Abstract
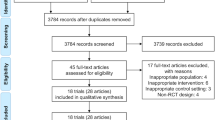
Increasing evidence indicates that exercise has beneficial effects on chronic inflammation, cardiorespiratory function, muscle and bone strength and metabolic markers in adults with chronic kidney disease (CKD), kidney failure or kidney transplants. However, the mechanisms that underlie these benefits have received little attention, and the available clinical evidence is mainly from small, short-duration (<12 weeks) exercise intervention studies. The available data, mainly from patients with CKD or on dialysis, suggest that exercise-mediated shifts towards a less inflammatory immune cell profile, enhanced activity of the NRF2 pathway and reduced monocyte infiltration into adipose tissue may underlie improvements in inflammatory biomarkers. Exercise-mediated increases in nitric oxide release and bioavailability, reduced angiotensin II accumulation in the heart, left ventricular remodelling and reductions in myocardial fibrosis may contribute to improvements in left ventricular hypertrophy. Exercise stimulates an anabolic response in skeletal muscle in CKD, but increases in mitochondrial mass and satellite cell activation seem to be impaired in this population. Exercise-mediated activation of the canonical wnt pathway may lead to bone formation and improvements in the levels of the bone-derived hormones klotho and fibroblast growth factor 23 (FGF23). Longer duration studies with larger sample sizes are needed to confirm these mechanisms in CKD, kidney failure and kidney transplant populations and provide evidence for targeted exercise interventions.
Key points
-
Shifts towards a less inflammatory monocyte and T cell profile, enhanced activity of the NRF2 pathway and reduced monocyte infiltration into adipose tissue might underlie exercise-mediated improvements in inflammatory biomarkers in people with chronic kidney disease (CKD) or on dialysis.
-
Exercise-mediated enhancements in nitric oxide release and bioavailability, reduced angiotensin II accumulation in the heart, left ventricular remodelling and reductions in myocardial fibrosis might improve left ventricular hypertrophy in CKD and kidney failure.
-
Few studies have examined the effects of exercise training on insulin resistance in people with CKD; however, early evidence suggests that a 6-month exercise intervention might have beneficial effects.
-
Exercise, particularly resistance exercise, stimulates an anabolic response in skeletal muscle in people with CKD; exercise-induced increases in mitochondrial mass and satellite cell activation seem to be impaired in this population.
-
Exercise-mediated activation of the canonical wnt pathway may lead to bone formation in CKD; reduced fibroblast growth factor-23 (FGF23) release and increased klotho release in bone might also contribute to improved bone mineral density and reduced bone loss.
-
Studies with longer durations and larger sample sizes are needed to confirm these potential mechanisms in all CKD and kidney failure populations and provide evidence to enable the development of effective targeted exercise interventions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Caspersen, C. J., Powell, K. E. & Christenson, G. M. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 100, 126–131 (1985).
Baker, L. A. et al. Clinical practice guideline exercise and lifestyle in chronic kidney disease. BMC Nephrol. 23, 75 (2022).
Girndt, M., Sester, U., Sester, M., Kaul, H. & Köhler, H. Impaired cellular immune function in patients with end-stage renal failure. Nephrol. Dial. Transpl. 14, 2807–2810 (1999).
Pertosa, G., Grandaliano, G., Gesualdo, L. & Schena, F. P. Clinical relevance of cytokine production in hemodialysis. Kidney Int. 76, S104–S111 (2000).
Stenvinkel, P. et al. IL-10, IL-6, and TNF-α: central factors in the altered cytokine network of uremia the good, the bad, and the ugly. Kidney Int. 67, 1216–1233 (2005).
Cobo, G., Lindholm, B. & Stenvinkel, P. Chronic inflammation in end-stage renal disease and dialysis. Nephrol. Dial. Transplant. 33, iii35–iii40 (2018).
Gupta, J. et al. Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC. Clin. J. Am. Soc. Nephrol. 7, 1938–1946 (2012).
Xiang, F. F. et al. Lymphocyte depletion and subset alteration correlate to renal function in chronic kidney disease patients. Ren. Fail. 38, 7–14 (2016).
UK Renal Registry. UK Renal Registry 24th Annual Report — data to 31/12/2020, Bristol, UK. https://ukkidney.org/audit-research/annual-report (2022).
Sun, J. et al. Biomarkers of cardiovascular disease and mortality risk in patients with advanced CKD. Clin. J. Am. Soc. Nephrol. 7, 1163–1172 (2016).
Viana, J. L. et al. Evidence for anti-inflammatory effects of exercise in CKD. J. Am. Soc. Nephrol. 25, 2121–2130 (2014).
Hemmati, N. et al. Effects of exercise training on immunological factors in kidney transplant recipients; a randomized controlled trial. Res. Sports Med. 30, 80–91 (2022).
Meléndez Oliva, E. et al. Effect of exercise on inflammation in hemodialysis patients: a systematic review. J. Pers. Med. 12, 1188 (2022).
Hale, K. H. et al. Multifunctional regulation of the biological effects of TNF by the soluble type I and type II TNF receptors. Cytokine 7, 26–38 (1995).
Dungey, M. et al. Regular exercise during haemodialysis promotes an anti-inflammatory leucocyte profile. Clin. Kidney J. 10, 813–821 (2017).
Shantsila, E. et al. Immunophenotypic characterization of human monocyte subsets: possible implications for cardiovascular disease pathophysiology. J. Thromb. Haemost. 9, 1056–1066 (2011).
Rogacev, K. S. et al. CD14++ CD16+ monocytes and cardiovascular outcome in patients with chronic kidney disease. Eur. Heart J. 32, 84–92 (2011).
Heine, G. H. et al. Monocyte subpopulations and cardiovascular risk in chronic kidney disease. Nat. Rev. Nephrol. 8, 362–369 (2012).
Muras-Szwedziak, K., Masajtis-Zagajewska, A., Pawłowicz, E. & Nowicki, M. Effects of a structured physical activity program on serum adipokines and markers of inflammation and volume overload in kidney transplant recipients. Ann. Transplant. 24, 569–575 (2019).
Hutchinson, G. M. et al. Effect of high intensity interval training and moderate intensity continuous training on lymphoid, myeloid and inflammatory cells in kidney transplant recipients. Exerc. Immunol. Rev. 28, 100–115 (2022).
Abreu, C. C. et al. Does resistance exercise performed during dialysis modulate Nrf2 and NF-κB in patients with chronic kidney disease? Life Sci. 188, 192–197 (2017).
Kim, H. J. & Vaziri, N. D. Contribution of impaired Nrf2-Keap1 pathway to oxidative stress and inflammation in chronic renal failure. Am. J. Physiol. Renal Physiol. 298, F662–F671 (2010).
Ahmed, S. M. U., Luo, L., Namani, A., Wang, X. J. & Tang, X. Nrf2 signalling pathway: pivotal roles in inflammation. Biochim. Biophys. Acta 1863, 585–597 (2017).
Bishop, N. C., Wadley, A. J., Hamrouni, M. & Roberts, M. J. Inactivity and obesity: consequences for macrophage-mediated inflammation and the development of cardiometabolic disease. Proc. Nutr. Soc. https://doi.org/10.1017/S0029665122002671 (2022).
Fuhro, M. I. et al. The impact of intradialytic exercise on immune cells expressing CCR5+ in patients with chronic kidney disease: a cross-over trial. Int. J. Artif. Organs 45, 221–226 (2022).
Martinez Cantarin, M. P., Whitaker-Menezes, D., Lin, Z. & Falkner, B. Uremia induces adipose tissue inflammation and muscle mitochondrial dysfunction. Nephrol. Dial. Transpl. 32, 943–951 (2017).
Chiu, Y. L. et al. A comprehensive characterization of aggravated aging-related changes in T lymphocytes and monocytes in end-stage renal disease: the iESRD study. Immun. Ageing 15, 27 (2018).
Duggal, N. A., Niemiro, G., Harridge, S. D. R., Simpson, R. J. & Lord, J. M. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nat. Rev. Immunol. 19, 563–572 (2019).
Tonelli, M. et al. Chronic kidney disease and mortality risk: a systematic review. J. Am. Soc. Nephrol. 17, 2034–2047 (2006).
van der Velde, M. et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int. 79, 1341–1352 (2011).
Chronic Kidney Disease Prognosis Consortium. et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375, 2073–2081 (2010).
Stevens, P. E. et al. Chronic kidney disease management in the United Kingdom: NEOERICA project results. Kidney Int. 72, 92–99 (2007).
Thompson, S. et al. Cause of death in patients with reduced kidney function. J. Am. Soc. Nephrol. 26, 2504–2511 (2015).
Webster, A. C., Nagler, E. V., Morton, R. L. & Masson, P. Chronic kidney disease. Lancet 389, 1238–1252 (2017).
Cozzolino, M. et al. Cardiovascular disease in dialysis patients. Nephrol. Dial. Transplant. 3, iii28–iii34 (2018).
Sarnak, M. J. et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108, 2154–2169 (2003).
Alexandrou, M. E. et al. Cardiorespiratory fitness assessed by cardiopulmonary exercise testing between different stages of pre-dialysis chronic kidney disease: a systematic review and meta-analysis. Nephrology 26, 972–980 (2021).
Lopes, A. A. et al. Associations of self-reported physical activity types and levels with quality of life, depression symptoms, and mortality in hemodialysis patients: the DOPPS. Clin. J. Am. Soc. Nephrol. 9, 1702–1712 (2014).
MacKinnon, H. J. et al. The association of physical function and physical activity with all-cause mortality and adverse clinical outcomes in nondialysis chronic kidney disease: a systematic review. Ther. Adv. Chronic Dis. 9, 209–226 (2018).
Tamiya, H. et al. Extended sedentary time increases the risk of all-cause death and new cardiovascular events in patients with diabetic kidney disease. Circ. J. 84, 2190–2197 (2020).
Fox, C. S. et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 380, 1662–1673 (2012).
Mahmoodi, B. K. et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: a meta-analysis. Lancet 380, 1649–1661 (2012).
Gansevoort, R. T. et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 382, 339–352 (2013).
Foley, R. N., Curtis, B. M., Randell, E. W. & Parfrey, P. S. Left ventricular hypertrophy in new hemodialysis patients without symptomatic cardiac disease. Clin. J. Am. Soc. Nephrol. 5, 805–813 (2010).
Maki, K. C., Wilcox, M. L., Dicklin, M. R., Kakkar, R. & Davidson, M. H. Left ventricular mass regression, all-cause and cardiovascular mortality in chronic kidney disease: a meta-analysis. BMC Nephrol. 23, 34 (2022).
Glassock, R. J., Pecoits-Filho, R. & Barberato, S. H. Left ventricular mass in chronic kidney disease and ESRD. Clin. J. Am. Soc. Nephrol. 4, S79–S91 (2009).
Tanaka, H. & Safar, M. E. Influence of lifestyle modification on arterial stiffness and wave reflections. Am. J. Hypertens. 18, 137–144 (2005).
Mustata, S., Chan, C., Lai, V. & Miller, J. A. Impact of an exercise program on arterial stiffness and insulin resistance in hemodialysis patients. J. Am. Soc. Nephrol. 15, 2713–2718 (2004).
Joyner, M. J. Effect of exercise on arterial compliance. Circulation 102, 1214–1215 (2000).
Toussaint, N. D., Polkinghorne, K. R. & Kerr, P. G. Impact of intradialytic exercise on arterial compliance and B-type natriuretic peptide levels in hemodialysis patients. Hemodial. Int. 12, 254–263 (2008).
Fagard, R. H. Exercise characteristics and the blood pressure response to dynamic physical training. Med. Sci. Sports Exerc. 33, S484–S492 (2001).
Gadelha, A. B. et al. Effects of pre-dialysis resistance training on sarcopenia, inflammatory profile, and anemia biomarkers in older community-dwelling patients with chronic kidney disease: a randomized controlled trial. Int. Urol. Nephrol. 53, 2137–2147 (2021).
Salhab, N. et al. Effect of intradialytic exercise on hyperphosphatemia and malnutrition. Nutrients 11, 2464 (2019).
Makhlough, A., Ilali, E., Mohseni, R. & Shahmohammadi, S. Effect of intradialytic aerobic exercise on serum electrolytes levels in hemodialysis patients. Iran. J. Kidney Dis. 6, 119–123 (2012).
Ito, O., Nakamura, T., Yamakoshi, S., Mori, N. & Masahiro, K. Effects of exercise training on renal damage and renin-angiotensin system in rats with chronic renal failure. Ann. Phys. Rehab. Med. 61, e82 (2018).
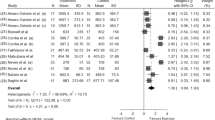
Graham-Brown, M. P. M. et al. A randomized controlled trial to investigate the effects of intra-dialytic cycling on left ventricular mass. Kidney Int. 99, 1478–1486 (2021).
Hayer, M. K. et al. Defining myocardial abnormalities across the stages of chronic kidney disease: a cardiac magnetic resonance imaging study. JACC Cardiovasc. Imaging 13, 2357–2367 (2020).
Penny, J. D. et al. Intradialytic exercise preconditioning: an exploratory study on the effect on myocardial stunning. Nephrol. Dial. Transpl. 34, 1917–1923 (2019).
McGuire, S. et al. Cardiac stunning during haemodialysis: the therapeutic effect of intra-dialytic exercise. Clin. Kidney J. 14, 1335–1344 (2021).
Giallauria, F. et al. Left ventricular remodelling in patients with moderate systolic dysfunction after myocardial infarction: favourable effects of exercise training and predictive role of N-terminal pro-brain natriuretic peptide. Eur. J. Cardiovasc. Prev. Rehabil. 15, 113–118 (2008).
Small, E. M. & Olson, E. N. Pervasive roles of microRNAs in cardiovascular biology. Nature 469, 336–342 (2011).
Kyselovič, J. & Varga, I. Research focused on microRNAs: a link between myocardial remodeling and growth during pathological processes and physical exercises. Ann. Transl. Med. 5, S20 (2017).
Pedersen, B. K. & Febbraio, M. A. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 8, 457–465 (2012).
Li, D. et al. Serum microRNA expression patterns in subjects after the 5-km exercise are strongly associated with cardiovascular adaptation. Front. Physiol. 12, 755656 (2021).
Estébanez, B., Jiménez-Pavón, D., Huang, C. J., Cuevas, M. J. & González-Gallego, J. Effects of exercise on exosome release and cargo in in vivo and ex vivo models: a systematic review. J. Cell. Physiol. 236, 3336–3353 (2021).
Van Guilder, G. P., Preston, C. C., Munce, T. A. & Faustino, R. S. Impacts of circulating microRNAs in exercise-induced vascular remodeling. Am. J. Physiol. Heart Circ. Physiol. 320, H2401–H2415 (2021).
Hou, Z. et al. Long term exercise-derived exosomal miR-342-5p: a novel exerkine for cardioprotection. Circ. Res. 124, 1386–1400 (2019).
Van Craenenbroeck, A. H. et al. Plasma levels of microRNA in chronic kidney disease: patterns in acute and chronic exercise. Am. J. Physiol. Heart Circ. Physiol. 309, H2008–H2016 (2015).
Kochan, Z., Szupryczynska, N., Malgorzewicz, S. & Karbowska, J. Dietary lipids and dyslipidaemia in chronic kidney disease. Nutrients 13, 3138 (2021).
Bulbul, M. C. et al. Disorders of lipid metabolism in chronic kidney disease. Blood Purif. 46, 144–152 (2018).
Spoto, B., Pisano, A. & Zoccali, C. Insulin resistance in chronic kidney disease: a systematic review. Am. J. Physiol. Renal Physiol. 311, F1087–F1108 (2016).
Chan, D. T., Watts, G. F., Irish, A. B. & Dogra, G. K. Insulin resistance and vascular dysfunction in chronic kidney disease: mechanisms and therapeutic interventions. Nephrol. Dial. Transplant. 32, 1274–1281 (2017).
Dave, N., Wu, J. & Thomas, S. Chronic kidney disease-induced insulin resistance: current state of the field. Curr. Diab. Rep. 18, 44 (2018).
Nakashima, A., Kato, K., Ohkido, I. & Yokoo, T. Role and treatment of insulin resistance in patients with chronic kidney disease: a review. Nutrients 13, 4349 (2021).
Bailey, J. L. Insulin resistance and muscle metabolism in chronic kidney disease. ISRN Endocrinol. 2013, 329606 (2013).
Shinohara, K. et al. Insulin resistance as an independent predictor of cardiovascular mortality in patients with end-stage renal disease. J. Am. Soc. Nephrol. 13, 1894–1900 (2002).
Schrauben, S. J. et al. Insulin resistance and chronic kidney disease progression, cardiovascular events, and death: findings from the chronic renal insufficiency cohort study. BMC Nephrol. 20, 60 (2019).
Kettner, A. et al. Cardiovascular and metabolic responses to submaximal exercise in haemodialysis patients. Kidney Int. 26, 66–71 (1984).
Castellino, P., Bia, M. & DeFronzo, R. A. Metabolic response to exercise in dialysis patients. Kidney Int. 32, 877–883 (1987).
Bowlby, W. et al. Physical activity and metabolic health in chronic kidney disease: a cross-sectional study. BMC Nephrol. 17, 187 (2016).
Goldberg, A. P. et al. Exercise training reduces coronary risk and effectively rehabilitates haemodialysis patients. Nephron 42, 311–316 (1986).
Barcellos, F. C., Santos, I. S., Umpierre, D., Bohlke, M. & Hallal, P. C. Effects of exercise in the whole spectrum of chronic kidney disease: a systematic review. Clin. Kidney J. 8, 753–765 (2015).
Pei, G. et al. Aerobic exercise in adults with chronic kidney disease (CKD): a meta-analysis. Int. Urol. Nephrol. 51, 1787–1795 (2019).
Yamamoto, R. et al. Efficacy of aerobic exercise on the cardiometabolic and renal outcomes in patients with chronic kidney disease: a systematic review of randomised controlled trials. J. Nephrol. 34, 155–164 (2021).
Toyama, K., Sugiyama, S., Oka, H., Sumida, H. & Ogawa, H. Exercise therapy correlates with improving renal function through modifying lipid metabolism in patients with cardiovascular disease and chronic kidney disease. J. Cardiol. 56, 142–146 (2010).
Miele, E. M. et al. High-density lipoprotein particle pattern and overall lipid responses to short-term moderate-intensity aerobic exercise training intervention in patients with chronic kidney disease. Clin. Kidney J. 10, 524–531 (2017).
Zhou, Y. et al. Twelve months of exercise training did not halt abdominal aortic calcification in patients with CKD — a sub-study of RENEXC-a randomised controlled trial. BMC Nephrol. 21, 233 (2020).
Navaneethan, S. D. et al. A trial of lifestyle modification on cardiopulmonary, inflammatory, and metabolic effects among obese with chronic kidney disease. Am. J. Nephrol. 42, 274–281 (2015).
Rosa, T. S. et al. Effects of dynamic and isometric resistance training protocols on metabolic profile in hemodialysis patients: a randomised controlled trial. Appl. Physiol. Nutr. Metab. 46, 1029–1037 (2021).
Molsted, S. et al. Improved glucose tolerance after high-load strength training in patients undergoing dialysis. Nephron. Clin. Pract. 123, 134–141 (2013).
Chen, G., Gao, L. & Li, X. Effects of exercise training on cardiovascular risk factors in kidney transplant recipients: a systematic review and meta-analysis. Ren. Fail. 41, 408–418 (2019).
De Smet, S. & Van Craenenbroeck, A. H. Exercise training in patients after kidney transplantation. Clin. Kidney J. 14, ii15–ii24 (2021).
Michou, V., Nikodimopoulou, M., Deligiannis, A. & Kouidi, E. Metabolic and functional effects of exercise training in diabetic kidney transplant recipients. World J. Transplant. 12, 184–194 (2022).
Coletta, D. K. et al. Changes in pre- and post-exercise gene expression among patients with chronic kidney disease and kidney transplant recipients. PLoS One 11, e0160327 (2016).
Karelis, A. D., Hérbert, M. J., Rabasa-Lhoret, R. & Räkel, A. Impact of resistance training on factors involved in the development of new-onset diabetes after transplantation in renal transplant recipients: an open randomised pilot study. Can. J. Diabetes 40, 382–388 (2016).
Ponticelli, C., Favi, E. & Ferraresso, M. New-onset diabetes after kidney transplantation. Medicina 57, 250 (2021).
Wang, X. H. & Mitch, W. E. Mechanisms of muscle wasting in chronic kidney disease. Nat. Rev. Nephrol. 10, 504–516 (2014).
John, S. G., Sigrist, M. K., Taal, M. W. & McIntyre, C. W. Natural history of skeletal muscle mass changes in chronic kidney disease stage 4 and 5 patients: an observational study. PLoS One 8, e65372 (2013).
Kouidi, E. et al. The effects of exercise training on muscle atrophy in haemodialysis patients. Nephrol. Dial. Transplant. 13, 685–699 (1998).
Molsted, S., Andersen, J. L., Harrison, A. P., Eidemak, I. & Mackey, A. L. Fiber type-specific response of skeletal muscle satellite cells to high-intensity resistance training in dialysis patients. Muscle Nerve 52, 736–745 (2015).
Watson, E. L. et al. Inflammation and physical dysfunction: responses to moderate intensity exercise in chronic kidney disease. Nephrol. Dial. Transpl. 37, 860–868 (2022).
Macdonald, J. H. et al. Muscle insulin-like growth factor status, body composition, and functional capacity in hemodialysis patients. J. Ren. Nutr. 14, 248–252 (2004).
Diesel, W. et al. Morphologic features of the myopathy associated with chronic renal failure. Am. J. Kidney Dis. 22, 677–684 (1993).
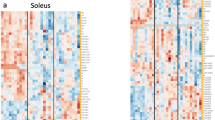
Watson, E. L. et al. Reductions in skeletal muscle mitochondrial mass are not restored following exercise training in patients with chronic kidney disease. FASEB J. 34, 1755–1767 (2020).
Ertuglu, L., Yildiz, A., Gamboa, J. & Ikizler, T. A. Skeletal muscle energetics in patients with moderate to advanced kidney disease. Kidney Res. Clin. Pract. 41, 14–21 (2022).
Wackerhage, H., Schoenfeld, B. J., Hamilton, D. L., Lehti, M. & Hulmi, J. J. Stimuli and sensors that initiate skeletal muscle hypertrophy following resistance exercise. J. Appl. Physiol. 126, 30–43 (2019).
Watson, E. L. et al. Progressive resistance exercise training in CKD: a feasibility study. Am. J. Kidney Dis. 66, 249–257 (2015).
Watson, E. L. et al. The effect of resistance exercise on inflammatory and myogenic markers in patients with Chronic Kidney Disease. Front. Physiol. 8, 541 (2017).
Mayhew, D. L., Kim, J. S., Cross, J. M., Ferrando, A. A. & Bamman, M. M. Translational signaling responses preceding resistance training-mediated myofiber hypertrophy in young and old humans. J. Appl. Physiol. 107, 1655–1662 (2009).
Kopple, J. D. et al. Exercise in maintenance hemodialysis patients induces transcriptional changes in genes favoring anabolic muscle. J. Am. Soc. Nephrol. 18, 2975–2986 (2007).
Kopple, J. D. et al. Effect of exercise on mRNA levels for growth factors in skeletal muscle of hemodialysis patients. J. Ren. Nutr. 16, 312–324 (2006).
Watson, E. L. et al. Combined walking exercise and alkali therapy in patients with CKD4-5 regulates intramuscular free amino acid pools and ubiquitin E3 ligase expression. Eur. J. Appl. Physiol. 113, 2111–2124 (2013).
Kosmadakis, G. C. et al. Benefits of regular walking exercise in advanced pre-dialysis chronic kidney disease. Nephrol. Dial. Transplant. 27, 997–1004 (2012).
Balakrishnan, V. S. et al. Resistance training increases muscle mitochondrial biogenesis in patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 5, 996–1002 (2010).
Beetham, K. S. et al. High-intensity interval training in chronic kidney disease: a randomized pilot study. Scand. J. Med. Sci. Sports 29, 1197–1204 (2019).
Gamboa, J. L. et al. Skeletal muscle mitochondrial dysfunction is present in patients with CKD before initiation of maintenance hemodialysis. Clin. J. Am. Soc. Nephrol. 15, 926–936 (2020).
Kemp, G. J. et al. Abnormal mitochondrial function and muscle wasting, but normal contractile efficiency, in haemodialysed patients studied non-invasively in vivo. Nephrol. Dial. Transplant. 19, 1520–1527 (2004).
de Sousa, C. V. et al. The antioxidant effect of exercise: a systematic review and meta-analysis. Sports Med. 47, 277–293 (2017).
Fisher-Wellman, K. & Bloomer, R. J. Acute exercise and oxidative stress: a 30 year history. Dyn. Med. 8, 1 (2009).
O’Sullivan, T. F., Smith, A. C. & Watson, E. L. Satellite cell function, intramuscular inflammation and exercise in chronic kidney disease. Clin. Kidney J. 11, 810–821 (2018).
Nishimune, H., Stanford, J. A. & Mori, Y. Role of exercise in maintaining the integrity of the neuromuscular junction. Muscle Nerve 49, 315–324 (2014).
Rudolf, R., Khan, M. M., Labeit, S. & Deschenes, M. R. Degeneration of neuromuscular junction in age and dystrophy. Front. Aging Neurosci. 6, 99 (2014).
Cannata-Andía, J. B. et al. Chronic kidney disease — mineral and bone disorders: pathogenesis and management. Calcif. Tissue Int. 108, 410–422 (2021).
Moe, S. et al. Definition, evaluation, and classification of renal osteodystrophy: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int. 69, 1945–1953 (2006).
Moe, S. M. & Nickolas, T. L. Fractures in patients with CKD: time for action. Clin. J. Am. Soc. Nephrol. 11, 1929–1931 (2016).
Covic, A. et al. Systematic review of the evidence underlying the association between mineral metabolism disturbances and risk of all-cause mortality, cardiovascular mortality and cardiovascular events in chronic kidney disease. Nephrol. Dial. Transpl. 24, 1506–1523 (2009).
Maïmoun, L. & Sultan, C. Effects of physical activity on bone remodeling. Metabolism 60, 373–388 (2011).
Howe, T. E. et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD000333 (2011).
Beck, B. R., Daly, R. M., Singh, M. A. F. & Taaffe, D. R. Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. J. Sci. Med. Sport 20, 438–445 (2017).
Cardoso, D. F. et al. Impact of physical activity and exercise on bone health in patients with chronic kidney disease: a systematic review of observational and experimental studies. BMC Nephrol. 21, 334 (2020).
Avin, K. G. et al. Voluntary wheel running has beneficial effects in a rat model of CKD-mineral bone disorder (CKD-MBD). J. Am. Soc. Nephrol. 30, 1898–1909 (2019).
Qin, L., Liu, W., Cao, H. & Xiao, G. Molecular mechanosensors in osteocytes. Bone Res. 8, 23 (2020).
Choi, R. B. & Robling, A. G. The Wnt pathway: an important control mechanism in bone’s response to mechanical loading. Bone 153, 116087 (2021).
Schiavi, S. C. Sclerostin and CKD-MBD. Curr. Osteoporos. Rep. 13, 159–165 (2015).
Neves, R. V. P. et al. Dynamic not isometric training blunts osteo-renal disease and improves the sclerostin/FGF23/Klotho axis in maintenance hemodialysis patients: a randomized clinical trial. J. Appl. Physiol. 130, 508–516 (2021).
Marinho, S. M. et al. In hemodialysis patients, intradialytic resistance exercise improves osteoblast function: a pilot study. J. Ren. Nutr. 26, 341–345 (2016).
Gomes, T. S. et al. Effect of aerobic exercise on markers of bone metabolism of overweight and obese patients with chronic kidney disease. J. Ren. Nutr. 27, 364–371 (2017).
Yasuda, H. Discovery of the RANKL/RANK/OPG system. J. Bone Miner. Metab. 39, 2–11 (2021).
Carrillo-López, N. et al. Role of the RANK/RANKL/OPG and Wnt/β-Catenin systems in CKD bone and cardiovascular disorders. Calcif. Tissue Int. 108, 439–451 (2021).
Tobeiha, M., Moghadasian, M. H., Amin, N. & Jafarnejad, S. RANKL/RANK/OPG pathway: a mechanism involved in exercise-induced bone remodeling. Biomed. Res. Int. 2020, 6910312 (2020).
Marinho, S. M., Eduardo, J. C. C. & Mafra, D. Effect of a resistance exercise training program on bone markers in hemodialysis patients. Sci. Sport. 32, 99–105 (2017).
Muñoz-Castañeda, J. R. et al. Klotho/FGF23 and Wnt signaling as important players in the comorbidities associated with chronic kidney disease. Toxins 12, 185 (2020).
Barker, S. L. et al. The demonstration of αKlotho deficiency in human chronic kidney disease with a novel synthetic antibody. Nephrol. Dial. Transpl. 30, 223–233 (2015).
Isakova, T. et al. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 79, 1370–1378 (2011).
Corrêa, H. L. et al. Blood flow restriction training blunts chronic kidney disease progression in humans. Med. Sci. Sports Exerc. 53, 249–257 (2020).
Leal, D. V., Ferreira, A., Watson, E. L., Wilund, K. R. & Viana, J. L. Muscle-bone crosstalk in chronic kidney disease: the potential modulatory effects of exercise. Calcif. Tissue Int. 108, 461–475 (2021).
Kirk, B., Feehan, J., Lombardi, G. & Duque, G. Muscle, bone, and fat crosstalk: the biological role of myokines, osteokines, and adipokines. Curr. Osteoporos. Rep. 18, 388–400 (2020).
Chowdhury, S. et al. Muscle derived interleukin-6 increases exercise capacity by signaling in osteoblasts. J. Clin. Invest. 130, 2888–2902 (2020).
Mera, P. et al. Osteocalcin signaling in myofibers is necessary and sufficient for optimum adaptation to exercise. Cell. Metab. 23, 1078–1092 (2016).
Acknowledgements
The authors’ work is supported by the National Institute for Health Research (NIHR) Leicester Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. J.L.V’s work is supported by the Portuguese Foundation of Science and Technology (UID/04045/2020) and the Portuguese Society of Nephrology.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, wrote the article and reviewed and/or edited the manuscript before submission. N.C.B. contributed substantially to discussion of the content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Naomi Clyne, Kamyar Kalantar-Zadeh and the other, anonymous, reviewer for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Accelerometery
-
An objective measurement of movement (acceleration) that is used to quantify the volume and intensity of physical activity.
- Blood flow restriction training
-
A technique that combines low-intensity exercise with blood flow occlusion through the application of a cuff or band with the aim of producing comparable effects with high-intensity exercise.
- Dynamic resistance exercise
-
Effort against a constant force that involves movement of a joint through the range of motion, for example, lifting weights or press ups.
- Isometric resistance exercise
-
Static contractions of a specific muscle or group of muscles with no resultant change in muscle length or joint movement.
- Mechanotransduction
-
The conversion of mechanical loading into biochemical signalling.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bishop, N.C., Burton, J.O., Graham-Brown, M.P.M. et al. Exercise and chronic kidney disease: potential mechanisms underlying the physiological benefits. Nat Rev Nephrol 19, 244–256 (2023). https://doi.org/10.1038/s41581-022-00675-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-022-00675-9
This article is cited by
-
Impact of resistance exercise on patients with chronic kidney disease
BMC Nephrology (2024)