Abstract
Tuberous sclerosis complex (TSC) is an autosomal dominant disorder characterized by the presence of proliferative lesions throughout the body. Management of TSC is challenging because patients have a multifaceted systemic illness with prominent neurological and developmental impact as well as potentially severe kidney, heart and lung phenotypes; however, every organ system can be involved. Adequate care for patients with TSC requires a coordinated effort involving a multidisciplinary team of clinicians and support staff. This clinical practice recommendation was developed by nephrologists, urologists, paediatric radiologists, interventional radiologists, geneticists, pathologists, and patient and family group representatives, with a focus on TSC-associated kidney manifestations. Careful monitoring of kidney function and assessment of kidney structural lesions by imaging enable early interventions that can preserve kidney function through targeted approaches. Here, we summarize the current evidence and present recommendations for the multidisciplinary management of kidney involvement in TSC.
Similar content being viewed by others
Introduction
Tuberous sclerosis complex (TSC) is an autosomal dominant disorder affecting both fetal development and postnatal growth, with major neurological and developmental effects in most patients and tumour development in multiple organ systems. The incidence of TSC at birth1 is of ~1 in 5,800, resulting in over one million currently affected patients worldwide2,3. The condition is often not recognized by most clinicians without specialist knowledge, as <40% of patients have the classic triad of facial angiofibromata, developmental delay and intractable epilepsy4. A systematic review identified the leading causes of mortality in patients with TSC of all ages to be epilepsy (especially status epilepticus and sudden unexpected death in epilepsy), kidney complications and complications from infections5. Highlighting the importance of kidney involvement, ~40% of adult patients with TSC have a low glomerular filtration rate (GFR)6, and TSC-associated kidney disease is the most common cause of death in adults with TSC7,8. The exact proportion of patients with TSC who have kidney failure is unclear, partly because TSC is not always available as a diagnosis code in kidney failure databases.
TSC-associated kidney disease comprises three major phenotypes: angiomyolipomata, cystic disease and renal cell carcinoma (RCC). These phenotypes are not mutually exclusive and patients often have a combination of angiomyolipomata and cysts, or (rarely) all three phenotypes. These kidney manifestations are listed in decreasing order of frequency, such that ~70–80% of patients have angiomyolipomata, ~50% have cystic kidney disease, and a diagnosis of kidney cancer or oncocytoma is present in 3–5% of patients. TSC-associated kidney manifestations are typically gradually detected with age. Importantly, normal kidney imaging and GFR in young children do not preclude future development of kidney lesions and all patients with TSC should have regular monitoring of kidney function and imaging9. The median ages for the detection of cysts and angiomyolipomata are 3 years and 8–13 years, respectively. However, both cysts and angiomyolipomata can develop in the first months of life, which justifies starting kidney monitoring from the point of diagnosis10,11,12,13,14,15,16,17. Staging of angiomyolipomata (Table 1) and cystic burden (Table 2) can be useful to clinically describe the disease and responses to therapy.
Patients with TSC kidney involvement are at considerable risk of receiving delayed or inappropriate health care. Patient groups have emerged to support patients and families and to improve knowledge of the disease and its care. Although updated general recommendations for the diagnosis and care of TSC have been published18, few publications explicitly provide nephrologists and urologists with information on kidney manifestations and management in TSC. Because adequate guidance for kidney care in TSC is often unavailable or difficult to access, many anecdotal reports exist of patients with TSC having unnecessary surgical procedures or nephrectomies, which worsens their risk of advanced chronic kidney disease (CKD). Moreover, the success of targeted therapeutic approaches, including mechanistic target of rapamycin complex 1 (mTORC1) inhibitor therapies for both angiomyolipomata19,20 and, although not approved, for some forms of TSC cystic kidney disease21, raises the expectation that kidney phenotypes in patients with TSC can be addressed to mitigate disease progression.
In this Consensus Statement, we sought to integrate the input of all physicians involved in the kidney management of patients with TSC, including nephrologists, urologists, geneticists, radiologists, interventional radiologists and pathologists, as well as patient representatives. We provide a global, systematic overview of the most current and accurate information regarding TSC-associated kidney disease. Our intent was to provide a single-source reference document for all physicians involved in the medical care of patients with TSC seeking to improve care at all ages.
Methods
Methodological support was provided by the Basque Office for Health Technology Assessment (OSTEBA) and the Basque Foundation for Health Innovation and Research (BIOEF) for this Clinical Practice Recommendation regarding the multidisciplinary management of kidney involvement in patients with TSC, which was developed over 6 months, from July 14 to December 27, 2021, in accordance with planning of the project ‘ERN Guidelines: Clinical Practice Guidelines and Clinical Decision Support Tools’, funded by the European Commission, DG SANTE, Tender SANTE/2018/B3/030.
Four working groups were established by the European Rare Kidney Disease Reference Network (ERKNET) to examine different clinical aspects of kidney involvement in TSC. Working group experts defined research questions, which were adapted by OSTEBA to ensure that only one intervention per question was included. The research questions were structured in four parts, according to the patient population, intervention, comparator and outcome (PICO) format. Working Group 1 analysed six research questions regarding genetic aspects of TSC; Working Group 2 analysed four research questions about comorbidities and follow-up; Working Group 3 proposed five questions related to diagnostic imaging and biopsy; and Working Group 4 addressed 16 issues related to treatment of the disease (Appendix 1, Supplementary information). The work of each working group was carried out simultaneously but independently.
Systematic evidence searches
A systematic search of evidence was conducted for all PICO questions. Meta-search engines were consulted as the first approach (Tripdatabase and Epistemonikos). Key words were identified based on the PICO framework and then translated into subject headings and free-text search terms. Depending on the clinical question as well as on practical considerations, working groups could request to limit the search based on publication language, abstract availability, publication period or publication type.
A preliminary search was conducted in one of the biomedical core databases (MEDLINE or Embase). Information specialists contacted the working groups to clarify terms and achieve a balanced search regarding specificity and sensitivity as well as to decide whether to consult systematic reviews or clinical trial databases like Database of Abstracts of Reviews of Effects (DARE), Cochrane Database of Systematic Reviews (CDSR), WHO International Clinical Trials Registry Platform (ICRTP), Cochrane Central Register of Controlled Trials (CENTRAL) and European Union Clinical Trials Register (EU-CTR). Different search strategies were decided for each working group (Appendix 2, Supplementary information). The definitive literature search strategy was revised and approved by the group. For all research questions, at least two core databases (MEDLINE or Embase) were explored. In addition, to ensure adequate coverage of all aspects, a complementary search in related platforms was performed as well as a search of relevant organizations and project websites related to TSC.
Selection and synthesis of scientific evidence
Electronic records of the references retrieved by searches were stored using a reference management web application (Rayyan)22. For the initial screening process, at least two independent methodologists from the OSTEBA-BIOEF technical team scanned titles and abstracts from the retrieved references to exclude irrelevant publications. Next, members of ERKNet and OSTEBA-BIOEF applied the inclusion and exclusion criteria (Appendix 3, Supplementary information) that were agreed upon for each clinical question. Original articles for selected references were retrieved, and full-text screening processes were performed applying a double-blind review. Any doubts about inclusion were resolved by discussion within the review team before results of the study were considered. Studies that failed to meet the inclusion criteria after full-text screening were excluded. A list of all excluded studies, with the explicit reasons for exclusion concisely stated, was provided for each question; a PRISMA flow diagram was used to explain the selection process.
Grading of recommendations
Initial recommendations were developed by members of each working group. During a face-to-face meeting, those recommendations were graded by the project leads and working group leads according to the methodology of the American Academy of Paediatrics23. Quality of evidence as well as the balance of potential benefits and harms were considered for the grading of recommendations as weak, moderate or strong. An additional grade of X was used for exceptional situations where validating studies could not be performed but there was a clear preponderance of benefit or harm.
TSC genetics
TSC is caused by inactivating pathogenic variants in either TSC1 or TSC2. A wide spectrum of such variants has been identified, including nonsense, missense, splice, out-of-frame and in-frame insertions and deletions (Figure 1 in Appendix 4, Supplementary information) as well as larger genomic rearrangements, ranging from single exon deletions to deletion of the entire gene and some of the surrounding genomic region, and genomic inversion events24 (Figure 2 in Appendix 4, Supplementary information). Most pathogenic variants (>90%) arise from small genetic alterations, with large genomic events occurring in TSC2 and in TSC1 in approximately 4.7% and 0.7% of individuals with TSC, respectively24. Although small pathogenic variants in each gene are widely distributed, several sites of recurrent variants have been identified in TSC1 and TSC2 (Figure 1 in Appendix 4, Supplementary information). These variants are typically either point mutations that occur at CpG sites, which are commonly methylated and thus prone to spontaneous mutation to thymidine through deamination of 5-methylcytosine, or indel variants occurring at short repeat sequences.
Thousands of small variants in TSC1 and TSC2 have been identified both in individuals with TSC and in unaffected populations (see the Human Variome Project database and the gnomAD browser). Assessment of whether such variants are pathogenic is straightforward in many cases but unclear in others. A variant is considered pathogenic if it clearly prevents protein synthesis and/or inactivates the function of TSC1 or TSC2 (ref. 25). The clinical significance of missense variants is often difficult to assess.
A pathogenic variant cannot be identified in 10–15% of children and adults diagnosed with TSC24,26,27,28. These patients typically have TSC symptoms and signs that are milder on average than those seen in other patients with TSC, and nearly all have mosaicism for a pathogenic variant in TSC2 or, much less commonly, TSC1 (refs. 26,27,28,29). Mosaicism is the occurrence of a genetic variant in some but not all cells of an individual and happens when a new variant occurs in an early embryonic cell but not in the fertilized egg30. Mosaic allele frequency typically varies across different tissues, reflecting the heterogeneous distribution of variant-containing cells. In ~18% of patients with TSC mosaicism, the pathogenic variant is not detected in blood DNA samples26,28,29. A diagnostic algorithm to guide the sequencing approach for the detection of TSC mosaicism in adults has been developed31. Many academic and commercial laboratories perform genetic analyses of TSC1 and TSC2 and can report varying levels of mosaicism. To our knowledge, the laboratory with the most sensitive clinically certified analysis is at the University of Alabama, which can identify and report down to 2% mosaicism. However, levels of mosaicism <2% are common in TSC26,28,29.
TSC2–PKD1 contiguous gene syndrome
The TSC2 and PKD1 genes are located directly adjacent to each other on chromosome 16, separated by only a few nucleotides at the 3′ end of each gene32 (Figure 2 in Appendix 4, Supplementary information). Consequently, genomic deletion events in which part or all of each gene is lost can lead to the inactivation of both genes32,33. Approximately 50% of all patients with genomic deletions in TSC2 also have involvement of the adjacent PKD1 and present with early-onset polycystic kidney disease (PKD) in addition to features of TSC32,33. Mosaicism for these events is common and observed in ~25% of the first affected family member with a contiguous gene deletion33.
Autosomal dominant inheritance
TSC is inherited in an autosomal dominant manner, and TSC genotypes have complete penetrance (that is, all individuals with an inherited TSC1 or TSC2 pathogenic variant will manifest some disease features) but disease onset and severity are variable26. Often, diagnosis of TSC in one individual leads to evaluation and diagnosis in other family members who had escaped medical attention34,35. Although penetrance is complete, expressivity is variable, even within the same family. Several reasons might underlie this variability, including mosaicism; intrinsic variability in the number of second-hit events sustained by a patient during disease development, which is a rate-limiting step for tumour formation; and the genetic context of the patient, meaning that both common and rare variants in other genes can also affect the clinical presentation18. The data supporting a role for mosaicism on disease phenotype is quite clear26,27,28,29 but, although genetic context effects are broadly considered to be important, there are currently limited data to support this.
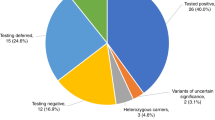
Diagnostic genetic testing and variant classification
If possible, diagnostic genetic testing (Box 1) should be accompanied by genetic counselling before and after testing. Classification of genetic variants should follow the standards and best-practice guidelines of the American College of Medical Genetics and the Association for Clinical Genomic Science25. Definite pathogenic variants in TSC1 or TSC2 are identified in many patients but, in others, no definite mutation is identified and variants of unknown significance (VUS) in either TSC1 or TSC2 might be reported. VUS should not be used in clinical decision-making given the potential harm from misinterpretation of their significance, both for the proband and for any relatives identified as carriers of the VUS through cascade testing.
Mosaicism considerations in genetic counselling
Only one-third of patients diagnosed with TSC have an affected parent. Thus, most affected individuals develop the disease owing to a pathogenic TSC1 or TSC2 variant that has arisen de novo (that is, sporadic TSC)18. However, low-level mosaicism for a pathogenic variant might occur in a parent without TSC manifestations. Mosaicism for a causal TSC1 or TSC2 variant can be present in all tissues, especially if the mosaic allele frequency is high (>5%), but this is not always the case26,27,28,29; rarely, pathogenic variants might be present exclusively in germ cells. Consequently, the parent of a child with seemingly sporadic TSC might have some degree of germ cell mosaicism, which would increase their probability of having a second child with TSC. For this reason, parents of a child with sporadic TSC are advised, during genetic counselling, that the risk of TSC in subsequent pregnancies is estimated at ~1–2%. Of note, the chance of transmission of a pathogenic variant in patients with mosaicism depends on the mosaic allele frequency in germ cells, which is relatively easy to determine in male patients through sperm analysis but is not feasible in female patients.
Genotype–phenotype correlations
Over the past 25 years, multiple studies showed that the severity of TSC2-associated TSC is greater than that of TSC1-associated disease36,37,38,39. A meta-analysis of the three largest studies37,38,39 (1,039 patients in total) confirmed that neurological, kidney and skin findings are more prominent in patients with pathogenic TSC2 variants. Furthermore, analysis of data available from the TSC Alliance Natural History Database (TSC2 n = 376, TSC1 n = 246) showed that multiple clinical manifestations are more severe in patients with TSC2 variants40,41; this finding has been replicated in studies from Greece42, China43,44,45,46,47, Japan48, Brazil49, Canada50 and Taiwan51. The TOSCA registry of patients with TSC from 31 countries showed that the mean age at diagnosis of angiomyolipoma was 13 years for those with TSC2 variants (n = 644) and 23 years for those with TSC1 variants (n = 197) and that bleeding complications were reported only in patients with TSC2 variants4. This difference in severity also extends to infants and young children with TSC. The EPISTOP study found that 52% of children with TSC1 pathogenic variants were free of seizures at age 2 years, compared with 13% for TSC2 (ref. 11). Furthermore, the prevalence of both cortical tubers (53% versus 84%) and multiple kidney cysts (0% versus 34%) is significantly lower in patients with TSC1 variants than in those with pathogenic TSC2 variants. The TACERN study also found that TSC2 pathogenic variants were associated with lower early-learning scores at age 2 years compared with TSC1 pathogenic variants52. Notably, specific missense variants in TSC1 and TSC2 have been associated with a mild disease phenotype, including TSC1 c.1864C>T53, TSC2 c.4508A>C54, TSC2 1864C>T53 and TSC2 R905Q55.
Genetic counselling and prenatal or pre-implantation testing
Genetic counselling is meant to provide individuals and families at risk of a genetic disorder with information on the nature, mode of inheritance and implications of that disorder to help them make informed medical and personal decisions56. Genetic counselling for TSC is challenging for several reasons18, including the considerable variability in presentation, even within a family. If a mosaic or heterozygous pathogenic variant has been identified in a patient with TSC, pre-implantation genetic diagnosis is possible. Many pre-implantation genetic diagnosis options are available, and their relative merits should be discussed before pregnancy given the required advance planning. A 2022 pilot study reported on non-invasive prenatal diagnosis based on cell-free DNA analysis57. Prenatal diagnosis of TSC and early intervention might improve developmental and cognitive outcomes, including reducing the incidence and/or severity of epilepsy in children with TSC58,59.
Diagnosis and monitoring of kidney involvement in TSC
Diagnosis and monitoring of hypertension
Substantial evidence from multiple observational studies and registries suggests an increased risk of hypertension in children and adults with TSC; this risk increases with age. In large studies, estimates of the prevalence of hypertension in this group vary from ~5% in children to 25% in adults overall15,16, but some smaller studies have reported a higher prevalence (up to 40%)60,61. Therefore, blood pressure should be monitored at least annually in all children and adults with TSC (Box 2).
Treatment of hypertension
Evidence on which antihypertensive agents should be used in patients with TSC is limited but, considering the benefits of angiotensin-converting enzyme (ACE) inhibitors in CKD62, expert opinion confirms that first-line treatment of hypertension associated with TSC should be a renin–angiotensin–aldosterone system inhibitor (that is, an ACE inhibitor or an angiotensin receptor blocker) in combination with calcium blockers or diuretics, if required. Of note, in children and adults with TSC who are receiving an mTORC1 inhibitor, reports suggest a low but increased risk of angio-oedema for those also being treated with an ACE inhibitor63. Some clinicians therefore advise that an angiotensin receptor blocker might be a preferable first-line treatment in these patients.
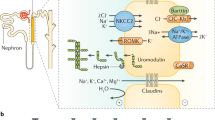
General guidelines for the management of hypertension in CKD, including thresholds for starting antihypertensive medication and targets for blood pressure, should be followed in most patients with TSC64. These guidelines include the European 2018 ESC/ESH guidelines for adults65 or the 2016 ESH guidelines for children66; in North America, the 2017 AAP guidelines are widely accepted67. Although specific data for the TSC population are lacking, based on current guidelines and evidence in the general CKD population64 (Fig. 1), we suggest that 24-h ambulatory blood pressure measurement might be helpful in patients with elevated office blood pressure values (that is, blood pressure ≥95th percentile for age, sex and height in children and ≥120/70 mmHg in adolescents and adults). Of note, an exception should be made for patients with TSC2–PKD1 contiguous gene syndrome, as lower blood pressure targets than those recommended for the general population seemed to preserve GFR68. In this population, treatment should start at lower blood pressure thresholds and have lower targets. Specifically, the KDIGO 2021 Clinical Practice Guideline on the Management of Blood Pressure in Chronic Kidney Disease suggest that kidney benefits might be greater in autosomal dominant PKD when the systolic blood pressure target is 95–110 mmHg in adults rather than 120–130 mmHg (ref. 64).
Current data suggest that the risk of hypertension rises in certain patients with tuberous sclerosis complex (TSC), including those with advanced chronic kidney disease (CKD)61, high angiomyolipoma stage or history of embolization procedures15. When children and adults with TSC are undergoing general anaesthesia, blood pressure should be monitored as part of their pre-anaesthesia assessment. Of note, in infants and young children with TSC, treatment with adrenocorticotropic hormone and corticosteroids increases the risk of hypertension significantly (up to 44%)187 and blood pressure (BP) monitoring should therefore be conducted more frequently than annually for these patients. ABPM, ambulatory blood pressure monitoring; ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; eGFR, estimated glomerular filtration rate; P95, 95th percentile.
The choice of antihypertensive agent can also be affected by the presence or absence of CKD with or without proteinuria and by lifestyle modifications. Given that large randomized controlled trials (RCTs) showed that sodium–glucose co-transporter 2 (SGLT2) inhibitors have benefits on mortality and CKD progression, we suggest that, even in the absence of specific evidence, these drugs should be considered for the TSC population.
Monitoring of kidney function
Kidney manifestations of TSC can present in early childhood and become increasingly common with age16. Compared with the general population, adults with TSC are at higher risk of developing progressive CKD69,70. In some cases, this CKD progression occurs without overt kidney involvement on imaging; therefore, kidney function monitoring using cystatin C or creatinine as well as urinary protein levels is advised in all adults with TSC (Box 3). Although children can have kidney lesions during early childhood, the risk of CKD detectable through blood tests (that is, through raised serum creatinine levels) is extremely low60,71. Therefore, in children without kidney involvement on imaging, estimated GFR (eGFR) monitoring can be reasonably deferred until adulthood. Of note, in patients with low muscle mass owing to severe neurological complications, standard creatinine-based equations can overestimate eGFR and cystatin C-based equations might be more accurate72,73. In cases of progressive CKD, general patient follow-up guidelines should be followed as no data suggest that children or adults with TSC should be managed differently74. Kidney function might need to be monitored more frequently after bleeding episodes and after embolization, until it stabilizes75,76. In cases of unexplained eGFR decline, attention to T2-weighted imaging for increased water in the kidney cortex or a kidney biopsy might be necessary to identify the microcystic variety of TSC kidney disease77,78.
Following the start of mTORC1 inhibitor therapy, most kidney angiomyolipomata shrink within the first 12 months and then remain stable20. However, one study79 reported that mTORC1 inhibitors did not prevent CKD progression in a minority of patients with impaired kidney function (eGFR <30 ml/min/1.73 m2). Of note, mTORC1 inhibitor therapy can lead to or exacerbate proteinuria, which should therefore be monitored before starting this treatment. Moreover, eGFR and proteinuria should be assessed every 3–12 months in patients receiving an mTORC1 inhibitor79. No evidence suggests that the investigation or treatment approach should be different for patients with TSC treated with an mTORC1 inhibitor compared with other patients with CKD80.
Children with TSC and kidney cysts might have polyuria owing to a urine-concentrating defect, placing them at risk of nocturnal enuresis81. However, owing to the theoretical risk of kidney cyst progression with vasopressin analogues (for example, desmopressin) reported in other cystic kidney diseases82, we advise against the use of these agents to manage nocturnal enuresis in children with TSC.
No data suggest that kidney stones, kidney cyst complications83,84,85 or urinary tract infections should be managed differently in children and adults with TSC compared with the general population. Children with TSC might have additional risk factors for kidney stone formation, including but not limited to the use of topiramate or a ketogenic diet for the treatment of epilepsy, and immobility in patients with severe neurological involvement86. These patients might benefit from biochemical monitoring of urine to detect an increased risk of kidney stone formation.
TSC2–PKD1 contiguous gene syndrome
An extensive kidney cystic phenotype is indicative of TSC2–PKD1 contiguous gene syndrome but diagnosis is confirmed by genetic testing. The genotype determines the rate of disease progression, including very severe manifestations in childhood87,88. Onset of cysts with rapid growth at an early age should alert clinicians and prompt early and multidisciplinary management at both clinical and radiological levels, with increased monitoring of blood pressure and kidney function.
Imaging and biopsy
Methods for kidney imaging in TSC
Kidney imaging aims to detect, characterize and monitor changes in TSC-associated tumours (angiomyolipomata, cysts and RCC), assess the risk of complications (mostly spontaneous bleeding of angiomyolipomata), and evaluate the response to therapeutic interventions (Box 4).
Angiomyolipomata are benign tumours most often characterized by the presence of intratumoural macroscopic fat. However, the amount of fat varies across tumours. Fat-poor angiomyolipomata (that is, without discernible fat on imaging) are frequent in patients with TSC and/or with lymphangioleiomyomatosis (LAM)89,90,91 and can be difficult to differentiate from other solid kidney tumours92. Moreover, the vessels within angiomyolipomata are fragile because they lack a complete elastic layer; microaneurysms can therefore appear on these vessels and bleed spontaneously93,94. TSC-associated angiomyolipomata tend to be multiple and bilateral. In patients with TSC2 pathogenic variants, angiomyolipomata arise at a younger age, are more prone to bleeding complications and grow faster than in those with sporadic angiomyolipomata16,93,95. In some advanced forms of the disease, coalescent angiomyolipomata can infiltrate the kidney parenchyma diffusely and lead to progressive CKD15,89,94,96. Kidney cysts in patients with TSC are usually asymptomatic and the presence of multiple cysts early in life might suggest PKD due to TSC2–PKD1 contiguous gene syndrome.
Three modalities can be used for kidney imaging: ultrasound, CT and MRI. No study has compared their accuracy in patients with TSC. Of note, although cysts can be easily detected with all three modalities, there are differences in detection accuracy for angiomyolipomata and RCC.
Angiomyolipomata usually appear hyperechoic and homogeneous in ultrasound imaging. However, these characteristics are not pathognomonic given that up to 8% of RCCs are hyperechoic96,97,98. In addition, some fat-poor angiomyolipomata might be isoechoic and difficult to detect on ultrasound94. Characterization of solid kidney lesions in paediatric patients with TSC could be refined with contrast-enhanced ultrasound99. Importantly, ultrasound does not deliver radiation and has high accuracy in patients with small body habitus. However, ultrasound results can be dependent on the experience of the operator and ultrasound accuracy decreases in patients with large body habitus, for whom CT and MRI provide better imaging of the kidneys.
CT is useful to detect macroscopic fat that appears as an area of negative density. However, its use in the follow-up of young patients is limited owing to cumulative radiation exposure96,97 and the need for intravenous contrast injections to ensure adequate lesion definition and assessment of intralesional microaneurysms100. Although the spatial resolution of MRI is lower than that of CT, it allows a multiparametric approach that can help characterize fat-poor angiomyolipomata101,102. Of note, similar to CT, contrast injection might be needed to better assess microaneurysms with MRI. CT and MRI also enable more precise lesion measurements than ultrasound, especially for coalescent lesions97. Diffuse infiltration of the kidney parenchyma by angiomyolipomata complicates lesion measurement, but serial CT or MRI acquired along similar planes still provides a better follow-up than ultrasound.
Overall, MRI is the preferred imaging technique to diagnose and follow-up TSC-related kidney tumours because it does not deliver ionizing radiation and has good soft tissue contrast even in the absence of contrast agents. However, the use of MRI has some limitations as it is not available in all centres and certain patient populations, including children and patients with claustrophobia or psychodevelopmental disorders, require general anaesthesia.
Risk factors for angiomyolipoma bleeding
The severity of spontaneous angiomyolipoma bleeding is highly variable and ranges from limited perirenal haematoma to life-threatening internal haemorrhage. Data on the risk factors for bleeding events in patients with TSC and kidney angiomyolipomata are very limited. No prospective studies have assessed the effect of intervention versus observation on the outcomes of TSC-associated angiomyolipomata bleeding. Of note, such studies might not be feasible given that the rate of spontaneous angiomyolipoma bleeding might be as low as 5% in very large cohorts of patients with TSC16. Consequently, bleeding risk factors have only been assessed in retrospective studies (prone to selection bias) in which most patients had sporadic angiomyolipomata. Size seems to be a major bleeding predictor (Box 5) — the average diameter of angiomyolipomata treated for bleeding was ≥70 mm in most studies103,104,105,106. However, many cut-off diameters have been suggested for preventive intervention: 30 mm (ref. 107), 35 mm (ref. 108), 40 mm (refs. 109,110), 50 mm (ref. 104), 60 mm (ref. 105), 73.5 mm (ref. 106) and 80 mm (refs. 103,111). This variability results from the difficulty in predicting bleeding based on size alone — not only can small (<40 mm) angiomyolipomata bleed, albeit rarely112, but most large angiomyolipomata never bleed, even in patients with TSC16,113,114. Thus, the optimal size threshold for intervention depends on the number of patients one is ready to treat to prevent one bleeding event. The 30 mm threshold proposed by the Washington conference107 corresponds to a safety strategy aimed at minimizing the risk of bleeding as much as possible.
Other reported risk factors include female sex16, age (15–50 years)106,113, TSC2 pathogenic variant16, the presence of symptoms (flank or abdominal pain, haematuria, nausea or vomiting)109,115, the presence of microaneurysms of >5 mm within the tumour116, increased tumour vascularity110,117, exophytic growth110 and high BMI106 (Box 5). However, how these factors should be combined to improve the prediction of bleeding remains unclear. One group developed a multivariate score including symptoms at presentation, tumour size, tumour vascularity and degree of exophytic growth. All four variables were evaluated individually, and a total score was then calculated (low risk 0–6; high risk 7–9), which was validated in an independent internal cohort with good results110.
Surveys among patients and evaluation of insurance claims showed that kidney imaging surveillance is lacking or inadequate in a substantial proportion of patients with TSC118,119. Yet, strict kidney imaging follow-up is needed to detect patients with rapidly progressing cysts that might have contiguous gene syndrome, to monitor the risk of bleeding due to angiomyolipoma rupture and to detect rapidly growing masses that might be indicative of RCC.
Age correlates strongly with the frequency, number and size of kidney lesions in patients with TSC15,16,120,121. The growth rate of angiomyolipomata is slow before adolescence and accelerates thereafter, then slowing down after the age of 40 years16,17,96,122. These data are in line with observed bleeding complications, which occur mostly between the ages of 15 and 50 years, although bleeding risk is present at any age15,16,113.
Risk of RCC and indication for biopsy
Cases of kidney cancer in children or adults with TSC, sometimes with the presence of multiple tumours123,124,125,126,127, have prompted the hypothesis that TSC might be a risk factor for kidney malignancies. However, this view remains controversial128. RCC in TSC is most often of the chromophobe or chromophobe-oncocytic subtype129,130, and multifocal RCC in two patients with RCC demonstrated the existence of distinct ‘second-hit’ genetic initiating events131. Several studies reported that the prevalence of kidney cancer is 1.4–4% in patients with TSC128,130,131,132. These estimations must be interpreted with care given potential selection biases, lack of histological confirmation in some reports and the presence of complex histology without definitive criteria to discriminate between RCC and angiomyolipoma.
Although advances in multiparametric MRI can help characterize kidney masses101,102, imaging alone cannot rule out kidney cancer in the case of fat-poor solid kidney masses91,92,97. Because fat-poor angiomyolipomata are frequent in patients with TSC, the absence of macroscopic fat within the mass is not sufficient to indicate biopsy89,90,91,96 (Box 6). The best criterium to suspect kidney cancer in patients with TSC remains the observation of rapid, sustained growth (>0.5 cm/year) at serial evaluations, although some angiomyolipomata grow rapidly17,90,91,133. Kidney cancers might also be present in lesions that do not respond to mTORC1 inhibitors134.
Treatment and management
Rationale for intervention
mTORC1 inhibition is the central therapeutic option for the kidney manifestations of TSC and this pharmacological approach needs to be compared with interventional radiological and surgical procedures. Findings from several high-quality studies on mTORC1 inhibitors in TSC were pooled in a meta-analysis135. Data from 621 patients with TSC-related angiomyolipomata showed that mTORC1 inhibitor use reduced the nephrectomy rate over time, thereby reducing the long-term risk of CKD in this cohort136. Data from 99 patients with TSC in France who underwent kidney replacement therapy demonstrated the increased risk of kidney failure in patients who had a history of nephrectomy or embolization61. Data from 351 patients with TSC in the Netherlands also demonstrated an increased risk of CKD in patients requiring arterial embolization15. Combined, these data justify the preference of medical over surgical or interventional therapy where possible to minimize the risk of CKD (Fig. 2). Moreover, mTORC1 inhibition not only has an impact on the size and growth rate of TSC-associated angiomyolipomata but also on intratumoural aneurysms137, which is an additional benefit given the important role of aneurysms in bleeding risk. Regarding cystic kidney disease in TSC, large cysts do not seem to respond to mTORC1 inhibition, although current evidence indicates some benefit in reducing the large burden of small cortical cysts as well as in microcystic and focal cystic disease138.
In cases of acute haemorrhage of an angiomyolipoma, radiological intervention should be considered as the first-line approach. If not directly available, patient management should not be delayed and surgery should be initiated (employing a nephron-sparing approach, if possible, in the acute setting). Upon determination of substantial bleeding risk of an angiomyolipoma (Box 5), mechanistic target of rapamycin complex 1 (mTORC1) inhibition is the first-line approach. If no response to this treatment is observed or its further use is limited by side effects, reassessment and consideration of alternative strategies are required. TSC, tuberous sclerosis complex. aWith haemodynamic compromise or without spontaneous termination; in cases of moderate self-limiting bleeding, medical (intensive care or transfusion) or conservative management might be an option.
In patients who are haemodynamically unstable owing to TSC-related kidney complications, medical therapy will not be sufficiently fast and such patients should undergo an interventional endovascular radiological procedure or, in some cases, a surgical intervention. Moreover, in patients where medical therapy is contraindicated or has failed, surgical or radiological interventions can be considered, accepting the increased risk of CKD.
mTORC1 inhibition-based therapy
Several studies demonstrated the benefit of mTORC1 inhibition in angiomyolipomata of >3 cm in diameter20,139. Given that the overall angiomyolipoma burden is associated with the future risk of CKD, experts agree that using mTORC1 inhibitor preventatively before any individual lesion has become >3 cm in diameter might be beneficial in cases of rapid angiomyolipomata growth (>0.5 cm per year in diameter) and high overall angiomyolipoma burden in the kidneys (Box 7).
Fat-poor angiomyolipomata tend to respond well to mTORC1 inhibition140. Indeed, mTORC1 inhibitors primarily affect the highly vascularized compartments of angiomyolipomata141,142,143. The adverse effect profile of mTORC1 inhibitors is acceptable (see below). Furthermore, long-term eGFR is preserved in patients with TSC treated with mTORC1 inhibitors79 (one study reported improvement144) compared with surgery or interventional radiology15,67,136.
Dosage
In the paediatric EXIST-1 RCT, which reported the impact of everolimus on angiomyolipoma in patients with TSC treated for subependymal giant cell astrocytoma145, the initial dose was 4.5 mg/m2/day. In EXIST-2, an RCT examining everolimus in patients with either TSC-associated or LAM-associated angiomyolipoma, everolimus was administered at a fixed dose of 10 mg/day20. Both trials adjusted the dose to achieve target trough levels of 5–15 ng/ml. EXIST-2 included 118 patients randomly assigned 2:1 to receive everolimus 10 mg (n = 79) or placebo (n = 39) once daily, and peak and trough concentrations of everolimus in blood remained stable over time146. The mean everolimus trough level in both adults (EXIST-2) and children (EXIST-1) was <10 ng/ml at all timepoints145,147.
Several other non-randomized studies used similar dosing strategies as EXIST-1 and EXIST-2 (refs. 148,149,150,151). The dose of 10 mg in EXIST-2 was primarily chosen based on maximum tolerated dose considerations. Dose adjustments were possible based on side effects and safety. After initiating the treatment with a 10 mg dose, the EXIST-2 trial reported dose adjustments for adverse events in 48% of patients receiving everolimus. Nonetheless, the treatment efficacy remained robust, in agreement with previous data on sirolimus showing efficacy irrespective of dose or trough levels19. In a retrospective study of 50 adult patients with TSC, 5 mg of everolimus per day was safe and as effective in the shrinkage of angiomyolipoma as the conventional dose (10 mg of everolimus per day)152. The inclusion criteria for the low-dose option were kidney dysfunction (defined as serum creatinine level ≥1.5 mg/dl) or low body weight (body weight <35 kg). Taken together, therapy can be started at 10 mg/day in adults or 4.5 mg/m2/day in children following the strategy from EXIST-2. Considering the weak relationship between trough levels and angiomyolipoma response observed146, the ability to monitor treatment response by imaging and the observation that immediate responses are rarely required in TSC-associated angiomyolipoma, a starting dose of 5 mg per day for adults and 2.5 mg/m2 for children seems a reasonable approach to ensure optimal adherence and minimal toxicity (Box 8). Of note, although not primarily indicated to guide dosing, trough levels can be helpful to assess adherence and avoid toxicity.
In a prospective observational cohort of 26 patients with TSC and angiomyolipoma of ≥4 cm in diameter, intermittent everolimus treatment (that is, pausing of treatment upon response and re-initiation upon documented growth) was effective for tumour control and management of adverse events. The everolimus dose was set at 10 mg once a day, and the criteria for stopping everolimus treatment were reduction of angiomyolipoma size to ≤4 cm, everolimus administration for ≥12 months or plateauing reduction of angiomyolipoma size. An abdominal CT or MRI scan was carried out every 3 months and, if the volume of the angiomyolipoma after withdrawal increased to >70% of the pretherapeutic volume, everolimus treatment was restarted at the initial dose153. This concept could be adopted to individualize patient treatment but most studies to date have not followed this approach.
No RCTs have assessed the use of sirolimus (also known as rapamycin) to treat kidney manifestations of TSC. However, based on the identical mode of action (mTORC1 inhibition) as well as on available data from two non-randomized studies, sirolimus might be an alternative to everolimus based on availability. In a 24-month prospective open-label, single-arm, single-centre phase II–III study, 17 patients with TSC aged >10 years presenting with at least one kidney angiomyolipoma of >2 cm in diameter were exposed to an increasing dose of rapamycin (1 mg every 2 weeks) to achieve stable plasma levels of between 4 and 8 ng/ml. According to Response Evaluation Criteria in Solid Tumours (RECIST) criteria, all patients achieved a partial response at year 1 and all but two had already achieved this partial response after 6 months154. In a 2-year multicentre phase II non-randomized, open-label trial, 16 patients with TSC with sporadic LAM and/or kidney angiomyolipoma were treated with oral sirolimus for up to 2 years. Steady-state blood levels were 3–10 ng/ml. Summated angiomyolipoma diameters decreased in all 16 patients and even by ≥30% in eight of these individuals155.
Duration and discontinuation
The median time for angiomyolipomata to respond to mTORC1 inhibitors was ~3 months in EXIST-2 (ref. 20). Therefore, a minimal follow-up of 6 months is required before assessing the clinical and radiological response (Box 9). Furthermore, the main effect of mTORC1 inhibitors in reducing angiomyolipoma volume was observed within the first 6–12 months of exposure19,20,148. Therefore, lack of an effect of mTORC1 inhibition on angiomyolipoma growth after a minimal follow-up of 12 months should prompt exploration of adherence, dosage and confirmation that the lesion is indeed a typical angiomyolipoma as well as alternative treatment options (discussed below). A potential decision for discontinuation based on continued growth under therapy should also consider the evidence for beneficial effects of mTORC1 inhibition on bleeding risk156. Follow-up studies, including the EXIST-2 cohort, support the ongoing efficacy and safety of mTORC1 inhibitors up to 4 years after treatment initiation156. Most adverse events (see below) with mTORC1 inhibitors are minor and predictable157. Dose adjustments might be helpful considering a pragmatic risk–benefit balance158. Importantly, mTORC1 inhibition should be discontinued (at least temporarily) in patients who are experiencing infection or severe adverse events. Note that discontinuing mTORC1 inhibition therapy might cause re-growth of angiomyolipomata as suggested in a post hoc analysis of a subgroup of the EXIST-2 study159. Therefore, monitoring of angiomyolipomata through imaging remains essential after discontinuation of mTORC1 inhibition (Box 10).
Side effects
Everolimus is generally well tolerated in both adult and paediatric patients with TSC, with most adverse events being of grade 1 or 2 severity and occurring within the first 6 months147,148. The side effects of mTORC1 inhibition are not specific to patients with TSC. The most common grade 1 or 2 adverse events caused by mTORC1 inhibitors in patients with TSC are aphthous stomatitis, irregular menstruation, hypercholesterolaemia or hypertriglyceridaemia, urinary tract infection, hypertension, dermatitis acneiform, insomnia and interstitial lung disease148,149. The most common grade 3 adverse events are irregular menstruation and aphthous stomatitis150. Of note, the incidence of stomatitis and irregular menstruation correlates with the dosage of everolimus152. The impact of mTORC1 inhibitor-associated hyperlipidaemia on cardiovascular outcomes is unclear; interestingly, data from animal models suggest that sirolimus can attenuate atherosclerotic plaque progression160,161. The FDA and EMA as well as national resources about drug safety and efficacy are useful for continuing pharmacosurveillance on the use of mTORC1 inhibitors. Nephrotoxicity has not been reported in patients with TSC exposed to everolimus, except for patients with severely compromised kidney function before treatment or patients with prior kidney intervention20,162. Some of these patients experienced an increase in proteinuria. The diagnostic algorithm of mTORC1 inhibitor-induced proteinuria is similar to that of the general population as described in the latest CKD guidelines by the KDIGO consortium163. Electrolyte, glucose and liver function monitoring is required for all patients treated with an mTORC1 inhibitor, irrespective of a TSC diagnosis.
Immunosuppressive regimens after kidney transplantation
No RCTs have examined the impact of different immunosuppressive regimens after kidney transplantation in patients with TSC67,164. Nonetheless, based on the effect of mTORC1 inhibition on several TSC-associated phenotypes, a regimen containing an mTORC1 inhibitor in the context of TSC-associated phenotypes known to respond to mTORC1 inhibition (for example, angiomyolipoma, subependymal giant cell astrocytoma, epilepsy, skin manifestations and LAM) should be considered165.
Interventional radiology
In most centres, an actively bleeding angiomyolipoma of any tumour size is an accepted indication for arterial embolization owing to the minimal invasiveness of the procedure166,167 (Fig. 2 and Box 11). However, in cases with moderate self-limiting bleeding, medical or conservative management can also be considered168,169. In asymptomatic angiomyolipoma, the potential benefit of arterial embolization is less clear. Expert opinion suggests preventive arterial embolization of angiomyolipoma with a threshold diameter >4 cm, especially in lesions with rich angiomatous content and distinct arterial supply166.
Arterial embolization is less invasive than surgery and thus the first-line approach for the treatment of relevant angiomyolipoma haemorrhaging. In the decision-making process regarding surgery as an alternative to arterial embolization, several factors should be considered: whether the blood supply allows selective arterial embolization, RENAL score170, comorbidities and risk of general anaesthesia, number and position of lesions within the kidney, and the technical skills of the interventional radiologist performing the procedure. In particular, effective targeting of the angiomatous arteries and avoidance of non-target embolization is key to avoiding nephron loss171. The RENAL nephrometry score is based on five anatomical characteristics of solid renal masses — radius, exophytic or endophytic aspect, nearness to the collecting system or sinus, anterior (a) or posterior (p) location, location with respect to the polar lines, and contact with the main renal artery or vein — and is used to quantify the degree of difficulty of a surgical approach172. Steroid prophylaxis has been used successfully to prevent post-embolization syndrome after treatment of TSC-associated angiomyolipoma with arterial embolization173,174. If embolization fails or is unavailable, surgery needs to be considered.
Surgical intervention
Partial nephrectomy is feasible in populations undergoing surgery for angiomyolipoma with minimal morbidity175; this approach seems appropriate for cases selected by the multidisciplinary decision algorithm as it maximizes preservation of normal kidney parenchyma in patients with TSC who are at risk of kidney failure (Box 11).
In RCC, many studies have demonstrated that partial nephrectomy can prevent CKD development and ensuant morbidity and mortality. Although patients with TSC can present with angiomyolipoma and concomitant RCC130,176, enucleation might still be appropriate. In the case of sporadic RCC, tumour enucleation, if technically possible, yields oncological results comparable to those of tumour resection with a safety margin; tumour enucleation is therefore a parenchymal-sparing therapy option even if malignancy is suspected. In practice, a combined procedure (enucleoresection) is usually conducted. Of note, resection with a margin should be considered if RCC suspicion is high, especially high-grade RCC. In cases of haemodynamic instability, attempting partial nephrectomy might be hazardous and could even compromise survival. Where main kidney arterial clamping stabilizes the patient and nephron-sparing surgery seems to be technically straightforward to perform within a reasonable time frame, partial nephrectomy might remain an option; this expert opinion is based on first principles.
Nephrectomy before transplantation
Similar to patients with autosomal dominant PKD and kidney failure undergoing kidney transplantation, nephrectomy before transplantation might be warranted if the native kidney in patients with TSC occupies so much space that ipsilateral kidney transplantation is not technically feasible83. Of note, large contemporary cohort studies show a 1.4–2.8% major complication rate for nephrectomy177, with blood transfusion rates as high as 9.1%, whereas the rates of haematuria and bleeding were reported at 4.2% and 5.4%, respectively, in a 2020 report on patients with TSC16. Whether the risks of nephrectomy are counter-balanced by the benefits of avoiding bleeding episodes is therefore unclear. Additionally, if the goal of routine nephrectomy in transplant recipients with TSC is to avoid future bleeding events after transplantation, this concern might be addressed with the routine use of an mTORC1 inhibitor after grafting20,137.
Given the weak retrospective evidence, routine nephrectomy in patients with TSC undergoing kidney transplantation should be avoided. However, special consideration should be given to this procedure on a case-by-case basis, including in cases of suspected kidney malignancy or of an angiomyolipoma with a high risk of bleeding that cannot be treated with mTORC1 inhibitors. In this last scenario, nephrectomy might be considered a more definitive treatment compared with arterial embolization95,178. Bleeding risk can be assessed using multiple risk factors (Box 5).
Treatment of RCC in patients with TSC
No RCTs have examined differential therapy of TSC-associated RCC compared with sporadic RCC. Consequently, no evidence supports specific therapeutic approaches in TSC-associated RCC. Studies in sporadic RCC regarding the impact of mTOR pathway pathogenic variants, including TSC1 and TSC2, on the response to mTORC1 inhibition provide no conclusive data179,180,181,182 and studies in patients with TSC are lacking. Compared with sporadic RCC, TSC-associated RCC seems to have different histopathological patterns and a more indolent course126,130 with only rare cases of related mortality reported to date126,130,183. Although these observations do not affect general treatment strategies directly, they might still be considered in individualized decision-making and patient counselling126. Moreover, specific emphasis on nephron-sparing strategies is required considering the multiplicity and recurrent nature of kidney tumours in TSC126.
Multidisciplinary management
Because every organ system can be involved in TSC, care should be coordinated and delivered by a multidisciplinary team in an expert centre184 (Fig. 3 and Box 12). Although attention can be drawn to the most affected organ system, organ involvement changes with age and engagement with the multidisciplinary team members should be fostered early. Nephrology involvement is crucial to help educate patients and their families and to enable appropriate intervention as the disease progresses. All patients with TSC-associated kidney lesions technically have CKD stage 1 (or more advanced CKD) and should be followed by a nephrologist at least annually. Such involvement of a TSC nephrologist can help guide appropriate kidney care and reduce the frequency of unnecessary surgical interventions. Such care can also increase the use of best practices185.
This algorithm depicts the optimal multidisciplinary approach for patients suspected of having tuberous sclerosis complex (TSC). This approach includes appropriate referral to an expert centre and coordination of multidisciplinary care with emphasis on kidney issues. eGFR, estimated glomerular filtration rate; TAND, TSC-associated neuropsychiatric disease.
Another responsibility of the multidisciplinary team is to care for the family as well as the patient. Discussing screening with family members is therefore recommended. Family members with TSC clinical features should be screened for the relevant pathogenic variant, if it is known; genetic testing has little value in family members with no clinical features of TSC. However, this opinion is subject to clinical judgement for individual patients and families.
Transition care
Another obligation of the multidisciplinary team is the creation of a plan or protocol for the transition from paediatric to adult care. This plan should include the specified age of transition, the steps in the process and the identification of health-care professionals for adult care. Medical issues and concerns change as the patient ages and can pose challenges for patients who transition to adult-oriented care186. Ideally, establishing a fully functional multidisciplinary TSC clinic for adults should be undertaken simultaneously with the efforts to develop a paediatric clinic or the same clinic should be used for both children and adults. The transition to adult medical care is especially challenging for adults who have a TSC-associated intellectual disability and other TSC-associated neuropsychiatric disorders. The adult clinic must be capable of handling all of those TSC-associated issues.
Conclusion
Patients with TSC are most often initially encountered in non-specialized centres where awareness of TSC-associated kidney disease development is limited. This lack of awareness can hamper optimal patient management. Many studies have investigated TSC-associated kidney disease. Here, we summarized expert recommendations on the renal management of these patients with TSC, including diagnosis and monitoring of kidney involvement, as well as available treatment options. These recommendations should inform health-care decisions for patients with TSC to reduce the disease burden and improve prognoses for this vulnerable population.
References
Bissler, J. J. & Christopher Kingswood, J. Renal manifestation of tuberous sclerosis complex. Am. J. Med. Genet. C Semin. Med. Genet. 178, 338–347 (2018).
Crino, P. B., Nathanson, K. L. & Henske, E. P. The tuberous sclerosis complex. N. Engl. J. Med. 355, 1345–1356 (2006).
Yates, J. R. Tuberous sclerosis. Eur. J. Hum. Genet. 14, 1065–1073 (2006).
Kingswood, J. C. et al. Renal angiomyolipoma in patients with tuberous sclerosis complex: findings from the TuberOus SClerosis registry to increase disease awareness. Nephrol. Dial. Transpl. 34, 502–508 (2019).
Zollner, J. P. et al. A systematic review on the burden of illness in individuals with tuberous sclerosis complex (TSC). Orphanet J. Rare Dis. 15, 23 (2020).
Bissler, J. J. & Kingswood, J. C. Optimal treatment of tuberous sclerosis complex associated renal angiomyolipomata: a systematic review. Ther. Adv. Urol. 8, 279–290 (2016).
Shepherd, C. W., Gomez, M. R., Lie, J. T. & Crowson, C. S. Causes of death in patients with tuberous sclerosis. Mayo Clin. Proc. 66, 792–796 (1991).
Amin, S. et al. Causes of mortality in individuals with tuberous sclerosis complex. Dev. Med. Child Neurol. 59, 612–617 (2017).
Ewalt, D. H., Sheffield, E., Sparagana, S. P., Delgado, M. R. & Roach, E. S. Renal lesion growth in children with tuberous sclerosis complex. J. Urol. 160, 141–145 (1998).
Xu, Z., Wu, J., Xu, G. & Luo, H. Abdominal ultrasonographic manifestations in pediatric patients with tuberous sclerosis complex. Transl. Pediatr. 9, 757–767 (2020).
Ogorek, B. et al. TSC2 pathogenic variants are predictive of severe clinical manifestations in TSC infants: results of the EPISTOP study. Genet. Med. 22, 1489–1497 (2020).
Korula, S. et al. Renal manifestations of tuberous sclerosis among children: an Indian experience and review of the literature. Clin. Kidney J. 7, 134–137 (2014).
Di Pinto, D., Balestracci, A. & Delgado, N. Renal manifestations of tuberous sclerosis in children [Spanish]. Arch. Argent. Pediatr. 107, 436–440 (2009).
Mettin, R. R. et al. Wide spectrum of clinical manifestations in children with tuberous sclerosis complex — follow-up of 20 children. Brain Dev. 36, 306–314 (2014).
Eijkemans, M. J. et al. Long-term follow-up assessing renal angiomyolipoma treatment patterns, morbidity, and mortality: an observational study in tuberous sclerosis complex patients in the Netherlands. Am. J. Kidney Dis. 66, 638–645 (2015).
Kingswood, J. C. et al. Renal manifestations of tuberous sclerosis complex: key findings from the final analysis of the TOSCA study focussing mainly on renal angiomyolipomas. Front. Neurol. 11, 972 (2020).
Warncke, J. C. et al. Pediatric renal angiomyolipomas in tuberous sclerosis complex. J. Urol. 197, 500–506 (2017).
Northrup, H. et al. Updated International Tuberous Sclerosis Complex Diagnostic Criteria and Surveillance and Management Recommendations. Pediatr. Neurol. 123, 50–66 (2021).
Bissler, J. J. et al. Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N. Engl. J. Med. 358, 140–151 (2008).
Bissler, J. J. et al. Everolimus for angiomyolipoma associated with tuberous sclerosis complex or sporadic lymphangioleiomyomatosis (EXIST-2): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 381, 817–824 (2013).
Bissler, J. J. et al. Tuberous sclerosis complex exhibits a new renal cystogenic mechanism. Physiol. Rep. 7, e13983 (2019).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan — a web and mobile app for systematic reviews. Syst. Rev. 5, 210 (2016).
American Academy of Pediatrics Steering Committee on Quality Improvement and Management. Classifying recommendations for clinical practice guidelines. Pediatrics 114, 874–877 (2004).
Salussolia, C. L., Klonowska, K., Kwiatkowski, D. J. & Sahin, M. Genetic etiologies, diagnosis, and treatment of tuberous sclerosis complex. Annu. Rev. Genomics Hum. Genet. 20, 217–240 (2019).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Giannikou, K. et al. Low-level mosaicism in tuberous sclerosis complex: prevalence, clinical features, and risk of disease transmission. Genet. Med. 21, 2639–2643 (2019).
Tyburczy, M. E. et al. Mosaic and intronic mutations in TSC1/TSC2 explain the majority of TSC patients with no mutation identified by conventional testing. PLoS Genet. 11, e1005637 (2015).
Treichel, A. M. et al. Phenotypic distinctions between mosaic forms of tuberous sclerosis complex. Genet. Med. 21, 2594–2604 (2019).
Klonowska, K. et al. Comprehensive genetic and phenotype analysis of 95 individuals with mosaic tuberous sclerosis complex. Am. J. Hum. Genet. 110, 979–988 (2023).
Devuyst, O. & Pei, Y. Next-generation sequencing for detection of somatic mosaicism in autosomal dominant polycystic kidney disease. Kidney Int. 97, 261–263 (2020).
Treichel, A. M., Kwiatkowski, D. J., Moss, J. & Darling, T. N. A diagnostic algorithm for enhanced detection of mosaic tuberous sclerosis complex in adults. Br. J. Dermatol. 182, 235–237 (2020).
Kozlowski, P. et al. Identification of 54 large deletions/duplications in TSC1 and TSC2 using MLPA, and genotype-phenotype correlations. Hum. Genet. 121, 389–400 (2007).
Sampson, J. R. et al. Renal cystic disease in tuberous sclerosis: role of the polycystic kidney disease 1 gene. Am. J. Hum. Genet. 61, 843–851 (1997).
Lyczkowski, D. A. et al. Intrafamilial phenotypic variability in tuberous sclerosis complex. J. Child Neurol. 22, 1348–1355 (2007).
Northrup, H., et al. (University of Washington, Seattle Copyright © 1993-2023, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved., 1993).
Jones, A. C. et al. Comprehensive mutation analysis of TSC1 and TSC2-and phenotypic correlations in 150 families with tuberous sclerosis. Am. J. Hum. Genet. 64, 1305–1315 (1999).
Au, K. S. et al. Genotype/phenotype correlation in 325 individuals referred for a diagnosis of tuberous sclerosis complex in the United States. Genet. Med. 9, 88–100 (2007).
Dabora, S. L. et al. Mutational analysis in a cohort of 224 tuberous sclerosis patients indicates increased severity of TSC2, compared with TSC1, disease in multiple organs. Am. J. Hum. Genet. 68, 64–80 (2001).
Sancak, O. et al. Mutational analysis of the TSC1 and TSC2 genes in a diagnostic setting: genotype — phenotype correlations and comparison of diagnostic DNA techniques in tuberous sclerosis complex. Eur. J. Hum. Genet. 13, 731–741 (2005).
Kothare, S. V. et al. Severity of manifestations in tuberous sclerosis complex in relation to genotype. Epilepsia 55, 1025–1029 (2014).
Kothare, S. V. et al. Genotype/phenotype in tuberous sclerosis complex: associations with clinical and radiologic manifestations. Epilepsia 55, 1020–1024 (2014).
Avgeris, S. et al. Mutational analysis of TSC1 and TSC2 genes in tuberous sclerosis complex patients from greece. Sci. Rep. 7, 16697 (2017).
Bai, D., Zhao, J., Li, L., Gao, J. & Wang, X. Analysis of genotypes and phenotypes in Chinese children with tuberous sclerosis complex. Sci. China Life Sci. 60, 763–771 (2017).
Cai, Y., Li, H. & Zhang, Y. Assessment of tuberous sclerosis complex associated with renal lesions by targeted next-generation sequencing in mainland China. Urology 101, 170.e1–170.e7 (2017).
Lin, S. et al. Tuberous sclerosis complex in Chinese patients: phenotypic analysis and mutational screening of TSC1/TSC2 genes. Seizure 71, 322–327 (2019).
Ding, Y. et al. Genotype and phenotype analysis of Chinese children with tuberous sclerosis complex: a pediatric cohort study. Front. Genet. 11, 204 (2020).
Yang, G. et al. Phenotypic and genotypic characterization of Chinese children diagnosed with tuberous sclerosis complex. Clin. Genet. 91, 764–768 (2017).
Togi, S., Ura, H., Hatanaka, H. & Niida, Y. Genotype and phenotype landscape of 283 Japanese patients with tuberous sclerosis complex. Int. J. Mol. Sci. 23, 11175 (2022).
Rosset, C. et al. Molecular analysis of TSC1 and TSC2 genes and phenotypic correlations in Brazilian families with tuberous sclerosis. PLoS One 12, e0185713 (2017).
Alsowat, D. et al. The phenotypic spectrum of tuberous sclerosis complex: a Canadian cohort. Child Neurol. Open 8, 2329048x211012817 (2021).
Hung, C. C. et al. Molecular and clinical analyses of 84 patients with tuberous sclerosis complex. BMC Med. Genet. 7, 72 (2006).
Farach, L. S. et al. Tuberous sclerosis complex genotypes and developmental phenotype. Pediatr. Neurol. 96, 58–63 (2019).
Farach, L. S. et al. TSC2 c.1864C>T variant associated with mild cases of tuberous sclerosis complex. Am. J. Med. Genet. A 173, 771–775 (2017).
Khare, L. et al. A novel missense mutation in the GTPase activating protein homology region of TSC2 in two large families with tuberous sclerosis complex. J. Med. Genet. 38, 347–349 (2001).
Jansen, A. C. et al. Unusually mild tuberous sclerosis phenotype is associated with TSC2 R905Q mutation. Ann. Neurol. 60, 528–539 (2006).
Hulshof, H. M. et al. Counselling in tuberous sclerosis complex: a survey on content and satisfaction in the Netherlands. Eur. J. Paediatr. Neurol. 25, 113–119 (2020).
Yang, X. Y. et al. Noninvasive prenatal diagnosis based on cell-free DNA for tuberous sclerosis: a pilot study. Mol. Genet. Genom. Med. 10, e1952 (2022).
Wang, X. et al. Prenatal diagnosis and intervention improve developmental outcomes and epilepsy prognosis in children with tuberous sclerosis complex. Dev. Med. Child Neurol. 64, 1230–1236 (2022).
Kotulska, K. et al. Prevention of epilepsy in infants with tuberous sclerosis complex in the EPISTOP trial. Ann. Neurol. 89, 304–314 (2021).
Janssens, P. et al. Renal progression factors in young patients with tuberous sclerosis complex: a retrospective cohort study. Pediatr. Nephrol. 33, 2085–2093 (2018).
Vabret, E., Couchoud, C., Lassalle, M. & Vigneau, C. From tuberous sclerosis complex to end stage renal disease: who are these patients? J. Nephrol. 34, 607–615 (2021).
Ruggenenti, P., Perna, A. & Remuzzi, G. ACE inhibitors to prevent end-stage renal disease: when to start and why possibly never to stop: a post hoc analysis of the REIN trial results. Ramipril Efficacy in Nephropathy. J. Am. Soc. Nephrol. 12, 2832–2837 (2001).
Duerr, M. et al. Increased incidence of angioedema with ACE inhibitors in combination with mTOR inhibitors in kidney transplant recipients. Clin. J. Am. Soc. Nephrol. 5, 703–708 (2010).
Cheung, A. K. et al. Executive summary of the KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 99, 559–569 (2021).
Williams, B. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 39, 3021–3104 (2018).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34, 1887–1920 (2016).
Flynn, J. T. et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Schrier, R. W. ACE inhibitors, left ventricular mass and renal cyst growth in ADPKD. Pharmacol. Res. 114, 166–168 (2016).
Bissler, J. et al. Long-term clinical morbidity in patients with renal angiomyolipoma associated with tuberous sclerosis complex. Urology 95, 80–87 (2016).
Vekeman, F. et al. Kidney involvement in tuberous sclerosis complex: the impact on healthcare resource use and costs. J. Med. Econ. 18, 1060–1070 (2015).
Malaga-Dieguez, L. et al. Early manifestations of renal disease in patients with tuberous sclerosis complex. Int. J. Nephrol. Renovasc. Dis. 10, 91–95 (2017).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Reese, P. P. & Feldman, H. I. More evidence that cystatin C predicts mortality better than creatinine. J. Am. Soc. Nephrol. 20, 2088–2090 (2009).
Stevens, P. E. & Levin, A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 158, 825–830 (2013).
Anis, O. et al. Selective arterial embolization for large or symptomatic renal angiomyolipoma: 10 years of follow-up. Urology 135, 82–87 (2020).
Lin, L. et al. Renal function, complications, and outcomes of a reduction in tumor size after transarterial embolization for renal angiomyolipomas: a meta-analysis. J. Int. Med. Res. 47, 1417–1428 (2019).
Kronick, J., Gabril, M. Y. & House, A. A. Microscopic kidney disease in tuberous sclerosis complex and treatment with mTOR inhibition. Am. J. Kidney Dis. 82, 772–775 (2023).
Bissler, J. J., Batchelor, D. & Kingswood, J. C. Progress in tuberous sclerosis complex renal disease. Crit. Rev. Oncog. 27, 35–49 (2022).
Bissler, J. J. et al. Effect of everolimus on renal function in patients with tuberous sclerosis complex: evidence from EXIST-1 and EXIST-2. Nephrol. Dial. Transpl. 34, 1000–1008 (2019).
Sharma, S. & Smyth, B. From proteinuria to fibrosis: an update on pathophysiology and treatment options. Kidney Blood Press. Res. 46, 411–420 (2021).
Ho, T. A. et al. Autosomal dominant polycystic kidney disease is associated with central and nephrogenic defects in osmoregulation. Kidney Int. 82, 1121–1129 (2012).
Janssens, P. et al. Expanding the role of vasopressin antagonism in polycystic kidney diseases: from adults to children? Pediatr. Nephrol. 33, 395–408 (2018).
Chapman, A. B. et al. Autosomal-dominant polycystic kidney disease (ADPKD): executive summary from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 88, 17–27 (2015).
Suwabe, T. et al. Clinical features of cyst infection and hemorrhage in ADPKD: new diagnostic criteria. Clin. Exp. Nephrol. 16, 892–902 (2012).
Jouret, F., Hogan, M. C. & Chebib, F. T. A practical guide for the management of acute abdominal pain with fever in patients with autosomal dominant polycystic kidney disease. Nephrol. Dial. Transpl. 37, 1426–1428 (2022).
Acharya, P. et al. Incidence and characteristics of kidney stones in patients on ketogenic diet: a systematic review and meta-analysis. Diseases 9, 39 (2021).
Reyna-Fabián, M. E. et al. TSC2/PKD1 contiguous gene syndrome, with emphasis on a case with an atypical mild polycystic kidney phenotype and a novel genetic variant. Nefrologia 40, 91–98 (2020).
Griffin, M. D. et al. Neonatal presentation of autosomal dominant polycystic kidney disease with a maternal history of tuberous sclerosis. Nephrol. Dial. Transpl. 12, 2284–2288 (1997).
Northrup, H., Krueger, D. A. & International Tuberous Sclerosis Complex Consensus Group. Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 international tuberous sclerosis complex consensus conference. Pediatr. Neurol. 49, 243–254 (2013).
Patel, U., Simpson, E., Kingswood, J. C. & Saggar-Malik, A. K. Tuberose sclerosis complex: analysis of growth rates aids differentiation of renal cell carcinoma from atypical or minimal-fat-containing angiomyolipoma. Clin. Radiol. 60, 665–673 (2005).
Avila, N. A., Dwyer, A. J. & Moss, J. Active surveillance of nonfatty renal masses in patients with lymphangioleiomyomatosis: use of CT features and patterns of growth to differentiate angiomyolipoma from renal cancer. AJR Am. J. Roentgenol. 209, 611–619 (2017).
Lane, B. R. et al. Clinical correlates of renal angiomyolipoma subtypes in 209 patients: classic, fat poor, tuberous sclerosis associated and epithelioid. J. Urol. 180, 836–843 (2008).
Rabenou, R. A. & Charles, H. W. Differentiation of sporadic versus tuberous sclerosis complex-associated angiomyolipoma. AJR Am. J. Roentgenol. 205, 292–301 (2015).
Dixon, B. P., Hulbert, J. C. & Bissler, J. J. Tuberous sclerosis complex renal disease. Nephron 118, e15–e20 (2011).
Koo, K. C. et al. Trends of presentation and clinical outcome of treated renal angiomyolipoma. Yonsei Med. J. 51, 728–734 (2010).
Rouviere, O., Nivet, H., Grenier, N., Zini, L. & Lechevallier, E. Kidney damage due to tuberous sclerosis complex: management recommendations. Diagn. Interv. Imaging 94, 225–237 (2013).
Buj Pradilla, M. J., Marti Balleste, T., Torra, R. & Villacampa Auba, F. Recommendations for imaging-based diagnosis and management of renal angiomyolipoma associated with tuberous sclerosis complex. Clin. Kidney J. 10, 728–737 (2017).
Jinzaki, M., Silverman, S. G., Akita, H., Mikami, S. & Oya, M. Diagnosis of renal angiomyolipomas: classic, fat-poor, and epithelioid types. Semin. Ultrasound CT MR 38, 37–46 (2017).
Chan, J. P. et al. Utility of contrast-enhanced ultrasound for solid mass surveillance and characterization in children with tuberous sclerosis complex: an initial experience. Pediatr. Nephrol. 36, 1775–1784 (2021).
Champagnac, J. et al. Microaneurysms in renal angiomyolipomas: can clinical and computed tomography features predict their presence and size? Diagn. Interv. Imaging 97, 321–326 (2016).
Heller, M. T., Furlan, A. & Kawashima, A. Multiparametric MR for solid renal mass characterization. Magn. Reson. Imaging Clin. N. Am. 28, 457–469 (2020).
Schieda, N. et al. Multicenter evaluation of multiparametric MRI clear cell likelihood scores in solid indeterminate small renal masses. Radiology 303, 590–599 (2022).
Dickinson, M., Ruckle, H., Beaghler, M. & Hadley, H. R. Renal angiomyolipoma: optimal treatment based on size and symptoms. Clin. Nephrol. 49, 281–286 (1998).
Sward, J., Henrikson, O., Lyrdal, D., Peeker, R. & Lundstam, S. Renal angiomyolipoma-patient characteristics and treatment with focus on active surveillance. Scand. J. Urol. 54, 141–146 (2020).
Kuusk, T. et al. Treatment of renal angiomyolipoma: pooled analysis of individual patient data. BMC Urol. 15, 123 (2015).
Lee, K. H. et al. Clinical behavior and management of three types of renal angiomyolipomas. J. Formos. Med. Assoc. 118, 162–169 (2019).
Krueger, D. A., Northrup, H. & International Tuberous Sclerosis Complex Consensus Group. Tuberous sclerosis complex surveillance and management: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference. Pediatr. Neurol. 49, 255–265 (2013).
Ruud Bosch, J. L. H. et al. Factors associated with the number and size of renal angiomyolipomas in sporadic angiomyolipoma (sAML): a study of adult patients with sAML managed in a Dutch tertiary referral center. Int. Urol. Nephrol. 50, 459–467 (2018).
Nelson, C. P. & Sanda, M. G. Contemporary diagnosis and management of renal angiomyolipoma. J. Urol. 168, 1315–1325 (2002).
Xu, X. F. et al. A scoring system based on clinical features for the prediction of sporadic renal angiomyolipoma rupture and hemorrhage. Medicine 99, e20167 (2020).
Dabbeche, C. et al. Role of embolization in renal angiomyolipomas [French]. J. Radiol. 87, 1859–1867 (2006).
Zeid, M. et al. Active surveillance for renal angiomyolipoma less than 4 centimeters: a systematic review of cohort studies. Cureus 14, e22678 (2022).
Cockerell, I. et al. Prevalence of renal angiomyolipomas and spontaneous bleeding related to angiomyolipomas in tuberous sclerosis complex patients in France and Norway — a questionnaire study. Urology 104, 70–76 (2017).
Bhatt, J. R. et al. Natural history of renal angiomyolipoma (AML): most patients with large AMLs >4cm can be offered active surveillance as an initial management strategy. Eur. Urol. 70, 85–90 (2016).
Ouzaid, I. et al. Active surveillance for renal angiomyolipoma: outcomes and factors predictive of delayed intervention. BJU Int. 114, 412–417 (2014).
Yamakado, K. et al. Renal angiomyolipoma: relationships between tumor size, aneurysm formation, and rupture. Radiology 225, 78–82 (2002).
Rimon, U. et al. Large renal angiomyolipomas: digital subtraction angiographic grading and presentation with bleeding. Clin. Radiol. 61, 520–526 (2006).
Cockerell, I. et al. Renal manifestations of tuberous sclerosis complex: patients’ and parents’ knowledge and routines for renal follow-up — a questionnaire study. BMC Nephrol. 19, 39 (2018).
Goedken, A. M., Samuels, J. A., Sato, T. S. & Harshman, L. A. Kidney imaging surveillance in commercially insured patients with tuberous sclerosis complex. Pediatr. Neurol. 117, 21–26 (2021).
Tsai, J. D., Wei, C. C., Chen, S. M., Lue, K. H. & Sheu, J. N. Association between the growth rate of renal cysts/angiomyolipomas and age in the patients with tuberous sclerosis complex. Int. Urol. Nephrol. 46, 1685–1690 (2014).
Rakowski, S. K. et al. Renal manifestations of tuberous sclerosis complex: incidence, prognosis, and predictive factors. Kidney Int. 70, 1777–1782 (2006).
Robert, A. et al. Renal involvement in tuberous sclerosis complex with emphasis on cystic lesions. Radiol. Med. 121, 402–408 (2016).
Lendvay, T. S., Broecker, B. & Smith, E. A. Renal cell carcinoma in a 2-year-old child with tuberous sclerosis. J. Urol. 168, 1131–1132 (2002).
Allison, J. W., James, C. A. & Figarola, M. S. Pediatric case of the day. Renal cell carcinoma in a child with tuberous sclerosis. Radiographics 19, 1388–1389 (1999).
Al-Saleem, T. et al. Malignant tumors of the kidney, brain, and soft tissues in children and young adults with the tuberous sclerosis complex. Cancer 83, 2208–2216 (1998).
Guo, J. et al. Tuberous sclerosis-associated renal cell carcinoma: a clinicopathologic study of 57 separate carcinomas in 18 patients. Am. J. Surg. Pathol. 38, 1457–1467 (2014).
Breysem, L., Nijs, E., Proesmans, W. & Smet, M. H. Tuberous sclerosis with cystic renal disease and multifocal renal cell carcinoma in a baby girl. Pediatr. Radiol. 32, 677–680 (2002).
Peron, A. et al. Do patients with tuberous sclerosis complex have an increased risk for malignancies? Am. J. Med. Genet. A 170, 1538–1544 (2016).
Henske, E. P., Cornejo, K. M. & Wu, C. L. Renal cell carcinoma in tuberous sclerosis complex. Genes 12, 1585 (2021).
Yang, P. et al. Renal cell carcinoma in tuberous sclerosis complex. Am. J. Surg. Pathol. 38, 895–909 (2014).
Tyburczy, M. E. et al. A shower of second hit events as the cause of multifocal renal cell carcinoma in tuberous sclerosis complex. Hum. Mol. Genet. 24, 1836–1842 (2015).
Sauter, M. et al. Rare manifestations and malignancies in tuberous sclerosis complex: findings from the TuberOus SClerosis registry to increAse disease awareness (TOSCA). Orphanet J. Rare Dis. 16, 301 (2021).
Yeoh, Z. W. et al. Natural history of angiomyolipoma in lymphangioleiomyomatosis: implications for screening and surveillance. Orphanet J. Rare Dis. 9, 151 (2014).
Battelli, C. & Cho, D. C. mTOR inhibitors in renal cell carcinoma. Therapy 8, 359–367 (2011).
Sasongko, T. H., Ismail, N. F. & Zabidi-Hussin, Z. Rapamycin and rapalogs for tuberous sclerosis complex. Cochrane Database Syst. Rev. 7, Cd011272 (2016).
Swallow, E. et al. Patterns of disease monitoring and treatment among patients with tuberous sclerosis complex-related angiomyolipomas. Urology 104, 110–114 (2017).
Bissler, J. J. et al. Everolimus for renal angiomyolipoma in patients with tuberous sclerosis complex or sporadic lymphangioleiomyomatosis: extension of a randomized controlled trial. Nephrol. Dial. Transpl. 31, 111–119 (2016).
Siroky, B. J. et al. Improvement in renal cystic disease of tuberous sclerosis complex after treatment with mammalian target of rapamycin inhibitor. J. Pediatr. 187, 318–322.e2 (2017).
Kingswood, J. C. et al. The effect of everolimus on renal angiomyolipoma in patients with tuberous sclerosis complex being treated for subependymal giant cell astrocytoma: subgroup results from the randomized, placebo-controlled, phase 3 trial EXIST-1. Nephrol. Dial. Transpl. 29, 1203–1210 (2014).
Watanabe, E. H. et al. The effect of sirolimus on angiomyolipoma is determined by decrease of fat-poor compartments and includes striking reduction of vascular structures. Sci. Rep. 11, 8493 (2021).
Wang, W. et al. CT characteristics predict the response to everolimus or sirolimus of renal angiomyolipomas in patients with tuberous sclerosis complex. Int. Urol. Nephrol. 51, 671–676 (2019).
Hatano, T. et al. Effect of everolimus treatment for regrown renal angiomyolipoma associated with tuberous sclerosis complex after transcatheter arterial embolization. Int. J. Clin. Oncol. 23, 1134–1139 (2018).
Brakemeier, S. et al. Treatment effect of mTOR-inhibition on tissue composition of renal angiomyolipomas in tuberous sclerosis complex (TSC). PLoS One 12, e0189132 (2017).
Zonnenberg, B. A. et al. Observational study of characteristics and clinical outcomes of Dutch patients with tuberous sclerosis complex and renal angiomyolipoma treated with everolimus. PLoS One 13, e0204646 (2018).
Bissler, J. J. et al. Effect of everolimus on renal function in patients with tuberous sclerosis complex (TSC): results from exist-1 and exist-2. Nephrol. Dial. Transplant. 29, iii43–iii44 (2014).
Budde, K. et al. Pharmacokinetics and pharmacodynamics of everolimus in patients with renal angiomyolipoma and tuberous sclerosis complex or lymphangioleiomyomatosis. Br. J. Clin. Pharmacol. 81, 958–970 (2016).
Bissler, J. J. et al. The effect of everolimus on renal angiomyolipoma in pediatric patients with tuberous sclerosis being treated for subependymal giant cell astrocytoma. Pediatr. Nephrol. 33, 101–109 (2018).
Hatano, T., Chikaraishi, K., Inaba, H., Endo, K. & Egawa, S. Outcomes of everolimus treatment for renal angiomyolipoma associated with tuberous sclerosis complex: a single institution experience in Japan. Int. J. Urol. 23, 833–838 (2016).
Robles, N. R. et al. Everolimus safety and efficacy for renal angiomyolipomas associated with tuberous sclerosis complex: a Spanish expanded access trial. Orphanet J. Rare Dis. 11, 128 (2016).
Cai, Y. et al. Assessing the outcomes of everolimus on renal angiomyolipoma associated with tuberous sclerosis complex in China: a two years trial. Orphanet J. Rare Dis. 13, 43 (2018).
Wu, C. Q., Wolf, D. S. & Smith, E. A. Fate of pediatric renal angiomyolipoma during mTOR inhibitor treatment in tuberous sclerosis complex. Urology 139, 161–167 (2020).
Hatano, T., Endo, K. & Tamari, M. Efficacy and safety of low-dose everolimus treatment for renal angiomyolipoma associated with tuberous sclerosis complex. Int. J. Clin. Oncol. 26, 163–168 (2021).
Hatano, T., Inaba, H., Endo, K. & Egawa, S. Intermittent everolimus administration for renal angiomyolipoma associated with tuberous sclerosis complex. Int. J. Urol. 24, 780–785 (2017).
Cabrera-López, C. et al. Assessing the effectiveness of rapamycin on angiomyolipoma in tuberous sclerosis: a two years trial. Orphanet J. Rare Dis. 7, 87 (2012).
Davies, D. M. et al. Sirolimus therapy for angiomyolipoma in tuberous sclerosis and sporadic lymphangioleiomyomatosis: a phase 2 trial. Clin. Cancer Res. 17, 4071–4081 (2011).
Bissler, J. J. et al. Everolimus long-term use in patients with tuberous sclerosis complex: four-year update of the EXIST-2 study. PLoS One 12, e0180939 (2017).
Bissler, J. J. et al. Everolimus for renal angiomyolipoma associated with tuberous sclerosis complex (TSC) from EXIST-2: continued efficacy and diminishing adverse events after ~3.5 years of treatment. Eur. Urol. Suppl. 14, e1 (2015).
Budde, K. et al. Predictive value of angiogenic biomarkers in tuberous sclerosis complex (TSC) patients with renal angiomyolipoma (AML). Eur. Urol. Suppl. 12, e981–e982 (2013).
Bissler, J. J. et al. Angiomyolipoma rebound tumor growth after discontinuation of everolimus in patients with tuberous sclerosis complex or sporadic lymphangioleiomyomatosis. PLoS One 13, e0201005 (2018).
Waksman, R. et al. Oral rapamycin inhibits growth of atherosclerotic plaque in apoE knock-out mice. Cardiovasc. Radiat. Med. 4, 34–38 (2003).
Pakala, R., Stabile, E., Jang, G. J., Clavijo, L. & Waksman, R. Rapamycin attenuates atherosclerotic plaque progression in apolipoprotein E knockout mice: inhibitory effect on monocyte chemotaxis. J. Cardiovasc. Pharmacol. 46, 481–486 (2005).
Franz, D. N. et al. Long-term use of everolimus in patients with tuberous sclerosis complex: final results from the EXIST-1 study. PLoS One 11, e0158476 (2016).
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 105, S1–S197 (2024).
Somers, M. J. & Paul, E. Safety considerations of mammalian target of rapamycin inhibitors in tuberous sclerosis complex and renal transplantation. J. Clin. Pharmacol. 55, 368–376 (2015).
Franz, D. N. et al. Effect of everolimus on skin lesions in patients treated for subependymal giant cell astrocytoma and renal angiomyolipoma: final 4-year results from the randomized EXIST-1 and EXIST-2 studies. J. Eur. Acad. Dermatol. Venereol. 32, 1796–1803 (2018).
Fernández-Pello, S. et al. Management of sporadic renal angiomyolipomas: a systematic review of available evidence to guide recommendations from the European Association of Urology renal cell carcinoma guidelines panel. Eur. Urol. Oncol. 3, 57–72 (2020).
Lenton, J., Kessel, D. & Watkinson, A. F. Embolization of renal angiomyolipoma: immediate complications and long-term outcomes. Clin. Radiol. 63, 864–870 (2008).
Danforth, T. L., Lane, B. R. & Novick, A. C. Conservative management of giant symptomatic angiomyolipomas in patients with the tuberous sclerosis complex. BJU Int. 100, 794–797 (2007).
Storm, D. W. & Mowad, J. J. Conservative management of a bleeding renal angiomyolipoma in pregnancy. Obstet. Gynecol. 107, 490–492 (2006).
Chan Park, M. et al. Varying outcomes among patients with large angiomyolipomas according to the treatment method. Urol. Int. 105, 680–686 (2021).
Andrassy, K. M. Comments on ‘KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 84, 622–623 (2013).
Kutikov, A. & Uzzo, R. G. The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J. Urol. 182, 844–853 (2009).
Bissler, J. J., Racadio, J., Donnelly, L. F. & Johnson, N. D. Reduction of postembolization syndrome after ablation of renal angiomyolipoma. Am. J. Kidney Dis. 39, 966–971 (2002).
Tsuchiya, S. et al. Prophylactic steroids for preventing postembolization syndrome after transcatheter arterial embolization of renal angiomyolipoma: a comparative study. Interv. Radiol. 8, 1–6 (2023).
Minervini, A. et al. Simple enucleation for the treatment of renal angiomyolipoma. BJU Int. 99, 887–891 (2007).
Yip, S. K., Tan, P. H., Cheng, W. S., Li, M. K. & Foo, K. T. Surgical management of angiomyolipoma: nephron-sparing surgery for symptomatic tumour. Scand. J. Urol. Nephrol. 34, 32–35 (2000).
Whiting, D. et al. Complications after radical nephrectomy according to age: analysis from the British Association of Urological Surgeons nephrectomy audit. J. Endourol. 36, 188–196 (2022).
Sooriakumaran, P. et al. Angiomyolipomata: challenges, solutions, and future prospects based on over 100 cases treated. BJU Int. 105, 101–106 (2010).
Voss, M. H. et al. PTEN expression, not mutation status in TSC1, TSC2, or mTOR, correlates with the outcome on everolimus in patients with renal cell carcinoma treated on the randomized RECORD-3 trial. Clin. Cancer Res. 25, 506–514 (2019).
Nassar, A. H. et al. Mutations and response to rapalogs in patients with metastatic renal cell carcinoma. Mol. Cancer Ther. 19, 690–696 (2020).
Kwiatkowski, D. J. et al. Mutations in TSC1, TSC2, and MTOR are associated with response to rapalogs in patients with metastatic renal cell carcinoma. Clin. Cancer Res. 22, 2445–2452 (2016).
Roldan-Romero, J. M. et al. PTEN expression and mutations in TSC1, TSC2 and MTOR are associated with response to rapalogs in patients with renal cell carcinoma. Int. J. Cancer 146, 1435–1444 (2020).
Bjornsson, J., Short, M. P., Kwiatkowski, D. J. & Henske, E. P. Tuberous sclerosis-associated renal cell carcinoma. Clinical, pathological, and genetic features. Am. J. Pathol. 149, 1201–1208 (1996).
Auvin, S. et al. A step-wise approach for establishing a multidisciplinary team for the management of tuberous sclerosis complex: a Delphi consensus report. Orphanet J. Rare Dis. 14, 91 (2019).
Fujimoto, A. et al. Establishment of a regional interdisciplinary medical system for managing patients with tuberous sclerosis complex (TSC). Sci. Rep. 8, 16747 (2018).
Thiele, E. A., Granata, T., Matricardi, S. & Chugani, H. T. Transition into adulthood: tuberous sclerosis complex, Sturge-Weber syndrome, and Rasmussen encephalitis. Epilepsia 55, 29–33 (2014).
McGarry, L., Messer, R., Cree-Green, M., Ray, K. & Knupp, K. Incidence of hypertension among children treated with adrenocorticotropic hormone (ACTH) or prednisolone for infantile spasms. J. Child Neurol. 35, 215–220 (2020).
Acknowledgements
This project was initiated by the Working Group for Autosomal Dominant Structural Kidney Disorders of ERKNet and supported by ERKNet. ERKNet is funded by the European Union within the framework of the EU4Health Programme (101085068). The manuscript was prepared in collaboration with the ERA working group G&K, of which R.U.M. is the Chair and D.M., C.B., F.J., M.L., O.D. and F.S. are members. D.M. is supported by the Research Foundation Flanders (FWO) (G0C8920N and G060623N) and a clinical senior research grant (1804123N). This Clinical Practice Recommendation has been endorsed by the following patient organizations and professional societies: European Tuberous Sclerosis Complex Association, Tuberous Sclerosis Complex International, European Society for Paediatric Nephrology, European Society of Urogenital Radiology, American Society of Paediatric Nephrology and the Tuberous Sclerosis Complex Alliance. The authors thank patients with tuberous sclerosis complex and their families for their trust and participation in research studies aimed at reducing the suffering of all patients with tuberous sclerosis complex, and for being a beacon of inspiration for clinicians and scientists to make things better.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content, and wrote, reviewed or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
S.S. is a Proctor for Intuitive Surgical System. D.J.K. has had research contracts with Genentech, AADI, and Revolution Medicines and has been a consultant to Genentech, AADI, Guidepoint, Bridgebio and Slingshot Insights. J.B.L. receives honorarium as an advisory board member for Novartis, Astellas, Pfizer, Roche, and Merck and is a consultant to Janssen. Bristol Myers Squibb conducts research at the centre that employs J.B.L. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Andrew A. House, Julian R. Sampson and John A. Sayer for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
EMA: http://www.ema.europa.eu/
FDA: http://www.fda.gov/
gnomAD browser: https://gnomad.broadinstitute.org/
Human Variome Project: https://databases.lovd.nl/shared/genes/TSC2
Supplementary information
Glossary
- Cortical tubers
-
A developmental brain lesion in which there is loss of normal cortical architecture with large ‘giant’ cells and gliosis.
- Enucleation
-
Tumour excision by blunt dissection along the natural cleavage plane between the peritumoural pseudocapsule and the kidney parenchyma. This method avoids the removal of visible kidney tissue.
- Enucleoresection
-
Minimally invasive endoscopic procedure used to remove kidney lesions.
- Expressivity
-
Refers to the extent and severity of tuberous sclerosis complex (TSC) symptoms and signs seen in an individual with TSC. For example, some individuals with a diagnosis of TSC have many cortical tubers, some have few and some have none.
- First principles
-
An approach used by Aristotle where complicated problems are reduced to fundamental elements and relationships and interventions can be posited to formulate solutions.
- Hyperechoic
-
The property of showing higher echogenicity (that is, appearing brighter on ultrasound images) than a tissue of reference.
- Isoechoic
-
The property of showing similar echogenicity to that of a tissue of reference.
- Post-embolization syndrome
-
An inflammatory response causing substantial fever and pain after arterial embolization.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mekahli, D., Müller, RU., Marlais, M. et al. Clinical practice recommendations for kidney involvement in tuberous sclerosis complex: a consensus statement by the ERKNet Working Group for Autosomal Dominant Structural Kidney Disorders and the ERA Genes & Kidney Working Group. Nat Rev Nephrol (2024). https://doi.org/10.1038/s41581-024-00818-0
Accepted:
Published:
DOI: https://doi.org/10.1038/s41581-024-00818-0