancer patients at time of initial diagnosis. Front. Oncol. 8, 623 (2018).
Ferraro, D. A. et al. Immunohistochemical PSMA expression patterns of primary prostate cancer tissue are associated with the detection rate of biochemical recurrence with 68Ga-PSMA-11-PET. Theranostics 10, 6082–6094 (2020).
Vlachostergios, P. J. et al. Prostate-specific membrane antigen uptake and survival in metastatic castration-resistant prostate cancer. Front. Oncol. 11, 630589 (2021).
Kratochwil, C. et al. Patients resistant against PSMA-targeting α-radiation therapy often harbor mutations in DNA damage-repair–associated genes. J. Nucl. Med. 61, 683–688 (2020).
Derlin, T. et al. Neuroendocrine differentiation and response to PSMA-targeted radioligand therapy in advanced metastatic castration-resistant prostate cancer: a single-center retrospective study. J. Nucl. Med. 61, 1602–1606 (2020).
Farwell, M. D., Pryma, D. A. & Mankoff, D. A. PET/CT imaging in cancer: current applications and future directions. Cancer 120, 3433–3445 (2014).
de Jong, I. J., Pruim, J., Elsinga, P. H., Vaalburg, W. & Mensink, H. J. A. 11C-Choline positron emission tomography for the evaluation after treatment of localized prostate cancer. Eur. Urol. 44, 32–39 (2003).
Nanni, C. et al. 18F-Fluciclovine PET/CT for the detection of prostate cancer relapse: a comparison to 11C-choline PET/CT. Clin. Nucl. Med. 40, e386–e391 (2015).
Pomper, M. G. et al. 11C-MCG: synthesis, uptake selectivity, and primate PET of a probe for glutamate carboxypeptidase II (NAALADase). Mol. Imaging 1, 96–101 (2002).
Mease, R. C. et al.N-[N-[(S)-1,3-Dicarboxypropyl]carbamoyl]-4-[18F]fluorobenzyl-L-cysteine, [18F]DCFBC: a new imaging probe for prostate cancer. Clin. Cancer Res. 14, 3036–3043 (2008).
Tateishi, U. Prostate-specific membrane antigen (PSMA)-ligand positron emission tomography and radioligand therapy (RLT) of prostate cancer. Jpn. J. Clin. Oncol. 50, 349–356 (2020).
Zippel, C., Ronski, S. C., Bohnet-Joschko, S., Giesel, F. L. & Kopka, K. Current status of PSMA-radiotracers for prostate cancer: data analysis of prospective trials listed on ClinicalTrials.gov. Pharmaceuticals 13, 12 (2020).
Banerjee, S. R. et al. 68Ga-labeled inhibitors of prostate-specific membrane antigen (PSMA) for imaging prostate cancer. J. Med. Chem. 53, 5333–5341 (2010).
Eder, M. et al. 68Ga-complex lipophilicity and the targeting property of a urea-based PSMA inhibitor for PET imaging. Bioconjug. Chem. 23, 688–697 (2012).
Afshar-Oromieh, A. et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur. J. Nucl. Med. Mol. Imaging 40, 486–495 (2013).
Morigi, J. J. et al. Prospective comparison of 18F-fluoromethylcholine versus 68Ga-PSMA PET/CT in prostate cancer patients who have rising PSA after curative treatment and are being considered for targeted therapy. J. Nucl. Med. 56, 1185–1190 (2015).
Afshar-Oromieh, A., Haberkorn, U., Eder, M., Eisenhut, M. & Zechmann, C. M. [68Ga]Gallium-labelled PSMA ligand as superior PET tracer for the diagnosis of prostate cancer: comparison with 18F-FECH. Eur. J. Nucl. Med. Mol. Imaging 39, 1085–1086 (2012).
Giesel, F. L. et al. 18F-Labelled PSMA-1007 shows similarity in structure, biodistribution and tumour uptake to the theragnostic compound PSMA-617. Eur. J. Nucl. Med. Mol. Imaging 43, 1929–1930 (2016).
Cardinale, J. et al. Preclinical evaluation of 18F-PSMA-1007, a new prostate-specific membrane antigen ligand for prostate cancer imaging. J. Nucl. Med. 58, 425–431 (2017).
Szabo, Z. et al. Initial evaluation of [18F]DCFPyL for prostate-specific membrane antigen (PSMA)-targeted PET imaging of prostate cancer. Mol. Imaging Biol. 17, 565–574 (2015).
Kesch, C., Kratochwil, C., Mier, W., Kopka, K. & Giesel, F. L. 68Ga or 18F for prostate cancer imaging? J. Nucl. Med. 58, 687–688 (2017).
Alberts, I. L. et al. Comparing the diagnostic performance of radiotracers in recurrent prostate cancer: a systematic review and network meta-analysis. Eur. J. Nucl. Med. Mol. Imaging 48, 2978–2989 (2021).
Evangelista, L. et al. [68Ga]Ga-PSMA versus [18F]PSMA positron emission tomography/computed tomography in the staging of primary and recurrent prostate cancer: a systematic review of the literature. Eur. Urol. Oncol. 5, 273–282 (2022).
Emmett, L., Pattison, D. A. & Roberts, M. J. All prostate-specific membrane antigen peptides are equal, but some are more equal than others. Eur. Urol. Oncol. 5, 283–284 (2022).
Afaq, A., Ell, P. J. & Bomanji, J. B. Is it time to fund routine NHS usage of PSMA PET-CT? Nucl. Med. Commun. 40, 975–979 (2019).
de Feria Cardet, R. E. et al. Is prostate-specific membrane antigen positron emission tomography/computed tomography imaging cost-effective in prostate cancer: an analysis informed by the proPSMA trial. Eur. Urol. 79, 413–418 (2021).
Gordon, L. G., Elliott, T. M., Joshi, A., Williams, E. D. & Vela, I. Exploratory cost-effectiveness analysis of 68Gallium-PSMA PET/MRI-based imaging in patients with biochemical recurrence of prostate cancer. Clin. Exp. Metastasis 37, 305–312 (2020).
Schwenck, J. et al. Intention-to-treat analysis of 68Ga-PSMA and 11C-Choline PET/CT versus CT for prostate cancer recurrence after surgery. J. Nucl. Med. 60, 1359–1365 (2019).
Shariat, S. F., Kattan, M. W., Vickers, A. J., Karakiewicz, P. I. & Scardino, P. T. Critical review of prostate cancer predictive tools. Fut. Oncol. 5, 1555–1584 (2009).
Briganti, A. et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur. Urol. 61, 480–487 (2012).
Gandaglia, G. et al. Development and internal validation of a novel model to identify the candidates for extended pelvic lymph node dissection in prostate cancer. Eur. Urol. 72, 632–640 (2017).
Eifler, J. B. et al. An updated prostate cancer staging nomogram (Partin tables) based on cases from 2006 to 2011. BJU Int. 111, 22–29 (2013).
Cimino, S. et al. Comparison between Briganti, Partin and MSKCC tools in predicting positive lymph nodes in prostate cancer: a systematic review and meta-analysis. Scand. J. Urol. 51, 345–350 (2017).
Bandini, M. et al. First North American validation and head-to-head comparison of four preoperative nomograms for prediction of lymph node invasion before radical prostatectomy. BJU Int. 121, 592–599 (2018).
Rayn, K. N. et al. Added value of multiparametric magnetic resonance imaging to clinical nomograms for predicting adverse pathology in prostate cancer. J. Urol. 200, 1041–1047 (2018).
Gandaglia, G. et al. A novel nomogram to identify candidates for extended pelvic lymph node dissection among patients with clinically localized prostate cancer diagnosed with magnetic resonance imaging-targeted and systematic biopsies. Eur. Urol. 75, 506–514 (2019).
Eggener, S. E. et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J. Urol. 185, 869–875 (2011).
Ost, P. et al. Prognostic factors influencing prostate cancer-specific survival in non-castrate patients with metastatic prostate cancer. Prostate 74, 297–305 (2014).
Perera, M. et al. Gallium-68 prostate-specific membrane antigen positron emission tomography in advanced prostate cancer-updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: a systematic review and meta-analysis. Eur. Urol. 77, 403–417 (2020).
Yaxley, J. W. et al. Risk of metastatic disease on 68gallium-prostate-specific membrane antigen positron emission tomography/computed tomography scan for primary staging of 1253 men at the diagnosis of prostate cancer. BJU Int. 124, 401–407 (2019).
Simsek, D. H., Sanli, Y., Engin, M. N., Erdem, S. & Sanli, O. Detection of metastases in newly diagnosed prostate cancer by using 68Ga-PSMA PET/CT and its relationship with modified D’Amico risk classification. Eur. J. Nucl. Med. Mol. Imaging 48, 1639–1649 (2021).
Maurer, T. et al. Diagnostic efficacy of 68Gallium-PSMA positron emission tomography compared to conventional imaging for lymph node staging of 130 consecutive patients with intermediate to high risk prostate cancer. J. Urol. 195, 1436–1443 (2016).
Uprimny, C. et al. 68Ga-PSMA-11 PET/CT in primary staging of prostate cancer: PSA and Gleason score predict the intensity of tracer accumulation in the primary tumour. Eur. J. Nucl. Med. Mol. Imaging 44, 941–949 (2017).
Sathekge, M. et al. 68Ga-PSMA-11 PET/CT in primary staging of prostate carcinoma: preliminary results on differences between black and white South-Africans. Eur. J. Nucl. Med. Mol. Imaging 45, 226–234 (2018).
Roberts, M. J. et al. 68Ga-PSMA PET/CT tumour intensity pre-operatively predicts adverse pathological outcomes and progression-free survival in localised prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 48, 477–482 (2021).
Jansen, B. H. E. et al. Pelvic lymph-node staging with 18F-DCFPyL PET/CT prior to extended pelvic lymph-node dissection in primary prostate cancer — the SALT trial. Eur. J. Nucl. Med. Mol. Imaging 48, 509–520 (2021).
Lopci, E. et al. Prospective evaluation of 68Ga-labeled prostate-specific membrane antigen ligand positron emission tomography/computed tomography in primary prostate cancer diagnosis. Eur. Urol. Focus 7, 764–771 (2021).
Bahler, C. D. et al. Prostate specific membrane antigen targeted positron emission tomography of primary prostate cancer: assessing accuracy with whole mount pathology. J. Urol. 203, 92–99 (2020).
Scheltema, M. J. et al. Diagnostic accuracy of 68Ga-prostate-specific membrane antigen (PSMA) positron-emission tomography (PET) and multiparametric (mp)MRI to detect intermediate-grade intra-prostatic prostate cancer using whole-mount pathology: impact of the addition of 68Ga-PSMA PET to mpMRI. BJU Int. 124 (Suppl. 1), 42–49 (2019).
Hicks, R. M. et al. Diagnostic accuracy of 68Ga-PSMA-11 PET/MRI compared with multiparametric MRI in the detection of prostate cancer. Radiology 289, 730–737 (2018).
Koseoglu, E. et al. Diagnostic ability of Ga-68 PSMA PET to detect dominant and non-dominant tumors, upgrading and adverse pathology in patients with PIRADS 4–5 index lesions undergoing radical prostatectomy. Prostate Cancer Prostatic Dis. 24, 202–209 (2021).
Knoedler, J. J. et al. The association of tumor volume with mortality following radical prostatectomy. Prostate Cancer Prostatic Dis. 17, 144–148 (2014).
Donato, P. et al. Improved specificity with 68Ga PSMA PET/CT to detect clinically significant lesions “invisible” on multiparametric MRI of the prostate: a single institution comparative analysis with radical prostatectomy histology. Eur. J. Nucl. Med. Mol. Imaging 46, 20–30 (2019).
Eiber, M. et al. Simultaneous 68Ga-PSMA HBED-CC PET/MRI improves the localization of primary prostate cancer. Eur. Urol. 70, 829–836 (2016).
Woo, S. et al. Prostate-specific membrane antigen positron emission tomography (PSMA-PET) for local staging of prostate cancer: a systematic review and meta-analysis. Eur. J. Hybrid. Imaging 4, 16 (2020).
Zhang, Q. et al. Comparison of 68Ga-PSMA-11 PET-CT with mpMRI for preoperative lymph node staging in patients with intermediate to high-risk prostate cancer. J. Transl. Med. 15, 230 (2017).
Wang, H. et al. PSMA-ligand uptake can serve as a novel biomarker in primary prostate cancer to predict outcome after radical prostatectomy. EJNMMI Res 11, 76 (2021).
Roberts, M. J. et al. Primary tumour PSMA intensity is an independent prognostic biomarker for biochemical recurrence-free survival following radical prostatectomy. Eur. J. Nucl. Med. Mol. Imaging 49, 3289–3294 (2022).
Ahmed, H. U. et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389, 815–822 (2017).
Donato, P. et al. Improved detection and reduced biopsies: the effect of a multiparametric magnetic resonance imaging-based triage prostate cancer pathway in a public teaching hospital. World J. Urol. 38, 371–379 (2020).
Rouvière, O. et al. Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): a prospective, multicentre, paired diagnostic study. Lancet Oncol. 20, 100–109 (2019).
van der Leest, M. et al. Head-to-head comparison of transrectal ultrasound-guided prostate biopsy versus multiparametric prostate resonance imaging with subsequent magnetic resonance-guided biopsy in biopsy-naïve men with elevated prostate-specific antigen: a large prospective multicenter clinical study. Eur. Urol. 75, 570–578 (2019).
Zhang, L. L. et al. 68Ga-PSMA PET/CT targeted biopsy for the diagnosis of clinically significant prostate cancer compared with transrectal ultrasound guided biopsy: a prospective randomized single-centre study. Eur. J. Nucl. Med. Mol. Imaging 48, 483–492 (2021).
Emmett, L. et al. The additive diagnostic value of prostate-specific membrane antigen positron emission tomography computed tomography to multiparametric magnetic resonance imaging triage in the diagnosis of prostate cancer (PRIMARY): a prospective multicentre study. Eur. Urol. 80, 682–689 (2021).
Ptasznik, G. et al. High prostate-specific membrane antigen (PSMA) positron emission tomography (PET) maximum standardized uptake value in men with PI-RADS score 4 or 5 confers a high probability of significant prostate cancer. BJU Int. https://doi.org/10.1111/bju.15736 (2022).
Fendler, W. P. et al. 68Ga-PSMA PET/CT detects the location and extent of primary prostate cancer. J. Nucl. Med. 57, 1720–1725 (2016).
Grubmuller, B. et al. PSMA ligand PET/MRI for primary prostate cancer: staging performance and clinical impact. Clin. Cancer Res. 24, 6300–6307 (2018).
Öbek, C. et al. The accuracy of 68Ga-PSMA PET/CT in primary lymph node staging in high-risk prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 44, 1806–1812 (2017).
Wong, H. S. et al. Comparative study between 68Ga-prostate-specific membrane antigen positron emission tomography and conventional imaging in the initial staging of prostate cancer. J. Med. Imaging Radiat. Oncol. 62, 816–822 (2018).
Ranasinghe, W. et al. Optimizing the diagnosis and management of ductal prostate cancer. Nat. Rev. Urol. 18, 337–358 (2021).
McEwan, L., McBean, R., Yaxley, J. & Wong, D. Unexpected significant findings non-related to prostate cancer identified using combined prostate-specific membrane antigen positron emission tomography/CT and diagnostic CT scan in primary staging for prostate cancer. J. Med. Imaging Radiat. Oncol. 63, 318–323 (2019).
Lawrence, M. G. et al. Knowing what’s growing: why ductal and intraductal prostate cancer matter. Sci. Transl. Med. 12, eaaz0152 (2020).
Aggarwal, R., Zhang, T., Small, E. J. & Armstrong, A. J. Neuroendocrine prostate cancer: subtypes, biology, and clinical outcomes. J. Natl Compr. Canc. Netw. 12, 719–726 (2014).
Thalgott, M. et al. One-stop-shop whole-body 68Ga-PSMA-11 PET/MRI compared with clinical nomograms for preoperative T and N staging of high-risk prostate cancer. J. Nucl. Med. 59, 1850–1856 (2018).
Donato, P. et al. 68Ga-PSMA PET/CT better characterises localised prostate cancer after MRI and transperineal prostate biopsy: is 68Ga-PSMA PET/CT guided biopsy the future? Eur. J. Nucl. Med. Mol. Imaging 47, 1843–1851 (2020).
Petersen, L. J. & Zacho, H. D. PSMA PET for primary lymph node staging of intermediate and high-risk prostate cancer: an expedited systematic review. Cancer Imaging 20, 10 (2020).
Hofman, M. S. et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet 395, 1208–1216 (2020).
Hope, T. A. et al. Metaanalysis of 68Ga-PSMA-11 PET accuracy for the detection of prostate cancer validated by histopathology. J. Nucl. Med. 60, 786–793 (2019).
Rowe, S. et al. Results from the OSPREY trial: a prospective phase 2/3 multi-center study of 18F-DCFPyL PET/CT imaging in patients with prostate cancer — examination of diagnostic accuracy. J. Nucl. Med. 60, 586–586 (2019).
Hope, T. A. et al. Accuracy of 68Ga-PSMA-11 for pelvic nodal metastasis detection prior to radical prostatectomy and pelvic lymph node dissection: a multicenter prospective phase III imaging study. J. Clin. Oncol. 38, 5502–5502 (2020).
Ferraro, D. A. et al. 68Ga-PSMA-11 PET has the potential to improve patient selection for extended pelvic lymph node dissection in intermediate to high-risk prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 47, 147–159 (2020).
van Leeuwen, P. J. et al. Gallium-68-prostate-specific membrane antigen (68Ga-PSMA) positron emission tomography (PET)/computed tomography (CT) predicts complete biochemical response from radical prostatectomy and lymph node dissection in intermediate- and high-risk prostate cancer. BJU Int. 124, 62–68 (2019).
Meijer, D. et al. The predictive value of preoperative negative prostate specific membrane antigen positron emission tomography imaging for lymph node metastatic prostate cancer. J. Urol. 205, 1655–1662 (2021).
Meijer, D. et al. External validation and addition of prostate-specific membrane antigen positron emission tomography to the most frequently used nomograms for the prediction of pelvic lymph-node metastases: an international multicenter study. Eur. Urol. 80, 234–242 (2021).
Dekalo, S. et al. Preoperative 68Ga-PSMA PET/CT defines a subgroup of high-risk prostate cancer patients with favorable outcomes after radical prostatectomy and lymph node dissection. Prostate Cancer Prostatic Dis. 24, 910–916 (2021).
Meijer, D. et al. Predicting early outcomes in patients with intermediate- and high-risk prostate cancer using prostate-specific membrane antigen positron emission tomography and magnetic resonance imaging. BJU Int. 129, 54–62 (2022).
Amiel, T. et al. Regional lymph node metastasis on PSMA PET correlates with decreased BCR-free and therapy-free survival after radical prostatectomy: a retrospective single-center single-arm observational study. J. Urol. 205, 1663–1670 (2021).
Wu, S. Y. et al. Impact of staging 68Ga-PSMA-11 PET scans on radiation treatment plans in patients with prostate cancer. Urology 125, 154–162 (2019).
Calais, J. et al. Potential impact of 68Ga-PSMA-11 PET/CT on the planning of definitive radiation therapy for prostate cancer. J. Nucl. Med. 59, 1714–1721 (2018).
Hruby, G. et al. 68Ga-PSMA-PET/CT staging prior to definitive radiation treatment for prostate cancer. Asia Pac. J. Clin. Oncol. 14, 343–346 (2018).
Donswijk, M. L. et al. Clinical impact of PSMA PET/CT in primary prostate cancer compared to conventional nodal and distant staging: a retrospective single center study. BMC Cancer 20, 723 (2020).
Gandaglia, G. et al. Prostate-specific membrane antigen imaging in clinical guidelines: European Association of Urology, National Comprehensive Cancer Network, and beyond. Eur. Urol. Focus. 7, 245–249 (2021).
Sanda, M. G. et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options. J. Urol. 199, 683–690 (2018).
Mason, B. R. et al. Current status of MRI and PET in the NCCN guidelines for prostate cancer. J. Natl Compr. Canc. Netw. 17, 506–513 (2019).
Castro, E. et al. Effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment for localised prostate cancer. Eur. Urol. 68, 186–193 (2015).
Gerhauser, C. et al. Molecular evolution of early-onset prostate cancer identifies molecular risk markers and clinical trajectories. Cancer Cell 34, 996–1011.e8 (2018).
Erho, N. et al. Discovery and validation of a prostate cancer genomic classifier that predicts early metastasis following radical prostatectomy. PLoS One 8, e66855 (2013).
Klein, E. A. et al. A genomic classifier improves prediction of metastatic disease within 5 years after surgery in node-negative high-risk prostate cancer patients managed by radical prostatectomy without adjuvant therapy. Eur. Urol. 67, 778–786 (2015).
Jairath, N. K. et al. A systematic review of the evidence for the decipher genomic classifier in prostate cancer. Eur. Urol. 79, 374–383 (2021).
Taylor, A. S. et al. Correlation between cribriform/intraductal prostatic adenocarcinoma and percent Gleason pattern 4 to a 22-gene genomic classifier. Prostate 80, 146–152 (2020).
Xu, M. J. et al. Genomic risk predicts molecular imaging-detected metastatic nodal disease in prostate cancer. Eur. Urol. Oncol. 2, 685–690 (2019).
Chu, C. E. et al. Prostate-specific membrane antigen and fluciclovine transporter genes are associated with variable clinical features and molecular subtypes of primary prostate cancer. Eur. Urol. 79, 717–721 (2021).
Kesch, C. et al. Correlation between genomic index lesions and mpMRI and 68Ga-PSMA-PET/CT imaging features in primary prostate cancer. Sci. Rep. 8, 16708 (2018).
Kasivisvanathan, V. et al. Magnetic resonance imaging-targeted biopsy versus systematic biopsy in the detection of prostate cancer: a systematic review and meta-analysis. Eur. Urol. 76, 284–303 (2019).
Van den Broeck, T. et al. Prognostic value of biochemical recurrence following treatment with curative intent for prostate cancer: a systematic review. Eur. Urol. 75, 967–987 (2019).
Saad, F., Olsson, C. & Schulman, C. C. Skeletal morbidity in men with prostate cancer: quality-of-life considerations throughout the continuum of care. Eur. Urol. 46, 731–739 (2004).
Fendler, W. P. et al. Assessment of 68Ga-PSMA-11 PET accuracy in localizing recurrent prostate cancer: a prospective single-arm clinical trial. JAMA Oncol. 5, 856–863 (2019).
Calais, J. et al. 18F-fluciclovine PET-CT and 68Ga-PSMA-11 PET-CT in patients with early biochemical recurrence after prostatectomy: a prospective, single-centre, single-arm, comparative imaging trial. Lancet Oncol. 9, 1286–1294 (2019).
Lieng, H. et al. Radiotherapy for recurrent prostate cancer: 2018 recommendations of the Australian and New Zealand Radiation Oncology Genito-Urinary group. Radiother. Oncol. 129, 377–386 (2018).
Gillessen, S. et al. Management of patients with advanced prostate cancer: report of the Advanced Prostate Cancer Consensus Conference 2019. Eur. Urol. 77, 508–547 (2020).
Abramowitz, M. C. et al. The Phoenix definition of biochemical failure predicts for overall survival in patients with prostate cancer. Cancer 112, 55–60 (2008).
Ceci, F. et al. 68Ga-PSMA-11 PET/CT in recurrent prostate cancer: efficacy in different clinical stages of PSA failure after radical therapy. Eur. J. Nucl. Med. Mol. Imaging 46, 31–39 (2019).
Preisser, F. et al. Persistent prostate-specific antigen after radical prostatectomy and its impact on oncologic outcomes. Eur. Urol. 76, 106–114 (2019).
Deandreis, D. et al. 68Ga-PSMA-11 PET/CT in recurrent hormone-sensitive prostate cancer (HSPC): a prospective single-centre study in patients eligible for salvage therapy. Eur. J. Nucl. Med. Mol. Imaging 47, 2804–2815 (2020).
Schmidt-Hegemann, N. S. et al. Outcome after PSMA PET/CT based radiotherapy in patients with biochemical persistence or recurrence after radical prostatectomy. Radiat. Oncol. 13, 37 (2018).
Meijer, D. et al. Biochemical persistence of prostate-specific antigen after robot-assisted laparoscopic radical prostatectomy: tumor localizations using PSMA PET/CT imaging. J. Nucl. Med. 62, 961–967 (2021).
Ceci, F. et al. Prediction nomogram for 68Ga-PSMA-11 PET/CT in different clinical settings of PSA failure after radical treatment for prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 47, 136–146 (2020).
Ceci, F. et al. Event-free survival after 68Ga-PSMA-11 PET/CT in recurrent hormone-sensitive prostate cancer (HSPC) patients eligible for salvage therapy. Eur. J. Nucl. Med. Mol. Imaging 49, 3257–3268 (2022).
Yilmaz, U., Komek, H., Can, C. & Altindag, S. The role of (68Ga)PSMA I&T in biochemical recurrence after radical prostatectomy: detection rate and the correlation between the level of PSA, Gleason score, and the SUVmax. Ann. Nucl. Med. 33, 545–553 (2019).
Dong, L. et al. Prospective evaluation of 68Ga-PSMA-11 PET/CT in Chinese men with biochemical recurrence after radical prostatectomy for prostate cancer: relationships between location of recurrence, time after prostatectomy, and serum PSA level. Med. Oncol. 37, 89 (2020).
Francolini, G. et al. Detection rate, pattern of relapse and influence on therapeutic decision of PSMA PET/CT in patients affected by biochemical recurrence after radical prostatectomy, a retrospective case series. Clin. Transl. Oncol. 23, 364–371 (2021).
Sonni, I. et al. Impact of 68Ga-PSMA-11 PET/CT on staging and management of prostate cancer patients in various clinical settings: a prospective single-center study. J. Nucl. Med. 61, 1153–1160 (2020).
Liu, W. et al. Utilization of salvage and systemic therapies for recurrent prostate cancer as a result of 18F-DCFPyL PET/CT restaging. Adv. Radiat. Oncol. 6, 100553 (2021).
Emmett, L. et al. Treatment outcomes from 68Ga-PSMA PET/CT-informed salvage radiation treatment in men with rising PSA after radical prostatectomy: prognostic value of a negative PSMA PET. J. Nucl. Med. 58, 1972–1976 (2017).
Emmett, L. et al. 3-Year freedom from progression after 68Ga-PSMA PET/CT-triaged management in men with biochemical recurrence after radical prostatectomy: results of a prospective multicenter trial. J. Nucl. Med. 61, 866–872 (2020).
Emmett, L. et al. Prospective, multisite, international comparison of 18F-fluoromethylcholine PET/CT, multiparametric MRI, and 68Ga-HBED-CC PSMA-11 PET/CT in men with high-risk features and biochemical failure after radical prostatectomy: clinical performance and patient outcomes. J. Nucl. Med. 60, 794–800 (2019).
Muller, J. et al. Clinical impact of 68Ga-PSMA-11 PET on patient management and outcome, including all patients referred for an increase in PSA level during the first year after its clinical introduction. Eur. J. Nucl. Med. Mol. Imaging 46, 889–900 (2019).
Celli, M. et al. Clinical value of negative 68Ga-PSMA PET/CT in the management of biochemical recurrent prostate cancer patients. Eur. J. Nucl. Med. Mol. Imaging 48, 87–94 (2021).
Mjaess, G. et al. Is there a role for repeating PSMA PET/CT after a negative scan in biochemical recurrent prostate cancer. Acta Oncol. 59, 1397–1400 (2020).
Thompson, I. M. et al. Adjuvant radiotherapy for pathological T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: long-term followup of a randomized clinical trial. J. Urol. 181, 956–962 (2009).
Bolla, M. et al. Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomised controlled trial (EORTC trial 22911). Lancet 380, 2018–2027 (2012).
Wiegel, T. et al. Adjuvant radiotherapy versus wait-and-see after radical prostatectomy: 10-year follow-up of the ARO 96-02/AUO AP 09/95 trial. Eur. Urol. 66, 243–250 (2014).
Hackman, G. et al. Randomised trial of adjuvant radiotherapy following radical prostatectomy versus radical prostatectomy alone in prostate cancer patients with positive margins or extracapsular extension. Eur. Urol. 76, 586–595 (2019).
Vale, C. L. et al. Adjuvant or early salvage radiotherapy for the treatment of localised and locally advanced prostate cancer: a prospectively planned systematic review and meta-analysis of aggregate data. Lancet 396, 1422–1431 (2020).
Kneebone, A. et al. Adjuvant radiotherapy versus early salvage radiotherapy following radical prostatectomy (TROG 08.03/ANZUP RAVES): a randomised, controlled, phase 3, non-inferiority trial. Lancet Oncol. 21, 1331–1340 (2020).
Roberts, M. J. et al. Event-free survival after radical prostatectomy according to prostate-specific membrane antigen-positron emission tomography and European Association of Urology biochemical recurrence risk groups. BJU Int. https://doi.org/10.1111/bju.15762 (2022).
Schmidt-Hegemann, N. S. et al. Outcome after PSMA PET/CT based salvage radiotherapy in patients with biochemical recurrence after radical prostatectomy: a bi-institutional retrospective analysis. J. Nucl. Med. 60, 227–233 (2019).
Zamboglou, C. et al. Metastasis-free survival and patterns of distant metastatic disease after prostate-specific membrane antigen positron emission tomography (PSMA-PET)-guided salvage radiation therapy in recurrent or persistent prostate cancer after prostatectomy. Int. J. Radiat. Oncol. Biol. Phys. 113, 1015–1024 (2022).
Calais, J., Czernin, J., Fendler, W. P., Elashoff, D. & Nickols, N. G. Randomized prospective phase III trial of 68Ga-PSMA-11 PET/CT molecular imaging for prostate cancer salvage radiotherapy planning [PSMA-SRT]. BMC Cancer 19, 18 (2019).
Feng, F. Y. et al. Validation of a 22-gene genomic classifier in patients with recurrent prostate cancer: an ancillary study of the NRG/RTOG 9601 randomized clinical trial. JAMA Oncol. 7, 544–552 (2021).
Hruby, G. et al. Delineating biochemical failure with 68Ga-PSMA-PET following definitive external beam radiation treatment for prostate cancer. Radiother. Oncol. 122, 99–102 (2017).
Raveenthiran, S. et al. The use of 68Ga-PET/CT PSMA to determine patterns of disease for biochemically recurrent prostate cancer following primary radiotherapy. Prostate Cancer Prostatic Dis. 22, 385–390 (2019).
Jansen, B. H. E. et al. Detection of recurrent prostate cancer using prostate-specific membrane antigen positron emission tomography in patients not meeting the phoenix criteria for biochemical recurrence after curative radiotherapy. Eur. Urol. Oncol. 5, 821–825 (2020).
Einspieler, I. et al. Detection efficacy of hybrid 68Ga-PSMA ligand PET/CT in prostate cancer patients with biochemical recurrence after primary radiation therapy defined by phoenix criteria. J. Nucl. Med. 58, 1081–1087 (2017).
Fendler, W. P. et al. False positive PSMA PET for tumor remnants in the irradiated prostate and other interpretation pitfalls in a prospective multi-center trial. Eur. J. Nucl. Med. Mol. Imaging 48, 501–508 (2021).
Lamb, D. S. et al. Relapse patterns after low-dose-rate prostate brachytherapy. Brachytherapy 20, 291–295 (2020).
Liu, W. et al. A prospective study of 18F-DCFPyL PSMA PET/CT restaging in recurrent prostate cancer following primary external beam radiotherapy or brachytherapy. Int. J. Radiat. Oncol. Biol. Phys. 106, 546–555 (2020).
Hope, T. A. et al. Imaging prostate cancer with prostate-specific membrane antigen PET/CT and PET/MRI: current and future applications. AJR Am. J. Roentgenol. 211, 286–294 (2018).
Trabulsi, E. J. et al. Optimum imaging strategies for advanced prostate cancer: ASCO guideline. J. Clin. Oncol. 38, 1963–1996 (2020).
Aluwini, S. et al. M1a prostate cancer: results of a Dutch multidisciplinary consensus meeting. BJUI Compass 2, 159–168 (2021).
National Comprehensive Cancer Network. NCCN Guidelines: prostate cancer. NCCN https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1459 (2022).
Anttinen, M. et al. A prospective comparison of 18F-prostate-specific membrane antigen-1007 positron emission tomography computed tomography, whole-body 1.5 T magnetic resonance imaging with diffusion-weighted imaging, and single-photon emission computed tomography/computed tomography with traditional imaging in primary distant metastasis staging of prostate cancer (PROSTAGE). Eur. Urol. Oncol. 4, 635–644 (2020).
Lengana, T. et al. 68Ga-PSMA PET/CT replacing bone scan in the initial staging of skeletal metastasis in prostate cancer: a fait accompli? Clin. Genitourin. Cancer 16, 392–401 (2018).
Ekmekcioglu, Ö., Busstra, M., Klass, N. D. & Verzijlbergen, F. Bridging the imaging gap: PSMA PET/CT has a high impact on treatment planning in prostate cancer patients with biochemical recurrence — a narrative review of the literature. J. Nucl. Med. 60, 1394–1398 (2019).
Han, S., Woo, S., Kim, Y. J. & Suh, C. H. Impact of 68Ga-PSMA PET on the management of patients with prostate cancer: a systematic review and meta-analysis. Eur. Urol. 74, 179–190 (2018).
Calais, J. et al. 68Ga-PSMA-11 PET/CT mapping of prostate cancer biochemical recurrence after radical prostatectomy in 270 patients with a PSA level of less than 1.0 ng/mL: impact on salvage radiotherapy planning. J. Nucl. Med. 59, 230–237 (2018).
De Bruycker, A. et al. Nodal oligorecurrent prostate cancer: anatomic pattern of possible treatment failure in relation to elective surgical and radiotherapy treatment templates. Eur. Urol. 75, 826–833 (2019).
Schiller, K. et al. Patterns of failure after radical prostatectomy in prostate cancer — implications for radiation therapy planning after 68Ga-PSMA-PET imaging. Eur. J. Nucl. Med. Mol. Imaging 44, 1656–1662 (2017).
Supiot, S. et al. OLIGOPELVIS GETUG P07, a multicenter phase II trial of combined high-dose salvage radiotherapy and hormone therapy in oligorecurrent pelvic node relapses in prostate cancer. Eur. Urol. 4, 405–414 (2021).
Hellman, S. & Weichselbaum, R. R. Oligometastases. J. Clin. Oncol. 13, 8–10 (1995).
Tosoian, J. J. et al. Oligometastatic prostate cancer: definitions, clinical outcomes, and treatment considerations. Nat. Rev. Urol. 14, 15–25 (2017).
Ong, W. L. et al. Prostate-specific membrane antigen-positron emission tomography/computed tomography (PSMA-PET/CT)-guided stereotactic ablative body radiotherapy for oligometastatic prostate cancer: a single-institution experience and review of the published literature. BJU Int. 124 (Suppl. 1), 19–30 (2019).
Bowden, P. et al. Fractionated stereotactic body radiotherapy for up to five prostate cancer oligometastases: interim outcomes of a prospective clinical trial. Int. J. Cancer 146, 161–168 (2020).
Habl, G. et al. Oligometastases from prostate cancer: local treatment with stereotactic body radiotherapy (SBRT). BMC Cancer 17, 361 (2017).
Kneebone, A. et al. Stereotactic body radiotherapy for oligometastatic prostate cancer detected via prostate-specific membrane antigen positron emission tomography. Eur. Urol. Oncol. 1, 531–537 (2018).
Fanetti, G. et al. Stereotactic body radiotherapy for castration-sensitive prostate cancer bone oligometastases. Med. Oncol. 35, 75 (2018).
Siva, S. et al. Stereotactic ablative body radiotherapy (SABR) for oligometastatic prostate cancer: a prospective clinical trial. Eur. Urol. 74, 455–462 (2018).
Ost, P. et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial. J. Clin. Oncol. 36, 446–453 (2018).
Phillips, R. et al. Outcomes of observation vs stereotactic ablative radiation for oligometastatic prostate cancer: the ORIOLE phase 2 randomized clinical trial. JAMA Oncol. 6, 650–659 (2020).
Glicksman, R. M. et al. Curative-intent metastasis-directed therapies for molecularly-defined oligorecurrent prostate cancer: a prospective phase II trial testing the oligometastasis hypothesis. Eur. Urol. 3, 374–382 (2021).
Deek, M. P. et al. Long-term outcomes and genetic predictors of response to metastasis-directed therapy versus observation in oligometastatic prostate cancer: analysis of STOMP and ORIOLE trials. J. Clin. Oncol. 29, 3377–3382 (2022).
Zilli, T. et al. The multicenter, randomized, phase 2 PEACE V-STORM trial: defining the best salvage treatment for oligorecurrent nodal prostate cancer metastases. Eur. Urol. Focus. 7, 241–244 (2020).
Bravi, C. A. et al. Long-term outcomes of salvage lymph node dissection for nodal recurrence of prostate cancer after radical prostatectomy: not as good as previously thought. Eur. Urol. 78, 661–669 (2020).
Afshar-Oromieh, A. et al. Comparison of PET imaging with a 68Ga-labelled PSMA ligand and 18F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 41, 11–20 (2014).
Knipper, S. et al. Metastases-yield and prostate-specific antigen kinetics following salvage lymph node dissection for prostate cancer: a comparison between conventional surgical approach and prostate-specific membrane antigen-radioguided surgery. Eur. Urol. Focus. 5, 50–53 (2019).
Farolfi, A. et al. Mapping prostate cancer lesions before and after unsuccessful salvage lymph node dissection using repeat PSMA PET. J. Nucl. Med. 61, 1037–1042 (2020).
Maurer, T. et al. 99mTechnetium-based prostate-specific membrane antigen-radioguided surgery in recurrent prostate cancer. Eur. Urol. 75, 659–666 (2019).
Horn, T. et al. Single lesion on prostate-specific membrane antigen-ligand positron emission tomography and low prostate-specific antigen are prognostic factors for a favorable biochemical response to prostate-specific membrane antigen-targeted radioguided surgery in recurrent prostate cancer. Eur. Urol. 76, 517–523 (2019).
Knipper, S. et al. Cohort study of oligorecurrent prostate cancer patients: oncological outcomes of patients treated with salvage lymph node dissection via prostate-specific membrane antigen-radioguided surgery. Eur. Urol. https://doi.org/10.1016/j.eururo.2022.05.031 (2022).
Seitz, A. K. et al. Preliminary results on response assessment using 68Ga-HBED-CC-PSMA PET/CT in patients with metastatic prostate cancer undergoing docetaxel chemotherapy. Eur. J. Nucl. Med. Mol. Imaging 45, 602–612 (2018).
Schmidkonz, C. et al. 68Ga-PSMA-11 PET/CT derived quantitative volumetric tumor parameters for classification and evaluation of therapeutic response of bone metastases in prostate cancer patients. Ann. Nucl. Med. 33, 766–775 (2019).
Scher, H. I. et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J. Clin. Oncol. 34, 1402–1418 (2016).
Fendler, W. P. et al. Prostate-specific membrane antigen ligand positron emission tomography in men with nonmetastatic castration-resistant prostate cancer. Clin. Cancer Res. 25, 7448–7454 (2019).
Farolfi, A. et al. PSMA-PET identifies PCWG3 target populations with superior accuracy and reproducibility when compared to conventional imaging: a multicenter retrospective study. J. Nucl. Med. 62, 675–678 (2020).
Wang, B. et al. A prospective trial of 68Ga-PSMA and 18F-FDG PET/CT in nonmetastatic prostate cancer patients with an early PSA progression during castration. Clin. Cancer Res. 26, 4551–4558 (2020).
Weber, M. et al. PSMA-ligand PET for early castration-resistant prostate cancer: a retrospective single-center study. J. Nucl. Med. 62, 88–91 (2021).
Deek, M. P. et al. Metastasis-directed therapy prolongs efficacy of systemic therapy and improves clinical outcomes in oligoprogressive castration-resistant prostate cancer. Eur. Urol. Oncol. 4, 447–455 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04631601 (2022).
Afshar, M., Evison, F., James, N. D. & Patel, P. Shifting paradigms in the estimation of survival for castration-resistant prostate cancer: a tertiary academic center experience. Urol. Oncol. 33, 338.e1–7 (2015).
Staniszewska, M. et al. Drug and molecular radiotherapy combinations for metastatic castration resistant prostate cancer. Nucl. Med. Biol. 96–97, 101–111 (2021).
Plouznikoff, N. et al. Evaluation of PSMA expression changes on PET/CT before and after initiation of novel antiandrogen drugs (enzalutamide or abiraterone) in metastatic castration-resistant prostate cancer patients. Ann. Nucl. Med. 33, 945–954 (2019).
Grubmuller, B. et al. Response assessment using [68Ga]Ga-PSMA ligand PET in patients undergoing systemic therapy for metastatic castration-resistant prostate cancer. Prostate 80, 74–82 (2020).
Komek, H., Can, C., Yilmaz, U. & Altindag, S. Prognostic value of 68Ga PSMA I&T PET/CT SUV parameters on survival outcome in advanced prostate cancer. Ann. Nucl. Med. 32, 542–552 (2018).
Hofman, M. S. et al. [177Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 19, 825–833 (2018).
Thang, S. P. et al. Poor outcomes for patients with metastatic castration-resistant prostate cancer with low prostate-specific membrane antigen (PSMA) expression deemed ineligible for 177Lu-labelled PSMA radioligand therapy. Eur. Urol. Oncol. 2, 670–676 (2019).
Ferdinandus, J. et al. Prognostic biomarkers in men with metastatic castration-resistant prostate cancer receiving [177Lu]-PSMA-617. Eur. J. Nucl. Med. Mol. Imaging 47, 2322–2327 (2020).
Buteau, J. P. et al. PSMA and FDG-PET as predictive and prognostic biomarkers in patients given [177Lu]Lu-PSMA-617 versus cabazitaxel for metastatic castration-resistant prostate cancer (TheraP): a biomarker analysis from a randomised, open-label, phase 2 trial. Lancet Oncol. 23, 1389–1397 (2022).
Chen, R. et al. The added value of 18F-FDG PET/CT compared with 68Ga-PSMA PET/CT in patients with castration-resistant prostate cancer. J. Nucl. Med. 63, 69–75 (2022).
Khreish, F. et al. Value of combined PET imaging with [18F]FDG and [68Ga]Ga-PSMA-11 in mCRPC patients with worsening disease during [177Lu]Lu-PSMA-617 RLT. Cancers 13, 4134 (2021).
Chen, R. et al. Diagnostic value of 18F-FDG PET/CT in patients with biochemical recurrent prostate cancer and negative 68Ga-PSMA PET/CT. Eur. J. Nucl. Med. Mol. Imaging 48, 2970–2977 (2021).
Shen, K. et al. The evolving role of 18F-FDG PET/CT in diagnosis and prognosis prediction in progressive prostate cancer. Front. Oncol. 11, 683793 (2021).
McGeorge, S. et al. Dual-tracer positron-emission tomography using prostate-specific membrane antigen and fluorodeoxyglucose for staging of prostate cancer: a systematic review. Adv. Urol. 2021, 1544208 (2021).
Hofman, M. S. & Emmett, L. Tumour heterogeneity and resistance to therapy in prostate cancer: a fundamental limitation of prostate-specific membrane antigen theranostics or a key strength? Eur. Urol. 76, 479–481 (2019).
Emmett, L. et al. ENZA-p trial protocol: a randomised phase II trial using PSMA as a therapeutic target and prognostic indicator in men with metastatic castration-resistant prostate cancer treated with enzalutamide (ANZUP 1901). BJU Int. 128, 642–651 (2021).
Dhiantravan, N. et al. UpFrontPSMA: a randomized phase 2 study of sequential 177Lu-PSMA-617 and docetaxel vs docetaxel in metastatic hormone-naïve prostate cancer (clinical trial protocol). BJU Int. 128, 331–342 (2021).
Pouliot, F. et al. The triple-tracer strategy against metastatic prostate cancer (3TMPO) study protocol. BJU Int. 130, 314–322 (2022).
Bander, N. H. et al. Targeting metastatic prostate cancer with radiolabeled monoclonal antibody J591 to the extracellular domain of prostate specific membrane antigen. J. Urol. 170, 1717–1721 (2003).
Benešová, M. et al. Preclinical evaluation of a tailor-made DOTA-conjugated PSMA inhibitor with optimized linker moiety for imaging and endoradiotherapy of prostate cancer. J. Nucl. Med. 56, 914–920 (2015).
Kratochwil, C. et al. 225Ac-PSMA-617 for PSMA-targeted α-radiation therapy of metastatic castration-resistant prostate cancer. J. Nucl. Med. 57, 1941–1944 (2016).
Morris, M. J. et al. Radium-223 mechanism of action: implications for use in treatment combinations. Nat. Rev. Urol. 16, 745–756 (2019).
Zechmann, C. M. et al. Radiation dosimetry and first therapy results with a 124I/131I-labeled small molecule (MIP-1095) targeting PSMA for prostate cancer therapy. Eur. J. Nucl. Med. Mol. Imaging 41, 1280–1292 (2014).
Ahmadzadehfar, H. et al. 68Ga-PSMA-11 PET as a gatekeeper for the treatment of metastatic prostate cancer with 223Ra: proof of concept. J. Nucl. Med 58, 438–444 (2017).
Gafita, A. et al. Nomograms to predict outcome after LuPSMA radionuclide therapy in men with metastatic castration-resistant prostate cancer: an international multicenter retrospective study. Lancet Oncol. 22, 1115–1125 (2021).
Emmett, L. et al. Results of a prospective phase 2 pilot trial of 177Lu-PSMA-617 therapy for metastatic castration-resistant prostate cancer including imaging predictors of treatment response and patterns of progression. Clin. Genitourin. Cancer 17, 15–22 (2019).
Sartor, O. et al. Lutetium-177–PSMA-617 for metastatic castration-resistant prostate cancer. N. Engl. J. Med. 385, 1091–1103 (2021).
Fang, M., Nakazawa, M., Antonarakis, E. S. & Li, C. Efficacy of abiraterone and enzalutamide in pre- and postdocetaxel castration-resistant prostate cancer: a trial-level meta-analysis. Prostate Cancer 2017, 8560827 (2017).
Hofman, M. S. et al. TheraP: 177Lu-PSMA-617 (LuPSMA) versus cabazitaxel in metastatic castration-resistant prostate cancer (mCRPC) progressing after docetaxel — overall survival after median follow-up of 3 years (ANZUP 1603). J. Clin. Oncol. 40, 5000–5000 (2022).
Haffner, M. C. et al. Genomic and phenotypic heterogeneity in prostate cancer. Nat. Rev. Urol. 18, 79–92 (2021).
Gafita, A. et al. Interim PSMA PET/CT for response evaluation during LuPSMA treatment in mCRPC (INTERIM PET): an explorative, multicenter study. J. Clin. Oncol. 39, 5066–5066 (2021).
Gafita, A. et al. Novel framework for treatment response evaluation using PSMA-PET/CT in patients with metastatic castration-resistant prostate cancer (RECIP 1.0): an international multicenter study. J. Nucl. Med. 63, 1651–1658 (2022).
Gafita, A. et al. Measuring response in metastatic castration-resistant prostate cancer using PSMA PET/CT: comparison of RECIST 1.1, aPCWG3, aPERCIST, PPP, and RECIP 1.0 criteria. Eur. J. Nucl. Med. Mol. Imaging 49, 4271–428 (2022).
Pathmanandavel, S. et al. The prognostic value of post-treatment PSMA and FDG PET/CT in metastatic, castration-resistant prostate cancer treated with 177LuPSMA-617 and NOX66 in a phase I/II trial (LuPIN). J. Nucl. Med. https://doi.org/10.2967/jnumed.122.264104 (2022).
Deegen, P. et al. The PSMA-targeting half-life extended BiTE Therapy AMG 160 has potent antitumor activity in preclinical models of metastatic castration-resistant prostate cancer. Clin. Cancer Res. 27, 2928–2937 (2021).
Subudhi, S. K. et al. Safety and efficacy of AMG 160, a half-life extended BiTE immune therapy targeting prostate-specific membrane antigen (PSMA), and other therapies for metastatic castration-resistant prostate cancer (mCRPC). J. Clin. Oncol. 39, TPS5088–TPS5088 (2021).
Wolf, P., Alzubi, J., Gratzke, C. & Cathomen, T. The potential of CAR T cell therapy for prostate cancer. Nat. Rev. Urol. 18, 556–571 (2021).
Venkatachalam, S., McFarland, T. R., Agarwal, N. & Swami, U. Immune checkpoint inhibitors in prostate cancer. Cancers 13, 2187 (2021).
Wang, F., Li, Z., Feng, X., Yang, D. & Lin, M. Advances in PSMA-targeted therapy for prostate cancer. Prostate Cancer Prostatic Dis. 25, 11–26 (2022).
Abufaraj, M. et al. Prospective evaluation of the performance of [68Ga]Ga-PSMA-11 PET/CT(MRI) for lymph node staging in patients undergoing superextended salvage lymph node dissection after radical prostatectomy. Eur. J. Nucl. Med. Mol. Imaging 46, 2169–2177 (2019).
Author information
Authors and Affiliations
Contributions
M.J.R., T.M., M.P., S.S. and W.P.F. researched data for the article. All authors contributed substantially to discussion of the content. M.J.R., T.M., M.P., S.S., L.E. and W.P.F. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
M.J.R. is supported by a Clinician Research Fellowship from the Metro North Office of Research, Queensland Health, and a Doctor in Training Research Scholarship from Avant Mutual Group Pty Ltd. W.P.F. received financial support from the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG, grant FE1573/3-1 / 659216), IFORES (D/107-81260, D/107-30240) and Wiedenfeld-Stiftung/Stiftung Krebsforschung Duisburg. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Hossein Jadvar and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Decipher: https://decipherbio.com
Memorial Sloan Kettering Cancer Centre: https://www.mskcc.org/nomograms/prostate/pre_op
Prolaris: https://prolaris.com
Supplementary information
Glossary
- Index lesion or tumour
-
Tumour focus displaying the highest International Society of Uro-Pathology (ISUP) Grade Group, or largest diameter for the same ISUP Grade Group, according to radical prostatectomy histopathology.
- Partial volume effect
-
A concept in cross-sectional imaging in which limited imaging resolution is unable to detect small structures or tissues.
- PI3K–AKT–mTOR pathway
-
Key signalling pathway that is central to cell growth and survival in both physiological and pathological conditions.
- PSA doubling time
-
(PSADT). A unit of measurement (ng/ml/year) that estimates the rate of change for a PSA level to increase twofold from the original measurement.
- Response Evaluation Criteria in Solid Tumors
-
(RECIST). Guidelines for evaluation of the efficacy of cancer treatments according to change in tumour burden detected by imaging.
- Standardized uptake value
-
(SUV). A semiquantitative measure of tracer uptake in a region of interest that normalizes the lesion activity to the injected activity and a measure of the volume of distribution.
- Stereotactic
-
Used in techniques for precise treatment, usually radiotherapy, to targets that are localized with 3D imaging.
- Stereotactic ablative radiotherapy
-
(SABR). A radiotherapy technique that delivers high doses with high accuracy, enabling high-dose delivery with fewer effects on surrounding tissues.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roberts, M.J., Maurer, T., Perera, M. et al. Using PSMA imaging for prognostication in localized and advanced prostate cancer. Nat Rev Urol 20, 23–47 (2023). https://doi.org/10.1038/s41585-022-00670-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-022-00670-6
This article is cited by
-
Limited prognostic role of routine serum markers (AP, CEA, LDH and NSE) in oligorecurrent prostate cancer patients undergoing PSMA-radioguided surgery
World Journal of Urology (2024)
-
Health-related quality of life of metastatic prostate cancer patients treated with prostate Radiotherapy
BMC Cancer (2023)
-
PSMA-targeted fluorescence guidance for robotic-assisted prostatectomy
Nature Reviews Urology (2023)
-
PROMISE V2 — something new, something old and something borrowed
Nature Reviews Urology (2023)
-
Falsch-positive – falsch-negative Befunde – Stellenwert der PSMA-PET/CT beim Staging von Patienten mit Prostatakarzinom
Journal für Urologie und Urogynäkologie/Österreich (2023)