Abstract
Deep brain stimulation (DBS) is a neurosurgical procedure that allows targeted circuit-based neuromodulation. DBS is a standard of care in Parkinson disease, essential tremor and dystonia, and is also under active investigation for other conditions linked to pathological circuitry, including major depressive disorder and Alzheimer disease. Modern DBS systems, borrowed from the cardiac field, consist of an intracranial electrode, an extension wire and a pulse generator, and have evolved slowly over the past two decades. Advances in engineering and imaging along with an improved understanding of brain disorders are poised to reshape how DBS is viewed and delivered to patients. Breakthroughs in electrode and battery designs, stimulation paradigms, closed-loop and on-demand stimulation, and sensing technologies are expected to enhance the efficacy and tolerability of DBS. In this Review, we provide a comprehensive overview of the technical development of DBS, from its origins to its future. Understanding the evolution of DBS technology helps put the currently available systems in perspective and allows us to predict the next major technological advances and hurdles in the field.
Key points
-
Deep brain stimulation (DBS) is a neurosurgical procedure that allows targeted circuit-based neuromodulation and is commonly used for the treatment of movement disorders such as Parkinson disease, tremor and dystonia.
-
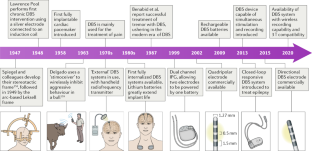
Innovations in the field of cardiac pacemakers have enabled pulse generators for DBS to evolve from external devices to small rechargeable, implantable devices.
-
With directional DBS leads, the current can be directed or shaped to personalize stimulation to individual anatomical structures.
-
Closed-loop DBS systems simultaneously record and stimulate neural activity, allowing the stimulation to be adjusted according to disease-specific neural biomarkers.
-
Open-access software can be used to localize DBS electrodes and, on the basis of the stimulation parameters, to model the volume of tissue activated around the electrodes, shedding light on key neurocircuitry elements.
-
As DBS systems become compatible with wireless networks, remote programming by physicians will become possible but privacy issues will also need to be addressed to prevent misuse, including ‘brainjacking’.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Lozano, A. M. et al. Deep brain stimulation: current challenges and future directions. Nat. Rev. Neurol. 15, 148–160 (2019).
Fasano, A., Aquino, C. C., Krauss, J. K., Honey, C. R. & Bloem, B. R. Axial disability and deep brain stimulation in patients with Parkinson disease. Nat. Rev. Neurol. 11, 98–110 (2015).
Moro, E. et al. Efficacy of pallidal stimulation in isolated dystonia: a systematic review and meta-analysis. Eur. J. Neurol. 24, 552–560 (2017).
Limousin, P. & Foltynie, T. Long-term outcomes of deep brain stimulation in Parkinson disease. Nat. Rev. Neurol. 15, 234–242 (2019).
Fontaine, D., Vandersteen, C., Magis, D. & Lanteri-Minet, M. Neuromodulation in cluster headache. Adv. Tech. Stand. Neurosurg. 42, 3–21 (2015).
Pereira, E. A. & Aziz, T. Z. Neuropathic pain and deep brain stimulation. Neurotherapeutics 11, 496–507 (2014).
Lee, D. J., Lozano, C. S., Dallapiazza, R. F. & Lozano, A. M. Current and future directions of deep brain stimulation for neurological and psychiatric disorders. J. Neurosurg. 131, 333–342 (2019).
Mallet, L. et al. Subthalamic nucleus stimulation in severe obsessive-compulsive disorder. N. Engl. J. Med. 359, 2121–2134 (2008).
Harmsen, I. E. et al. Clinical trials for deep brain stimulation: current state of affairs. Brain Stimul. 13, 378–385 (2020).
Deeb, W. et al. Proceedings of the Fourth Annual Deep Brain Stimulation Think Tank: a review of emerging issues and technologies. Front. Integr. Neurosci. 10, 38 (2016).
Cagnan, H., Denison, T., McIntyre, C. & Brown, P. Emerging technologies for improved deep brain stimulation. Nat. Biotechnol. 37, 1024–1033 (2019).
Ramirez-Zamora, A. et al. Proceedings of the Sixth Deep Brain Stimulation Think Tank modulation of brain networks and application of advanced neuroimaging, neurophysiology, and optogenetics. Front. Neurosci. 13, 936 (2019).
Kellmeyer, P. et al. The Effects of closed-loop medical devices on the autonomy and accountability of persons and systems. Camb. Q. Healthc. Ethics 25, 623–633 (2016).
Pycroft, L. et al. Brainjacking: implant security issues in invasive neuromodulation. World Neurosurg. 92, 454–462 (2016).
Coffey, R. J. Deep brain stimulation devices: a brief technical history and review. Artif. Organs 33, 208–220 (2009).
Pool, J. L. Psychosurgery in older people. J. Am. Geriatr. Soc. 2, 456–466 (1954).
Delgado, J. M. et al. Intracerebral radio stimulation and recording in completely free patients. J. Nerv. Ment. Dis. 147, 329–340 (1968).
Delgado, J. M., Obrador, S. & Martin-Rodriguez, J. G. in Surgical Approaches in Psychiatry (eds Laitinen, L. & Livingston, K. E.) 215–223 (Medical and Technical Publishing, 1973).
Heath, R. G. Electrical self-stimulation of the brain in man. Am. J. Psychiatry 120, 571–577 (1963).
Heath, R. G. Modulation of emotion with a brain pacemamer. Treatment for intractable psychiatric illness. J. Nerv. Ment. Dis. 165, 300–317 (1977).
Bickford, R. G., Petersen, M. C., Dodge, H. W. Jr. & Sem-Jacobsen, C. W. Observations on depth stimulation of the human brain through implanted electrographic leads. Proc. Staff. Meet. Mayo Clin. 28, 181–187 (1953).
Sem-Jacobsen, C. W. Depth-electrographic observations related to Parkinson’s disease. Recording and electrical stimulation in the area around the third ventricle. J. Neurosurg. 24 (Suppl. 1), 388–402 (1966).
Bechtereva, N. P., Bondartchuk, A. N., Smirnov, V. M., Meliutcheva, L. A. & Shandurina, A. N. Method of electrostimulation of the deep brain structures in treatment of some chronic diseases. Confin. Neurol. 37, 136–140 (1975).
Bechtereva, N. P., Kambarova, D. K., Smirnov, V. M. & Shandurina, A. N. in Neurosurgical Treatment in Psychiatry, Pain, and Epilepsy (eds Sweet, W. H. et al.) 581–613 (Univ. Park Press, 1977).
Blomstedt, P. & Hariz, M. I. Deep brain stimulation for movement disorders before DBS for movement disorders. Parkinsonism Relat. Disord. 16, 429–433 (2010).
Melzack, R. & Wall, P. D. Pain mechanisms: a new theory. Science 150, 971–979 (1965).
Mazars, G., Mérienne, L. & Cioloca, C. Use of thalamic stimulators in the treatment of various types of pain [French]. Ann. Med. Interne 126, 869–871 (1975).
Hosobuchi, Y., Adams, J. E. & Rutkin, B. Chronic thalamic stimulation for the control of facial anesthesia dolorosa. Arch. Neurol. 29, 158–161 (1973).
Hariz, M. I., Blomstedt, P. & Zrinzo, L. Deep brain stimulation between 1947 and 1987: the untold story. Neurosurg. Focus. 29, E1 (2010).
Brice, J. & McLellan, L. Suppression of intention tremor by contingent deep-brain stimulation. Lancet 1, 1221–1222 (1980).
Blomstedt, P. & Hariz, M. Closed loop stimulation for tremor was invented in 1980. Brain Stimul. 12, 1072–1073 (2019).
Benabid, A. L., Pollak, P., Louveau, A., Henry, S. & de Rougemont, J. Combined (thalamotomy and stimulation) stereotactic surgery of the VIM thalamic nucleus for bilateral Parkinson disease. Appl. Neurophysiol. 50, 344–346 (1987).
Kiss, Z. H. T. & Hariz, M. “New and improved” DBS batteries? Brain Stimul. 12, 833–834 (2019).
Hariz, M. Battery obsolescence, industry profit and deep brain stimulation. Acta Neurochir. 161, 2047–2048 (2019).
Steigerwald, F., Muller, L., Johannes, S., Matthies, C. & Volkmann, J. Directional deep brain stimulation of the subthalamic nucleus: A pilot study using a novel neurostimulation device. Mov. Disord. 31, 1240–1243 (2016).
Angelov, S. D. et al. Electrophoretic deposition of ligand-free platinum nanoparticles on neural electrodes affects their impedance in vitro and in vivo with no negative effect on reactive gliosis. J. Nanobiotechnology 14, 3 (2016).
Koenen, S. et al. Optimizing in vitro impedance and physico-chemical properties of neural electrodes by electrophoretic deposition of Pt nanoparticles. Chemphyschem 18, 1108–1117 (2017).
Kronenbuerger, M. et al. Brain alterations with deep brain stimulation: new insight from a neuropathological case series. Mov. Disord. 30, 1125–1130 (2015).
Moss, J., Ryder, T., Aziz, T. Z., Graeber, M. B. & Bain, P. G. Electron microscopy of tissue adherent to explanted electrodes in dystonia and Parkinson’s disease. Brain 127, 2755–2763 (2004).
Fenoy, A. J., Villarreal, S. J. & Schiess, M. C. Acute and subacute presentations of cerebral edema following deep brain stimulation lead implantation. Stereotact. Funct. Neurosurg. 95, 86–92 (2017).
De Ridder, D., Vanneste, S., Plazier, M., van der Loo, E. & Menovsky, T. Burst spinal cord stimulation: toward paresthesia-free pain suppression. Neurosurgery 66, 986–990 (2010).
Kapural, L. et al. Novel 10-kHz high-frequency therapy (HF10 therapy) is superior to traditional low-frequency spinal cord stimulation for the treatment of chronic back and leg pain: the SENZA-RCT randomized controlled trial. Anesthesiology 123, 851–860 (2015).
Schultz, D. M. et al. Sensor-driven position-adaptive spinal cord stimulation for chronic pain. Pain. Physician 15, 1–12 (2012).
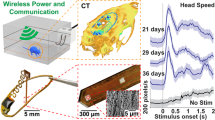
Hosain, M. K., Kouzani, A. Z., Tye, S. J., Abulseoud, O. A. & Berk, M. Design and analysis of an antenna for wireless energy harvesting in a head-mountable DBS device. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2013, 3078–3081 (2013).
Hong, B. et al. Detection of bacterial DNA on neurostimulation systems in patients without overt infection. Clin. Neurol. Neurosurg. 184, 105399 (2019).
Jitkritsadakul, O. et al. Systematic review of hardware-related complications of deep brain stimulation: do new indications pose an increased risk? Brain Stimul. 10, 967–976 (2017).
Piacentino, M., Pilleri, M. & Bartolomei, L. Hardware-related infections after deep brain stimulation surgery: review of incidence, severity and management in 212 single-center procedures in the first year after implantation. Acta Neurochir. 153, 2337–2341 (2011).
Tarakji, K. G. et al. Antibacterial envelope to prevent cardiac implantable device infection. N. Engl. J. Med. 380, 1895–1905 (2019).
Sauer, T., Wolf, M. E., Blahak, C., Capelle, H. H. & Krauss, J. K. Neuroleptic-like malignant syndrome after battery depletion in a patient with deep brain stimulation for secondary parkinsonism. Mov. Disord. Clin. Pract. 4, 629–631 (2017).
Hancu, I. et al. On the (Non-)equivalency of monopolar and bipolar settings for deep brain stimulation fMRI studies of Parkinson’s disease patients. J. Magn. Reson. Imaging 49, 1736–1749 (2019).
Bronstein, J. M. et al. The rationale driving the evolution of deep brain stimulation to constant-current devices. Neuromodulation 18, 85–88 (2015).
Lettieri, C. et al. Clinical outcome of deep brain stimulation for dystonia: constant-current or constant-voltage stimulation? A non-randomized study. Eur. J. Neurol. 22, 919–926 (2015).
Preda, F. et al. Switching from constant voltage to constant current in deep brain stimulation: a multicenter experience of mixed implants for movement disorders. Eur. J. Neurol. 23, 190–195 (2016).
Lempka, S. F., Johnson, M. D., Miocinovic, S., Vitek, J. L. & McIntyre, C. C. Current-controlled deep brain stimulation reduces in vivo voltage fluctuations observed during voltage-controlled stimulation. Clin. Neurophysiol. 121, 2128–2133 (2010).
Cheung, T. et al. Longitudinal impedance variability in patients with chronically implanted DBS devices. Brain Stimul. 6, 746–751 (2013).
Grill, W. M. Model-based analysis and design of waveforms for efficient neural stimulation. Prog. Brain Res. 222, 147–162 (2015).
Akbar, U. et al. Randomized, blinded pilot testing of nonconventional stimulation patterns and shapes in Parkinson’s disease and essential tremor: evidence for further evaluating narrow and biphasic pulses. Neuromodulation 19, 343–356 (2016).
De Jesus, S. et al. Square biphasic pulse deep brain stimulation for essential tremor: the BiP tremor study. Parkinsonism Relat. Disord. 46, 41–46 (2018).
McIntyre, C. C. & Grill, W. M. Selective microstimulation of central nervous system neurons. Ann. Biomed. Eng. 28, 219–233 (2000).
Hofmann, L., Ebert, M., Tass, P. A. & Hauptmann, C. Modified pulse shapes for effective neural stimulation. Front. Neuroeng. 4, 9 (2011).
Popovych, O. V., Lysyansky, B., Rosenblum, M., Pikovsky, A. & Tass, P. A. Pulsatile desynchronizing delayed feedback for closed-loop deep brain stimulation. PLoS One 12, e0173363 (2017).
Popovych, O. V., Lysyansky, B. & Tass, P. A. Closed-loop deep brain stimulation by pulsatile delayed feedback with increased gap between pulse phases. Sci. Rep. 7, 1033 (2017).
Popovych, O. V. & Tass, P. A. Multisite delayed feedback for electrical brain stimulation. Front. Physiol. 9, 46 (2018).
Benabid, A. L. et al. Chronic electrical stimulation of the ventralis intermedius nucleus of the thalamus as a treatment of movement disorders. J. Neurosurg. 84, 203–214 (1996).
Kirsch, A. D., Hassin-Baer, S., Matthies, C., Volkmann, J. & Steigerwald, F. Anodic versus cathodic neurostimulation of the subthalamic nucleus: A randomized-controlled study of acute clinical effects. Parkinsonism Relat. Disord. 55, 61–67 (2018).
Grill, W. M. Temporal pattern of electrical stimulation is a new dimension of therapeutic innovation. Curr. Opin. Biomed. Eng. 8, 1–6 (2018).
Brocker, D. T. et al. Optimized temporal pattern of brain stimulation designed by computational evolution. Sci. Transl. Med. 9, eaah3532 (2017).
Birdno, M. J. et al. Stimulus features underlying reduced tremor suppression with temporally patterned deep brain stimulation. J. Neurophysiol. 107, 364–383 (2012).
Brocker, D. T. et al. Improved efficacy of temporally non-regular deep brain stimulation in Parkinson’s disease. Exp. Neurol. 239, 60–67 (2013).
Krauss, J. K., Yianni, J., Loher, T. J. & Aziz, T. Z. Deep brain stimulation for dystonia. J. Clin. Neurophysiol. 21, 18–30 (2004).
Cassar, I. R., Titus, N. D. & Grill, W. M. An improved genetic algorithm for designing optimal temporal patterns of neural stimulation. J. Neural Eng. 14, 066013 (2017).
Lee, S., Asaad, W. F. & Jones, S. R. Computational modeling to improve treatments for essential tremor. Drug Discov. Today Dis. Model. 19, 19–25 (2016).
Tass, P. A. Phase Resetting in Medicine and Biology: Stochastic Modelling and Data Analysis (Springer, 1999).
Tass, P. A. A model of desynchronizing deep brain stimulation with a demand-controlled coordinated reset of neural subpopulations. Biol. Cybern. 89, 81–88 (2003).
Popovych, O. V. & Tass, P. A. Control of abnormal synchronization in neurological disorders. Front. Neurol. 5, 268 (2014).
Markram, H., Lubke, J., Frotscher, M. & Sakmann, B. Regulation of synaptic efficacy by coincidence of postsynaptic APs and EPSPs. Science 275, 213–215 (1997).
Tass, P. A. & Majtanik, M. Long-term anti-kindling effects of desynchronizing brain stimulation: a theoretical study. Biol. Cybern. 94, 58–66 (2006).
Hauptmann, C. & Tass, P. A. Cumulative and after-effects of short and weak coordinated reset stimulation: a modeling study. J. Neural Eng. 6, 016004 (2009).
Tass, P. A. et al. Coordinated reset has sustained aftereffects in Parkinsonian monkeys. Ann. Neurol. 72, 816–820 (2012).
Adamchic, I. et al. Coordinated reset neuromodulation for Parkinson’s disease: proof-of-concept study. Mov. Disord. 29, 1679–1684 (2014).
Wang, J. et al. Coordinated reset deep brain stimulation of subthalamic nucleus produces long-lasting, dose-dependent motor improvements in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine non-human primate model of parkinsonism. Brain Stimul. 9, 609–617 (2016).
Bouthour, W. et al. Biomarkers for closed-loop deep brain stimulation in Parkinson disease and beyond. Nat. Rev. Neurol. 15, 343–352 (2019).
Hoang, K. B. & Turner, D. A. The emerging role of biomarkers in adaptive modulation of clinical brain stimulation. Neurosurgery 85, E430–E439 (2019).
Shute, J. B. et al. Thalamocortical network activity enables chronic tic detection in humans with Tourette syndrome. Neuroimage Clin. 12, 165–172 (2016).
Swann, N. C. et al. Adaptive deep brain stimulation for Parkinson’s disease using motor cortex sensing. J. Neural Eng. 15, 046006 (2018).
Herron, J. A. et al. Chronic electrocorticography for sensing movement intention and closed-loop deep brain stimulation with wearable sensors in an essential tremor patient. J. Neurosurg. 127, 580–587 (2017).
Little, S. et al. Adaptive deep brain stimulation in advanced Parkinson disease. Ann. Neurol. 74, 449–457 (2013).
Arlotti, M. et al. Eight-hours adaptive deep brain stimulation in patients with Parkinson disease. Neurology 90, e971–e976 (2018).
Tinkhauser, G. et al. Directional local field potentials: a tool to optimize deep brain stimulation. Mov. Disord. 33, 159–164 (2018).
Piña-Fuentes, D. et al. Toward adaptive deep brain stimulation for dystonia. Neurosurg. Focus 45, E3 (2018).
Sinclair, N. C. et al. Subthalamic nucleus deep brain stimulation evokes resonant neural activity. Ann. Neurol. 83, 1027–1031 (2018).
Rosa, M. et al. Adaptive deep brain stimulation controls levodopa-induced side effects in Parkinsonian patients. Mov. Disord. 32, 628–629 (2017).
Deffains, M., Iskhakova, L., Katabi, S., Israel, Z. & Bergman, H. Longer β oscillatory episodes reliably identify pathological subthalamic activity in Parkinsonism. Mov. Disord. 33, 1609–1618 (2018).
Little, S. et al. Bilateral adaptive deep brain stimulation is effective in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 87, 717–721 (2016).
Little, S. et al. Adaptive deep brain stimulation for Parkinson’s disease demonstrates reduced speech side effects compared to conventional stimulation in the acute setting. J. Neurol. Neurosurg. Psychiatry 87, 1388–1389 (2016).
Shah, S. A., Tinkhauser, G., Chen, C. C., Little, S. & Brown, P. Parkinsonian tremor detection from subthalamic nucleus local field potentials for closed-loop deep brain stimulation. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2018, 2320–2324 (2018).
Cagnan, H. et al. Stimulating at the right time: phase-specific deep brain stimulation. Brain 140, 132–145 (2017).
Basu, I. et al. Pathological tremor prediction using surface electromyogram and acceleration: potential use in ‘ON-OFF’ demand driven deep brain stimulator design. J. Neural Eng. 10, 036019 (2013).
Tan, H. et al. Decoding voluntary movements and postural tremor based on thalamic LFPs as a basis for closed-loop stimulation for essential tremor. Brain Stimul. 12, 858–867 (2019).
Velisar, A. et al. Dual threshold neural closed loop deep brain stimulation in Parkinson disease patients. Brain Stimul. 12, 868–876 (2019).
Morrell, M. J. & RNS System in Epilepsy Study Group. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology 77, 1295–1304 (2011).
Elder, C., Friedman, D., Devinsky, O., Doyle, W. & Dugan, P. Responsive neurostimulation targeting the anterior nucleus of the thalamus in 3 patients with treatment-resistant multifocal epilepsy. Epilepsia Open. 4, 187–192 (2019).
Voges, B. R. et al. Deep brain stimulation of anterior nucleus thalami disrupts sleep in epilepsy patients. Epilepsia 56, e99–e103 (2015).
Boon, P. et al. A prospective, multicenter study of cardiac-based seizure detection to activate vagus nerve stimulation. Seizure 32, 52–61 (2015).
Fisher, R. S. et al. Automatic vagus nerve stimulation triggered by ictal tachycardia: clinical outcomes and device performance — the U.S. E-37 Trial. Neuromodulation 19, 188–195 (2016).
Wolf, M. E., Blahak, C., Saryyeva, A., Schrader, C. & Krauss, J. K. Deep brain stimulation for dystonia-choreoathetosis in cerebral palsy: pallidal versus thalamic stimulation. Parkinsonism Relat. Disord. 63, 209–212 (2019).
Sani, O. G. et al. Mood variations decoded from multi-site intracranial human brain activity. Nat. Biotechnol. 36, 954–961 (2018).
Kremen, V. et al. Integrating brain implants with local and distributed computing devices: a next generation epilepsy management system. IEEE J. Transl. Eng. Health Med. 6, 2500112 (2018).
Khanna, P. et al. Enabling closed-loop neurostimulation research with downloadable firmware upgrades. IEEE Biomed. Circuits Syst. Conf. https://doi.org/10.1109/BioCAS.2015.7348348 (2015).
Liu, T. et al. Improved subthalamic nucleus depiction with quantitative susceptibility mapping. Radiology 269, 216–223 (2013).
Wang, Y. & Liu, T. Quantitative susceptibility mapping (QSM): decoding MRI data for a tissue magnetic biomarker. Magn. Reson. Med. 73, 82–101 (2015).
Sudhyadhom, A., Haq, I. U., Foote, K. D., Okun, M. S. & Bova, F. J. A high resolution and high contrast MRI for differentiation of subcortical structures for DBS targeting: the Fast Gray Matter Acquisition T1 Inversion Recovery (FGATIR). Neuroimage 47 (Suppl. 2), T44–T52 (2009).
Horn, A. et al. Lead-DBS v2: towards a comprehensive pipeline for deep brain stimulation imaging. Neuroimage 184, 293–316 (2019).
Coenen, V. A., Madler, B., Schiffbauer, H., Urbach, H. & Allert, N. Individual fiber anatomy of the subthalamic region revealed with diffusion tensor imaging: a concept to identify the deep brain stimulation target for tremor suppression. Neurosurgery 68, 1069–1075 (2011).
Tourdias, T., Saranathan, M., Levesque, I. R., Su, J. & Rutt, B. K. Visualization of intra-thalamic nuclei with optimized white-matter-nulled MPRAGE at 7T. Neuroimage 84, 534–545 (2014).
Kanowski, M. et al. Direct visualization of anatomic subfields within the superior aspect of the human lateral thalamus by MRI at 7T. AJNR Am. J. Neuroradiol. 35, 1721–1727 (2014).
Duchin, Y. et al. Patient-specific anatomical model for deep brain stimulation based on 7 Tesla MRI. PLoS One 13, e0201469 (2018).
Plantinga, B. R. et al. Individualized parcellation of the subthalamic nucleus in patients with Parkinson’s disease with 7T MRI. Neuroimage 168, 403–411 (2018).
Dembek, T. A. et al. Directional DBS leads show large deviations from their intended implantation orientation. Parkinsonism Relat. Disord. 67, 117–121 (2019).
Bonmassar, G., Angelone, L. M. & Makris, N. A virtual patient simulator based on human connectome and 7 T MRI for deep brain stimulation. Int. J. Adv. Life Sci. 6, 364–372 (2014).
Husch, A., Petersen, M. V., Gemmar, P., Goncalves, J. & Hertel, F. PaCER — a fully automated method for electrode trajectory and contact reconstruction in deep brain stimulation. Neuroimage Clin. 17, 80–89 (2017).
Lauro, P. M. et al. DBSproc: an open source process for DBS electrode localization and tractographic analysis. Hum. Brain Mapp. 37, 422–433 (2016).
Miocinovic, S., Noecker, A. M., Maks, C. B., Butson, C. R. & McIntyre, C. C. Cicerone: stereotactic neurophysiological recording and deep brain stimulation electrode placement software system. Acta Neurochir. Suppl. 97, 561–567 (2007).
Horn, A. & Kuhn, A. A. Lead-DBS: a toolbox for deep brain stimulation electrode localizations and visualizations. Neuroimage 107, 127–135 (2015).
Milchenko, M. et al. ESM-CT: a precise method for localization of DBS electrodes in CT images. J. Neurosci. Methods 308, 366–376 (2018).
Chakravorti, S. et al. Validation of an automatic algorithm to identify NeuroPace depth leads in CT images. Proc. SPIE https://doi.org/10.1117/12.2512580 (2019).
Sitz, A. et al. Determining the orientation angle of directional leads for deep brain stimulation using computed tomography and digital x-ray imaging: a phantom study. Med. Phys. 44, 4463–4473 (2017).
Boutet, A. et al. Neuroimaging technological advancements for targeting in functional neurosurgery. Curr. Neurol. Neurosci. Rep. 19, 42 (2019).
Ewert, S. et al. Optimization and comparative evaluation of nonlinear deformation algorithms for atlas-based segmentation of DBS target nuclei. Neuroimage 184, 586–598 (2019).
Chaturvedi, A., Lujan, J. L. & McIntyre, C. C. Artificial neural network based characterization of the volume of tissue activated during deep brain stimulation. J. Neural Eng. 10, 056023 (2013).
Schmidt, C., Grant, P., Lowery, M. & van Rienen, U. Influence of uncertainties in the material properties of brain tissue on the probabilistic volume of tissue activated. IEEE Trans. Biomed. Eng. 60, 1378–1387 (2013).
Butson, C. R., Cooper, S. E., Henderson, J. M. & McIntyre, C. C. Patient-specific analysis of the volume of tissue activated during deep brain stimulation. Neuroimage 34, 661–670 (2007).
Horn, A. et al. Deep brain stimulation induced normalization of the human functional connectome in Parkinson’s disease. Brain 142, 3129–3143 (2019).
Akram, H. et al. Subthalamic deep brain stimulation sweet spots and hyperdirect cortical connectivity in Parkinson’s disease. Neuroimage 158, 332–345 (2017).
Bot, M. et al. Deep brain stimulation for Parkinson’s disease: defining the optimal location within the subthalamic nucleus. J. Neurol. Neurosurg. Psychiatry 89, 493–498 (2018).
Dembek, T. A. et al. Probabilistic sweet spots predict motor outcome for deep brain stimulation in Parkinson disease. Ann. Neurol. 86, 527–538 (2019).
Horn, A. et al. Connectivity predicts deep brain stimulation outcome in Parkinson disease. Ann. Neurol. 82, 67–78 (2017).
Neumann, W. J. et al. A localized pallidal physiomarker in cervical dystonia. Ann. Neurol. 82, 912–924 (2017).
Reich, M. M. et al. Probabilistic mapping of the antidystonic effect of pallidal neurostimulation: a multicentre imaging study. Brain 142, 1386–1398 (2019).
Schonecker, T. et al. Postoperative MRI localisation of electrodes and clinical efficacy of pallidal deep brain stimulation in cervical dystonia. J. Neurol. Neurosurg. Psychiatry 86, 833–839 (2015).
Al-Fatly, B. et al. Connectivity profile of thalamic deep brain stimulation to effectively treat essential tremor. Brain 142, 3086–3098 (2019).
Dembek, T. A. et al. Probabilistic mapping of deep brain stimulation effects in essential tremor. Neuroimage Clin. 13, 164–173 (2017).
Baldermann, J. C. et al. Connectivity profile predictive of effective deep brain stimulation in obsessive–compulsive disorder. Biol. Psychiatry 85, 735–743 (2019).
Horn, A. The impact of modern-day neuroimaging on the field of deep brain stimulation. Curr. Opin. Neurol. 32, 511–520 (2019).
Horn, A. et al. Probabilistic conversion of neurosurgical DBS electrode coordinates into MNI space. Neuroimage 150, 395–404 (2017).
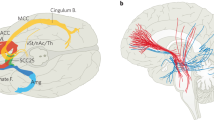
Lozano, A. M. & Lipsman, N. Probing and regulating dysfunctional circuits using deep brain stimulation. Neuron 77, 406–424 (2013).
Choi, K. S., Riva-Posse, P., Gross, R. E. & Mayberg, H. S. Mapping the “depression switch” during intraoperative testing of subcallosal cingulate deep brain stimulation. JAMA Neurol. 72, 1252–1260 (2015).
Riva-Posse, P. et al. A connectomic approach for subcallosal cingulate deep brain stimulation surgery: prospective targeting in treatment-resistant depression. Mol. Psychiatry 23, 843–849 (2018).
Li, N. et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat. Commun. 11, 3364 (2020).
Rezai, A. R. et al. Is magnetic resonance imaging safe for patients with neurostimulation systems used for deep brain stimulation? Neurosurgery 57, 1056–1062 (2005).
Boutet, A. et al. 3-Tesla MRI of deep brain stimulation patients: safety assessment of coils and pulse sequences. J. Neurosurg. 132, 586–594 (2019).
Boutet, A. et al. Functional MRI safety and artifacts during deep brain stimulation: experience in 102 patients. Radiology 293, 174–183 (2019).
Denning, T., Matsuoka, Y. & Kohno, T. Neurosecurity: security and privacy for neural devices. Neurosurg. Focus. 27, E7 (2009).
Zizek, S. Like a Thief in Broad Daylight — Power in the Era of Post-human Capitalism (Seven Stories Press, 2018).
Hittinger, E. & Jaramillo, P. Internet of Things: energy boon or bane? Science 364, 326–328 (2019).
[No authors listed] A connected world will be a playground for hackers. The Economist https://www.economist.com/technology-quarterly/2019/09/12/a-connected-world-will-be-a-playground-for-hackers (2019).
Pugh, J., Pycroft, L., Sandberg, A., Aziz, T. & Savulescu, J. Brainjacking in deep brain stimulation and autonomy. Ethics Inf. Technol. 20, 219–232 (2018).
Spiegel, E. A., Wycis, H. T., Marks, M. & Lee, A. J. Stereotaxic apparatus for operations on the human brain. Science 106, 349–350 (1947).
Delgado, J. M. R. Physical Control of the Mind: Toward a Psychocivilized Society (Harper and Row, 1969).
Acknowledgements
The work on this manuscript was supported by an unconditional grant of the World Society for Stereotactic and Functional Neurosurgery (WSSFN). The working process was coordinated with the Research and Education committees of the WSSFN.
Author information
Authors and Affiliations
Contributions
All authors contributed to all aspects of manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
J. K. K. is a consultant for Medtronic and Boston Scientific. P. B. is a consultant for Medtronic. W. M. G. is the Director, Chief Scientific Officer and share owner of Deep Brain Innovations, LLC. He also receives royalty payments for licensed patents on temporal patterns of deep brain stimulation. M. I. H. has received travel expenses and honoraria from Boston Scientific for speaking at meetings. A. H. was supported by the German Research Council (DFG grant 410169619) and reports lecture fees from Medtronic and Boston Scientific unrelated to the present work. P. A. T. works as a consultant for Boston Scientific Neuromodulation. J. V. works as a consultant to Boston Scientific, Medtronic, and Newronika and has received honoraria for lectures from Boston Scientific and Medtronic as well as research grants from Boston Scientific and Medtronic. A. M. L. has served as a consultant for Boston Scientific, Medtronic, Aleva, and Abbott and is a co-founder of Functional Neuromodulation. All other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Neurology thanks V. Visser-Vandewalle and Y. Temel for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Brainjacking
-
The unauthorized control of an implanted brain device, theoretically through Bluetooth or wireless internet technology.
- Gate theory
-
Theory describing the ‘gating’ of pain signals, whereby the transmission of non-painful stimuli can block or override painful signals at the level of the spinal cord.
- Quadripolar electrodes
-
Deep brain stimulation (DBS) electrodes configured with four equally spaced contacts — the most commonly used DBS electrode configuration.
- Radiofrequency coupled coils
-
Early deep brain stimulation systems powered the delivery of stimulation using an implanted radiofrequency receiving coil. These systems evolved and were replaced by the modern-day battery-coupled pulse generators.
- Implantable pulse generator
-
(IPG). A battery, typically implanted below the clavicle and connected via subcutaneous extension cables to intracranial electrodes. The IPG generates and transmits electrical impulses at a specified frequency, amplitude and pulse width.
- Parameter space
-
The available combinations of voltage, current, pulse width, contact selection, current shape and stimulation pattern when programming a deep brain stimulation device.
- Segmented leads
-
Deep brain stimulation electrodes with multiple different contacts through which current can be transmitted.
- Electrode contacts
-
Non-insulated regions near the distal tip of an electrode from which electrical impulses are transmitted.
- Waveforms
-
The shapes of the electrical impulses transmitted from a deep brain stimulation contact, most often represented in 2D as a function of voltage or current over time.
- Volume of tissue activated
-
(VTA). The estimated spatial extent of the electric field surrounding an activated deep brain stimulation contact at a given stimulation parameter setting.
- Energy-harvesting
-
Having the capability to capture energy from the surrounding environment, including from thermal, vibratory, electromagnetic and acoustic sources.
- Biphasic pulses
-
Electrical impulses consisting of both a positively and a negatively charged component. During each stimulus, a reversal between cathodic and anodic stimulation occurs.
- Cathodic and anodic
-
During stimulation, an electrode contact can function as a cathode (or current sink) or as an anode (source of current) relative to the implantable pulse generator or to other electrode contacts.
- Spike timing-dependent plasticity
-
Concept by which the timing of presynaptic and postsynaptic excitatory potentials affects the overall synaptic strength.
- Neuronal coincidence rates
-
The incidence of temporally overlapping presynaptic and postsynaptic excitatory potentials.
- Power spectra
-
In the context of local field potentials, it refers to the strength or intensity of the electric field based on frequency, commonly categorized as delta (1–3 Hz), theta (4–8 Hz), alpha (4–9 Hz), beta (15–30 Hz) and gamma (>30 Hz).
Rights and permissions
About this article
Cite this article
Krauss, J.K., Lipsman, N., Aziz, T. et al. Technology of deep brain stimulation: current status and future directions. Nat Rev Neurol 17, 75–87 (2021). https://doi.org/10.1038/s41582-020-00426-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-020-00426-z
This article is cited by
-
Subthalamic nucleus deep brain stimulation alleviates oxidative stress via mitophagy in Parkinson’s disease
npj Parkinson's Disease (2024)
-
Image-guided programming deep brain stimulation improves clinical outcomes in patients with Parkinson’s disease
npj Parkinson's Disease (2024)
-
Benchmarking signal quality and spatiotemporal distribution of interictal spikes in prolonged human iEEG recordings using CorTec wireless brain interchange
Scientific Reports (2024)
-
Monolithic silicon for high spatiotemporal translational photostimulation
Nature (2024)
-
The role of neuromodulation in the management of drug-resistant epilepsy
Neurological Sciences (2024)