Abstract
The galectin family consists of carbohydrate (glycan) binding proteins that are expressed by a wide variety of cells and bind to galactose-containing glycans. Galectins can be located in the nucleus or the cytoplasm, or can be secreted into the extracellular space. They can modulate innate and adaptive immune cells by binding to glycans on the surface of immune cells or intracellularly via carbohydrate-dependent or carbohydrate-independent interactions. Galectins expressed by immune cells can also participate in host responses to infection by directly binding to microorganisms or by modulating antimicrobial functions such as autophagy. Here we explore the diverse ways in which galectins have been shown to impact immunity and discuss the opportunities and challenges in the field.
Similar content being viewed by others
Introduction
Canonical pathways of immune regulation involve ligand–receptor interactions that transmit predicable signalling outcomes1. The discrete nature of such ligand–receptor pairs, including the specific signalling pathways they engage, lends well to genetic and pharmacological approaches to define their biological functions. However, another level of essential immune regulation involves interactions of greater complexity. Mammals express various carbohydrate (glycan) binding proteins (GBPs) that recognize glycosylated proteins and glycosylated lipids (glycoconjugates). The targeted modifications on these glycoconjugates are highly variable2. Glycan modifications cannot be predicted based on the amino acid sequence of a given glycoprotein but, instead, are dictated by the repertoire of glycosyltransferases and substrates responsible for their synthesis3. As a result, the same protein (or lipid) can be decorated by different carbohydrate modifications depending on the type, differentiation and overall activation state of a given cell3. In this way, the nature and abundance of glycans of a given glycoconjugate, not protein or lipid levels alone, can dictate how well a given GBP binds. As different glycoconjugates may express the same glycan structure, different proteins or lipids on a cell surface may be engaged by a given GBP, allowing GBPs to potentially modulate or activate various distinct receptors. Thus, the role of GBPs in immune signalling and regulation fundamentally differs from other immune regulators, such as cytokine-receptor pathways.
Galectins were the first family of GBPs for which immune regulatory activity was described and they represent the most ancient arm of mammalian GBP evolution4,5. In vertebrates, more than 16 galectins have been characterized (galectin-1–galectin-16), and are often classified according to their overall structure into prototype galectins, chimaera-type galectins and tandem-repeat galectins6 (Fig. 1). Galectin-1 and -3 are expressed in nearly every tissue and by most cell types examined7,8, whereas other galectins appear to have a more restricted expression profile: galectin-7 is mainly expressed by stratified epithelial cells; galectin-9 is mainly expressed by gastrointestinal epithelial cells, the thymus and endothelial cells; and galectin-12 is mainly expressed by adipocytes9,10,11,12.
Galectins can be classified into prototypical galectins, chimaera-type galectins and tandem-repeat galectins according to their overall structural features. Prototypical galectins exist in a monomer–dimer equilibrium with the extent of dimerization at steady state differing for each individual galectin. a, Extracellular galectins can engage common glycan motifs that can be present on many different glycoproteins and glycolipids, which are expressed on the surface of most cells. As such, galectins can bind a wide variety of glycoprotein and glycolipid receptors, which can result in distinct signalling outcomes depending on the different types of receptors engaged. Importantly, the glycan modifications of cell surface proteins can change following cellular activation and differentiation. This can result in galectin engagement of completely different glycoprotein or glycolipid targets and, therefore, different signalling outcomes. In immune cells (both innate immune cells such as macrophages and dendritic cells, and adaptive immune cells such as T cells and B cells), such interactions can affect cell activation, cytokine secretion, chemotaxis and cell fate. b, Galectins are synthesized and are either secreted or reside in the cytosol, due to their lack of a classical signal sequence, but can also shuttle to the nucleus. Cytosolic galectins can impact cellular signalling by directly binding intracellular targets such as BCL-2 and ALG2-interacting protein X (ALIX) (Supplementary Table 3) through carbohydrate-independent interactions. This can affect cell signalling, survival, phagocytosis and autophagy. c, Intracellular galectins can also bind exposed glycans following organelle damage, inducing autophagy (shown in detail in Fig. 4).
Galectins can be found in the extracellular space where they are able to bind a broad range of glycoconjugates13,14, including those located on the cell surface and extracellular matrix. In addition, galectins are unique amongst GBPs in that they can regulate diverse processes intracellularly, which can occur through glycan-independent or glycan-dependent interactions14. Given that galectins are expressed in many tissues, coupled with their ability to regulate immune activities through diverse intracellular and extracellular processes, galectin-mediated immune regulation shows a high level of complexity.
Here, we highlight the diverse mechanisms by which galectins can regulate adaptive and innate immune responses. We first describe the general characteristics of galectins and explore their roles in regulating adaptive immunity, in particular T cell biology, and in regulating innate immunity, including macrophage activation, immune cell recruitment and phagocytosis. We also discuss the diverse ways in which galectins may influence the consequence of pathogen exposure and highlight the recent discovery that cytosolic galectins can function as sensors of organelle injury. It should be noted that galectins have also been implicated in modulating the tumour microenvironment through altering vascular biology and by engaging the immune system, which has been discussed in detail elsewhere15,16,17,18,19.
General characteristics of galectins
Nearly all mammalian members of the galectin family bind predominantly to a common glycan modification, galactose β1,4-N-acetylglucosamine (LacNAc), which is present on different glycoproteins on the surface of nearly every cell20,21,22. Similar to other GBPs, galectins are present in the extracellular space, where they can bind to glycosylated cell surface receptors and, thereby, modulate the behaviour of many different types of cell. However, many galectins have been shown to bind to a large number of different cell surface glycoproteins (Supplementary Table 1), which makes it very challenging to study these proteins using approaches commonly employed to study the classical one protein–one receptor paradigm. In addition, LacNAc modifications, which can change depending on the differentiation and activation state of a given cell, can modulate different galectin–glycan interactions, potentially altering the intracellular signalling pathways that are activated following galectin exposure (Supplementary Table 2). In this way, the impact of extracellular galectins on a given receptor can change depending on the glycan signature of the receptor.
Unlike other GBPs, galectins also reside intracellularly and, indeed, represent the only protein family with known intracellular carbohydrate-binding activity. The presence of galectins in the cytosol was initially intriguing, considering that their ligands are carbohydrates that are synthesized and exocytosed through the endoplasmic reticulum–Golgi pathway and are primarily found in the extracellular environment (Box 1). However, it has since been shown that galectins can also interact with intracellular proteins through glycan-independent mechanisms2 (Fig. 1). Different galectins appear to engage distinct sets of intracellular partners, which is consistent with the fact that galectins have only a moderate degree of homology (approximately 30–40% sequence identity among most members). Galectin-3, in particular, has a unique amino-terminal non-lectin domain that can interact with intracellular proteins. Moreover, it was recently discovered that intracellular galectins can interact with glycans that are exposed to the cytosol after endolysosomal damage. Here, the binding of galectins allows for the formation of ‘signalling platforms’ that can modulate numerous cellular processes, including autophagy.
In contrast to most other immune regulators, many galectins are constitutively expressed in a wide range of tissues. However, each galectin can exhibit unique tissue expression patterns, and tissue differentiation, injury and inflammation can enhance galectin expression. The mechanism by which galectins are secreted from cells include an as yet incompletely defined, endoplasmic reticulum–Golgi-independent pathway following cell activation, differentiation or injury23,24,25,26. As galectins bind to glycan ligands that are widely found on most cells, key regulatory mechanisms have evolved that limit galectin activity (both spatially and temporally) following their release into the extracellular space. For example, some galectin family members are sensitive to oxidative inactivation or proteolytic degradation following exposure to the extracellular environment6,27,28,29,30,31.
It is important to note that these properties have significant implications for the design and interpretation of experiments that interrogate the activity of galectins. This is especially true for in vivo models where galectins are systemically administered, as well as in vitro experiments where cells are incubated with galectins (Box 2). Thus, although galectins have been implicated in a wide variety of immune pathways, investigations to define exactly how they influence immune activity within an organism can be challenging.
Here, we primarily focus our discussion on studies that addressed the function of endogenous galectins in experiments in which specific galectins were either inhibited or genetically deleted. We have also included select studies in which the function of galectins were demonstrated in vitro using galectins administered to the cell culture, but describe the limitations of these studies in Box 2.
Regulation of adaptive immunity
The earliest and most extensive studies demonstrating that galectins regulate immune activity primarily focused on T cells. Key findings include the ability of galectins to modulate processes in the development and contraction of an adaptive immune response such as T cell activation and apoptosis (Fig. 2). These studies have implicated an anti-inflammatory role for many galectins in nearly every aspect of adaptive immune responses, from activation to resolution, and thereby provide a possible negative feedback mechanism in the setting of autoimmunity through various distinct extracellular and intracellular mechanisms.
Galectins can modulate adaptive immune cells through both intracellular and extracellular mechanisms and via their effects on antigen-presenting cells (APCs) and other innate immune cells. a, Extracellular galectin-3 can modulate T cell activation through engagement of extracellular glycans on co-receptors such as CD8 and other cell surface glycoconjugates, which restricts CD8 interactions with the T cell receptor (TCR) and, ultimately, MHC class I at the immmunological synapse. This, in turn, weakens TCR signalling. Galectin-3-mediated restriction of CD8 in this manner is mediated by β1,6-N-acetylglucosaminyltransferase V (MGAT5), an enzyme that is induced by IL-10 and catalyses the formation of branched N-glycans bearing polylactosamine structures that are common galectin ligands37. Intracellular galectin-3 can upregulate the threshold for TCR activation by binding the adaptor protein ALG2-interacting protein X (ALIX)38, whereas galectin-9 can have the opposite effect on the TCR through engagement of intracellular partners that remain to be described41. b, Galectin-1, -8 or -9 knockout mice appear to have a defect in T cell contraction after challenge, and extracellular administration of galectin-1, -2, -3, -8 and -9 has been shown to induce apoptosis in T cells in vitro45,46,47,48. However, whether and how these galectins regulate T cell fate in vivo remains to be elucidated, especially in view of the issues described in Box 2. In addition, intracellular galectin-3 can inhibit T cell apoptosis through interactions with the anti-apoptotic protein BCL-2 (refs. 49,50). c, Galectins have also been shown to regulate B cell differentiation through extracellular and possibly intracellular processes. For example, galectin-3 knockout B cells display an enhanced proclivity to differentiate into germinal centre B cells and plasma cells that produce IgG2c or IgG3, all of which may enhance the probability of antibody-mediated autoimmunity59. Galectin-3 expressed by B cells can suppress B cell differentiation, probably via intracellular mechanisms59. d, On naive B cells, galectin-9 can recruit glycosylated forms of the transmembrane proteins CD22 and CD45 to the B cell receptor (BCR). CD45 is bound by the phosphatase SHP1, which downregulates BCR signalling55,56. In contrast, germinal centre B cells express the carbohydrate I antigen which reduces the ability of galectin-9 to facilitate CD22 and CD45-mediated inhibition of B cell signalling and enhances B cell responses following antigen engagement.
T cell activation
Recombinant galectins have been shown to engage a range of glycoproteins that are involved in orchestrating T cell activation, including CD2, CD7, CD8, CD43, CD45 and the T cell receptor (TCR)32. This can result in their reorganization and alter the half-life of surface receptors, as well as changes in membrane structure, which may impact signalling microdomains and influence T cell activation33,34.
Early studies of the role of galectins in T cell function examined the impact of β1,6-N-acetylglucosaminyltransferase V (MGAT5), which is responsible for generating branched N-glycans bearing polylactosamine structures commonly recognized by galectins21,35,36. In the mouse experimental autoimmune encephalomyelitis (EAE) model of multiple sclerosis, Mgat5 knockout mice showed higher levels of autoimmunity and enhanced TCR signalling36. In vitro incubation of wild type T cells with lactose, which removes galectin-3 from the cell surface, resulted in the relocalization of key signalling constituents to the immunological synapse and in enhanced signalling outcomes36. This suggests that altered galectin binding on the surface of T cells in Mgat5 knockout mice may account for the observed T cell phenotype.
More recently, the anti-inflammatory cytokine IL-10 was shown to upregulate the expression of Mgat5 in T cells. The authors demonstrated that MGAT5 enhances the glycosylation of the TCR, and that increased binding of extracellular galectin-3 to the TCR affects the co-localization of the TCR and CD8, thereby increasing the threshold for T cell activation37. Importantly, unlike in wild-type mice, IL-10-mediated upregulation of MGAT5 expression in galectin-3 knockout mice did not lower the activation threshold of CD8+ T cells37, supporting a role for galectin-3 in elevating the threshold for TCR signalling.
Intracellular galectin-3 has been shown to translocate to the cytosolic side of the immunological synapse in CD4+ T cells upon activation, where it downregulates the surface expression of key components of the TCR, thereby limiting T cell activation38. Although additional studies are needed to define the mechanisms responsible for this outcome, intracellular galectin-3 may accomplish this through non-carbohydrate-dependent intracellular interactions with the multifunctional adapter protein ALG2-interacting protein X (ALIX)38,39. Intracellular galectin-3 was also found to be localized in the immunological synapse in both naive and memory CD8+ T cells when activated by γ-herpesvirus (MHV68)40. Galectin-3 knockout mice mount a stronger MHV68-specific CD8+ T cell response compared with wild-type mice40, indicating that intracellular galectin-3 can upregulate the threshold for T cell activation. Overall, these studies suggest that both extracellular and intracellular galectin-3 can dampen T cell activation by altering the distribution and half-life of distinct cell surface glycoproteins.
T cell differentiation
Similar to galectin-3, intracellular galectin-9 is recruited to the cytosolic side of the immune synapse upon T cell activation41. Enhanced expression of galectin-9 is associated with an increased production of T cell cytokines, including IL-17, following T cell activation41. Galectin-9 knockout mice exhibit reduced IgA production following oral antigen exposure, which correlated with a reduced number of T helper 17 cells (TH17 cells) and lower levels of IL-17 production42. As exposure to an IL-17 blocking antibody can reduce IgA production, these results suggest that galectin-9 may increase IgA production by promoting the differentiation of CD4+ T cells into TH17 cells42. Moreover, galectins can affect T cell activation and differentiation through the modulation of antigen-presenting cells (APCs), as described in the discussion of innate immune cells.
T cell contraction
Following the initial activation and expansion of T cells in response to pathogen challenge, a contraction of the T cell population occurs43. The earliest and most informative studies that examined the direct interactions of galectins with T cells implicated galectin-1 in the process of T cell contraction. Here, the incubation of activated T cells with galectin-1 in vitro resulted in apoptosis44. This activity does not appear to be limited to galectin-1, as similar in vitro studies suggested that extracellular galectin-2, -3, -8 and -9 may exert an immunosuppressive function by directly inducing apoptosis in T cells45,46,47,48. Additional studies indicate that intracellular galectin-3 can also inhibit T cell apoptosis in a cell-intrinsic manner49,50 and galectin-3 was shown to have sequence homology with and bind to the anti-apoptosis protein BCL-2 (ref. 50).
In the EAE mouse model of multiple sclerosis, systemic administration of galectin-1 and -9 inhibits autoimmunity, which likely reflects the ability of these galectins to induce apoptosis of autoreactive T cells44. However, as outlined in Box 2, there are caveats to interpreting galectin activity in animal studies where galectins are systemically administered. Nevertheless, these findings were strengthened in experiments with knockout mice where the deletion of specific galectins exacerbated disease in models of autoimmune conditions45,46,47,51. For example, galectin-1, -8 or -9 knockouts have an exaggerated clinical score and increased numbers of TH1 cells and TH17 cells in the EAE model45. Of note, increases in the number of CD8+ T cells have also been observed in galectin-9 knockout mice following challenge with herpes simplex virus (HSV)52, suggesting that the regulation of T cell fate is not limited to CD4+ T cells or autoimmunity. Together, these studies suggest that several different types of galectins have a role in the contraction of T cell populations and raises the possibility that systemic administration of galectins may be of therapeutic value in autoimmune diseases.
B cells
The various mechanisms by which galectins can modulate T cells would also be expected to impact T cell-dependent B cell responses. As described above, galectin-9 appears to enhance the production of IgA by plasma cells by promoting the differentiation of TH17 cells42. In contrast, intracellular galectin-3 appears to impair the differentiation of B cells into IgA-producing plasma cells, as it was shown that peritoneal B1 cells from galectin-3 knockout mice exhibited enhanced differentiation to IgA-producing plasma cells when treated with IL-5 plus TGFβ1 in vitro53. Moreover, there are indications that extracellular galectins may also directly engage B cell surface glycans and affect B cell signalling, activation and differentiation into antibody secreting cells54. For example, endogenous galectin-9 can be found on the surface of primary naive B cells, where it appears to regulate microdomain clustering, particularly of CD22 and CD45. This can suppress B cell receptor (BCR) signalling through CD45-mediated recruitment of SHP1 (refs. 55,56), resulting in an inhibition of B cell activation and their subsequent differentiation into plasma cells57. Likewise, changes in the glycosylation of surface proteins of B cells can impact the binding of extracellular galectin-1 and galectin-8 and affect B cell differentiation. For example, it was shown that functional impairment of both galectin-1 and galectin-8 through knockout, knockdown or the use of inhibitors can reduce B cell differentiation into plasma cells in vitro58. Galectin-3 can also attenuate germinal centre B cell development through the suppression of IFNγ production and T follicular helper cell differentiation, as shown in a mouse model of lupus59. Galectin-3 knockout mice exhibited a higher number of germinal centre B cells, increased levels of autoantibodies and a propensity to develop lupus-like autoimmune disease. This is likely mediated through a B cell intrinsic processs59, as demonstrated by adoptive transfer experiments.
Regulation of innate immunity
As galectins are expressed and potentially released by a wide range of cells, innate immune cells may encounter them at various stages of an immune response, and various innate immune cells are known to express galectins. Accordingly, a large number of studies have shown that galectins can regulate various aspects of innate immunity (reviewed elsewhere31,60,61,62,63,64) and contribute to diverse immune and inflammatory responses (Fig. 3). Some galectins promote these responses, whereas others have suppressive roles; for a given galectin, this may depend on the experimental conditions or models used. Additionally, numerous studies have shown that galectins can also function as intracellular regulators in innate immune cells and that many intracellular galectin activities are independent of carbohydrate binding (Supplementary Table 3).
Several different galectins have been shown to affect macrophage polarization, phagocytosis and inflammasome activation. For example, galectin-3 was shown to be induced in cardiac macrophages in models of myocardial infarction where it promoted their polarization into M2-like macrophages, which contribute to tissue repair by promoting fibrosis and clearance of apoptotic cells after myocardial infarction79. Here, galectin-3 expression was induced via IL-10-mediated activation of the transcription factor STAT3. In vitro experiments have also shown that IL-4 induces galectin-3 expression and galectin-3 facilitates M2-like macrophage polarization by binding CD98, which induces PI3K (ref. 78). By contrast, galectin-12 (which is primarily located intracellularly and expressed by adipocytes, where it has a key role in adipogenesis12) is also expressed by myeloid cells80, where it was shown to be a positive regulator of M1 macrophage polarization in response to treatment with lipopolysaccharide (LPS)81. This was related to decreased activation of IKKα/β, AKT and ERK downstream of Toll-like receptor 4 (TLR4) which results in decreased activation of NF-κB, resulting in M1 polarization. Intracellular galectin-3 is also a positive regulator of the NLRP3 inflammasome75,76 and was shown to physically associate with NLRP3 in isolated hepatic macrophages, promoting IL-1β production75. Moreover, intracellular galectin-3 is a positive regulator of macrophage phagocytosis. In vitro experiments showed that it is localized at the cytosolic side of phagosomes where it is involved in actin rearrangement82. Similar observations were made in cultured primary microglia83. Additional studies suggest that galectin-3 controls the activation state of cofilin, which affects actin filament organization and stability83. Intracellular galectin-9 has also been shown to enhance phagocytosis through the regulation of actin filament formation84.
Overall, these studies point to the differential regulation of common intracellular pathways in macrophages and other immune cells by different galectins. The potential role of intracellular versus extracellular galectins in this context continues to be studied. Galectin-3, which is released following tissue injury, has been proposed to act as an extracellular damage-associated molecular pattern that induces innate immune cell activation65. However, most studies in this context have the caveat of relying on recombinant (rather than endogenous) galectin-3 for the assessment of its activity.
Regulation of APCs
In addition to directly affecting T cell signalling, galectins can inhibit or augment the activation of APCs and their cytokine secretion, which, in turn, can impact T cell activation and differentiation. This was first observed following allogeneic mating of galectin-1 knockout mice, which led to an increased rate of spontaneous abortions, consistent with impaired fetal–maternal tolerance66. Galectin-1 was also shown to enhance the ability of tolerogenic dendritic cells to suppress autoimmunity in the EAE mouse model of multiple sclerosis, where the adoptive transfer of dendritic cells isolated from wild-type mice, but not galectin-1 knockout mice, reduced EAE progression. This occurred even when transferred after the initial disease onset, suggesting that galectin-1 can facilitate tolerance through a dendritic cell-mediated process in this setting67. Similar observations were made in a mouse model of the autoimmune condition Sjögren syndrome68.
Two studies using bone marrow-derived dendritic cells from galectin-3 knockout mice concluded that galectin-3 suppresses the production of various cytokines, including IL-10 and IL-23, in dendritic cells69,70. This activity may explain how galectin-3 can suppress TH2-type and TH17-type polarization in CD4+ T cells in experiments in which these were co-cultured with dendritic cells40,70. Another study using galectin-3 knockout mice indicated that galectin-3 suppresses Notch signalling upon stimulation with the Notch ligand Jagged1 (JAG1), which attenuates bone marrow-derived dendritic cell IL12p40 production71. In vitro experiments showed that knockdown of galectin-1 or galectin-3 in dendritic cells increases allogenic T cell responses72, implying that these galectins dampen such responses. However, galectin-3 has also been shown to enhance APC-mediated T cell activation in some settings. For example, in a model of ConA-induced hepatitis, galectin-3 knockout mice had attenuated T cell responses, which was linked to a reduced production of IL-12 and enhanced production of IL-10 by dendritic cells and macrophages73. Such apparent discrepancies in the role of galectin-3 during APC-mediated T cell activation or suppression have not yet been resolved.
Macrophage activation
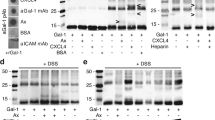
Various stimuli can trigger the activation of macrophages via extracellular and intracellular mediators. Among the intracellular mediators, the inflammasome is critical for the secretion of the pro-inflammatory cytokines IL-1β and IL-18. Studies indicate that galectin-3 can affect inflammasome activation. For example, in a model of dextran sulfate sodium (DSS)-induced colitis, galectin-3 knockout mice developed less severe colitis than wild-type mice, and the authors demonstrated that endogenous galectin-3 can promote NLRP3 inflammasome activation within macrophages74. In another study using isolated hepatic macrophages, a physical association between galectin-3 and NLRP3 was demonstrated75. Also, in a model of biliary disease, galectin-3 knockout mice exhibited reduced disease severity along with attenuated TH17-type immune responses in the liver76. Here, the deficiency in galectin-3 resulted in lower NLRP3 inflammasome expression and a lower amount of IL-1β in macrophages76. These studies indicate that galectin-3 can induce both NLRP3 inflammasome expression and activation in macrophages, and thereby enhance their inflammatory activity.
Similar to galectin-3, galectin-9 also interacts intracellularly with NLRP3, but with opposite effects. In primary peritoneal macrophages and HEK293T cells, galectin-9 was shown to promote the formation of a complex between NLRP3 and the autophagy receptor p62, thereby facilitating the autophagic degradation of NLRP3 (ref. 77). Galectin-9 knockout mice exhibited enhanced NLRP3 inflammasome activation and NLRP3-dependent inflammation77.
Macrophage polarization
Under the influence of various extracellular stimuli, macrophages can be differentiated in vitro into pro-inflammatory M1-like macrophages (when ‘classically’ activated with IFNγ and lipopolysaccharide (LPS)) or anti-inflammatory M2-like macrophages (when ‘alternatively’ activated with IL-4 or IL-10). Experiments with bone marrow-derived macrophages from galectin-3 knockout, siRNA-mediated galectin-3 knockdown and pharmacologic inhibition of galectin-3 revealed that galectin-3 facilitates the IL-4-induced activation of M2-like macrophages78. Moreover, galectin-3 was shown to be expressed by cardiac macrophages in animal models of myocardial infarction, where it promoted their polarization into M2-like macrophages. These contribute to tissue repair by promoting fibrosis and clearance of apoptotic cells after myocardial infarction79. In this system, the expression of galectin-3 was induced by IL-10, which activates the transcription factor STAT3. In contrast, galectin-12, which is primarily expressed by adipocytes and plays a key role in adipogenesis12, but is also expressed by myeloid cells80, was shown to be a positive regulator of M1-like macrophage polarization in response to treatment with LPS81. This was linked to its enhancement of IKKα/β, AKT and ERK activation, which results in increased activation of NF-κB and AP1, favouring M1-like macrophage polarization81.
Macrophage phagocytosis
Various cell surface receptors facilitate phagocytosis, and intracellular galectins appear to have a role in this process. For example, it was shown that peritoneal macrophages isolated from galectin-3 knockout mice exhibited a lower capacity to phagocytose IgG-opsonized erythrocytes when compared with wild type cells82. Here, intracellular galectin-3 was found to localize to the cytosolic side of the erythrocyte-containing phagosomes. It appeared to be involved in actin rearrangement, given that galectin-3 knockout macrophages exhibited a lower degree of actin rearrangement upon Fcγ receptor cross-linking82. Similar observations were made following the knockdown of galectin-3 in cultured primary microglia, where these cells exhibited reduced phagocytosis and altered actin rearrangement83. Additional studies suggest that intracellular galectin-3 controls the activation state of cofilin, which affects actin filament organization and stability83, providing a potential mechanism whereby galectin-3 may upregulate phagocytosis.
Intracellular galectin-9 may likewise enhance phagocytosis. Bone marrow-derived dendritic cells from galectin-9 knockout mice showed a reduced uptake of zymosan particles in vitro84. Knockdown of galectin-9 in human monocyte-derived dendritic cells yielded similar findings and also reduced actin filament formation84. Additional in vitro studies with the above-stated sources of dendritic cells, with galectin-9 knocked out or knocked down, suggested that galectin-9, similar to galectin-3, has an intracellular function in the control of phagocytosis, possibly by affecting actin dynamics84.
Innate immune cell recruitment
Galectins also appear to modulate key cellular activities that culminate in leukocyte recruitment, likely by affecting chemoattraction and/or cell adhesion, potentially through both extracellular and intracellular signalling pathways. For example, in psoriasis, a chronic skin condition manifested by epidermal hyperplasia and an infiltration of inflammatory cells into the skin (in particular neutrophils), galectin-3 was found to be downregulated in the lesional epidermis both in humans and in mouse models85. In a mouse model of psoriasis induced by topical application of imiquimod, galectin-3 was shown to inhibit neutrophil accumulation in lesional skin by serving as a negative regulator of the expression of mediators associated with neutrophil recruitment, including S100A7, CXCL1 and CXCL8 (ref. 85). Galectin-3 can also suppress the JNK pathway, which is involved in S100A7 production85.
Similar to galectin-3, galectin-7 was also downregulated in lesional skin in patients with psoriasis, as well as in a mouse model of psoriasis where disease is induced by intradermal injection of IL-23, known to promote the production of IL-17A, a key cytokine responsible for the development of the disease86. Knockdown experiments in a human keratinocyte cell line and in primary cultures of human keratinocytes showed that endogenous galectin-7 suppresses the IL-17A-induced expression of IL-6 and IL-8, two key cytokines responsible for neutrophil accumulation in psoriatic skin lesions. This appeared to be due to the suppression of miR-146 by galectin-7, resulting in a downregulation of the ERK pathway and a subsequent reduction in the production of IL-6 and IL-8 (ref. 86). These findings were further supported by the observation that galectin-7 knockout mice have enhanced epidermal hyperplasia and skin inflammation in response to intradermal IL-23 injection86, further indicating that galectin-7 has a suppressive role in psoriasis pathogenesis.
In contrast, in models of airway inflammation induced by various infectious agents, galectin-3 knockout mice displayed impaired neutrophil recruitment87,88,89. Experiments with myeloid cell-specific galectin-3 knockout mice indicated that myeloid cells are a source of secreted galectin-3 that contributes to neutrophil accumulation in the lungs in response to LPS-induced airway inflammation90. Moreover, galectin-3 was also implicated in neutrophil recruitment in mice that received a footpad injection of the parasite Leishmania major91. It is not clear why galectin-3 deficiency in these models results in an attenuated neutrophil response, whereas in the model of skin inflammation it results in an enhanced response85.
Galectin-3 has also been linked to the development of allergic airway inflammation through the modulation of the eosinophil response. Compared with wild-type mice, galectin-3 knockout mice had lower levels of airway inflammation, including eosinophil infiltration, in models of acute and chronic asthma92,93. By contrast, in a mouse model of acute asthma, galectin-1 deficiency resulted in greater airway hyper-responsiveness and eosinophil airway infiltration, suggesting that galectin-1 can suppress allergic airway inflammation in this context94.
Another example of a role of galectin-3 in promoting immune cell recruitment was provided by the study of a model of multiple sclerosis induced by Theiler murine encephalomyelitis virus (TMEV). Galectin-3 knockout mice exhibited lower numbers of CD45+ immune cells infiltrating the subventricular zone in the brain compared with wild-type mice, which correlated with lower levels of chemokines (CCL2, CCL5, CCL and CXCL10)95.
Thus, the roles of endogenous galectins in inflammatory cell recruitment continue to be clarified. Some galectins, such as galectin-3, appear to promote inflammation via the activation or recruitment of innate immune cells in conditions such as colitis and airway inflammation. In contrast, both galectin-3 and galectin-7 can inhibit leukocyte chemotaxis in the setting of psoriasis, and galectin-1 appears to suppress airway eosinophil accumulation in a mouse model of asthma.
Autophagy in response to intracellular vacuolar damage
As described in Box 1, glycoconjugates reside in the lumen of various organelles; here, they are not accessible to intracellular galectins. However, under certain conditions these vesicles are damaged, thereby allowing glycoconjugates to be exposed to the cytoplasmic milieu where they can be bound by cytosolic galectins. The exposed glycans serve as anchors or adaptors for intracellular galectins, although different galectins appear to engage distinct sets of glycoconjugates. In this context, the intracellular galectins bind both carbohydrates and non-carbohydrates — and thereby form a signalling platform that allows for the modulation of cellular responses including autophagy (Fig. 4), the recruitment of antibacterial mediators and, potentially, also inflammasome activation.
Under normal conditions, glycoconjugates reside in the lumen of organelles and thus are not accessible to intracellular galectins, which are located in the cytosol or the nucleus. However, these organelles can become disrupted by intracellular bacteria that cause damage to phagosomes as they escape into the cytosol, toxins secreted into cells by extracellular bacteria, certain viruses and intracellular protein aggregates. Lysosomal damage can also be induced with agents such as Leu-Leu-O-Me (LLOMe) and glycyl-l-phenylalanine 2-naphthylamide (GPN). This can lead to the exposure of glycoconjugates to the cytosolic milieu, where these can be bound by various intracellular galectins. Given that galectins can also bind to various signalling molecules via non-carbohydrate interaction, this can lead to the formation of ‘signalling platforms’ that can induce autophagic activation and bacterial destruction. For example, galectin-8 was shown to bind to the autophagy adaptor NDP52 and initiate the formation of antibacterial autophagosomes around Salmonella-containing vesicles117. Galectin-3 was shown to direct the recruitment of the interferon-inducible guanylate binding proteins to intracellular vacuoles damaged by intracellular bacteria116. In a model of lysosomal damage, galectin-3 and galectin-8 were found to bind to exposed β-galactosides on damaged membranes, where both galectins can become associated with the autophagy regulator TRIM16 and triggered autophagy104. In another model, galectin-8 was shown to associate with the mTOR apparatus, which is normally localized on the surface of lysosomes and serves as an inhibitor of autophagy. This results in inactivation of mTOR and thus autophagic activation106. Galectin-9 binding to glycoproteins on damaged lysosomes results in displacement of its cytosolic binding partner, the deubiquitinase USP9X (ref. 107). This inhibits the enzyme and enhances cellular ubiquitination responses, leading to the activation of a protein kinase TAK1 and, in turn, its downstream AMP-activated protein kinase (AMPK), an inducer of autophagy107.
Endolysosomal damage can be caused by stressors such as intracellular infections, including those by bacteria (see below), viruses96 and protozoa97, as well as oxidative stress98, free radical formation99 and endocytosed nanoparticles100. Another group of notable insults are membrane disruptive protein aggregates, which are implicated in neurodegenerative diseases (Box 3).
To date, the binding of galectins to cytosolic glycans on damaged organelles has been shown for galectin-1, -3, -7, -8 and -9. Alterations in host cell surface glycosylation by extracellular glycosidases, as can occur during inflammation99, may result in the differential recruitment of cytosolic galectins to damaged endosomes/lysosomes and in altered autophagic activation101. From a practical perspective, the formation of galectin puncta, resulting from accumulation of these proteins around damaged organelles, is now recognized as a sensitive method to detect lysosomal membrane permeabilization102.
Experimentally, lysosomal damage can be induced with agents such as Leu-Leu-O-Me (LLOMe), and experiments using this agent have uncovered several mechanisms by which galectins may be involved in the activation of autophagy. For example, the clearance of Mycobacterium tuberculosis by macrophages was enhanced by the treatment of cells with LLOMe. This appeared to be mediated by the binding of galectin-3 to exposed β-galactosides on damaged membranes, where it then associates with the autophagy regulator TRIM16, which proved critical for autophagy induction and bacterial clearance103. Galectin-8 has also been reported to engage TRIM16 following LLOMe-mediated lysosomal damage. This induced secretory autophagy, resulting in the translocation of IL-1β to the extracellular milieu104. Interestingly, galectin-3 was also found to mediate the repair of damaged lysosomes following binding to glycoconjugates in damaged organelles in cells treated with LLOM, which appeared to be mediated through its interaction with ALIX105, an intracellular binding partner of galectin-3 (refs. 38,39).
Another agent that causes lysosomal damage is glycyl-l-phenylalanine 2-naphthylamide (GPN). In human peripheral blood monocyte-derived macrophages treated with this agent, galectin-8 becomes associated with the mTOR apparatus, which normally localizes on the surface of lysosomes and serves as an autophagy inhibitor. This results in inactivation of mTOR and, thus, autophagic activation106.
Lysosomal membrane damage-induced autophagy is also associated with ubiquitination responses. Jia et al. reported that binding of cytosolically exposed glycans by galectin-9 is critical for this response107. According to their model, galectin-9 binding to lysosomal glycoproteins following lysosomal injury induced by LLOMe results in displacement of the deubiquitinase USP9X, one of its cytosolic binding partners107. This inhibits the enzyme and enhances cellular ubiquitination responses. Ultimately, it leads to the activation of AMP-activated protein kinase (AMPK), an inducer of autophagy107.
The role of galectins in infection
Given that galectins can directly engage pathogens, and also regulate fundamental aspects of innate and adaptive immunity, galectins possess the ability to regulate host responses to pathogens through various mechanisms (see also Box 4; see Supplementary Table 4). Although this has been mostly studied in galectin-3 knockout mice, studies demonstrating the involvement of other galectins have started to emerge and demonstrate that different galectins are involved in host defence to bacteria, viruses, fungi and parasites (Table 1). It should be noted that galectin-mediated regulation of immune defences to microbes is not limited to pathogens, as exposure to galectin inhibitors can result in strain-specific outgrowth of distinct commensal bacteria108, suggesting that galectins may also directly modulate the composition of the microbiota.
Bacterial infections
Compared with wild-type mice, galectin-3 knockout mice have a higher pathogen burden following infection with various bacteria87,109,110,111 and this was associated with various different cellular responses and mechanisms, as summarized in Table 1. These include compromised killing of bacteria by macrophages and impaired neutrophil recruitment. Although galectin-3 can directly bind to and even directly mediate the killing of various bacteria (Box 4), such as Heliobacter pylori109,112, it is unclear whether the increased bacterial loads in galectin-3 knockout mice reflect a deficit in microbial killing. On the other hand, galectin-3 knockout mice were more resistant to infections by some other bacteria, including Brucella abortus and Rhodococcus equi. This was linked to the ability of galectin-3 to suppress the production of pro-inflammatory cytokines that are critical for clearance of bacteria by the host immune cells113,114.
Galectins can affect the cellular responses by functioning as a sensor of vacuolar damage induced by intracellular bacteria. Shigella flexneri115, Yersinia pseudotuberculosis, Legionella pneumophila116, Salmonella Typhimurium117 and Listeria monocytogenes101 can undergo phagosomal escape and induce endolysosomal damage. In these infections, galectin-3 was found to accumulate near the intracellular pathogens97,115,116, where it bound to host N-glycans that became exposed to the cytosol due to phagosomal damage. In the context of Y. pseudotuberculosis or L. pneumophila infection, galectin-3 was shown to facilitate the recruitment of the interferon-inducible guanylate binding proteins GBP1 and GBP2 to damaged intracellular vacuoles containing the microbes116. GBP1 and GBP2 are antimicrobial factors previously known to be recruited to pathogen-containing vacuoles.
The antibacterial response most extensively studied in the context of bacterial endolysosomal damage is autophagy. This was first shown for galectin-8, which binds to exposed glycans on damaged vesicles containing S. Typhimurium117, along with galectin-3 and galectin-9. The accumulation of galectin-8, but not the other two galectins, on damaged vesicles was shown to initiate autophagic activation, resulting in the destruction of the bacteria. Multiple lines of experimental evidence indicated that intracellular galectin-8 binds directly to NDP52, a regulator of autophagy117. In this complex, the N-terminal domain of galectin-8 binds host N-glycans on damaged phagosomes and the carboxy-terminal domain engages NDP52 to facilitate autophagy117,118.
In the context of L. monocytogenes infection, galectin-3 was shown to attenuate autophagy101. In this study, galectin-3 and galectin-8 did not significantly compete with each other in binding to glycans on damaged phagosomes101, consistent with the distinct glycan-binding preferences of these two galectins21,22,119. Additional data suggested that alterations in host cell surface glycosylation by extracellular glycosidases may result in the differential recruitment of cytosolic galectins to damaged endosomes/lysosomes and in altered autophagic activation101. Similar findings were also observed in Chinese hamster ovary cells with endosomal damage due to free radical formation, where galectin-3 and galectin-8 were found to reside in different microdomains on the damaged endosomes120.
There have been far fewer studies on other galectins, especially those containing one carbohydrate-recognition domain. In cells infected with group A Streptococcus, galectin-1 and galectin-7 were found to accumulate around bacteria-containing autophagosomes, and this was dependent on Toll-interacting protein (TOLLIP), which is recruited to bacteria-containing endosomal vacuoles prior to the escape of the bacteria121. Both galectins were shown to participate in bacterial autophagy121.
A study of the role of galectins in the host defence against M. tuberculosis showed that galectin-3, -8 and -9 are all recruited to the same mycobacterial population in infected macrophage cell lines and primary macrophages, where they co-localized with markers of autophagy122. By studying macrophage cell lines with these three galectins knocked out individually and comparing these with macrophages missing all three galectins, the critical role of galectin-8 in autophagic clearance of M. tuberculosis was established122.
Lysosomal damage can also be caused by bacterial toxins. Vacuolating cytotoxin A (VacA), secreted by extracellular H. pylori, was shown to form pores in host cells123. Galectin-8 aggregates around damaged lysosomes after H. pylori infection through binding to the host O-glycans124. This was followed by autophagic activation — an outcome that failed to occur in galectin-8 knockdown cells. VacA-deficient H. pylori induced less galectin-8 aggregation than its wild type counterpart124, which is consistent with the ability of VacA to induce lysosomal injury.
Viruses
Studies of the roles of galectins in viral infections are still relatively scarce. However, there is evidence that galectin-3 may have a role in the host response to viral infections through intracellular mechanisms. These include the observation that it can promote inflammasome assembly and activation in macrophages infected by avian influenza A H5N1 virus125 and suppress TNF production in hepatocytes infected by cytomegalovirus126.
In SARS-CoV-2 infection, serum levels of galectin-1 (ref. 127), galectin-3 (ref. 128) and galectin-9 (ref. 129) are elevated and correlate positively with markers of inflammation and tissue injury. Here, galectins may be predictors of disease severity and may contribute to cytokine release syndrome130. The receptor binding domain of SARS-CoV-2 also possesses some similarities to galectins with regards to its sequence, structure and capacity for carbohydrate binding131, which may account for the observation that glycans can facilitate SARS-CoV-2 entry into cells132.
Fungi
Galectin-3 knockout mice were shown to have a lower fungal burden compared with wild-type mice when systemically infected with Candida albicans (in the kidneys and brain)133 or Histoplasma capsulatum (in the liver)134, indicating that galectin-3 suppresses the host response against fungi. This was linked to its ability to suppress the production of reactive oxygen species (ROS) in neutrophils and, consequently, the fungal killing activity of these cells133, and its ability to suppress IL-23 production in dendritic cells69,134. However, another study of galectin-3 in C. albicans infection showed that galectin-3 knockout mice were more susceptible to infection135, and additional investigations are needed to resolve this discrepancy. Galectin-3 has also been shown to have a suppressive effect on pulmonary aspergillosis88 and cryptococcosis136, as determined by the reduced survival and higher pulmonary fungal burden in galectin-3 knockout mice compared with wild-type mice following intratracheal infections. This was associated with its function in promoting neutrophil infiltration into the airways88 and promoting TH17 cell responses136.
There has been much less research into the role of other galectins in infection, but galectin-1 has been shown to have a protective effect in mice infected with the yeast H. capsulatum137. Galectin-1 knockout showed shorter survival and an increased yeast burden after intratracheal infection, which was associated with a role of galectin-1 in limiting pro-inflammatory cytokine responses and neutrophil pulmonary infiltration137.
Parasites
Several studies have investigated the role of galectin-3 in parasite infections. Remarkably, unlike in some bacterial and fungal infections, galectin-3 deficiency consistently resulted in an increased parasite load in all infection models studied91,138,139,140,141,142,143, suggesting that galectin-3 has a protective role. In most of these infections, the increase in parasite load correlated with a decrease in inflammatory responses in galectin-3 knockout mice and with decreased neutrophil recruitment to the infected sites (Table 1). Mechanistically, the role of galectin-3 in anti-parasite immunity has been linked to its ability to suppress TH1 cell responses141, regulate Toll-like receptor expression on APCs142 and modulate the frequency of peripheral regulatory T cells (Treg cells), both at the sites of infection and in draining lymph nodes139.
There are only a limited number of studies of the roles of other galectins in parasite infections. However, it appears that galectin-1 dampens immunity to parasitic infections144, given that galectin-1 knockout mice survived longer and had a lower parasite count in muscle tissue compared with wild-type mice when subjected to intraperitoneal infection with Trypanosoma cruzi. This is consistent with the often observed opposite effects of galectin-1 and galectin-3 in various innate immune cells, as described above.
As summarized in Table 1, galectins have been shown to either promote or suppress host defences against pathogens. The differential effect of the same galectin in the context of different pathogens is likely because different pathogens affect distinct cell types and tissues, where galectin functions may vary. As for the mechanism of action, many studies listed in Table 1 have suggested that galectins can regulate the recruitment and activation of immune cells that are critically associated with host defence against pathogens. However, other studies highlighted the role of galectins in directly interacting with microbes extracellularly (Supplementary Table 4).
Conclusion
Many studies have demonstrated that galectins can modulate immune cell functions by engaging key cell surface receptors. However, very few strategies have been developed to validate these functions in vivo or investigate whether galectins can be of therapeutic use. This may, in part, reflect challenges associated with delivering galectins locally or systemically, given their ability to agglutinate cells in a nonspecific way and the unlikelihood that systemically delivered galectins would reach desired targets.
Studies using genetic targeting of the proposed cell surface counter-receptors that phenocopy key findings observed in galectin knockouts have also been lacking. This is likely related to the fact that various galectins have been shown to bind to a large number of different cell surface receptors (Supplementary Table 1), and thus can potentially signal through multiple receptors. This makes it very challenging to verify the role of these putative glyco-receptors in vivo. Instead of specific receptors, the concept of ‘galectin lattices’145, which emphasizes a mechanism whereby glycan modification is key for regulating cellular responses by galectins, is intriguing, although additional studies are needed to fully define such a pathway. A galectin lattice is a complex macromolecular structure composed of glycoproteins and/or glycolipids bound by galectins at the cell surface that can influence receptor signalling, glycoprotein and glycolipid cell surface half-life and overall interactions with other cell surface glycoproteins and glycolipids. Regardless of whether galectins mediate some of their biological functions through galectin lattices or individual receptors, methods to inhibit galectin–glycan interactions in general, either through blocking antibodies or glycan derivatives, have been explored and hold promise for establishing their functions146.
As galectins also act intracellularly, modulating immune cell functions by targeting intracellular galectin activities also holds promise. Indeed, the list of intracellular partners continues to expand (Supplementary Table 3). However, validation of these functions in vivo, including the role of the intracellular binding partners, is equally challenging. This is, in part, due to the lack of key studies defining the features of galectins responsible for intracellular carbohydrate-independent interactions, making it difficult to use structural approaches to design druggable targets to modulate intracellular functions.
Given the ability of both extracellular and intracellular galectins to exert immunoregulatory activity, new tools and innovative approaches must be developed to more precisely address the functions of different galectins. These approaches may include studies of tissue-specific conditional knockout mice and methods that allow the examination of the trafficking of endogenous galectins in the extracellular space. They may also include the ex vivo culturing of complex tissues, in conjunction with the use of cell-permeable and impermeable galectin inhibitors147. Indeed, small molecule and antibody-based inhibitors will be critical in determining the relative contribution of extracellular versus intracellular galectin activities in vivo. Although some well-defined small molecule inhibitors of galectin-3, such as GB0139 and GB1107, are now available148, they are known to also inhibit other galectins (for example, galectin-1), albeit with lower efficacy. Similarly, reagents capable of defining the concentration and activity state (given their sensitivity to oxidation and/or proteolytic inactivation) of a given galectin are needed, as current agents are often cross-reactive between different galectin family members and fail to distinguish the distinct activity states of a target galectin.
Despite the challenges in studying galectin activity in vivo, numerous studies continue to implicate galectins in various diseases. The discovery and implementation of tools designed to more accurately define galectin function will not only facilitate their study but may also have translational potential. For example, given the role of galectins in autoimmune diseases and inflammatory diseases, approaches to induce the expression of immunosuppressive galectins, or inhibit pro-inflammatory activities of certain galectins, may prove valuable as a treatment strategy for these diseases146. In contrast, during infection, where augmented immune function may be desirable, inhibiting or enhancing the activity of certain immunosuppressive or immunostimulatory activities of individual galectins may be therapeutically beneficial149. As galectins regulate a wide variety of biological processes, the manipulation of galectin function remains an open and promising area of research.
References
Yoshimura, A., Naka, T. & Kubo, M. SOCS proteins, cytokine signalling and immune regulation. Nat. Rev. Immunol. 7, 454–465 (2007).
Rabinovich, G. A., van Kooyk, Y. & Cobb, B. A. Glycobiology of immune responses. Ann. N. Y. Acad. Sci. 1253, 1–15 (2012).
Cummings, R. D. The repertoire of glycan determinants in the human glycome. Mol. Biosyst. 5, 1087–1104 (2009).
Levi, G., Tarrab-Hazdai, R. & Teichberg, V. I. Prevention and therapy with electrolectin of experimental autoimmune myasthenia gravis in rabbits. Eur. J. Immunol. 13, 500–507 (1983).
Cummings, R. D. et al. in Essentials of Glycobiology (ed. Varki, A.) 4th edn., 491–503 (Cold Spring Harbor Laboratory Press, 2022).
Arthur, C. M., Baruffi, M. D., Cummings, R. D. & Stowell, S. R. Evolving mechanistic insights into galectin functions. Methods Mol. Biol. 1207, 1–35 (2015).
de Waard, A., Hickman, S. & Kornfeld, S. Isolation and properties of β-galactoside binding lectins of calf heart and lung. J. Biol. Chem. 251, 7581–7587 (1976).
Dias-Baruffi, M. et al. Differential expression of immunomodulatory galectin-1 in peripheral leukocytes and adult tissues and its cytosolic organization in striated muscle. Glycobiology 20, 507–520 (2010).
Chen, X. et al. Intestinal epithelial cells express galectin-9 in patients with food allergy that plays a critical role in sustaining allergic status in mouse intestine. Allergy 66, 1038–1046 (2011).
Wada, J., Ota, K., Kumar, A., Wallner, E. I. & Kanwar, Y. S. Developmental regulation, expression, and apoptotic potential of galectin-9, a β-galactoside binding lectin. J. Clin. Invest. 99, 2452–2461 (1997).
Imaizumi, T. et al. Interferon-γ stimulates the expression of galectin-9 in cultured human endothelial cells. J. Leukoc. Biol. 72, 486–491 (2002).
Yang, R. Y. et al. Ablation of a galectin preferentially expressed in adipocytes increases lipolysis, reduces adiposity, and improves insulin sensitivity in mice. Proc. Natl Acad. Sci. USA 108, 18696–18701 (2011).
Kamili, N. A. et al. Key regulators of galectin–glycan interactions. Proteomics 16, 3111–3125 (2016).
Johannes, L., Jacob, R. & Leffler, H. Galectins at a glance. J. Cell. Sci. 131, jcs208884 (2018).
Mendez-Huergo, S. P., Blidner, A. G. & Rabinovich, G. A. Galectins: emerging regulatory checkpoints linking tumor immunity and angiogenesis. Curr. Opin. Immunol. 45, 8–15 (2017).
Ruvolo, P. P. Galectin 3 as a guardian of the tumor microenvironment. Biochim. Biophys. Acta 1863, 427–437 (2016).
Elola, M. T. et al. Galectins: multitask signaling molecules linking fibroblast, endothelial and immune cell programs in the tumor microenvironment. Cell Immunol. 333, 34–45 (2018).
Cardoso, A. C., Andrade, L. N., Bustos, S. O. & Chammas, R. Galectin-3 determines tumor cell adaptive strategies in stressed tumor microenvironments. Front. Oncol. 6, 127 (2016).
Girotti, M. R., Salatino, M., Dalotto-Moreno, T. & Rabinovich, G. A. Sweetening the hallmarks of cancer: galectins as multifunctional mediators of tumor progression. J. Exp. Med. 217, e20182041 (2020).
Hirabayashi, J. et al. Oligosaccharide specificity of galectins: a search by frontal affinity chromatography. Biochim. Biophys. Acta 1572, 232–254 (2002).
Stowell, S. R. et al. Galectin-1, -2, and -3 exhibit differential recognition of sialylated glycans and blood group antigens. J. Biol. Chem. 283, 10109–10123 (2008).
Carlsson, S. et al. Affinity of galectin-8 and its carbohydrate recognition domains for ligands in solution and at the cell surface. Glycobiology 17, 663–676 (2007).
Cooper, D. N. & Barondes, S. H. Evidence for export of a muscle lectin from cytosol to extracellular matrix and for a novel secretory mechanism. J. Cell Biol. 110, 1681–1691 (1990).
Cho, M. & Cummings, R. D. Galectin-1, a β-galactoside-binding lectin in Chinese hamster ovary cells. II. Localization and biosynthesis. J. Biol. Chem. 270, 5207–5212 (1995).
Cerri, D. G. et al. Degeneration of dystrophic or injured skeletal muscles induces high expression of galectin-1. Glycobiology 18, 842–850 (2008).
Banfer, S. et al. Molecular mechanism to recruit galectin-3 into multivesicular bodies for polarized exosomal secretion. Proc. Natl Acad. Sci. USA 115, E4396–E4405 (2018).
Stowell, S. R. et al. Ligand reduces galectin-1 sensitivity to oxidative inactivation by enhancing dimer formation. J. Biol. Chem. 284, 4989–4999 (2009).
Hirabayashi, J. & Kasai, K. Effect of amino acid substitution by sited-directed mutagenesis on the carbohydrate recognition and stability of human 14-kDa β-galactoside-binding lectin. J. Biol. Chem. 266, 23648–23653 (1991).
Teichberg, V. I., Silman, I., Beitsch, D. D. & Resheff, G. A β-d-galactoside binding protein from electric organ tissue of Electrophorus electricus. Proc. Natl Acad. Sci. USA 72, 1383–1387 (1975).
Ochieng, J. et al. Galectin-3 is a novel substrate for human matrix metalloproteinases-2 and -9. Biochemistry 33, 14109–14114 (1994).
Robinson, B. S. et al. The sweet-side of leukocytes: galectins as master regulators of neutrophil function. Front. Immunol. 10, 1762 (2019).
Thiemann, S. & Baum, L. G. Galectins and immune responses — just how do they do those things they do? Annu. Rev. Immunol. 34, 243–264 (2016).
Pereira, M. S. et al. Glycans as key checkpoints of T cell activity and function. Front. Immunol. 9, 2754 (2018).
Gilson, R. C., Gunasinghe, S. D., Johannes, L. & Gaus, K. Galectin-3 modulation of T-cell activation: mechanisms of membrane remodelling. Prog. Lipid Res. 76, 101010 (2019).
Stowell, S. R. et al. Human galectin-1 recognition of poly-N-acetyllactosamine and chimeric polysaccharides. Glycobiology 14, 157–167 (2004).
Demetriou, M., Granovsky, M., Quaggin, S. & Dennis, J. W. Negative regulation of T-cell activation and autoimmunity by Mgat5 N-glycosylation. Nature 409, 733–739 (2001).
Smith, L. K. et al. Interleukin-10 directly inhibits CD8+ T cell function by enhancing N-glycan branching to decrease antigen sensitivity. Immunity 48, 299–312 e295 (2018).
Chen, H. Y. et al. Galectin-3 negatively regulates TCR-mediated CD4+ T-cell activation at the immunological synapse. Proc. Natl Acad. Sci. USA 106, 14496–14501 (2009).
Wang, S. F. et al. Galectin-3 promotes HIV-1 budding via association with Alix and Gag p6. Glycobiology 24, 1022–1035 (2014).
Kaur, M. et al. Galectin-3 regulates γ-herpesvirus specific CD8 T cell immunity. iScience 9, 101–119 (2018).
Chen, H. Y. et al. Intracellular galectin-9 enhances proximal TCR signaling and potentiates autoimmune diseases. J. Immunol. 204, 1158–1172 (2020).
Liang, C. C. et al. Galectin-9 is critical for mucosal adaptive immunity through the T helper 17–IgA axis. Am. J. Pathol. 188, 1225–1235 (2018).
Murali-Krishna, K. et al. Counting antigen-specific CD8 T cells: a reevaluation of bystander activation during viral infection. Immunity 8, 177–187 (1998).
Perillo, N. L., Pace, K. E., Seilhamer, J. J. & Baum, L. G. Apoptosis of T cells mediated by galectin-1. Nature 378, 736–739 (1995).
Toscano, M. A. et al. Differential glycosylation of TH1, TH2 and TH-17 effector cells selectively regulates susceptibility to cell death. Nat. Immunol. 8, 825–834 (2007).
Zhu, C. et al. The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat. Immunol. 6, 1245–1252 (2005).
Pardo, E. et al. Galectin-8 as an immunosuppressor in experimental autoimmune encephalomyelitis and a target of human early prognostic antibodies in multiple sclerosis. PLoS ONE 12, e0177472 (2017).
Sturm, A. et al. Human galectin-2: novel inducer of T cell apoptosis with distinct profile of caspase activation. J. Immunol. 173, 3825–3837 (2004).
Amani, M. F., Rolig, A. S. & Redmond, W. L. Intracellular galectin-3 is essential for OX40-mediated memory CD8+ T cell development. J. Immunol. 205, 1857–1866 (2020).
Yang, R. Y., Hsu, D. K. & Liu, F. T. Expression of galectin-3 modulates T-cell growth and apoptosis. Proc. Natl Acad. Sci. USA 93, 6737–6742 (1996).
Hernandez, J. D. & Baum, L. G. Ah, sweet mystery of death! Galectins and control of cell fate. Glycobiology 12, 127R–136R (2002).
Reddy, P. B. et al. Influence of galectin-9/Tim-3 interaction on herpes simplex virus-1 latency. J. Immunol. 187, 5745–5755 (2011).
Oliveira, F. L. et al. Lack of galectin-3 up-regulates IgA expression by peritoneal B1 lymphocytes during B cell differentiation. Cell Tissue Res. 363, 411–426 (2016).
Giovannone, N., Smith, L. K., Treanor, B. & Dimitroff, C. J. Galectin–glycan interactions as regulators of B cell immunity. Front. Immunol. 9, 2839 (2018).
Giovannone, N. et al. Galectin-9 suppresses B cell receptor signaling and is regulated by I-branching of N-glycans. Nat. Commun. 9, 3287 (2018).
Cao, A. et al. Galectin-9 binds IgM-BCR to regulate B cell signaling. Nat. Commun. 9, 3288 (2018).
Smith, L. K., Fawaz, K. & Treanor, B. Galectin-9 regulates the threshold of B cell activation and autoimmunity. eLife 10, e64557 (2021).
Tsai, C. M. et al. Galectin-1 and galectin-8 have redundant roles in promoting plasma cell formation. J. Immunol. 187, 1643–1652 (2011).
Beccaria, C. G. et al. Galectin-3 deficiency drives lupus-like disease by promoting spontaneous germinal centers formation via IFN-γ. Nat. Commun. 9, 1628 (2018).
Liu, F. T., Yang, R. Y. & Hsu, D. K. Galectins in acute and chronic inflammation. Ann. N. Y. Acad. Sci. 1253, 80–91 (2012).
Sato, S., St-Pierre, C., Bhaumik, P. & Nieminen, J. Galectins in innate immunity: dual functions of host soluble β-galactoside-binding lectins as damage-associated molecular patterns (DAMPs) and as receptors for pathogen-associated molecular patterns (PAMPs). Immunol. Rev. 230, 172–187 (2009).
Rabinovich, G. A. & Toscano, M. A. Turning ‘sweet’ on immunity: galectin–glycan interactions in immune tolerance and inflammation. Nat. Rev. Immunol. 9, 338–352 (2009).
Henderson, N. C. & Sethi, T. The regulation of inflammation by galectin-3. Immunol. Rev. 230, 160–171 (2009).
Sato, S. in Comprehensive Glycoscience Vol. 5 (ScienceDirect, 2021).
Sato, S. & Nieminen, J. Seeing strangers or announcing “danger”: galectin-3 in two models of innate immunity. Glycoconj. J. 19, 583–591 (2002).
Blois, S. M. et al. A pivotal role for galectin-1 in fetomaternal tolerance. Nat. Med. 13, 1450–1457 (2007).
Ilarregui, J. M. et al. Tolerogenic signals delivered by dendritic cells to T cells through a galectin-1-driven immunoregulatory circuit involving interleukin 27 and interleukin 10. Nat. Immunol. 10, 981–991 (2009).
Martinez Allo, V. C. et al. Suppression of age-related salivary gland autoimmunity by glycosylation-dependent galectin-1-driven immune inhibitory circuits. Proc. Natl Acad. Sci. USA 117, 6630–6639 (2020).
Fermin Lee, A. et al. Galectin-3 modulates TH17 responses by regulating dendritic cell cytokines. Am. J. Pathol. 183, 1209–1222 (2013).
Jiang, H. R. et al. Galectin-3 deficiency reduces the severity of experimental autoimmune encephalomyelitis. J. Immunol. 182, 1167–1173 (2009).
Fermino, M. L. et al. Lack of galectin-3 increases Jagged1/Notch activation in bone marrow-derived dendritic cells and promotes dysregulation of T helper cell polarization. Mol. Immunol. 76, 22–34 (2016).
Mobergslien, A. & Sioud, M. Galectin-1 and -3 gene silencing in immature and mature dendritic cells enhances T cell activation and interferon-gamma production. J. Leukoc. Biol. 91, 461–467 (2012).
Volarevic, V. et al. Galectin-3 deficiency prevents concanavalin A-induced hepatitis in mice. Hepatology 55, 1954–1964 (2012).
Simovic Markovic, B. et al. Galectin-3 plays an important pro-inflammatory role in the induction phase of acute colitis by promoting activation of NLRP3 inflammasome and production of IL-1β in macrophages. J. Crohns Colitis 10, 593–606 (2016).
Tian, J. et al. Galectin-3 regulates inflammasome activation in cholestatic liver injury. FASEB J. 30, 4202–4213 (2016).
Arsenijevic, A. et al. Gal-3 Deficiency suppresses Novosphyngobium aromaticivorans inflammasome activation and IL-17 driven autoimmune cholangitis in mice. Front. Immunol. 10, 1309 (2019).
Wang, W. et al. Galectin-9 targets NLRP3 for autophagic degradation to limit inflammation. J. Immunol. 206, 2692–2699 (2021).
MacKinnon, A. C. et al. Regulation of alternative macrophage activation by galectin-3. J. Immunol. 180, 2650–2658 (2008).
Shirakawa, K. et al. IL (Interleukin)-10–STAT3–galectin-3 axis is essential for osteopontin-producing reparative macrophage polarization after myocardial infarction. Circulation 138, 2021–2035 (2018).
Xue, H., Yang, R. Y., Tai, G. & Liu, F. T. Galectin-12 inhibits granulocytic differentiation of human NB4 promyelocytic leukemia cells while promoting lipogenesis. J. Leukoc. Biol. 100, 657–664 (2016).
Wan, L. et al. Galectin-12 enhances inflammation by promoting M1 polarization of macrophages and reduces insulin sensitivity in adipocytes. Glycobiology 26, 732–744 (2016).
Sano, H. et al. Critical role of galectin-3 in phagocytosis by macrophages. J. Clin. Invest. 112, 389–397 (2003).
Reichert, F. & Rotshenker, S. Galectin-3 (MAC-2) controls microglia phenotype whether amoeboid and phagocytic or branched and non-phagocytic by regulating the cytoskeleton. Front. Cell Neurosci. 13, 90 (2019).
Querol Cano, L. et al. Intracellular Galectin-9 controls dendritic cell function by maintaining plasma membrane rigidity. iScience 22, 240–255 (2019).
Shi, Z. R. et al. Decrease of galectin-3 in keratinocytes: a potential diagnostic marker and a critical contributor to the pathogenesis of psoriasis. J. Autoimmun. 89, 30–40 (2018).
Chen, H. L. et al. Galectin-7 downregulation in lesional keratinocytes contributes to enhanced IL-17A signaling and skin pathology in psoriasis. J. Clin. Invest. 131, e130740 (2021).
Nieminen, J., St-Pierre, C., Bhaumik, P., Poirier, F. & Sato, S. Role of galectin-3 in leukocyte recruitment in a murine model of lung infection by Streptococcus pneumoniae. J. Immunol. 180, 2466–2473 (2008).
Snarr, B. D. et al. Galectin-3 enhances neutrophil motility and extravasation into the airways during Aspergillus fumigatus infection. PLoS Pathog. 16, e1008741 (2020).
Farnworth, S. L. et al. Galectin-3 reduces the severity of pneumococcal pneumonia by augmenting neutrophil function. Am. J. Pathol. 172, 395–405 (2008).
Humphries, D. C. et al. Selective myeloid depletion of galectin-3 offers protection against acute and chronic lung injury. Front. Pharmacol. 12, 715986 (2021).
Bhaumik, P., St-Pierre, G., Milot, V., St-Pierre, C. & Sato, S. Galectin-3 facilitates neutrophil recruitment as an innate immune response to a parasitic protozoa cutaneous infection. J. Immunol. 190, 630–640 (2013).
Zuberi, R. I. et al. Critical role for galectin-3 in airway inflammation and bronchial hyperresponsiveness in a murine model of asthma. Am. J. Pathol. 165, 2045–2053 (2004).
Ge, X. N. et al. Allergen-induced airway remodeling is impaired in galectin-3-deficient mice. J. Immunol. 185, 1205–1214 (2010).
Ge, X. N. et al. Regulation of eosinophilia and allergic airway inflammation by the glycan-binding protein galectin-1. Proc. Natl Acad. Sci. USA 113, E4837–E4846 (2016).
James, R. E. et al. Loss of galectin-3 decreases the number of immune cells in the subventricular zone and restores proliferation in a viral model of multiple sclerosis. Glia 64, 105–121 (2016).
Montespan, C. et al. Multi-layered control of galectin-8 mediated autophagy during adenovirus cell entry through a conserved PPxY motif in the viral capsid. PLoS Pathog. 13, e1006217 (2017).
Machado, F. C. et al. Recruitment of galectin-3 during cell invasion and intracellular trafficking of Trypanosoma cruzi extracellular amastigotes. Glycobiology 24, 179–184 (2014).
Pascua-Maestro, R., Diez-Hermano, S., Lillo, C., Ganfornina, M. D. & Sanchez, D. Protecting cells by protecting their vulnerable lysosomes: identification of a new mechanism for preserving lysosomal functional integrity upon oxidative stress. PLoS Genet. 13, e1006603 (2017).
Hung Y. H. et al. Spatiotemporally controlled induction of autophagy-mediated lysosome turnover. Nat. Commun. 4, 2111 (2013).
Munson, M. J. et al. A high-throughput galectin-9 imaging assay for quantifying nanoparticle uptake, endosomal escape and functional RNA delivery. Commun. Biol. 4, 211 (2021).
Weng, I. C. et al. Cytosolic galectin-3 and -8 regulate antibacterial autophagy through differential recognition of host glycans on damaged phagosomes. Glycobiology 28, 392–405 (2018).
Aits, S. et al. Sensitive detection of lysosomal membrane permeabilization by lysosomal galectin puncta assay. Autophagy 11, 1408–1424 (2015).
Chauhan, S. et al. TRIMs and galectins globally cooperate and TRIM16 and galectin-3 co-direct autophagy in endomembrane damage homeostasis. Dev. Cell 39, 13–27 (2016).
Kimura, T. et al. Dedicated SNAREs and specialized TRIM cargo receptors mediate secretory autophagy. EMBO J. 36, 42–60 (2017).
Jia, J. et al. Galectin-3 coordinates a cellular system for lysosomal repair and removal. Dev. Cell 52, 69–87.e8 (2020).
Jia, J. et al. Galectins control mTOR in response to endomembrane damage. Mol. Cell 70, 120–135.e8 (2018).
Jia, J. et al. AMPK, a regulator of metabolism and autophagy, is activated by lysosomal damage via a novel galectin-directed ubiquitin signal transduction system. Mol. Cell 77, 951–969.e9 (2020).
Stowell, S. R. et al. Innate immune lectins kill bacteria expressing blood group antigen. Nat. Med. 16, 295–301 (2010).
Park, A. M., Hagiwara, S., Hsu, D. K., Liu, F. T. & Yoshie, O. Galectin-3 plays an important role in innate immunity to gastric infection by Helicobacter pylori. Infect. Immun. 84, 1184–1193 (2016).
Ferrer, M. F. et al. Macrophages and galectin 3 control bacterial burden in acute and subacute murine leptospirosis that determines chronic kidney fibrosis. Front. Cell Infect. Microbiol. 8, 384 (2018).
Quattroni, P. et al. Galectin-3 binds Neisseria meningitidis and increases interaction with phagocytic cells. Cell. Microbiol. 14, 1657–1675 (2012).
Fowler, M., Thomas, R. J., Atherton, J., Roberts, I. S. & High, N. J. Galectin-3 binds to Helicobacter pylori O-antigen: it is upregulated and rapidly secreted by gastric epithelial cells in response to H. pylori adhesion. Cell Microbiol. 8, 44–54 (2006).
Tana, F. L. et al. Galectin-3 regulates proinflammatory cytokine function and favours Brucella abortus chronic replication in macrophages and mice. Cell Microbiol. 23, e13375 (2021).
Ferraz, L. C. et al. Lack of galectin-3 alters the balance of innate immune cytokines and confers resistance to Rhodococcus equi infection. Eur. J. Immunol. 38, 2762–2775 (2008).
Paz, I. et al. Galectin-3, a marker for vacuole lysis by invasive pathogens. Cell Microbiol. 12, 530–544 (2010).
Feeley, E. M. et al. Galectin-3 directs antimicrobial guanylate binding proteins to vacuoles furnished with bacterial secretion systems. Proc. Natl Acad. Sci. USA 114, E1698–E1706 (2017).
Thurston, T. L., Wandel, M. P., von Muhlinen, N., Foeglein, A. & Randow, F. Galectin 8 targets damaged vesicles for autophagy to defend cells against bacterial invasion. Nature 482, 414–418 (2012).
Li, S. et al. Sterical hindrance promotes selectivity of the autophagy cargo receptor NDP52 for the danger receptor galectin-8 in antibacterial autophagy. Sci. Signal. 6, ra9 (2013).
Stowell, S. R. et al. Dimeric galectin-8 induces phosphatidylserine exposure in leukocytes through polylactosamine recognition by the C-terminal domain. J. Biol. Chem. 283, 20547–20559 (2008).
Hong, M. H. et al. Intracellular galectins control cellular responses commensurate with cell surface carbohydrate composition. Glycobiology 30, 49–57 (2019).
Lin, C. Y. et al. Autophagy receptor Tollip facilitates bacterial autophagy by recruiting galectin-7 in response to group A streptococcus infection. Front. Cell Infect. Microbiol. 10, 583137 (2020).
Bell, S. L., Lopez, K. L., Cox, J. S., Patrick, K. L. & Watson, R. O. Galectin-8 senses phagosomal damage and recruits selective autophagy adapter TAX1BP1 to control Mycobacterium tuberculosis infection in macrophages. mBio 12, e0187120 (2021).
Palframan, S. L., Kwok, T. & Gabriel, K. Vacuolating cytotoxin A (VacA), a key toxin for Helicobacter pylori pathogenesis. Front. Cell Infect. Microbiol. 2, 92 (2012).
Li, F. Y. et al. Helicobacter pylori induces intracellular galectin-8 aggregation around damaged lysosomes within gastric epithelial cells in a host O-glycan-dependent manner. Glycobiology 29, 151–162 (2019).
Chen, Y. J. et al. Galectin-3 enhances avian H5N1 influenza A virus-induced pulmonary inflammation by promoting NLRP3 inflammasome activation. Am. J. Pathol. 188, 1031–1042 (2018).
Stojanovic, B. et al. Galectin-3 deficiency facilitates TNF-α-dependent hepatocyte death and liver inflammation in MCMV infection. Front. Microbiol. 10, 185 (2019).
Markovic, S. S. et al. Galectin-1 as the new player in staging and prognosis of COVID-19. Sci. Rep. 12, 1272 (2022).
Cervantes-Alvarez, E. et al. Galectin-3 as a potential prognostic biomarker of severe COVID-19 in SARS-CoV-2 infected patients. Sci. Rep. 12, 1856 (2022).
Bozorgmehr, N. et al. Galectin-9, a player in cytokine release syndrome and a surrogate diagnostic biomarker in SARS-CoV-2 infection. mBio 12, e00384-21 (2021).
Caniglia, J. L., Asuthkar, S., Tsung, A. J., Guda, M. R. & Velpula, K. K. Immunopathology of galectin-3: an increasingly promising target in COVID-19. F1000Res 9, 1078 (2020).
Wu, S. C. et al. The SARS-CoV-2 receptor-binding domain preferentially recognizes blood group A. Blood Adv. 5, 1305–1309 (2021).
Nguyen, L. et al. Sialic acid-containing glycolipids mediate binding and viral entry of SARS-CoV-2. Nat. Chem. Biol. 18, 81–90 (2022).
Wu, S. Y. et al. Cell intrinsic galectin-3 attenuates neutrophil ROS-dependent killing of Candida by modulating CR3 downstream Syk activation. Front. Immunol. 8, 48 (2017).
Wu, S. Y., Yu, J. S., Liu, F. T., Miaw, S. C. & Wu-Hsieh, B. A. Galectin-3 negatively regulates dendritic cell production of IL-23/IL-17-axis cytokines in infection by Histoplasma capsulatum. J. Immunol. 190, 3427–3437 (2013).
Linden, J. R., De Paepe, M. E., Laforce-Nesbitt, S. S. & Bliss, J. M. Galectin-3 plays an important role in protection against disseminated candidiasis. Med. Mycol. 51, 641–651 (2013).
Almeida, F. et al. Galectin-3 impacts Cryptococcus neoformans infection through direct antifungal effects. Nat. Commun. 8, 1968 (2017).
Rodrigues, L. C. et al. Protective effect of galectin-1 during Histoplasma capsulatum infection is associated with prostaglandin E2 and nitric oxide modulation. Mediators Inflamm. 2016, 5813794 (2016).
Oliveira, R. M. et al. Galectin-3 plays a protective role in Leishmania (Leishmania) amazonensis infection. Glycobiology 31, 1378–1389 (2021).
Fermino, M. L. et al. Galectin-3 negatively regulates the frequency and function of CD4+CD25+Foxp3+ regulatory T cells and influences the course of Leishmania major infection. Eur. J. Immunol. 43, 1806–1817 (2013).
Quenum Zangbede, F. O., Chauhan, A., Sharma, J. & Mishra, B. B. Galectin-3 in M2 macrophages plays a protective role in resolution of neuropathology in brain parasitic infection by regulating neutrophil turnover. J. Neurosci. 38, 6737–6750 (2018).
Bernardes, E. S. et al. Toxoplasma gondii infection reveals a novel regulatory role for galectin-3 in the interface of innate and adaptive immunity. Am. J. Pathol. 168, 1910–1920 (2006).
Pineda, M. A., Cuervo, H., Fresno, M., Soto, M. & Bonay, P. Lack of galectin-3 prevents cardiac fibrosis and effective immune responses in a murine model of Trypanosoma cruzi infection. J. Infect. Dis. 212, 1160–1171 (2015).
da Silva, A. A. et al. Galectin-3: a friend but not a foe during Trypanosoma cruzi experimental infection. Front. Cell Infect. Microbiol. 7, 463 (2017).
Poncini, C. V. et al. Trypanosoma cruzi infection imparts a regulatory program in dendritic cells and T cells via galectin-1-dependent mechanisms. J. Immunol. 195, 3311–3324 (2015).
Nabi, I. R., Shankar, J. & Dennis, J. W. The galectin lattice at a glance. J. Cell Sci. 128, 2213–2219 (2015).
Hirani, N. et al. Target inhibition of galectin-3 by inhaled TD139 in patients with idiopathic pulmonary fibrosis. Eur. Respir. J. 57, 2002559 (2021).
Stegmayr, J. et al. Extracellular and intracellular small-molecule galectin-3 inhibitors. Sci. Rep. 9, 2186 (2019).
Slack, R. J., Mills, R. & Mackinnon, A. C. The therapeutic potential of galectin-3 inhibition in fibrotic disease. Int. J. Biochem. Cell Biol. 130, 105881 (2021).
Sehrawat, S. et al. Galectin-9/TIM-3 interaction regulates virus-specific primary and memory CD8 T cell response. PLoS Pathog. 6, e1000882 (2010).
Davicino, R. C. et al. Galectin-1-driven tolerogenic programs aggravate Yersinia enterocolitica infection by repressing antibacterial immunity. J. Immunol. 199, 1382–1392 (2017).
Bunn, P. T. et al. Galectin-1 impairs the generation of anti-parasitic TH1 cell responses in the liver during experimental visceral leishmaniasis. Front. Immunol. 8, 1307 (2017).
Poncini, C. V. et al. Trypanosoma cruzi infection imparts a regulatory program in dendritic cells and T cells via galectin-1-dependent mechanisms. J. Immunol. 195, 3311–3324 (2015).
Bertelli, A. et al. Anti-inflammatory role of galectin-8 during Trypanosoma cruzi chronic infection. Front. Cell Infect. Microbiol. 10, 285 (2020).
Straube, T. et al. pH-dependent recycling of galectin-3 at the apical membrane of epithelial cells. Traffic 14, 1014–1027 (2013).
Lakshminarayan, R. et al. Galectin-3 drives glycosphingolipid-dependent biogenesis of clathrin-independent carriers. Nat. Cell Biol. 16, 595–606 (2014).
Honig, E., Schneider, K. & Jacob, R. Recycling of galectin-3 in epithelial cells. Eur. J. Cell Biol. 94, 309–315 (2015).
Renard, H. F. et al. Endophilin-A3 and galectin-8 control the clathrin-independent endocytosis of CD166. Nat. Commun. 11, 1457 (2020).
Ivashenka, A. et al. Glycolipid-dependent and lectin-driven transcytosis in mouse enterocytes. Commun. Biol. 4, 173 (2021).
Jiang, P., Gan, M., Yen, S. H., McLean, P. J. & Dickson, D. W. Impaired endo-lysosomal membrane integrity accelerates the seeding progression of α-synuclein aggregates. Sci. Rep. 7, 7690 (2017).
Burbidge, K. et al. LGALS3 (galectin 3) mediates an unconventional secretion of SNCA/α-synuclein in response to lysosomal membrane damage by the autophagic–lysosomal pathway in human midbrain dopamine neurons. Autophagy 18, 1020–1048 (2021).
Siew, J. J. et al. Galectin-3 is required for the microglia-mediated brain inflammation in a model of Huntington’s disease. Nat. Commun. 10, 3473 (2019).
Vasta, G. R. Roles of galectins in infection. Nat. Rev. Microbiol. 7, 424–438 (2009).
Robinson, B., Arthur, C. M., Kamili, N. A. & Stowell, S. R. Galectin regulation of host microbial interactions. Trends Glycosci. Glycotechnol. 30, SE185–SE198 (2018).
Mey, A., Leffler, H., Hmama, Z., Normier, G. & Revillard, J. P. The animal lectin galectin-3 interacts with bacterial lipopolysaccharides via two independent sites. J. Immunol. 156, 1572–1577 (1996).
Nita-Lazar, M. et al. Desialylation of airway epithelial cells during influenza virus infection enhances pneumococcal adhesion via galectin binding. Mol. Immunol. 65, 1–16 (2015).
Lujan, A. L. et al. Glycosylation-dependent galectin-receptor interactions promote Chlamydia trachomatis infection. Proc. Natl Acad. Sci. USA 115, E6000–E6009 (2018).
Stowell, S. R. et al. Microbial glycan microarrays define key features of host–microbial interactions. Nat. Chem. Biol. 10, 470–476 (2014).
Stechly, L. et al. Galectin-4-regulated delivery of glycoproteins to the brush border membrane of enterocyte-like cells. Traffic 10, 438–450 (2009).
Lindstedt, R., Apodaca, G., Barondes, S. H., Mostov, K. E. & Leffler, H. Apical secretion of a cytosolic protein by Madin–Darby canine kidney cells. Evidence for polarized release of an endogenous lectin by a nonclassical secretory pathway. J. Biol. Chem. 268, 11750–11757 (1993).
Sato, S., Burdett, I. & Hughes, R. C. Secretion of the baby hamster kidney 30-kDa galactose-binding lectin from polarized and nonpolarized cells: a pathway independent of the endoplasmic reticulum–Golgi complex. Exp. Cell Res. 207, 8–18 (1993).
Vasta, G. R. Galectins as pattern recognition receptors: structure, function, and evolution. Adv. Exp. Med. Biol. 946, 21–36 (2012).
Kohatsu, L., Hsu, D. K., Jegalian, A. G., Liu, F. T. & Baum, L. G. Galectin-3 induces death of Candida species expressing specific β-1,2-linked mannans. J. Immunol. 177, 4718–4726 (2006).
Lo, T. H. et al. Galectin-3 promotes noncanonical inflammasome activation through intracellular binding to lipopolysaccharide glycans. Proc. Natl Acad. Sci. USA 118, e2026246118 (2021).
Acknowledgements
This work was supported, in part, by the Ministry of Science and Technology Thematic Progam, the Academia Sinica Thematic Program and the Academia Sinica Summit Program to F.-T.L., as well as the Burroughs Wellcome Trust Career Award for Medical Scientists and the National Institutes of Health (NIH) U01 CA242109 and DP5 OD019892 to S.R.S. The authors thank C. Arthur, H. Verkerke, A. Paul, P. Wu and H.-L. Chen for helpful discussion, and C.-S. Li and W.-H. Lin for preparation of the illustrations. They are grateful to C. Bevins at UC Davis for reading the manuscript and making many valuable comments and suggestions.
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to this Review.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Immunology thanks Sachiko Sato, Gerardo Vasta and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, FT., Stowell, S.R. The role of galectins in immunity and infection. Nat Rev Immunol 23, 479–494 (2023). https://doi.org/10.1038/s41577-022-00829-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41577-022-00829-7
This article is cited by
-
The intracellular interplay between galectin-1 and FGF12 in the assembly of ribosome biogenesis complex
Cell Communication and Signaling (2024)
-
Membrane organization by tetraspanins and galectins shapes lymphocyte function
Nature Reviews Immunology (2024)
-
Balancing Act of the Intestinal Antimicrobial Proteins on Gut Microbiota and Health
Journal of Microbiology (2024)
-
Plasma Proteomic Analysis Based on 4D-DIA Evaluates the Clinical Response to Imrecoxib in the Early Treatment of Osteoarthritis
Rheumatology and Therapy (2024)
-
Macrophage-driven cardiac inflammation and healing: insights from homeostasis and myocardial infarction
Cellular & Molecular Biology Letters (2023)