Abstract
Neuromyelitis optica spectrum disorder (NMOSD) is a rare inflammatory CNS disease that primarily manifests as relapsing episodes of severe optic neuritis and myelitis. Diagnosis of NMOSD is supported by the detection of IgG autoantibodies that target the aquaporin 4 (AQP4) water channel, which, in the CNS, is an astrocyte-specific protein. AQP4 antibody binding leads to AQP4 internalization, complement-dependent and antibody-dependent cellular cytotoxicity, and water channel dysfunction. Cumulative attack-related injury causes disability in NMOSD, so the prevention of attacks is expected to prevent disability accrual. Until recently, no regulator-approved therapies were available for NMOSD. Traditional immunosuppressant therapies, including mycophenolate mofetil, azathioprine and rituximab, were widely used but their benefits have not been assessed in controlled studies. In 2019 and 2020, five phase II and III randomized placebo-controlled trials of four mechanism-based therapies for NMOSD were published and demonstrated that all four effectively prolonged the time to first relapse. All four drugs were monoclonal antibodies: the complement C5 antibody eculizumab, the IL-6 receptor antibody satralizumab, the B cell-depleting antibody inebilizumab, which targets CD19, and rituximab, which targets CD20. We review the pathophysiology of NMOSD, the rationale for the development of these mechanism-based drugs, the methodology and outcomes of the five trials, and the implications of these findings for the treatment of NMOSD.
Key points
-
Improved understanding of the pathophysiological mechanisms of neuromyelitis optica spectrum disorder enabled the development and testing of targeted treatments that have now received regulatory approval.
-
Randomized trials of eculizumab, inebilizumab, satralizumab and rituximab demonstrated that all four reduced the time to protocol-defined first relapse, thereby meeting the primary end points.
-
Differences in the trial designs prevent conclusions about which drug is preferable as first-line treatment. Factors that influence treatment decisions include previous experience with therapy, efficacy, safety, accessibility, cost and convenience.
-
The accessibility and affordability of the newly approved treatments for neuromyelitis optica spectrum disorder will vary between countries and regions and will influence decisions to initiate or switch to these drugs.
-
The RIN-1 trial included too few patients for the quantification of risk reduction; however, the extensive clinical experience with rituximab and its relatively low cost mean that it will remain an important treatment option.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Lennon, V. A. et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet 364, 2106–2112 (2004). This paper reported the discovery of the NMO biomarker NMO-IgG.
Lennon, V. A., Kryzer, T. J., Pittock, S. J., Verkman, A. S. & Hinson, S. R. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J. Exp. Med. 202, 473–477 (2005). This paper reported that AQP4 is the antigenic target of NMO-IgG.
Wingerchuk, D. M. et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85, 177–189 (2015).
Wingerchuk, D. M., Hogancamp, W. F., O’Brien, P. C. & Weinshenker, B. G. The clinical course of neuromyelitis optica (Devic’s syndrome). Neurology 53, 1107–1114 (1999).
Wingerchuk, D. M., Lennon, V. A., Pittock, S. J., Lucchinetti, C. F. & Weinshenker, B. G. Revised diagnostic criteria for neuromyelitis optica. Neurology 66, 1485–1489 (2006).
Wingerchuk, D. M., Lennon, V. A., Lucchinetti, C. F., Pittock, S. J. & Weinshenker, B. G. The spectrum of neuromyelitis optica. Lancet Neurol. 6, 805–815 (2007).
Flanagan, E. P. et al. Epidemiology of aquaporin-4 autoimmunity and neuromyelitis optica spectrum. Ann. Neurol. 79, 775–783 (2016).
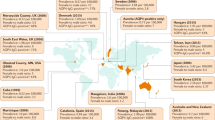
Hor, J. Y. et al. Epidemiology of neuromyelitis optica spectrum disorder and its prevalence and incidence worldwide. Front. Neurol. 11, 501 (2020).
Papp, V. et al. Worldwide incidence and prevalence of neuromyelitis optica: a systematic review. Neurology 96, 59–77 (2021).
Apiwattanakul, M. et al. Diagnostic utility of NMO/AQP4-IgG in evaluating CNS inflammatory disease in Thai patients. J. Neurol. Sci. 320, 118–120 (2012).
Nagaishi, A. et al. Clinical features of neuromyelitis optica in a large Japanese cohort: comparison between phenotypes. J. Neurol. Neurosurg. Psychiatry 82, 1360–1364 (2011).
Quek, A. M. et al. Effects of age and sex on aquaporin-4 autoimmunity. Arch. Neurol. 69, 1039–1043 (2012).
Wingerchuk, D. M., Pittock, S. J., Lucchinetti, C. F., Lennon, V. A. & Weinshenker, B. G. A secondary progressive clinical course is uncommon in neuromyelitis optica. Neurology 68, 603–605 (2007).
Jacob, A. et al. Treatment of neuromyelitis optica with rituximab: retrospective analysis of 25 patients. Arch. Neurol. 65, 1443–1448 (2008).
Costanzi, C. et al. Azathioprine: tolerability, efficacy, and predictors of benefit in neuromyelitis optica. Neurology 77, 659–666 (2011).
Kitley, J. et al. Methotrexate is an alternative to azathioprine in neuromyelitis optica spectrum disorders with aquaporin-4 antibodies. J. Neurol. Neurosurg. Psychiatry 84, 918–921 (2013).
Elsone, L. et al. Long-term efficacy, tolerability and retention rate of azathioprine in 103 aquaporin-4 antibody-positive neuromyelitis optica spectrum disorder patients: a multicentre retrospective observational study from the UK. Mult. Scler. 20, 1533–1540 (2014).
Jacob, A. et al. Treatment of neuromyelitis optica with mycophenolate mofetil: retrospective analysis of 24 patients. Arch. Neurol. 66, 1128–1133 (2009).
Kim, S. H. et al. Clinical efficacy of plasmapheresis in patients with neuromyelitis optica spectrum disorder and effects on circulating anti-aquaporin-4 antibody levels. J. Clin. Neurol. 9, 36–42 (2013).
Kim, S. H., Huh, S. Y., Lee, S. J., Joung, A. & Kim, H. J. A 5-year follow-up of rituximab treatment in patients with neuromyelitis optica spectrum disorder. JAMA Neurol. 70, 1110–1117 (2013).
Kitley, J. et al. Prognostic factors and disease course in aquaporin-4 antibody-positive patients with neuromyelitis optica spectrum disorder from the United Kingdom and Japan. Brain 135, 1834–1849 (2012).
Cree, B. A. C. et al. Inebilizumab for the treatment of neuromyelitis optica spectrum disorder (N-MOmentum): a double-blind, randomised placebo-controlled phase 2/3 trial. Lancet 394, 1352–1363 (2019).
Pittock, S. J. et al. Eculizumab in aquaporin-4-positive neuromyelitis optica spectrum disorder. N. Engl. J. Med. 381, 614–625 (2019).
Yamamura, T. et al. Trial of satralizumab in neuromyelitis optica spectrum disorder. N. Engl. J. Med. 381, 2114–2124 (2019).
Traboulsee, A. et al. Safety and efficacy of satralizumab monotherapy in neuromyelitis optica spectrum disorder: a randomised, double-blind, multicentre, placebo-controlled phase 3 trial. Lancet Neurol. 19, 402–412 (2020).
Tahara, M. et al. Safety and efficacy of rituximab in neuromyelitis optica spectrum disorders (RIN-1 study): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 19, 298–306 (2020).
Keegan, M. et al. Plasma exchange for severe attacks of CNS demyelination: predictors of response. Neurology 58, 143–146 (2002).
Watanabe, S. et al. Therapeutic efficacy of plasma exchange in NMO-IgG-positive patients with neuromyelitis optica. Mult. Scler. 13, 128–132 (2007).
Bonnan, M. et al. Plasma exchange in severe spinal attacks associated with neuromyelitis optica spectrum disorder. Mult. Scler. 15, 487–492 (2009).
Bonnan, M. & Cabre, P. Plasma exchange in severe attacks of neuromyelitis optica. Mult. Scler. Int. 2012, 787630 (2012).
Lim, Y. M., Pyun, S. Y., Kang, B. H., Kim, J. & Kim, K. K. Factors associated with the effectiveness of plasma exchange for the treatment of NMO-IgG-positive neuromyelitis optica spectrum disorders. Mult. Scler. 19, 1216–1218 (2013).
Morgan, S. M., Zantek, N. D. & Carpenter, A. F. Therapeutic plasma exchange in neuromyelitis optica: a case series. J. Clin. Apher. 29, 171–177 (2014).
Aungsumart, S. & Apiwattanakul, M. Clinical outcomes and predictive factors related to good outcomes in plasma exchange in severe attack of NMOSD and long extensive transverse myelitis: case series and review of the literature. Mult. Scler. Relat. Disord. 13, 93–97 (2017).
Kleiter, I. et al. Apheresis therapies for NMOSD attacks: a retrospective study of 207 therapeutic interventions. Neurol. Neuroimmunol. Neuroinflamm. 5, e504 (2018).
Kumawat, B. L., Choudhary, R., Sharma, C. M., Jain, D. & Hiremath, A. Plasma exchange as a first line therapy in acute attacks of neuromyelitis optica spectrum disorders. Ann. Indian Acad. Neurol. 22, 389–394 (2019).
Songthammawat, T. et al. A pilot study comparing treatments for severe attacks of neuromyelitis optica spectrum disorders: Intravenous methylprednisolone (IVMP) with add-on plasma exchange (PLEX) versus simultaneous ivmp and PLEX. Mult. Scler. Relat. Disord. 38, 101506 (2020).
Ipe, T. S. et al. Therapeutic plasma exchange for neuromyelitis optica spectrum disorder: a multicenter retrospective study by the ASFA neurologic diseases subcommittee. J. Clin. Apher. 35, 25–32 (2020).
Abboud, H. et al. Treatment of acute relapses in neuromyelitis optica: steroids alone versus steroids plus plasma exchange. Mult. Scler. J. 22, 185–192 (2016).
Mori, S., Kurimoto, T., Ueda, K. & Nakamura, M. Short-term effect of additional apheresis on visual acuity changes in patients with steroid-resistant optic neuritis in neuromyelitis optica spectrum disorders. Jpn. J. Ophthalmol. 62, 525–530 (2018).
Weinshenker, B. G. et al. A randomized trial of plasma exchange in acute central nervous system inflammatory demyelinating disease. Ann. Neurol. 46, 878–886 (1999).
Kleiter, I. et al. Neuromyelitis optica: evaluation of 871 attacks and 1,153 treatment courses. Ann. Neurol. 79, 206–216 (2016).
Weinshenker, B. G. et al. Neuromyelitis optica IgG predicts relapse after longitudinally extensive transverse myelitis. Ann. Neurol. 59, 566–569 (2006).
Matiello, M. et al. NMO-IgG predicts the outcome of recurrent optic neuritis. Neurology 70, 2197–2200 (2008).
[No authors listed] Neuromyelitis optica. Nat. Rev. Dis. Primers 6, 84 (2020).
Cree, B. A. et al. An open label study of the effects of rituximab in neuromyelitis optica. Neurology 64, 1270–1272 (2005).
Damato, V., Evoli, A. & Iorio, R. Efficacy and safety of rituximab therapy in neuromyelitis optica spectrum disorders: a systematic review and meta-analysis. JAMA Neurol. 73, 1342–1348 (2016).
Gao, F. et al. Effectiveness of rituximab in neuromyelitis optica: a meta-analysis. BMC Neurol. 19, 36 (2019).
Jeong, I. H. et al. Comparative analysis of treatment outcomes in patients with neuromyelitis optica spectrum disorder using multifaceted endpoints. Mult. Scler. 22, 329–339 (2016).
Kim, S. H. et al. Treatment outcomes with rituximab in 100 patients with neuromyelitis optica: influence of FCGR3A polymorphisms on the therapeutic response to rituximab. JAMA Neurol. 72, 989–995 (2015).
Mealy, M. A., Wingerchuk, D. M., Palace, J., Greenberg, B. M. & Levy, M. Comparison of relapse and treatment failure rates among patients with neuromyelitis optica: multicenter study of treatment efficacy. JAMA Neurol. 71, 324–330 (2014).
Nosadini, M. et al. Rituximab monitoring and redosing in pediatric neuromyelitis optica spectrum disorder. Neurol. Neuroimmunol. Neuroinflamm. 3, e188 (2016).
Poupart, J. et al. Evaluation of efficacy and tolerability of first-line therapies in NMOSD. Neurology 94, e1645–e1656 (2020).
Zephir, H. et al. Rituximab as first-line therapy in neuromyelitis optica: efficiency and tolerability. J. Neurol. 262, 2329–2335 (2015).
Giovannelli, J. et al. Meta-analysis comparing first-line immunosuppressants in neuromyelitis optica. Ann. Clin. Transl. Neurol. https://doi.org/10.1002/acn3.51451 (2021).
Greco, R. et al. Allogeneic hematopoietic stem cell transplantation for neuromyelitis optica. Ann. Neurol. 75, 447–453 (2014).
Burt, R. K. et al. Autologous nonmyeloablative hematopoietic stem cell transplantation for neuromyelitis optica. Neurology 93, e1732–e1741 (2019).
Hau, L. et al. Allogeneic haematopoietic stem cell transplantation in a refractory case of neuromyelitis optica spectrum disorder. Mult. Scler. Relat. Disord. 42, 102110 (2020).
Kunchok, A. et al. Application of 2015 seronegative neuromyelitis optica spectrum disorder diagnostic criteria for patients with myelin oligodendrocyte glycoprotein IgG-associated disorders. JAMA Neurol. 77, 1572–1575 (2020).
Reindl, M. & Waters, P. Myelin oligodendrocyte glycoprotein antibodies in neurological disease. Nat. Rev. Neurol. 15, 89–102 (2019). This review provides a clear and concise overview of MOG antibody disease.
Chen, J. J. et al. Steroid-sparing maintenance immunotherapy for MOG-IgG associated disorder. Neurology 95, e111–e120 (2020).
Hacohen, Y. B. et al. Disease course and treatment responses in children with relapsing myelin oligodendrocyte glycoprotein antibody-associated disease. JAMA Neurol. 75, 478–487 (2018).
Ramanathan, S. et al. Clinical course, therapeutic responses and outcomes in relapsing MOG antibody-associated demyelination. J. Neurol. Neurosurg. Psychiatry 89, 127–137 (2018).
Whittam, D. H. et al. Treatment of MOG-IgG-associated disorder with rituximab: an international study of 121 patients. Mult. Scler. Relat. Disord. 44, 102251 (2020).
Cobo-Calvo, A. et al. Evaluation of treatment response in adults with relapsing MOG-Ab-associated disease. J. Neuroinflammation 16, 134 (2019).
Lucchinetti, C. F. et al. A role for humoral mechanisms in the pathogenesis of Devic’s neuromyelitis optica. Brain 125, 1450–1461 (2002).
Howe, C. L. et al. Neuromyelitis optica IgG stimulates an immunological response in rat astrocyte cultures. Glia 62, 692–708 (2014).
Hinson, S. R. et al. Molecular outcomes of neuromyelitis optica (NMO)-IgG binding to aquaporin-4 in astrocytes. Proc. Natl Acad. Sci. USA 109, 1245–1250 (2012).
Hinson, S. R. et al. Pathogenic potential of IgG binding to water channel extracellular domain in neuromyelitis optica. Neurology 69, 2221–2231 (2007).
Hinson, S. R. et al. Aquaporin-4-binding autoantibodies in patients with neuromyelitis optica impair glutamate transport by down-regulating EAAT2. J. Exp. Med. 205, 2473–2481 (2008).
Vincent, T. et al. Functional consequences of neuromyelitis optica-IgG astrocyte interactions on blood-brain barrier permeability and granulocyte recruitment. J. Immunol. 181, 5730–5737 (2008).
Duan, T., Smith, A. J. & Verkman, A. S. Complement-independent bystander injury in AQP4-IgG seropositive neuromyelitis optica produced by antibody-dependent cellular cytotoxicity. Acta Neuropathol. Commun. 7, 112 (2019).
Fujihara, K. et al. Interleukin-6 in neuromyelitis optica spectrum disorder pathophysiology. Neurol. Neuroimmunol. Neuroinflamm. 7, e841 (2020).
Sagan, S. A. et al. Tolerance checkpoint bypass permits emergence of pathogenic T cells to neuromyelitis optica autoantigen aquaporin-4. Proc. Natl Acad. Sci. USA 113, 14781–14786 (2016).
Pohl, M. et al. T cell-activation in neuromyelitis optica lesions plays a role in their formation. Acta Neuropathol. Commun. 1, 85 (2013).
Vaknin-Dembinsky, A. et al. T-cell responses to distinct AQP4 peptides in patients with neuromyelitis optica (NMO). Mult. Scler. Relat. Disord. 6, 28–36 (2016).
Cotzomi, E. et al. Early B cell tolerance defects in neuromyelitis optica favour anti-AQP4 autoantibody production. Brain 142, 1598–1615 (2019).
Bennett, J. L. et al. Intrathecal pathogenic anti-aquaporin-4 antibodies in early neuromyelitis optica. Ann. Neurol. 66, 617–629 (2009).
Cobo-Calvo, A. et al. Purified IgG from aquaporin-4 neuromyelitis optica spectrum disorder patients alters blood-brain barrier permeability. PLoS ONE 15, e0238301 (2020).
Shimizu, F. et al. Sera from neuromyelitis optica patients disrupt the blood-brain barrier. J. Neurol. Neurosurg. Psychiatry 83, 288–297 (2012).
Guo, Y. et al. Pathogenic implications of cerebrospinal fluid barrier pathology in neuromyelitis optica. Acta Neuropathol. 133, 597–612 (2017).
Shimizu, F. et al. Glucose-regulated protein 78 autoantibody associates with blood-brain barrier disruption in neuromyelitis optica. Sci. Transl Med. 9, eaai9111 (2017).
Tedder, T. F. CD19: a promising B cell target for rheumatoid arthritis. Nat. Rev. Rheumatol. 5, 572–577 (2009).
Lee, D. S. W., Rojas, O. L. & Gommerman, J. L. B cell depletion therapies in autoimmune disease: advances and mechanistic insights. Nat. Rev. Drug Discov. 20, 179–199 (2021).
Icoz, S. et al. Enhanced IL-6 production in aquaporin-4 antibody positive neuromyelitis optica patients. Int. J. Neurosci. 120, 71–75 (2010).
Uzawa, A. et al. Markedly increased CSF interleukin-6 levels in neuromyelitis optica, but not in multiple sclerosis. J. Neurol. 256, 2082–2084 (2009).
Wang, H. et al. Notable increased cerebrospinal fluid levels of soluble interleukin-6 receptors in neuromyelitis optica. Neuroimmunomodulation 19, 304–308 (2012).
Chihara, N. et al. Plasmablasts as migratory IgG-producing cells in the pathogenesis of neuromyelitis optica. PLoS ONE 8, e83036 (2013).
Chihara, N. et al. Interleukin 6 signaling promotes anti-aquaporin 4 autoantibody production from plasmablasts in neuromyelitis optica. Proc. Natl Acad. Sci. USA 108, 3701–3706 (2011).
Uzawa, A. et al. Interleukin-6 analysis of 572 consecutive CSF samples from neurological disorders: A special focus on neuromyelitis optica. Clin. Chim. Acta 469, 144–149 (2017).
Uzawa, A. et al. Cerebrospinal fluid interleukin-6 and glial fibrillary acidic protein levels are increased during initial neuromyelitis optica attacks. Clin. Chim. Acta 421, 181–183 (2013).
Uzawa, A. et al. Cytokine and chemokine profiles in neuromyelitis optica: significance of interleukin-6. Mult. Scler. 16, 1443–1452 (2010).
Barros, P. O. et al. Prediction of disease severity in neuromyelitis optica by the levels of interleukin (IL)-6 produced during remission phase. Clin. Exp. Immunol. 183, 480–489 (2016).
Takeshita, Y. et al. Effects of neuromyelitis optica-IgG at the blood-brain barrier in vitro. Neurol. Neuroimmunol. Neuroinflamm. 4, e311 (2017).
Wilson, R. et al. Condition-dependent generation of aquaporin-4 antibodies from circulating B cells in neuromyelitis optica. Brain 141, 1063–1074 (2018).
Ayzenberg, I. et al. Interleukin 6 receptor blockade in patients with neuromyelitis optica nonresponsive to anti-CD20 therapy. JAMA Neurol. 70, 394–397 (2013).
Soltys, J. et al. Membrane assembly of aquaporin-4 autoantibodies regulates classical complement activation in neuromyelitis optica. J. Clin. Invest. 129, 2000–2013 (2019).
Pittock, S. J. et al. Eculizumab in AQP4-IgG-positive relapsing neuromyelitis optica spectrum disorders: an open-label pilot study. Lancet Neurol. 12, 554–562 (2013).
Cree, B. A. et al. Placebo-controlled study in neuromyelitis optica-Ethical and design considerations. Mult. Scler. 22, 862–872 (2016).
Levy, M. The ethics of placebo controlled clinical trials in NMO-a balance of risks. Mult. Scler. Relat. Disord. 4, 512–514 (2015).
Lennon-Chrimes, S. et al. Characterisation of the PK and PD of satralizumab, a recycling antibody, to support Q4W dosing in patients with NMOSD. Eur. J. Neurol. 27, 930 (2020).
Berthele, A. et al. Pharmacokinetic/pharmacodynamic properties of eculizumab support established efficacy in patients with NMOSD: findings from the phase 3 PREVENT study. Eur. J. Neurol. 27, 351 (2020).
Wingerchuk, D. M. et al. Long-term safety and efficacy of eculizumab in aquaporin-4 IgG-positive NMOSD. Ann. Neurol. 89, 1088–1098 (2021).
Pittock, S. et al. Long-term efficacy and safety of eculizumab monotherapy in AQP4+ neuromyelitis optica spectrum disorder (1578). Neurology 96, 1578 (2021).
Cree, B. et al. Long term efficacy outcomes with inebilizumab treatment in NMOSD: the N-MOmentum Trial (2329). Neurology 96, 2329 (2021).
Cree, B. et al. Long term safety outcomes with inebilizumab treatment in NMOSD: the N-MOmentum Trial (2283). Neurology 96, 2283 (2021).
Waters, P. J. et al. Serologic diagnosis of NMO: a multicenter comparison of aquaporin-4-IgG assays. Neurology 78, 665–671 (2012). This study provided a blinded comparison of various assay methodologies for the detection of AQP4-IgG.
Levy, M., Fujihara, K. & Palace, J. New therapies for neuromyelitis optica spectrum disorder. Lancet Neurol. 20, 60–67 (2021).
Marignier, R. et al. Disability outcomes in the N-MOmentum trial of inebilizumab in neuromyelitis optica spectrum disorder. Neurol. Neuroimmunol. Neuroinflamm. 8, e978 (2021).
Zhang, C. et al. Safety and efficacy of tocilizumab versus azathioprine in highly relapsing neuromyelitis optica spectrum disorder (TANGO): an open-label, multicentre, randomised, phase 2 trial. Lancet Neurol. 19, 391–401 (2020).
Pittock, S. J. et al. Eculizumab monotherapy for NMOSD: data from PREVENT and its open-label extension. Mult. Scler. https://doi.org/10.1177/13524585211038291 (2021).
Luna, G. et al. Infection risks among patients with multiple sclerosis treated with fingolimod, natalizumab, rituximab, and injectable therapies. JAMA Neurol. 77, 184–191 (2020).
Pittock, S. J. et al. Response to: Eculizumab package insert recommendations for meningococcal vaccinations: call for clarity and a targeted approach for use of the drug in neuromyelitis optica spectrum disorder. CNS Spectr. 26, 195–196 (2021).
Socie, G. et al. Eculizumab in paroxysmal nocturnal haemoglobinuria and atypical haemolytic uraemic syndrome: 10-year pharmacovigilance analysis. Br. J. Haematol. 185, 297–310 (2019).
Aktas, O. et al. Serum glial fibrillary acidic protein: a neuromyelitis optica spectrum disorder biomarker. Ann. Neurol. 89, 895–910 (2021).
Acknowledgements
We thank L. Dacy and M. Curtis for technical assistance and S. Lambert for media support.
Author information
Authors and Affiliations
Contributions
S.P. wrote the article. S.P. and A.Z. researched data for the article. S.P. and B.G.W. made substantial contributions to discussion of content. All authors reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
S.P. reports grants, personal fees and non-financial support from Alexion Pharmaceuticals; grants, personal fees, non-financial support and other support from MedImmune/VielaBio; and personal fees for consulting from Genentech/Roche. He is a named inventor on patent 8,889,102 (Application US12/678,350, Neuromyelitis optica autoantibodies as a marker for neoplasia) and a named inventor and assignee on patent 9,891,219B2 (Application US12/573,942, Methods for treating neuromyelitis optica [NMO] by administration of eculizumab to an individual who is aquaporin 4 (AQP4)-IgG autoantibody positive). B.G.W. receives royalties from Hospices Civil de Lyon, MVZ Labour PD Dr. Volkmann und Kollegen GbR, Oxford University, and RSR for a patent of NMO-IgG as a diagnostic test for neuromyelitis optica spectrum disorders. He has served on adjudication committees for clinical trials in neuromyelitis optica spectrum disorders conducted by Alexion and MedImmune/VielaBio, and has consulted for Chugai/Roche/Genentech and Mitsubishi–Tanabe regarding clinical trial design for neuromyelitis optica spectrum disorders. He has also received honoraria for speaking at internal meetings of Genentech and Novartis and at external meetings for Roche. A.Z. declares no competing interests.
Additional information
Peer review information
Nature Reviews Neurology thanks P. Cabre, M.I. Leite, I. Nakashima and D. Sato for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pittock, S.J., Zekeridou, A. & Weinshenker, B.G. Hope for patients with neuromyelitis optica spectrum disorders — from mechanisms to trials. Nat Rev Neurol 17, 759–773 (2021). https://doi.org/10.1038/s41582-021-00568-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-021-00568-8
This article is cited by
-
hUC-MSCs-derived MFGE8 ameliorates locomotor dysfunction via inhibition of ITGB3/ NF-κB signaling in an NMO mouse model
npj Regenerative Medicine (2024)
-
Rapid AQP4-IgG detection in neuromyelitis optica spectrum disorder
Nature Reviews Neurology (2023)
-
Establishment of a comprehensive diagnostic model for neuromyelitis optica spectrum disorders based on the analysis of laboratory indicators and clinical data
Neurological Sciences (2023)
-
Satralizumab: A Review in Neuromyelitis Optica Spectrum Disorder
CNS Drugs (2023)
-
A case of microscopic polyangiitis with acute-onset visual acuity loss
International Urology and Nephrology (2023)