Abstract
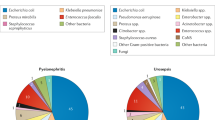
For over a century, acute ‘post-streptococcal glomerulonephritis’ (APSGN) was the prototypical form of bacterial infection-associated glomerulonephritis, typically occurring after resolution of infection and a distinct infection-free latent period. Other less common forms of infection-associated glomerulonephritides resulted from persistent bacteraemia in association with subacute bacterial endocarditis and shunt nephritis. However, a major paradigm shift in the epidemiology and bacteriology of infection-associated glomerulonephritides has occurred over the past few decades. The incidence of APSGN has sharply declined in the Western world, whereas the number of Staphylococcus infection-associated glomerulonephritis (SAGN) cases increased owing to a surge in drug-resistant Staphylococcus aureus infections, both in the hospital and community settings. These Staphylococcus infections range from superficial skin infections to deep-seated invasive infections such as endocarditis, which is on the rise among young adults owing to the ongoing intravenous drug use epidemic. SAGN is markedly different from APSGN in terms of its demographic profile, temporal association with active infection and disease outcomes. The diagnosis and management of SAGN is challenging because of the lack of unique histological features, the frequently occult nature of the underlying infection and the older age and co-morbidities in the affected patients. The emergence of multi-drug-resistant bacterial strains further complicates patient treatment.
Key points
In the last century, acute post-streptococcal glomerulonephritis (APSGN) was the prototypical infection-associated GN.
Over the past few decades, the incidence of APSGN declined sharply in the Western world, whereas the number of Staphylococcus infection-associated glomerulonephritis (SAGN) cases increased. The surge in staphylococcal infections, mainly methicillin-resistant Staphylococcus aureus (MRSA), is a probable contributing factor.
APSGN still occurs with high frequency among highly populated and economically disadvantaged communities around the world, where group A β-haemolytic streptococcal infections are common.
APSGN remains the most common cause of acute GN among children, whereas SAGN has very different demographic features and mainly affects the elderly population.
SAGN is associated with ongoing infection when the patient presents with acute GN and antibiotic treatment is the mainstay of management; aggressive immunosuppressive treatment is clearly contraindicated and detrimental to the patient when the infection is still active.
Infective endocarditis is one of the most frequent infections implicated in SAGN; epidemic intravenous drug use is a major contributing factor, as well as the increased use of cardiac devices in elderly patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Jennette, J. C., Silva, F. G., Olson, J. L., D’Agati, V. D. (eds) Heptinstall’s Pathology of the Kidney 7th edn Vol. 1 Ch. 3 91–118 (Wolters Kluwer, 2014).
Cook, H. T. & Pickering, M. C. in Heptinstall’s Pathology of the Kidney 7th edn Vol. 1 Ch. 9 (eds Jennette, J. C. et al.) 341–366 (Wolters Kluwer, 2014).
Satoskar, A. A. & Nadasdy, T. in Silva’s Diagnostic Renal Pathology 2nd edn Ch. 7 (eds Zhou, X. J. et al.) 243–264 (Cambridge Univ. Press, 2017).
Satoskar, A. A., Nadasdy, T. & Silva, F. in Heptinstall’s Pathology of the Kidney 7th edn Vol. 1 Ch. 10 (eds Jennette, J. C. et al.) (Wolters Kluwer, 2014).
Boils, C. L. in Bacterial Infections and the Kidney Ch. 4 (eds Satoskar, A. A. & Nadasdy, T.) 87–116 (Springer, 2017).
Longcope, W. T. et al. Relationship of acute infections to glomerular nephritis. J. Clin. Invest. 5, 7 (1928).
Dillon, H. C., Reeves, M. S. & Maxted, W. R. Acute glomerulonephritis following skin infection due to streptococci of M-type 2. Lancet 291, 543–545 (1968).
Wilmers, M. J., Cunliffe, A. C. & Williams, R. E. Type-12 streptococci associated with acute haemorrhagic nephritis. Lancet 267, 17–18 (1954).
World Health Organization. The current evidence for the burden of group A streptococcal diseases (WHO, 2005).
Carapetis, J. R., Steer, A. C., Mulholland, E. K. & Weber, M. The global burden of group A streptococcal diseases. Lancet Infect. Dis. 5, 685–694 (2005).
Rodriguez-Iturbe, B. & Musser, J. M. The current state of post-streptococcal glomerulonephritis. J. Am. Soc. Nephrol. 19, 1855–1864 (2008).
Kanjanabuch, T., Kittikowit, W. & Eiam-Ong, S. An update on acute postinfectious glomerulonephritis worldwide. Nat. Rev. Nephrol. 5, 259–269 (2009).
World Health Organization. A review of the technical basis for the control of conditions associated with GAS infections (WHO, 2005).
DeLeo, F. R., Otto, M., Kreiswirth, B. N. & Chambers, H. F. Community-associated methicillin-resistant Staphylococcus aureus. Lancet 375, 1557–1568 (2010).
Tattevin, P., Diep, B. A., Jula, M. & Perdreau-Remington, F. Long-term follow-up of methicillin-resistant Staphylococcus aureus molecular epidemiology after emergence of clone USA300 in San Francisco jail populations. J. Clin. Microbiol. 46, 4056–4057 (2008).
Tattevin, P., Diep, B. A., Jula, M. & Perdreau-Remington, F. Methicillin-resistant Staphylococcus aureus USA300 clone in long-term care facility. Emerg. Infect. Dis. 15, 953–955 (2009).
Nimmo, G. R. USA300 abroad: global spread of a virulent strain of community-associated methicillin-resistant Staphylococcus aureus. Clin. Microbiol. Infect. 18, 725–734 (2012).
Pan, E. S. et al. Increasing prevalence of methicillin-resistant Staphylococcus aureus infection in California jails. Clin. Infect. Dis. 37, 1384–1388 (2003).
King, M. D. et al. Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann. Intern. Med. 144, 309–317 (2006).
Chatterjee, S. S. & Otto, M. Improved understanding of factors driving methicillin-resistant Staphylococcus aureus epidemic waves. Clin. Epidemiol. 5, 205–217 (2013).
Nasr, S. et al. IgA dominant acute poststaphylococcal glomerulonephritis complicating diabetic nephropathy. Hum. Pathol. 34, 1235 (2003).
Pola, E. et al. Onset of Berger disease after Staphylococcus aureus infection: septic arthritis after anterior cruciate ligament reconstruction. Arthroscopy 19, E29 (2003).
Satoskar, A. A. et al. Staphylococcus infection-associated glomerulonephritis mimicking IgA nephropathy. Clin. J. Am. Soc. Nephrol. 1, 1179–1186 (2006).
Haas, M., Racusen, L. C. & Bagnasco, S. M. IgA-dominant postinfectious glomerulonephritis: a report of 13 cases with common ultrastructural features. Hum. Pathol. 39, 1309–1316 (2008).
Worawichawong, S. et al. Immunoglobulin A-dominant postinfectious glomerulonephritis: frequent occurrence in nondiabetic patients with Staphylococcus aureus infection. Hum. Pathol. 42, 279–284 (2011).
Satoskar, A. A. et al. Staphylococcus infection-associated GN — spectrum of IgA staining and prevalence of ANCA in a single-center cohort. Clin. J. Am. Soc. Nephrol. 12, 39–49 (2017).
Jackson, K. A. et al. Invasive methicillin-resistant staphylococcus aureus infections among persons who inject drugs — six sites, 2005–2016. MMWR Morb. Mortal. Wkly Rep. 67, 625–628 (2018).
Vosti, K. L., Johnson, R. H. & Dillon, M. F. Further characterization of purified fractions of M protein from a strain of group A, type 12 streptococcus. J. Immunol. 107, 104–114 (1971).
Nordstrand, A., McShan, W. M., Ferretti, J. J., Holm, S. E. & Norgren, M. Allele substitution of the streptokinase gene reduces the nephritogenic capacity of group A streptococcal strain NZ131. Infect. Immun. 68, 1019–1025 (2000).
Ohkuni, H. et al. Immunological studies of post-streptococcal sequelae: serological studies with an extracellular protein associated with nephritogenic streptococci. Clin. Exp. Immunol. 54, 185–193 (1983).
Anthony, B. F., Kaplan, E. L., Wannamaker, L. W., Briese, F. W. & Chapman, S. S. Attack rates of acute nephritis after type 49 streptococcal infection of the skin and of the respiratory tract. J. Clin. Invest. 48, 1697–1704 (1969).
Rodriguez-Iturbe, B., Castillo, L., Valbuena, R. & Cuenca, L. Attack rate of poststreptococcal nephritis in families: a prospective study. Lancet 317, 401–403 (1981).
Poon-King, T. et al. Recurrent epidemic nephritis in South Trinidad. N. Engl. J. Med. 277, 728 (1967).
Fish, A. J., Herdman, R. C., Michael, A. F., Pickering, R. J. & Good, R. A. Epidemic acute glomerulonephritis associated with type 49 streptococcal pyoderma. II. Correlative study of light, immunofluorescent and electron microscopic findings. Am. J. Med. 48, 28–39 (1970).
Rodriguez-Iturbe, B. Epidemic post-streptococcal glomerulonephritis. Kidney Int. 25, 129–136 (1984).
Rodriguez-Iturbe, B. et al. Epidemic glomerulonephritis in Maracaibo: evidence for progression to chronicity. Clin. Nephrol. 5, 197 (1976).
Drachman, R., Aladjem, M. & Vardy, P. A. Natural-history of an acute glomerulonephritis epidemic in children — an 11-year to 12-year follow-up. Isr. J. Med. Sci. 18, 603–607 (1982).
Mori, K., Ito, Y., Kamikawaji, N. & Sasazuki, T. Elevated IgG titer against the C region of streptococcal M protein and its immunodeterminants in patients with poststreptococcal acute glomerulonephritis. J. Pediatr. 131, 293–299 (1997).
Perlman, L. V., Herdman, R. C., Kleinman, H. & Vernier, R. L. Poststreptococcal glomerulonephritis. A ten-year follow-up of an epidemic. JAMA 194, 63–70 (1965).
VanDeVoorde, R. G. 3rd Acute poststreptococcal glomerulonephritis: the most common acute glomerulonephritis. Pediatr. Rev. 36, 3–12 (2015).
Vogel, A. M. et al. Post-streptococcal glomerulonephritis: some reduction in a disease of disparities. J. Paediatr. Child Health 55, 652–658 (2019).
Ramanathan, G. et al. Analysis of clinical presentation, pathological spectra, treatment and outcomes of biopsy-proven acute postinfectious glomerulonephritis in adult indigenous people of the Northern Territory of Australia. Nephrology 22, 403–411 (2017).
Coppo, R., Gianoglio, B., Porcellini, M. G. & Maringhini, S. Frequency of renal diseases and clinical indications for renal biopsy in children (report of the Italian National Registry of Renal Biopsies in Children). Group of Renal Immunopathology of the Italian Society of Pediatric Nephrology and Group of Renal Immunopathology of the Italian Society of Nephrology. Nephrol. Dial. Transplant. 13, 293–297 (1998).
Shulman, S. T. et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 55, 1279–1282 (2012).
Bisno, A. L. et al. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Clin. Infect. Dis. 35, 113–125 (2002).
Parks, T., Smeesters, P. R., Curtis, N. & Steer, A. C. ASO titer or not? When to use streptococcal serology: a guide for clinicians. Eur. J. Clin. Microbiol. Infect. Dis. 34, 845–849 (2015).
Nasr, S. H. et al. Postinfectious glomerulonephritis in the elderly. J. Am. Soc. Nephrol. 22, 187–195 (2011).
Mazzucco, G. et al. Different patterns of renal damage in type 2 diabetes mellitus: a multicentric study on 393 biopsies. Am. J. Kidney Dis. 39, 713–720 (2002).
Lien, J. W., Mathew, T. H. & Meadows, R. Acute post-streptococcal glomerulonephritis in adults: a long-term study. Q. J. Med. 48, 99–111 (1979).
Gunasekaran, K., Krishnamurthy, S., Mahadevan, S., Harish, B. N. & Kumar, A. P. Clinical characteristics and outcome of post-infectious glomerulonephritis in children in Southern India: a prospective study. Indian J. Pediatr. 82, 896–903 (2015).
Rodriguez-Iturbe, B. et al. Characterization of the glomerular antibody in acute poststreptococcal glomerulonephritis. Ann. Intern. Med. 92, 478 (1980).
Parikh, S. V., Haddad, N. & Hebert, L. A. in Comprehensive Clinical Nephrology 5th edn Ch. 80 (eds Johnson, R., Feehally, J. & Floege, J.) (Saunders, 2014).
Pavelsky, P. M. Renal replacement therapy in AKI. Adv. Chronic Kidney Dis. 20, 76–84 (2013).
Roy, S. 3rd, Murphy, W. M. & Arant, B. S. Jr Poststreptococcal crescenteric glomerulonephritis in children: comparison of quintuple therapy versus supportive care. J. Pediatr. 98, 403–410 (1981).
Melby, P. C. et al. Poststreptococcal glomerulonephritis in the elderly. Report of a case and review of the literature. Am. J. Nephrol. 7, 235–240 (1987).
Wong, W., Morris, M. C. & Zwi, J. Outcome of severe acute post-streptococcal glomerulonephritis in New Zealand children. Pediatr. Nephrol. 24, 1021–1026 (2009).
Zent, R. et al. Crescentic nephritis at Groote Schuur Hospital, South Africa—not a benign disease. Clin. Nephrol. 42, 22–29 (1994).
Clark, G. et al. Poststreptococcal glomerulonephritis in children: clinicopathological correlations and long-term prognosis. Pediatr. Nephrol. 2, 381–388 (1998).
Potter, E. V. et al. Twelve to seventeen-year follow-up of patients with poststreptococcal acute glomerulonephritis in Trinidad. N. Engl. J. Med. 307, 725–729 (1982).
Baldwin, D. S. Poststreptococcal glomerulonephritis. A progressive disease? Am. J. Med. 62, 1–11 (1977).
Buzio, C. et al. Significance of albuminuria in the follow-up of acute poststreptococcal glomerulonephritis. Clin. Nephrol. 41, 259–264 (1994).
Vogl, W. et al. Long-term prognosis for endocapillary glomerulonephritis of poststreptococcal type in children and adults. Nephron 44, 58–65 (1986).
Spector, D. A., Millan, J., Zauber, N. & Burton, J. Glomerulonephritis and Staphylococcus aureus infections. Clin. Nephrol. 14, 256 (1980).
Danovitch, G. M., Nord, E. P., Barki, Y. & Krugliak, L. Staphylococcal lung abscess and acute glomerulonephritis. Isr. J. Med. Sci. 15, 840–843 (1979).
Sato, M., Nakazoro, H. & Ofuji, T. The pathogenetic role of Staphylococcus aureus in primary human glomerulonephritis. Clin. Nephrol. 11, 190–195 (1979).
Maher, E. R., Hamilton, D. V., Thiru, S. & Wheatley, T. Acute renal failure due to glomerulonephritis associated with staphylococcal infection. Postgrad. Med. J. 60, 433–434 (1984).
Salyer, W. R. & Salyer, D. C. Unilateral glomerulonephritis. J. Pathol. 113, 247–251 (1974).
Koyama, A. et al. Glomerulonephritis associated with MRSA infection: a possible role of bacterial superantigen. Kidney Int. 47, 207–216 (1995).
Yoh, K. et al. A case of superantigen-related glomerulonephritis after methicillin-resistant Staphylococcus aureus (MRSA) infection. Clin. Nephrol. 48, 311–316 (1997).
Kobayashi, M. & Koyama, A. Methicillin-resistant Staphylococcus aureus (MRSA) infection in glomerulonephritis—a novel hazard emerging on the horizon. Nephrol. Dial Transplant. 13, 2999–3001 (1998).
Hirayama, K. et al. Henoch-Schonlein purpura nephritis associated with methicillin-resistant Staphylococcus aureus infection. Nephrol. Dial Transplant. 13, 2703–2704 (1998).
Yoh, K. et al. Cytokines and T cell responses in superantigen-related glomerulonephritis following methicillin-resistant Staphylococcus aureus infection. Nephrol. Dial Transplant. 15, 1170–1174 (2000).
Yamashita, Y. et al. Glomerulonephritis after methicillin-resistant Staphylococcus aureus infection resulting in end-stage renal failure. Intern. Med. 40, 424–427 (2001).
Satoskar, A. A. et al. Henoch-Schönlein purpura-like presentation in IgA-dominant Staphylococcus infection-associated glomerulonephritis-a diagnostic pitfall. Clin. Nephrol. 79, 302–312 (2013).
Montoliu, J. et al. Henoch-Schonlein purpura complicating staphylococcal endocarditis in a heroin addict. Am. J. Nephrol. 7, 137–139 (1987).
Kitamura, T., Nakase, H. & Iizuka, H. Henoch-Schonlein purpura after postoperative Staphylococcus aureus infection with hepatic IgA nephropathy. J. Nephrol. 19, 687–690 (2006).
Hemminger, J. A. & Satoskar, A. A. in Bacterial Infections and the Kidney Ch. 2 (eds Satoskar, A. A. & Nadasdy, T.) 37–61 (Springer, 2017).
Nasr, S. H., Radhakrishnan, J. & D’Agati, V. D. Bacterial infection-related glomerulonephritis in adults. Kidney Int. 83, 792–803 (2013).
Bu, R. et al. Clinicopathologic features of IgA-dominant infection-associated glomerulonephritis: a pooled analysis of 78 cases. Am. J. Nephrol. 41, 98–106 (2015).
Kimata, T., Tsuji, S., Yoshimura, K., Tsukaguchi, H. & Kaneko, K. Methicillin-resistant Staphylococcus aureus-related glomerulonephritis in a child. Pediatr. Nephrol. 27, 2149–2152 (2012).
Peacock, S. J., de Silva, I. & Lowy, F. D. What determines nasal carriage of Staphylococcus aureus? Trends Microbiol. 9, 605–610 (2001).
Von Eiff, C., Becker, K., Machka, K., Stammer, H. & Peters, G. Nasal carriage as a source of Staphylococcus aureus bacteremia. Study group. N. Engl. J. Med. 344, 11–16 (2001).
Wertheim, H. F. et al. Risk and outcome of nosocomial Staphylococcus aureus bacteremia in nasal carriers versus non-carriers. Lancet 364, 703–705 (2004).
Foster, T. J. Colonization and infection of the human host by staphylococci: adhesion, survival and immune evasion. Vet. Dermatol. 20, 456–470 (2009).
Boils, C. L., Nasr, S. H., Walker, P. D., Couser, W. G. & Larsen, C. P. Update on endocarditis-associated glomerulonephritis. Kidney Int. 87, 1241–1249 (2015).
Hemminger, J. et al. Acute glomerulonephritis with large confluent IgA-dominant deposits associated with liver cirrhosis. PLOS ONE 13, e0193274 (2018).
Takada, D. et al. IgA nephropathy featuring massive wire loop-like deposits in two patients with alcoholic cirrhosis. BMC Nephrol. 18, 362 (2017).
Nagaba, Y. et al. Effective antibiotic treatment of methicillin-resistant Staphylococcus aureus-associated glomerulonephritis. Nephron 92, 297–303 (2002).
Riley, A. M., Wall, B. M. & Cooke, C. R. Favorable outcome after aggressive treatment of infection in a diabetic patient with MRSA-related IgA nephropathy. Am. J. Med. Sci. 337, 221–223 (2009).
Kapadia, A. S., Panda, M. & Fogo, A. B. Postinfectious glomerulonephritis: is there a role for steroids? Indian J. Nephrol. 21, 116–119 (2011).
Zeledon, J. I. et al. Glomerulonephritis causing acute renal failure during the course of bacterial infections. Histological varieties, potential pathogenetic pathways and treatment. Int. Urol. Nephrol. 40, 461–470 (2008).
Montseny, J. J. et al. The current spectrum of infectious glomerulonephritis. Experience with 76 patients and review of the literature. Medicine 74, 63–73 (1995).
Wang, S. et al. Clinical, pathological, and prognostic characteristics of glomerulonephritis related to staphylococcal infection. Medicine 95, e3386 (2016).
Ebright, J. R. & Komorowski, R. Gonococcal endocarditis associated with immune complex glomerulonephritis. Am. J. Med. 68, 793–796 (1980).
Bookman, I., Scholey, J. W., Jassal, S. V., Lajoie, G. & Herzenberg, A. M. Necrotizing glomerulonephritis caused by Bartonella henselae endocarditis. Am. J. Kidney Dis. 43, e25–e30 (2004).
Elzouki, A. Y., Akthar, M. & Mirza, K. Brucella endocarditis associated with glomerulonephritis and renal vasculitis. Pediatr. Nephrol. 10, 748–751 (1996).
Bell, E. T. Glomerular lesions associated with endocarditis. Am. J. Pathol. 8, 639–664 (1932).
Cordeiro, A., Costa, H. & Laginha, F. Immunologic phase of subacute bacterial endocarditis. A new concept and general considerations. Am. J. Cardiol. 16, 477–481 (1965).
Bayer, A. S. & Theofilopoulos, A. N. Immunopathogenetic aspects of infective endocarditis. Chest 97, 204–212 (1990).
Gutman, R. A., Striker, G. E., Gilliland, B. C. & Cutler, R. E. The immune complex glomerulonephritis of bacterial endocarditis. Medicine 51, 1–25 (1972).
Morel-Maroger, L., Sraer, J. D., Herreman, G. & Godeau, P. Kidney in subacute endocarditis. Pathological and immunofluorescence findings. Arch. Pathol. 94, 205–213 (1972).
Agarwal, A. et al. Subacute bacterial endocarditis masquerading as type III essential mixed cryoglobulinemia. J. Am. Soc. Nephrol. 8, 1971–1976 (1997).
Majumdar, A. et al. Renal pathological findings in infective endocarditis. Nephrol. Dial. Transplant. 15, 1782–1787 (2000).
Eknoyan, G., Lister, B. J., Kim, H. S. & Greenberg, S. D. Renal complications of bacterial endocarditis. Am. J. Nephrol. 5, 457–469 (1985).
Fatima, S. et al. Epidemiology of infective endocarditis in rural upstate New York, 2011–2016. J. Clin. Med. Res. 9, 754–758 (2017).
Fleischauer, A. T., Ruhl, L., Rhea, S. & Barnes, E. Hospitalizations for endocarditis and associated health care costs among persons with diagnosed drug dependence — North Carolina, 2010–2015. MMWR Morb. Mortal. Wkly Rep. 66, 569–573 (2017).
Shiffman, M. L. The next wave of hepatitis C virus: the epidemic of intravenous drug use. Liver. Int. 38, (Suppl. 1), 34–39 (2018).
Bassetti, S. & Battegay, M. Staphylococcus aureus infections in injection drug users: risk factors and prevention strategies. Infection 3, 163–169 (2003).
Chirinos, J. A. et al. Endocarditis associated with antineutrophil cytoplasmic antibodies: a case report and review of the literature. Clin. Rheumatol. 26, 590–595 (2007).
Tiliakos, A. M. & Tiliakos, N. A. Dual ANCA positivity in subacute bacterial endocarditis. J. Clin. Rheumatol. 14, 38–40 (2008).
Uh, M., McCormick, I. A. & Kelsall, J. T. Positive cytoplasmic antineutrophil cytoplasmic antigen with PR3 specificity glomerulonephritis in a patient with subacute bacterial endocarditis. J. Rheumatol. 38, 1527–1528 (2011).
Langlois, V. et al. Antineutrophil cytoplasmic antibodies associated with infective endocarditis. Medicine 95, e2564 (2016).
Bor, D. H., Woolhandler, S., Nardin, R., Brusch, J. & Himmelstein, D. U. Infective endocarditis in the U.S., 1998–2009: a nationwide study. PLOS ONE 8, e60033 (2013).
Johnson, J. A., Boyce, T. G., Cetta, F., Steckelberg, J. M. & Johnson, J. N. Infective endocarditis in the pediatric patient: a 60-year single-institution review. Mayo Clinic Proc. 87, 629–635 (2012).
Fournier, P. E. et al. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clin. Infect. Dis. 51, 131–140 (2010).
Hoen, B. et al. Infective endocarditis in patients with negative blood cultures: analysis of 88 cases from a one-year nationwide survey in France. Clin. Infect. Dis. 20, 501–506 (1995).
Yates, M. et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann. Rheum. Dis. 75, 1583–1594 (2016).
Baddour, L. et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications. Circulation 132, 1435–1486 (2015).
Haas, M. in Heptinstall’s Pathology of the Kidney 7th edn Vol. 1 Ch. 12 (eds Jennette, J. C. et al.) 463–524 (Wolters Kluwer, 2014).
Glassock, R. J. et al. Staphylococcus-related glomerulonephritis and poststreptococcal glomerulonephritis: why defining “post” is important in understanding and treating infection-related glomerulonephritis. Am. J. Kidney Dis. 65, 826–832 (2015).
Nadasdy, T. & Hebert, L. A. Infection-related glomerulonephritis: understanding mechanisms. Semin. Nephrol. 31, 369–375 (2011).
Nasr, S. H. & D’Agati, V. D. IgA-dominant postinfectious glomerulonephritis: a new twist on an old disease. Nephron Clin. Pract. 119, c18–c26 (2011).
Nast, C. C. Infection-related glomerulonephritis: changing demographics and outcomes. Adv. Chronic Kidney Dis. 19, 68–75 (2012).
Tadema, H., Heeringa, P. & Kallenberg, C. G. Bacterial infections in Wegener’s granulomatosis: mechanisms potentially involved in autoimmune pathogenesis. Curr. Opin. Rheumatol. 23, 366–371 (2011).
Salmela, A. et al. Chronic nasal Staphylococcus aureus carriage identifies a subset of newly diagnosed granulomatosis with polyangiitis with high relapse rate. Rheumatology 56, 965–972 (2017).
Oliveira, D. B. G. Linked help from bacterial proteins drives autoantibody production in small vessel vasculitis. Med. Hypotheses 112, 24–26 (2018).
Sethi, S. et al. Atypical postinfectious glomerulonephritis is associated with abnormalities in the alternative pathway of complement. Kidney Int. 83, 293–299 (2012).
Smith, R. J. H. et al. C3 glomerulopathy — understanding a rare complement-driven renal disease. Nat. Rev. Nephrol. 15, 129–143 (2019).
Ozlok, A. & Yildiz, A. Hepatitis C virus associated glomerulopathies. World J. Gastroenterol. 20, 7544–7554 (2014).
Sinniah, R. Occurrence of mesangial IgA and IgM deposits in a control necropsy population. J. Clin. Pathol. 36, 276–279 (1983).
Ji, S. et al. The fate of glomerular mesangial igA deposition in the donated kidney after allograft transplantation. Clin. Transplant. 18, 536–540 (2004).
Suzuki, K. et al. Incidence of latent mesangial IgA deposition in renal allograft donors in Japan. Kidney Int. 63, 2286–2294 (2003).
Lange, K., Seligson, G. & Cronin, W. Evidence for the in situ origin of poststreptococcal glomerulonephritis: glomerular localization of endostreptosin and the clinical significance of the subsequent antibody response. Clin. Nephrol. 19, 3–10 (1983).
Vogt, A., Batsford, S., Rodriguez-Iturbe, B. & Garcia, R. Cationic antigens in poststreptococcal glomerulonephritis. Clin. Nephrol. 20, 271–279 (1983).
Yoshizawa, N. et al. Role of streptococcal antigen in the pathogenesis of acute post-streptococcal glomerulonephritis, characterization of the antigen and a proposed mechanism for the disease. J. Immunol. 148, 3110 (1992).
Froude, J., Zabriskie, J. B., Buchen, D., Rzucidlo, E. & Kakani, R. Immunochemical studies of nephritis strain associated protein (Nsap) and streptokinase (Ska). Zentralbl. Bakteriol. 22, S203–S205 (1992).
Kefalides, N. A. et al. Antibodies to basement membrane collagen and to laminin are present in sera from patients with poststreptococcal glomerulonephritis. J. Exp. Med. 163, 588–602 (1986).
Komaru, Y., Ishioka, K., Oda, T., Ohtake, T. & Kobayashi, S. Nephritis-associated plasmin receptor (NAPlr) positive glomerulonephritis caused by Aggregatibacter actinomycetemcomitans bacteremia: a case report. Clin. Nephrol. 90, 155–160 (2018).
Oda, T. et al. The role of nephritis-associated plasmin receptor (NAPlr) in glomerulonephritis associated with streptococcal infection. J. Biomed. Biotechnol. 2012, 417675 (2012).
Batsford, S. R., Mezzano, S., Mihatsch, M., Schiltz, E. & Rodriguez-Iturbe, B. Is the nephritogenic antigen in post-streptococcal glomerulonephritis pyrogenic exotoxin B (SPE B) or GAPDH? Kidney Int. 68, 1120–1129 (2005).
Schick, B. in Scharlach (eds Escherich, T., Shick, B.) 151 (A. Hölder, 1912).
Okamoto, S. & Nagase, S. Pathogenic mechanisms of invasive group A Streptococcus infections by influenza virus-group A Streptococcus superinfection. Microbiol. Immunol. 62, 141–149 (2018).
Pla, E. et al. Onset of Berger’s disease after Staphylococcus aureus infection: septic arthritis after anterior cruciate ligament reconstruction. Arthroscopy 19, 4 (2003).
Delves, P. J., Martin, S. J., Burton, D. R. & Roitt, I. M. Roitt’s Essential Immunology 11th edn (John Wiley & Sons, 2011).
Safi, R. et al. Neutrophils contribute to vasculitis by increased release of neutrophil extracellular traps in Behçet’s disease. J. Dermatol. Sci. 92, 143–150 (2018).
Skopelja-Gardner, S., Jones, J. D. & Rigby, W. F. C. “NETtling” the host: breaking of tolerance in chronic inflammation and chronic infection. J. Autoimmun. 88, 1–10 (2018).
DeLorenze, G. N. et al. Polymorphisms in HLA class II genes are associated with susceptibility to Staphylococcus aureus infection in a white population. J. Infect. Dis. 213, 816–823 (2016).
Kambham, N. & Troxell, M. in Bacterial Infections and the Kidney Ch. 3 (eds Satoskar, A. A. & Nadasdy, T.) 63–85 (Springer, 2017).
Okada, M. et al. Central venous catheter infection-related glomerulonephritis under long-term parenteral nutrition: a report of two cases. BMC Res. Notes 9, 196 (2016).
Jeffres, M. N., Isakow, W., Doherty, J. A., Micek, S. T. & Kollef, M. H. A retrospective analysis of possible renal toxicity associated with vancomycin in patients with health-care associated methicillin-resistant Staphylococcus aureus pneumonia. Clin. Ther. 29, 1107–1115 (2007).
Hernandez, F. J. et al. Non-invasive imaging of Staphylococcus infections with a nuclease-activated probe. Nat. Med. 20, 301–306 (2014).
Olson, M. E., Slater, S. R., Rupp, M. E. & Fey, P. D. Rifampicin enhances activity of daptomycin and vancomycin against both a polysaccharide intercellular adhesin (PIA)-dependent and -independent Staphylococcus epidermidis biofilm. J. Antimicrob. Chemother. 65, 2164–2171 (2010).
Olson, M. E. et al. Staphylococcus epidermidis agr quorum-sensing system: signal identification, cross talk, and importance in colonization. J. Bacteriol. 196, 3482–3493 (2014).
Author information
Authors and Affiliations
Contributions
A.A.S. researched data for the article, made substantial contributions to discussions of the content and wrote, reviewed and edited the manuscript before submission. S.V.P. researched data for the article and wrote part of the manuscript. T.N. reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Nephrology thanks B. Najafian, T. Oda and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Scabetic lesions
-
Contagious skin condition caused by mites, tiny insect-like parasites that infect the top layer of the skin.
- Pyoderma
-
Bacterial skin infection with formation of skin pustules.
- Acute nephritic syndrome
-
Syndrome characterized by abrupt onset oedema and dark ‘cola-coloured’ or ‘tea-coloured’ urine, with or without renal impairment and sub-nephrotic proteinuria.
- Hypertensive urgency
-
Marked elevation of blood pressure without target organ damage, such as pulmonary oedema, cardiac ischaemia, neurological deficits or acute renal failure.
- Anti-streptolysin O
-
Antibody targeted against the toxic Streptolysin O enzyme produced by Group A Streptococcus bacteria.
- Superantigens
-
Class of antigens that binds directly to HLA molecules without internal processing of the antigenic peptide, resulting in non-specific activation of T lymphocytes and polyclonal T cell activation with massive cytokine release.
- Pauci-immune staining pattern
-
Lack of or very few immune complex deposits.
- Hyaline thrombi
-
Intracapillary proteinaceous globules resembling hyaline material.
- Osler nodes
-
Painful red, raised lesions found on hands and feet, associated with a number of conditions including infective endocarditis, caused by immune complex deposition.
- Janeway lesions
-
Non-tender, small erythematous or haemorrhagic macular or nodular lesions on the palms or soles only a few millimetres in diameter that are indicative of infective endocarditis (in contrast to Osler’s nodes, which are painful).
- Splinter haemorrhages
-
Tiny red blood clots running vertically under the nails. These can be associated with multiple autoimmune conditions including infective endocarditis, scleroderma, systemic lupus erythematosus, rheumatoid arthritis and anti-phospholipid syndrome.
- Valvular vegetations
-
Mass of fibrin, platelets, inflammatory cells and microcolonies of microorganisms collecting on heart valvular surfaces in infective endocarditis. Sterile vegetations may also occur (absence of microorganisms in them) in systemic lupus erythematosus.
- Membranoproliferative GN
-
Glomerular inflammatory disease with hypercellularity in the expanded mesangium as well as in the intracapillary lumina, imparting a nodular–lobular appearance to the glomerulus. This can have many different aetiologies.
- Serum cryoglobulins
-
Immune complexes that precipitate at temperatures below normal body temperature.
- Cytokine storm
-
Secretion of large quantities of activating compounds (cytokines) due to a surge in activated immune cells, usually T lymphocytes.
Rights and permissions
About this article
Cite this article
Satoskar, A.A., Parikh, S.V. & Nadasdy, T. Epidemiology, pathogenesis, treatment and outcomes of infection-associated glomerulonephritis. Nat Rev Nephrol 16, 32–50 (2020). https://doi.org/10.1038/s41581-019-0178-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-019-0178-8
This article is cited by
-
State transitions across the Strep A disease spectrum: scoping review and evidence gaps
BMC Infectious Diseases (2024)
-
Nephropathologie infektiöser Erkrankungen
Die Pathologie (2024)
-
Glomerulonephritis: immunopathogenesis and immunotherapy
Nature Reviews Immunology (2023)
-
Pathogenesis, epidemiology and control of Group A Streptococcus infection
Nature Reviews Microbiology (2023)
-
Clinical profile of children with acute post-streptococcal glomerulonephritis
Pediatric Nephrology (2023)