Abstract
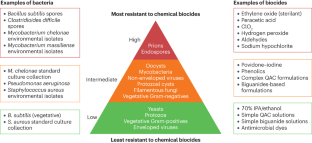
Chemical biocides are used for the prevention and control of infection in health care, targeted home hygiene or controlling microbial contamination for various industrial processes including but not limited to food, water and petroleum. However, their use has substantially increased since the implementation of programmes to control outbreaks of methicillin-resistant Staphylococcus aureus, Clostridioides difficile and severe acute respiratory syndrome coronavirus 2. Biocides interact with multiple targets on the bacterial cells. The number of targets affected and the severity of damage will result in an irreversible bactericidal effect or a reversible bacteriostatic one. Most biocides primarily target the cytoplasmic membrane and enzymes, although the specific bactericidal mechanisms vary among different biocide chemistries. Inappropriate usage or low concentrations of a biocide may act as a stressor while not killing bacterial pathogens, potentially leading to antimicrobial resistance. Biocides can also promote the transfer of antimicrobial resistance genes. In this Review, we explore our current understanding of the mechanisms of action of biocides, the bacterial resistance mechanisms encompassing both intrinsic and acquired resistance and the influence of bacterial biofilms on resistance. We also consider the impact of bacteria that survive biocide exposure in environmental and clinical contexts.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Fraise, A. in Principles and Practice of Disinfection, Preservation and Sterilization 5th edn (eds Fraise, A. P., Maillard, J.-Y. & Sattar, S.) 1–4 (Wiley-Blackwell, 2013).
Pasteur, L. On the extension of the germ theory to the etiology of certain common diseases [French]. Comptes Rendus de l’Académie des Sciences XC, 1033–1044 (1880).
Walker, L., Levine, H. & Jucker, M. Koch’s postulates and infectious proteins. Acta Neuropathol. 112, 1–4 (2006).
Carter, K. C. Ignaz Semmelweis, Carl Mayrhofer, and the rise of germ theory. Med. Hist. 29, 33–53 (1985).
Maillard, J.-Y. et al. Does microbicide use in consumer products promote antimicrobial resistance? A critical review and recommendations for a cohesive approach to risk assessment. Microb. Drug. Res. 19, 344–354 (2013). This opinion paper highlights the issues associated with a lack of definition of ‘biocide resistance’ and with a lack of consensus for measuring bacterial resistance to biocides.
European Commission. Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR). Assessment of the Antibiotic Resistance Effects of Biocides. European Commission http://ec.europa.eu/health/ph_risk/committees/04_scenihr/docs/scenihr_o_021.pdf (2009).
Mueller, S. & Beraud, S. S. L. The Biocides Market in the Times of Coronavirus. S&P Global Commodity Insights https://www.spglobal.com/commodityinsights/en/ci/research-analysis/the-biocides-market-in-the-times-of-coronavirus.html (2020).
Maillard, J.-Y. Resistance of bacteria to biocides. Microbiol. Spectrum 6, ARBA-0006-2017 (2018).
Ko, S., An, H. S., Bang, J. H. & Park, S. W. An outbreak of Burkholderia cepacia complex pseudobacteremia associated with intrinsically contaminated commercial 0.5% chlorhexidine solution. Am. J. Infect. Control 43, 266–268 (2015).
Nakashima, A. K., McCarthy, M. A., Martone, W. J. & Anderson, R. L. Epidemic septic arthritis caused by Serratia marcescens and associated with benzalkonium chloride antiseptic. J. Clin. Microbiol. 25, 1014–1018 (1987).
Hsueh, P.-R. et al. Nosocomial pseudoepidemic caused by Bacillus cereus traced to contaminated ethyl alcohol from a liquor factory. J. Clin. Microbiol. 37, 2280–2284 (1999).
Poole, K. Mechanisms of bacterial biocide and antibiotic resistance. J. Appl. Microbiol. 92, 55S–64S (2002).
Griffiths, P. A., Babb, J. R., Bradley, C. R. & Fraise, A. P. Glutaraldehyde resistant Mycobacterium chelonae from endoscope washer disinfectors. J. Appl. Microbiol. 82, 519–526 (1997).
Martin, D. J. H., Denyer, S. P., McDonnell, G. & Maillard, J.-Y. Resistance and cross-resistance to oxidising agents of bacterial isolates from endoscope washer disinfectors. J. Hosp. Infect. 69, 377–383 (2008). This paper presents evidence of vegetative bacteria isolated from an endoscope washer disinfector (using chlorine dioxide high-level disinfection), resistant to in-use concentration of chlorine dioxide and other reactive biocides.
Martin, D. J. H., Wesgate, R., Denyer, S. P., McDonnell, G. & Maillard, J.-Y. Bacillus subtilis vegetative isolate surviving chlorine dioxide exposure: an elusive mechanism of resistance. J. Appl. Microbiol. 119, 1541–1551 (2015).
Russell, A. D. Biocides — mechanisms of action and microbial resistance. World J. Microbiol. Biotechnol. 8, 58–59 (1992).
McDonnell, G. & Russell, A. D. Antiseptics and disinfectants: activity, action, and resistance. Clin. Microbiol. Rev. 12, 147–179 (1999). This review highlights the limitation of biocide efficacy depending on their chemistry and the propensity for microbial resistance resulting from exposure to a low concentration of a biocide.
Russell, A. D. Biocide use and antibiotic resistance: the relevance of laboratory findings to clinical and environmental situations. Lancet Infect. Dis. 3, 794–803 (2003).
Maillard, J.-Y. Impact of benzalkonium chloride, benzethonium chloride and chloroxylenol on bacterial resistance and cross-resistance to antimicrobials. J. Appl. Microbiol. 133, 3322–3346 (2022).
Wand, M. E. & Sutton, J. M. Efflux-mediated tolerance to cationic biocides, a cause for concern? Microbiology 168, 1263 (2022).
Vijayakumar, R. & Sandle, T. A review on biocide reduced susceptibility due to plasmid-borne antiseptic-resistant genes — special notes ion pharmaceutical environmental isolates. J. Appl. Microbiol. 126, 1011–1022 (2019).
Jones, I. A. & Joshi, L. Biocide use in the antimicrobial era: a review. Molecules 26, 2276 (2021).
Al-Adham, I., Haddadin, R. & Collier, P. in Principles and Practice of Disinfection, Preservation and Sterilization 5th edn (eds Fraise, A. P., Maillard, J.-Y. & Sattar, S.) 5–70 (Wiley-Blackwell, 2013).
Singer, A. C., Shaw, H., Rhodes, V. & Hart, A. Review of antimicrobial resistance in the environment and its relevance to environmental regulators. Front. Microbiol. 7, 1728 (2016).
Leggett, M. J., Setlow, P., Sattar, S. A. & Maillard, J.-Y. Assessing the activity of microbicides against bacterial spores: knowledge and pitfalls. J. Appl. Microbiol. 120, 1174–1180 (2016).
Forbes, S. et al. Formulation of biocides increases antimicrobial potency and mitigates the enrichment of nonsusceptible bacteria in multispecies. Appl. Environ. Microbiol. 83, e3054-16 (2017).
Maillard, J.-Y. Bacterial target sites for biocide action. J. Appl. Microbiol. 92, 16S–27S (2002).
Sani, M.-A. et al. Maculatin 1.1 disrupts Staphylococcus aureus lipid membranes via a pore mechanism. Antimicrob. Agents Chemother. 57, 3593–3600 (2013).
Johnston, M. D., Hanlon, G. W., Denyer, S. P. & Lambert, R. J. W. Membrane damage to bacteria caused by single and combined biocides. J. Appl. Microbiol. 94, 1015–1023 (2003).
Barros, A. C., Melo, L. F. & Pereira, A. A multi-purpose approach to the mechanisms of action of two biocides (benzalkonium chloride and dibromonitrilopropionamide): discussion of Pseudomonas fluorescens’ viability and death. Front. Microbiol. 13, 842414 (2022).
Linley, E., Denyer, S. P., McDonnell, G., Simons, C. & Maillard, J.-Y. Use of hydrogen peroxide as a biocide: new consideration of its mechanisms of biocidal action. J. Antimicrob. Chemother. 67, 1589–1596 (2012).
Setlow, B., Atluri, S., Kitchel, R., Koziol-Dube, K. & Setlow, P. Role of dipicolinic acid in resistance and stability of spores of Bacillus subtilis with or without DNA-protective α/β-type small acid-soluble proteins. J. Bacteriol. 188, 3740–3747 (2006).
Leggett, M. J. et al. Resistance to and killing by the sporicidal microbicide peracetic acid. J. Antimicrob. Chemother. 70, 773–779 (2015).
Alkhalifa, S. et al. Analysis of the destabilization of bacterial membranes by quaternary ammonium compounds: a combined experimental and computational study. ChemBioChem 21, 1510–1516 (2020).
Bore, E. et al. Adapted tolerance to benzalkonium chloride in Escherichia coli K-12 studied by transcriptome and proteome analyses. Microbiology 153, 935–946 (2007).
Roth, M. et al. Transcriptomic analysis of E. coli after exposure to a sublethal concentration of hydrogen peroxide revealed a coordinated up-regulation of the cysteine biosynthesis pathway. Antioxidants 11, 655 (2022).
Denyer, S. P. & Maillard, J.-Y. Cellular impermeability and uptake of biocides and antibiotics in Gram-negative bacteria. J. Appl. Microbiol. 92, 35S–45S (2002).
Denyer, S. P. Mechanisms of action of biocides. Int. Biodeter. 26, 89–100 (1990).
McMurry, L. M., Oethinger, M. & Levy, S. B. Triclosan targets lipid synthesis. Nature 394, 531–532 (1998).
Simões, L. C. et al. Persister cells in a biofilm treated with a biocide. Biofouling 27, 403–411 (2011).
Fernandes, S., Gomes, I. B., Sousa, S. F. & Simões, M. Antimicrobial susceptibility of persister biofilm cells of Bacillus cereus and Pseudomonas fluorescens. Microorganisms 10, 160 (2022).
Maillard, J.-Y. Usage of antimicrobial biocides and products in the healthcare environment: efficacy, policies, management and perceived problems. Ther. Clin. Risk Manag. 1, 340–370 (2005).
Russell, A. D. & McDonnell, G. Concentration: a major factor in studying biocidal action. J. Hosp. Infect. 44, 1–3 (2000).
Lambert, P. A. Cellular impermeability and uptake of biocides and antibiotics in Gram-positive bacteria and mycobacteria. J. Appl. Microbiol. 92, 46S–54S (2002).
Lambert, R. J. W., Hanlon, G. W. & Denyer, S. P. The synergistic effect of EDTA/antimicrobial combinations on Pseudomonas aeruginosa. J. Appl. Microbiol. 96, 244–253 (2004).
Leggett, M. J., McDonnell, G., Denyer, S. P., Setlow, P. & Maillard, J.-Y. Bacterial spore structures and their protective role in biocide resistance. J. Appl. Microbiol. 113, 485–498 (2012).
Maillard, J.-Y. Innate resistance to sporicides and potential failure to decontaminate. J. Hosp. Infect. 77, 204–209 (2011).
Vickery, K. et al. Presence of biofilm containing viable multiresistant organisms despite terminal cleaning on clinical surfaces in an intensive care unit. J. Hosp. Infect. 80, 52–55 (2012).
Hu, H. et al. Intensive care unit environmental surfaces are contaminated by multidrug-resistant bacteria in biofilms: combined results of conventional culture, pyrosequencing, scanning electron microscopy, and confocal laser microscopy. J. Hosp. Infect. 91, 35–44 (2015).
Ledwoch, K. et al. Beware biofilm! Dry biofilms containing bacterial pathogens on multiple healthcare surfaces; a multi-centre study. J. Hosp. Infect. 100, E47–E56 (2018).
Ledwoch, K. et al. Is a reduction in viability enough to determine biofilm susceptibility to a biocide? Infect. Control. Hosp. Epidemiol. 42, 1486–1492 (2021).
Bridier, A., Dubois-Brissonnet, F., Greub, G., Thomas, V. & Briandet, R. Dynamics of the action of biocides in Pseudomonas aeruginosa biofilms. Antimicrob. Agents Chemother. 55, 2648–2654 (2011).
Stewart, P. S. Antimicrobial tolerance in biofilms. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.MB-0010-2014 (2015).
Bas, S., Kramer, M. & Stopar, D. Biofilm surface density determines biocide effectiveness. Front. Microbiol. 8, 2443 (2017).
Araújo, P. A., Mergulhão, F., Melo, L. & Simões, M. The ability of an antimicrobial agent to penetrate a biofilm is not correlated with its killing or removal efficiency. Biofouling 30, 673–683 (2014).
Wood, T. K., Knabel, S. J. & Kwana, B. W. Bacterial persister cell formation and dormancy. Appl. Environ. Microbiol. 79, 7116–7121 (2013).
Podlesek, Z. & Bertok, D. Z. The DNA damage inducible SOS response is a key player in the generation of bacterial persister cells and population wide tolerance. Front. Microbiol. 4, 1785 (2020).
Ciusa, M. L. et al. A novel resistance mechanism to triclosan that suggests horizontal gene transfer and demonstrates a potential selective pressure for reduced biocide susceptibility in clinical strains of Staphylococcus aureus. Int. J. Antimicrob. Agents 40, 210–220 (2012).
Jia, Y., Lu, H. & Zhua, L. Molecular mechanism of antibiotic resistance induced by mono- and twin-chained quaternary ammonium compounds. Sci. Total Environ. 832, 155090 (2022).
Schindler, B. D. & Kaatz, G. W. Multidrug efflux pumps of Gram-positive bacteria. Drug Res. Updates 27, 1–13 (2016).
Poole, K. Outer membranes and efflux: the path to multidrug resistance in Gram-negative bacteria. Curr. Pharm. Biotechnol. 3, 77–98 (2002).
Chitsaz, M. & Brown, M. H. The role played by drug efflux pumps in bacterial multidrug resistance. Essays Biochem. 61, 127–139 (2017).
Rajamohan, G., Srinivasan, V. B. & Gebreyes, W. A. Novel role of Acinetobacter baumannii RND efflux transporters in mediating decreased susceptibility to biocides. J. Antimicrob. Chemother. 65, 228–232 (2010).
LaBreck, P. T. et al. Systematic analysis of efflux pump-mediated antiseptic resistance in Staphylococcus aureus suggests a need for greater antiseptic stewardship. mSphere 5, e00959-19 (2020).
Wand, M. E., Darby, E. M., Blair, J. M. A. & Sutton, J. M. Contribution of the efflux pump AcrAB-TolC to the tolerance of chlorhexidine and other biocides in Klebsiella spp. J. Med. Microbiol. 71, 001496 (2022).
Fernández-Cuenca, F. et al. Reduced susceptibility to biocides in Acinetobacter baumannii: association with resistance to antimicrobials, epidemiological behaviour, biological cost and effect on the expression of genes encoding porins and efflux pumps. J. Antimicrob. Chemother. 70, 3222–3229 (2015).
Kim, M. et al. Widely used benzalkonium chloride disinfectants can promote antibiotic resistance. Appl. Environ. Microbiol. 84, 1201–1218 (2018).
Nordholt, N., Kanaris, O., Schmidt, S. B. I. & Schreiber, F. Persistence against benzalkonium chloride promotes rapid evolution of tolerance during periodic disinfection. Nat. Commun. 12, 6792 (2021).
Amsalu, A. et al. Efflux pump-driven antibiotic and biocide cross-resistance in Pseudomonas aeruginosa isolated from different ecological niches: a case study in the development of multidrug resistance in environmental hotspots. Microorganisms 8, 1647 (2020).
Sánchez, M. B. et al. Predictive studies suggest that the risk for the selection of antibiotic resistance by biocides is likely low in Stenotrophomonas maltophilia. PLoS ONE 10, e0132816 (2015).
Bay, D. C. & Turner, R. J. Diversity and evolution of the small multidrug resistance protein family. BMC Evol. Biol. 9, 140 (2009).
Hansen, L. S., Jensen, L. B., Sørensen, H. I. & Sørensen, S. J. Substrate specificity of the OqxAB multidrug resistance pump in Escherichia coli and selected enteric bacteria. J. Antimicrob. Chemother. 60, 145–147 (2007).
Kaatz, G. W. & Seo, S. M. Effect of substrate exposure and other growth condition manipulations on norA expression. J. Antimicrob. Chemother. 54, 364–369 (2004).
Mima, T., Joshi, S., Gomez-Escalada, M. & Schweizer, H. P. Identification and characterization of TriABC-OpmH, a triclosan efflux pump of Pseudomonas aeruginosa requiring two membrane fusion proteins. J. Bacteriol. 189, 7600–7609 (2007).
Buffet-Bataillon, S., Tattevin, P., Maillard, J.-Y., Bonnaure-Mallet, M. & Jolivet-Gougeon, A. Efflux pump induction by quaternary ammonium compounds and fluoroquinolone resistance in bacteria. Future Microbiol. 11, 81–92 (2016).
Reza, A., Sutton, J. M. & Rahman, K. M. Effectiveness of efflux pump inhibitors as biofilm disruptors and resistance breakers in Gram-negative (ESKAPEE) bacteria. Antibiotics 8, 229 (2019).
Kvist, M., Hancok, V. & Klemm, O. P. Inactivation if efflux pumps abolishes bacterial biofilm formation. Appl. Environ. Microbiol. 74, 7376–7382 (2008).
Soto, S. M. Role of efflux pumps in the antibiotic resistance of bacteria embedded in a biofilm. Virulence 4, 223–229 (2013).
Chevalier, S. et al. Structure function and regulation of Pseudomonas aeruginosa porins. FEMS Microbiol. Rev. 41, 698–772 (2017).
Svetlíková, Z. et al. Role of porins in the susceptibility of Mycobacterium smegmatis and Mycobacterium chelonae to aldehyde-based disinfectants and drugs. Antimicrob. Agents Chemother. 53, 4015–4018 (2009).
Stahl, C. et al. MspA provides the main hydrophilic pathway through the cell wall of Mycobacterium smegmatis. Mol. Microbiol. 40, 451–464 (2001).
Pereira, B. M. P., Wang, X. K. & Tagkopoulos, I. Biocide-induced emergence of antibiotic resistance in Escherichia coli. Front. Microbiol. 12, 640923 (2021).
Silver, S. Bacterial silver resistance: molecular biology and uses and misuse of silver compounds. FEMS Microbiol. Rev. 27, 341–353 (2003).
Casado Muñoz, M. C. et al. Comparative proteomic analysis of a potentially probiotic Lactobacillus pentosus MP-10 for the identification of key proteins involved in antibiotic resistance and biocide tolerance. Int. J. Food Microbiol. 222, 8–15 (2016).
Allen, M. J., White, G. F. & Morby, A. P. The response of Escherichia coli to exposure to the biocide polyhexamethylene biguanide. Microbiology 152, 989–1000 (2006).
Motgatla, R. M., Gouws, P. A. & Brözel, V. S. Mechanisms contributing to hypochlorous acid resistance of a Salmonella isolate from a poultry-processing plant. J. Appl. Microbiol. 92, 566–573 (2002).
Wu, C. H. A review of microbial injury and recovery methods in food. Food Microbiol. 25, 735–744 (2008).
Yildiz, F. H. & Schoolnik, G. K. Vibrio cholerae O1 E1 Tor: identification of a gene cluster required for the rugose colony type, exopolysaccharide production, chlorine resistance and biofilm formation. Proc. Natl Acad. Sci. USA 96, 4028–4033 (1999).
Koska, M. et al. Distinct long- and short-term adaptive mechanisms in Pseudomonas aeruginosa. Microbiol. Spectr. 10, e0304322 (2022).
Keim, K. C., George, I. K., Reynolds, L. & Smith, A. C. The clinical significance of Staphylococcus aureus small colony variants. Lab. Med. 54, 227–234 (2023).
Seaman, P. F., Ochs, D. & Day, M. J. Small-colony variants: a novel mechanism for triclosan resistance in methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 59, 43–450 (2007).
Pitton, M. et al. Mutation to ispA produces stable small-colony variants of Pseudomonas aeruginosa that have enhanced aminoglycoside resistance. Antimicrob. Agents Chemother. 66, e0062122 (2022).
Zhou, S., Rao, Y., Li, J., Huang, Q. & Rao, X. Staphylococcus aureus small-colony variants: formation, infection, and treatment. Microbiol. Res. 260, 127040 (2022).
Fischer, A. J. Small colonies, bigger problems? New evidence that Staphylococcus aureus small colony variants can worsen lung inflammation in cystic fibrosis rats. Infect. Immun. 90, e0041322 (2022).
McNamara, P. J. & Proctor, R. A. Staphylococcus aureus small colony variants, electron transport and persistent infections. Int. J. Antimicrob. Agents 14, 117–122 (2000).
Gilman, S. & Saunders, V. A. Accumulation of gentamicin by Staphylococcus aureus: the role of the transmembrane electrical potential. J. Antimicrob. Chemother. 17, 37–44 (1986).
Guo, H. et al. Biofilm and small colony variants — an update on Staphylococcus aureus strategies toward drug resistance. Int. J. Mol. Sci. 23, 1241 (2022).
Wesgate, R., Fanning, S., Hu, Y. & Maillard, J.-Y. The effect of exposure to microbicide residues at ‘during use’ concentrations on antimicrobial susceptibility profile, efflux, conjugative plasmid transfer and metabolism of Escherichia coli. Antimicrob. Agents Chemother. 64, e01131-20 (2020).
Bischofberger, A. M., Baumgartner, M., Pfrunder-Cardozo, K. R., Allen, R. C. & Hall, A. R. Associations between sensitivity to antibiotics, disinfectants and heavy metals in natural, clinical and laboratory isolates of Escherichia coli. Environ. Microbiol. 22, 2664–2679 (2020).
Webber, M. A., Coldham, N. G., Woodward, M. J. & Piddock, L. J. V. Proteomic analysis of triclosan resistance in Salmonella enterica serovar Typhimurium. J. Antimicrob. Chemother. 62, 92–97 (2008).
Condell, O. et al. Comparative analysis of Salmonella susceptibility and tolerance to the biocide chlorhexidine identifies a complex cellular defense network. Front. Microbiol. 5, 373 (2014). This paper identifies the expression of multiple mechanisms in response to biocide exposure, reporting for the first time, to our knowledge, a complex cellular defence network and emphasizing that bacterial response to biocide stress does rely on a combination of mechanisms.
Curiao, T. et al. Multiple adaptive routes of Salmonella enterica Typhimurium to biocide and antibiotic exposure. BMC Genomics 17, 491 (2016).
Pi, B. R., Yu, D. L., Hua, X. T., Ruan, Z. & Yu, Y. S. Genomic and transcriptome analysis of triclosan response of a multidrug-resistant Acinetobacter baumannii strain, MDR-ZJ06. Arch. Microbiol. 199, 223–230 (2017).
Curiao, T. et al. Polymorphic variation in susceptibility and metabolism of triclosan-resistant mutants of Escherichia coli and Klebsiella pneumoniae clinical strains obtained after exposure to biocides and antibiotics. Antimicrob. Agents Chemother. 59, 3413–3423 (2015).
McMurry, L. M., Oethinger, M. & Levy, S. B. Overexpression of marA, soxS, or acrAB produces resistance to triclosan in laboratory and clinical strains of Escherichia coli. FEMS Microbiol. Lett. 166, 305–309 (1998).
Bailey, A. M. et al. Exposure of Escherichia coli and serovar Typhimurium to triclosan induces a species-specific response, including drug detoxification. J. Antimicrob. Chemother. 64, 973–985 (2009).
Dejoies, L., Le Neindre, K., Reissier, S., Felden, B. & Cattoir, V. Distinct expression profiles of regulatory RNAs in the response to biocides in Staphylococcus aureus and Enterococcus faecium. Sci. Rep. 11, 6892 (2021). This paper documents the impact of biocide exposure at a subinhibitory concentration on the expression of small RNA (sRNA) in Staphylococcus aureus and Enterococcus faecium, demonstrating that sRNA-mediated responses were mostly repressed potentially leading to specific bacterial response and adaptation to biocides.
Demple, B. Redox signaling and gene control in the Escherichia coli soxRS oxidative stress regulon — a review. Gene 179, 53–57 (1996).
Koutsolioutsou, A., Pena-Llopis, S. & Demple, B. Constitutive soxR mutations contribute to multiple-antibiotic resistance in clinical Escherichia coli isolates. Antimicrob. Agents Chemother. 49, 2746–2752 (2005).
Wand, M. E., Bock, L. J., Bonney, L. C. & Sutton, J. M. Mechanisms of increased resistance to chlorhexidine and cross-resistance to colistin following exposure of Klebsiella pneumoniae clinical isolates to chlorhexidine. Antimicrob. Agents Chemother. 61, e01162-16 (2016).
Kastbjerg, V. G., Hein-Kristensen, L. & Gram, L. Triclosan-induced aminoglycoside-tolerant Listeria monocytogenes isolates can appear as small-colony variants. Antimicrob. Agents Chemother. 58, 3124–3132 (2014).
McMurry, L. M., McDermott, P. F. & Levy, S. B. Genetic evidence that InhA of Mycobacterium smegmatis is a target for triclosan. Antimicrob. Agents Chemother. 43, 711–713 (1999).
International Organization for Standardization. ISO: 20776-1. Clinical Laboratory Testing and In Vitro Diagnostic Test Systems: Susceptibility Testing of Infectious Agents and Evaluation of Performance of Antimicrobial Susceptibility Test Devices. Part 1. Reference Method for Testing the In Vitro Activity of Antimicrobial Agents Against Rapidly Growing Aerobic Bacteria Involved in Infectious Diseases (British Standard Institute, 2006).
European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 4.0 (EUCAST, 2014).
Andrews, J. M. BSAC Working Party on Susceptibility Testing. BSAC standardized disc susceptibility testing method (version 8). J. Antimicrob. Chemother. 64, 454–489 (2009).
Bock, L. J., Hind, C. K., Sutton, J. M. & Wand, M. E. Growth media and assay plate material can impact on the effectiveness of cationic biocides and antibiotics against different bacterial species. Lett. Appl. Microbiol. 66, 368–377 (2018).
Kampf, G. Suitability of methods to determine resistance to biocidal active substances and disinfectants — a systematic review. Hygiene 2, 109–119 (2022).
Kahlmeter, G. et al. European harmonization of MIC breakpoints for antimicrobial susceptibility testing of bacteria. J. Antimicrob. Chemother. 52, 145–148 (2003).
Coelho et al. The use of machine learning methodologies to analyse antibiotic and biocide susceptibility in Staphylococcus aureus. PLoS ONE 8, e55582 (2013).
Walsh, S. E. et al. Development of bacterial resistance to several biocides and effects on antibiotic susceptibility. J. Hosp. Infect. 55, 98–107 (2003).
Alonso-Calleja, C., Guerrero-Ramos, E., Alonso-Hernando, A. & Capita, R. Adaptation and cross-adaptation of Escherichia coli ATCC 12806 to several food-grade biocides. Food Control 56, 86–94 (2015).
Cowley, N. L. et al. Effects of formulation on microbicide potency and mitigation of the development of bacterial insusceptibility. Appl. Environ. Microbiol. 81, 7330–7338 (2015).
Wesgate, R., Grasha, P. & Maillard, J.-Y. Use of a predictive protocol to measure the antimicrobial resistance risks associated with biocidal product usage. Am. J. Infect. Control 44, 458–464 (2016).
Randall, L. P. et al. Commonly used farm disinfectants can select for mutant Salmonella enterica serovar Typhimurium with decreased susceptibility to biocides and antibiotics without compromising virulence. J. Antimicrob. Chemother. 60, 1273–1280 (2007).
Weber, D. J., Rutala, W. A. & Sickbert-Bennett, E. E. Outbreaks associated with contaminated antiseptics and disinfectants. Antimicrob. Agents Chemother. 51, 4217–4224 (2007). This review presents evidence of bacterial contamination of biocidal products and highlights the reasons for product failure, including contamination with an intrinsically resistant bacterium or spore, or product misuse.
Maillard, J.-Y. in Blocks’ Disinfection, Sterilization and Preservation 6th edn (eds McDonnell, G. & Hansen, J.) 44–67 (Wolters Kluwer, 2020).
de Frutos, M. et al. Serratia marcescens outbreak due to contaminated 2% aqueous chlorhexidine. Enferm. Infecc. Microbiol. Clin. 35, 624–629 (2016).
Anyiwo, C. E., Coker, A. O. & Daniel, S. O. Pseudomonas aeruginosa in postoperative wounds from chlorhexidine solutions. J. Hosp. Infect. 3, 189–191 (1982).
Wishart, M. M. & Riley, T. V. Infection with Pseudomonas maltophilia hospital outbreak due to contaminated disinfectant. Med. J. Aust. 2, 710–712 (1976).
Georgia Division of Public Health. Abscesses in an allergy practice due to Mycobacterium chelonae. Georgia Epidemiol. Rep. 6, 2 (1960).
Guinness, M. & Levey, J. Contamination of aqueous dilutions of Resiguard disinfectant with Pseudomonas. Med. J. Aust. 2, 392 (1976).
Cason, J. S., Jackson, D. M., Lowbury, E. J. & Ricketts, C. R. Antiseptic and septic prophylaxis for burns: use of silver nitrate and of isolators. Br. Med. J. 2, 1288–1294 (1966).
Duarte, R. S. et al. Epidemic of postsurgical infections caused by Mycobacterium massiliense. J. Clin. Microbiol. 47, 2149–2155 (2009).
Ben Miloud, S., Ali, M. M., Boutiba, I., Van Houdt, R. & Chouchani, C. First report of cross resistance to silver and antibiotics in Klebsiella pneumoniae isolated from patients and polluted water in Tunisia. Water Environ. J. 35, 730–739 (2021).
Molina-González, D., Alonso-Calleja, C., Alonso-Hernando, A. & Capita, R. Effect of sub-lethal concentrations of biocides on the susceptibility to antibiotics of multi-drug resistant Salmonella enterica strains. Food Control 40, 329–334 (2014).
Amos, G. C. A. et al. The widespread dissemination of integrons throughout bacterial communities in a riverine system. ISME J. 12, 681–691 (2018).
Randall, L. P. et al. Fitness and dissemination of disinfectant-selected multiple-antibiotic-resistant (MAR) strains of Salmonella enterica serovar Typhimurium in chickens. J. Antimicrob. Chemother. 61, 156–162 (2008).
Cole, E. C. et al. Investigation of antibiotic and antibacterial agent cross-resistance in target bacteria from homes of antibacterial product users and nonusers. J. Appl. Microbiol. 95, 664–676 (2003).
Carson, R. T., Larson, E., Levy, S. B., Marshall, B. M. & Aiello, A. E. Use of antibacterial consumer products containing quaternary ammonium compounds and drug resistance in the community. J. Antimicrob. Chemother. 62, 1160–1162 (2008).
Short, F. L. et al. Benzalkonium chloride antagonises aminoglycoside antibiotics and promotes evolution of resistance. eBioMedicine 73, 103653 (2021).
Liu, Q. et al. Frequency of biocide-resistant genes and susceptibility to chlorhexidine in high-level mupirocin-resistant, methicillin-resistant Staphylococcus aureus (MuH MRSA). Diagn. Microbiol. Infect. Dis. 82, 278–283 (2015). This paper shows multiple efflux gene carriage in Staphylococcus aureus clinical isolates, where most of the isolates harbour two or more efflux pump gene determinants.
Hijazi, K. et al. Susceptibility to chlorhexidine amongst multidrug-resistant clinical isolates of Staphylococcus epidermidis from bloodstream infections. Int. J. Antimicrob. Agents 48, 86–90 (2016).
Conceição, T., Coelho, C., de Lencastre, H. & Aires-de-Sousa, M. High prevalence of biocide resistance determinants in Staphylococcus aureus isolates from three African countries. Antimicrob. Agents Chemother. 60, 678–681 (2015).
Wand, M. E. et al. Characterization of pre-antibiotic era Klebsiella pneumoniae isolates with respect to antibiotic/disinfectant susceptibility and virulence in Galleria mellonella. Antimicrob. Agents Chemother. 59, 3966–3972 (2015).
Lin, F. et al. Molecular characterization of reduced susceptibility to biocides in clinical isolates of Acinetobacter baumannii. Front. Microbiol. 8, 1836 (2017).
Elkhatib, W. F., KhaIiI, M. A. F. & Ashour, H. M. Integrons and antiseptic resistance genes mediate resistance of Acinetobacter baumannii and Pseudomonas aeruginosa isolates from intensive care unit patients with wound infections. Curr. Mol. Med. 19, 286–293 (2019).
Goodarzi, R., Yousefimashouf, R., Taheri, M., Nouri, F. & Asghari, B. Susceptibility to biocides and the prevalence of biocides resistance genes in clinical multidrug-resistant Pseudomonas aeruginosa isolates from Hamadan, Iran. Mol. Biol. Rep. 48, 5275–5281 (2021).
Namaki, M. et al. Prevalence of resistance genes to biocides in antibiotic-resistant Pseudomonas aeruginosa clinical isolates. Mol. Biol. Rep. 49, 2149–2155 (2022).
Boutarfi, Z. et al. Biocide tolerance and antibiotic resistance of Enterobacter spp. isolated from an Algerian hospital environment. J. Glob. Antimicrob. Res. 18, 291–297 (2019).
Medardus, J. J. et al. In-feed use of heavy metal micronutrients in U.S. swine production systems and its role in persistence of multidrug-resistant Salmonellae. Appl. Environ. Microbiol. 80, 2317–2325 (2014).
Correa, J. E., De Paulis, A., Predari, S., Sordelli, D. O. & Jeric, P. E. First report of qacG, qacH and qacJ genes in Staphylococcus haemolyticus human clinical isolates. J. Antimicrob. Chemother. 62, 956–960 (2008).
Jiang, X. et al. Examination of quaternary ammonium compound resistance in Proteus mirabilis isolated from cooked meat products in China. Front. Microbiol. 8, 2417 (2017).
Jiang, X. et al. Characterization and horizontal transfer of qacH-associated class 1 integrons in Escherichia coli isolated from retail meats. Int. J. Food Microbiol. 258, 12–17 (2017).
Wales, A. D. & Davies, R. H. Co-selection of resistance to antibiotics, biocides and heavy metals, and its relevance to foodborne pathogens. Antibiotics 4, 567–604 (2015).
Pal, C. et al. Metal resistance and its association with antibiotic resistance. Adv. Microb. Physiol. 70, 261–313 (2017).
Sidhu, M. S., Heir, E., Leegaard, T., Wiger, K. & Holck, A. Frequency of disinfectant resistance genes and genetic linkage with beta-lactamase transposon Tn552 among clinical staphylococci. Antimicrob. Agents Chemother. 46, 2797–2803 (2002).
Harrison, K. R., Kappell, A. D. & McNamara, P. J. Benzalkonium chloride alters phenotypic and genotypic antibiotic resistance profiles in a source water used for drinking water treatment. Environ. Poll. 257, 113472 (2020).
Siani, H. & Maillard, J.-Y. Best practice in healthcare environment decontamination. Eur. J. Infect. Control. Infect. Dis. 34, 1–11 (2015).
Van Asselt, A.J. & te Giffel, M. C. in Handbook of Hygiene Control in the Food Industry (eds Lelieveld, H. L. M., Mostert, M. A. & Holah, J.) 69–92 (Woodhead Publishing, 2005).
Maillard, J.-Y. et al. Reducing antibiotic prescribing and addressing the global problem of antibiotic resistance by targeted hygiene in the home and everyday life settings: a position paper. Am. J. Infect. Control. 48, 1090–1099 (2020).
Wellcome Trust. The Global Response to AMR. Momentum, Success, and Critical Gaps. Wellcome Trust https://cms.wellcome.org/sites/default/files/2020-11/wellcome-global-response-amr-report.pdf (2020).
O’Neil, J. Tackling Drug-Resistant Infections Globally; Final Report and Recommendations. Wellcome Trust and HM Government https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf (2016).
Zhang, M., Chen, L., Ye, C. & Yu, X. Co-selection of antibiotic resistance via copper sock loading on bacteria from drinking water bio-filter. Eviron. Poll. 233, 132–141 (2018).
Fernando, D. M., Xu, W., Loewen, P. C., Zhanel, G. G. & Kumar, A. Triclosan can select for an AdeIJK-overexpressing mutant of Acinetobacter baumannii ATCC 17978 that displays reduced susceptibility to multiple antibiotics. Antimicrob. Agents Chemother. 58, 6424–6431 (2014).
Mc Cay, P. H., Ocampo-Sosa, A. O. & Fleming, G. T. A. Effect of subinhibitory concentrations of benzalkonium chloride on the competitiveness of Pseudomonas aeruginosa grown in continuous culture. Microbiology 156, 30–38 (2010).
Mavri, A. & Smole Možina, S. Development of antimicrobial resistance in Campylobacter jejuni and Campylobacter coli adapted to biocides. Int. J. Food Microbiol. 160, 304–312 (2013).
Tong, C. et al. Chlorine disinfectants promote microbial resistance in Pseudomonas sp. Environ. Res. 199, 111296 (2021).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the manuscript.
Corresponding author
Ethics declarations
Competing interests
J.-Y.M. is the Director of Biocide Consult Ltd. M.P. declares no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks Anabela Borges, Ilias Tagkopoulos, Manuel Simões and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ECHA: https://echa.europa.eu/information-on-chemicals/biocidal-active-substances
ECHA, Biocidal Product Regulation: https://echa.europa.eu/regulations/biocidal-products-regulation/legislation
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maillard, JY., Pascoe, M. Disinfectants and antiseptics: mechanisms of action and resistance. Nat Rev Microbiol 22, 4–17 (2024). https://doi.org/10.1038/s41579-023-00958-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41579-023-00958-3
This article is cited by
-
Co-selection for antibiotic resistance by environmental contaminants
npj Antimicrobials and Resistance (2024)
-
Operando investigation of the synergistic effect of electric field treatment and copper for bacteria inactivation
Nature Communications (2024)



