Abstract
IgGs are essential soluble components of the adaptive immune response that evolved to protect the body from infection. Compared with other immunoglobulins, the role of IgGs is distinguished and enhanced by their high circulating levels, long half-life and ability to transfer from mother to offspring, properties that are conferred by interactions with neonatal Fc receptor (FcRn). FcRn binds to the Fc portion of IgGs in a pH-dependent manner and protects them from intracellular degradation. It also allows their transport across polarized cells that separate tissue compartments, such as the endothelium and epithelium. Further, it is becoming apparent that FcRn functions to potentiate cellular immune responses when IgGs, bound to their antigens, form IgG immune complexes. Besides the protective role of IgG, IgG autoantibodies are associated with numerous pathological conditions. As such, FcRn blockade is a novel and effective strategy to reduce circulating levels of pathogenic IgG autoantibodies and curtail IgG-mediated diseases, with several FcRn-blocking strategies on the path to therapeutic use. Here, we describe the current state of knowledge of FcRn–IgG immunobiology, with an emphasis on the functional and pathological aspects, and an overview of FcRn-targeted therapy development.
Similar content being viewed by others
Introduction
Antibodies, or immunoglobulins, are an inherent part of vertebrate humoral immune responses. On the one hand, the extreme variability of the antigen-binding fragment (Fab) domain enables antibodies to specifically recognize an almost infinite number of epitopes. On the other hand, the “constant” crystallizable fragment (Fc) domain allows them to engage with various soluble and cellular molecules, such as components of the complement pathway or Fc receptors (FcRs), and to trigger highly tailored immune responses. In mammals, different Fc domains have evolved that correspond to specific immunoglobulin classes, namely IgA, IgD, IgE, IgG and IgM1. Similarly, numerous receptors also emerged that engage and provide specialized characteristics to each of these immunoglobulin classes. IgGs, the most prevalent antibody class, have unique features that are attributable to their interaction with neonatal Fc receptor (FcRn). FcRn is responsible for the transfer of IgGs from mother to offspring and across mucosal surfaces, in addition to maintaining high concentrations and a long half-life of this class of antibody in the circulation. Although Fc receptors for IgG (FcγRs) are crucial to IgG effector functions2, the role of FcRn in responding to IgG immune complexes (IgG-ICs) has been gaining attention. FcRn is distinctively and directly involved in innate and adaptive immune responses to IgG-ICs, beyond its better-known role in the prevention of IgG catabolism. The important advances in the FcRn field over the past century (Supplementary Fig. 1) have allowed for the translation of these studies into the therapeutic age of FcRn. Here, we discuss the biology of FcRn in the immune response, in addition to its roles in protection against infectious diseases and cancer, and in the promotion of autoimmunity, with a focus on the advances in clinical trials for FcRn-blocking therapeutics. Although FcRn is also a receptor for albumin, we only discuss this briefly and refer the reader to other excellent reviews on this topic3,4.
Basic concepts of FcRn biology
From FCGRT to FcRn
In humans, the FcRn heavy chain is encoded by the Fcγ receptor and transporter (FCGRT) gene, located on chromosome 19q13.35. The gene contains seven exons and six introns, with exons 2–5 encoding the signal sequence and extracellular α1-α2-α3 domains, exon 6 encoding the transmembrane domain and exon 7 encoding the cytoplasmic tail6. FCGRT orthologues exist in most mammalian and marsupial species and the encoded proteins display high amino acid conservation with the human receptor, although in some species (ruminants, pigs, dogs, rabbits) deletions of 5–10 amino acids in the cytoplasmic tail have been described7. The α1-α2-α3 domains of FcRn share high structural homology with MHC class I molecules and non-covalently associate with β2-microglobulin (β2m), forming a heterodimer8,9,10,11 (Fig. 1a). Unlike the high genetic variability observed in some FcγRs and MHC class I molecules, FCGRT is predominantly monomorphic with variability that is limited to its promoter in the form of variable number of tandem repeats (VNTRs)12 (Box 1). Further, contrary to MHC class I molecules, the FcRn peptide binding groove is occluded, preventing it from presenting peptides10,13. Despite this, FcRn biogenesis involves the endoplasmic reticulum chaperones used by MHC class I molecules in its assembly and interactions with elements of the MHC class II pathway, such as the invariant chain, indicating the unique nature of FcRn function14,15.
a, Ribbon diagram of the human neonatal Fc receptor (FcRn) heavy chain (red) with indicated α1, α2 and α3 domains, and β2-microglobulin (β2m; blue) light chain (Protein Data Bank (PDB) ID 1EXU). b, Ternary complex between human FcRn, human albumin (purple) and portion of human IgG1 Fc fragment (cyan) (PDB ID 4N0U). Albumin and half of the IgG1 Fc in ribbon and surface diagrams are shown with the indicated domains: albumin domains I (DI, purple), II (DII, light purple) and III (DIII, dark purple), and IgG1 Fc domains CH2 and CH3. Bottom-right inset box shows FcRn residues E115, E116, D130 and E133 binding with Fc residues H310 and H435 (not shown). Bottom-left inset box shows that, at acidic pH, the presence of H166 leads to intramolecular hydrogen bonding, which facilitates optimal binding of human FcRn residues W53 and W59 with albumin. Human FcRn residues S58 (not shown), N149 and H161 make various hydrogen-bonded interactions with albumin DI whereas FcRn residues W53 and W59 engage albumin DIII. c, Cartoon representation of two FcRn–β2m heterodimers engaging monomeric IgG (in a T conformation), which presumably occurs on the membrane of acidified recycling endosomes. A short stalk, the transmembrane domain and the cytoplasmic domain are also depicted. Fab, antigen-binding fragment.
FcRn cellular distribution and regulation of expression
FcRn is expressed beyond the neonatal stage, in adult life, and is widely present throughout human body tissues, including parenchymal (epithelium, endothelium, hepatocytes and keratinocytes) and haematopoietic cell types16,17,18,19,20,21. The list of cells, tissues and organs that express FcRn is rapidly expanding (Supplementary Fig. 2), with gaps in our knowledge of FcRn’s function in many cells and tissues remaining20,21,22 (https://www.proteinatlas.org/ENSG00000104870-FCGRT/single+cell+type). Within the immune compartment, FcRn expression is especially high in myeloid cells such as monocytes, tissue-resident macrophages, dendritic cells (DCs) and neutrophils; in lymphocytes, low levels of FcRn are present in B cells but no FcRn expression has been detected in T cells or natural killer (NK) cells20,21,23,24. FcRn is mostly distributed intracellularly within vesicular networks, particularly in acidic endosomes, that allow for interactions with IgG and albumin; it is also present at the cell surface, especially in monocytes, macrophages, DCs and neutrophils20,24. The precise role of surface FcRn on these cell subsets is unclear.
FcRn expression is regulated by factors such as cytokines or infectious stimuli, with many transcription factor binding sites identified in FCGRT. FcRn expression is rapidly increased by tumour necrosis factor (TNF) stimulation of intestinal epithelial cell lines, human primary monocytes and the THP-1 monocytic cell line, and depends on NF-κB binding to FCGRT introns25. The Toll-like receptor agonists lipopolysaccharide and CpG oligodeoxynucleotides also increase FcRn expression in THP-1 cells, which is also probably due to NF-κB activation25. Transforming growth factor β1 (TGFβ1) promotes FcRn expression in porcine intestinal epithelial cells through JUN N-terminal kinase (JNK) activation and c-JUN transcription factor binding to the FCGRT promoter26. Similarly, transmissible gastroenteritis virus infection upregulates FcRn expression in porcine intestinal epithelial cells through NF-κB, which has four binding sites in the FcRn promoter, and Zika virus infection in pregnant mice upregulates FcRn expression in the placenta27,28. Conversely, FcRn expression can be downregulated by interferon-γ (IFNγ)-mediated JAK–STAT1 signalling in epithelial cells, THP-1 cells and human peripheral blood mononuclear cells, with multiple possible mechanisms of downregulation, including STAT1 binding to an IFNγ activation site in the FCGRT promoter region29. Overall, more investigation is needed to thoroughly explore the regulation of FcRn expression in the panoply of immune and non-immune cell subsets that express it.
FcRn–ligand interactions
FcRn engagement of the IgG Fc occurs at the CH3 and CH2 domain interface, with the Fab arms directed towards the membrane10,11,30,31,32 (Fig. 1b,c). This binding involves Fc residues I253, T254, H310, H433 and H435, which mediate various hydrogen-bonded and salt bridge interactions with E115 and D130 on human FcRn32,33 (Fig. 1b). The presence of imidazole side chains on histidine provides a pH-dependent switch whereby at pH 5–6 the group is positively charged, allowing for FcRn–IgG interaction, whereas at pH 7.4 it is neutral and the binding is lost33,34,35. In addition to the variability that exists within a given species at the level of IgG subclasses, allotypes, glycosylation or different Fab arms, mammalian FcRn and IgG orthologues have subtle amino acid differences that are the basis for the range of binding affinities observed within and between different species36,37,38. Notable examples are the lower binding affinity of human FcRn to human IgG3 (due to the presence of R435 instead of H435) and the inability of human FcRn to engage most mouse IgGs (except for weak binding to IgG2b)36,39. Adding further complexity is the fact that IgGs also bind antigens and interact with other receptors: for instance, the FcRn binding site for IgGs and the cytoplasmic Fc receptor tripartite motif containing 21 (TRIM21) overlap with each other40. In contrast, classical FcγRs bind to IgG at a distinct site41, such that IgG can potentially engage both FcRn and FcγRs simultaneously42,43. Guided by this knowledge, IgG Fc engineering has allowed the development of IgG variants with different binding affinities to FcRn at acidic or neutral pH to enhance FcRn binding for extending IgG half-life (Box 2 and reviewed in44) or forcing the degradation of IgG antibodies; the best example is the IgG1MST-HN variant, also known as IgG1YTE-KF (M252Y/S254T/T256E/H433K/N434F), which has substantially higher binding to FcRn at acidic pH and retains binding at neutral pH45, and is also known as an antibody that enhances IgG degradation (Abdeg). Indeed, the Fc fragment derived from this Abdeg, known as efgartigimod, is the first FcRn antagonist approved by the US Food and Drug Administration (FDA) (see below).
As IgG is a heterotetramer, two FcRn molecules can engage a single IgG46,47, and physiological FcRn–IgG interactions are believed to occur at a 2:1 ratio48,49 (Fig. 1c). Recently, through the use of negative stain electron microscopy, 2:1 receptor–ligand complexes were observed in which the Fab arms had a T-shaped or a mixed Y/T-shaped conformation (relative to FcRn)50. Whether the Fab arms can come in direct contact with FcRn has not been shown, although they certainly affect FcRn binding51,52,53,54,55,56. The evidence for such influences arose from observations that monoclonal antibodies possessing identical Fc domains yet distinct Fab domains exhibit different affinities for FcRn, resulting in modifications of their half-life51,52. Explanations for these “long-distance perturbations” are still emerging, with studies indicating that these effects may be mediated by differences in the distribution of the positive charges in the Fab domains53,54,56,57 and/or allosteric effects50,55.
FcRn also engages albumin in a pH-dependent manner58 (Box 3) and more recently has been described as a pH-independent receptor for two members of the Enterovirus B family: echoviruses and coxsackievirus A959,60,61 (Box 4).
Physiological functions of FcRn
The pH-dependent ligand binding is crucial for FcRn’s passive and active immune functions. The passive functions involve recycling and transcytosis, which allow FcRn to salvage monomeric IgG from intracellular degradation and to transport it across cell layers; the active functions involve IgG-IC engagement and enhancement of innate and adaptive immunity.
Passive immune functions
FcRn as a recycling receptor
IgGs have a remarkably long half-life compared to other antibody isotypes. Although β2m-deficient mice (B2m−/−) were initially used to illustrate the role of FcRn as an IgG recycling receptor62,63,64, the first direct evidence for FcRn’s involvement in the recycling of IgGs and prevention of catabolism was described in 2003, upon generation of FcRn-deficient mice (Fcgrt−/−)65. FcRn ablation resulted in significantly lower levels of serum IgG1, IgG2a, IgG2b and IgG3 (mice notably lack IgG4, which is specific to humans), with no differences in the levels of IgA and IgM65. The half-life of IgG1 is 9 days in wild type mice, whereas in FcRn-deficient mice it is dramatically lower at only ~1.4 days65. In humans, the half-life of serum IgG, but not of IgA or IgM, is similarly long at 20–23 days (except for R435 IgG3-carrying allotypes)39,66, partly based on observations of a rare human disorder with β2m deficiency called familial hypercatabolic hypoproteinemia67. Vascular endothelial cells, macrophages and monocytes, which are highly pinocytic, are responsible for the recycling of IgGs in mice, whereas B cells and DCs are not17,68,69 (Fig. 2a). FcRn recycles IgGs by binding to the Fc region at acidic pH in the early endosome, and by releasing the IgG at neutral pH by exocytosis at the cell surface (Fig. 2b). This is a saturable process such that levels of IgG that exceed this protective activity are diverted to lysosomes for degradation70,71. The sorting of monomeric IgGs into FcRn+ recycling endosomes soon after pinocytic uptake and the dynamics of exocytosis have been visualized through advances in microscopy techniques, mainly in endothelial cell lines and more recently in primary macrophages72,73,74,75,76. Like IgGs, small, monomeric human IgG-ICs are recycled and protected via FcRn (Fig. 2b) in haematopoietic cells in mice, suggesting a similar mode of trafficking; large, multimeric human IgG-ICs, on the other hand, are not efficiently recycled yet are degraded more rapidly when FcRn is absent77 (Fig. 2c). In human cell lines, large multimeric human IgG-ICs are excluded from recycling sorting tubules and are instead mainly directed to FcRn+LAMP1+ lysosomes, which may be important for the antigen presentation functions of FcRn74,77,78 (Fig. 2c; see below). Blockade of the IgG interactions with FcRn via FcRn blockers in humans also reduces serum IgGs and IgG-ICs, showing the physiological relevance of these observations in model systems20,79,80. More studies are needed to understand how FcRn directs monomeric IgGs and small IgG-ICs to recycling endosomes for prevention of catabolism while directing relatively large IgG-ICs to antigen presentation compartments and lysosomes for regulated degradation, and how the size of IgG-ICs determines each of these outcomes (see below).
a, IgG recycling occurs within macrophages, monocytes and endothelial cells, based on mouse studies. b, Monomeric IgGs and small IgG immune complexes (IgG-ICs) consisting of a single antibody engaging two antigens are taken up by pinocytosis as they can not bind to neonatal Fc receptor (FcRn) at the neutral pH of the cell surface. Following the formation of an early endosome and its acidification, FcRn can bind to IgGs, which are diverted into recycling endosomes (Rab4+Rab11+) and exocytosed within Rab11+ exosomes, where the IgGs or small IgG-ICs are released from FcRn at neutral pH, extending their half-life in the body, while FcRn is recovered for another round of recycling. When FcRn is saturated, the excess unbound antibody is degraded in the lysosome. c, FcRn retains and regulates the degradation of multimeric IgG-ICs. Multimeric IgG-ICs bind Fc receptors for IgG (FcγRs) on the cell surface (neutral pH), where they are taken up into endosomes by receptor-mediated endocytosis allowing for co-engagement with FcRn and FcγRs at acidic pH. The multimeric IgG-ICs are retained in a FcRn+LAMP1+ lysosomal compartment (pH ~5.5) enriched in antigen presentation machinery (dashed arrow). It is not well understood how FcRn differentiates between the recycling and retention pathways. LAMP1, lysosomal-associated membrane protein 1.
FcRn as a transport receptor
In addition to its recycling function, FcRn has a fundamental role in maintaining the tissue distribution of IgGs by their transcytosis, which is the movement of IgGs across polarized endothelial cells and numerous types of epithelial cells. This was first studied in neonatal rodents, in which passive acquisition of IgGs from ingested maternal milk occurs through transcytosis across the intestinal epithelium81,82. Later, it was shown that FcRn was also capable of bidirectional transfer of IgGs in intestinal epithelial cell lines83 and between the lamina propria and gut lumen in human FcRn transgenic adult mice84,85 as well as at other locations (reviewed in86). Still, FcRn might exhibit a dominant vectoral direction of transport87,88. For example, endothelial FcRn at the blood–brain barrier has been proposed to mediate the unidirectional transport of IgGs out of the brain and into the blood, which may maintain the immune-privileged status of the brain89,90. Although the precise role of FcRn at the blood–brain barrier and other tissue interfaces is still emerging89,91,92,93, it is now well recognized that FcRn can thus mediate unidirectional or bidirectional IgG transfer, which has important implications for the delivery of therapeutics and potentially of vaccines94,95. Here, we focus on the most evident human example: the passive acquisition of immunity in the offspring from the mother.
FcRn and passive immunity
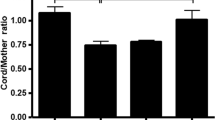
The passage of maternal antibodies to offspring is an important evolutionary mechanism of protection that operates in mammals and birds96. In humans, the acquisition of maternal IgG occurs in utero, whereby most antibodies are transferred during the third trimester of pregnancy97,98. IgG1 antibodies are transferred with the highest efficiency, followed by IgG4, with IgG2 and IgG3 subclasses having the lowest efficiency39,99,100. Several factors contribute to this Fc-dependent unidirectional transport, and their precise elucidation and effect on therapies, infections and vaccination during pregnancy is still ongoing (Box 5). In the human hemomonochorial placenta, as the gestation proceeds, the extensive invasiveness of trophoblasts into uterine tissues allows their direct contact with maternal blood, which is believed to facilitate IgG passage given that the antibody must traverse only three layers — syncytiotrophoblasts, embryonic connective tissue and embryonic capillary endothelium101 (Fig. 3). Indeed, the presence of FcRn has been amply demonstrated in human term placental trophoblasts, placental cell lines, cultured human placental epithelial cells and more recently in placental fetal endothelium and macrophages (Hofbauer cells)22,23,102,103,104,105,106,107,108,109,110. Outside of the direct evidence from mouse models, the ex vivo human placental transfer model was essential to illustrate the dominant role of FcRn in this process65,111,112. Using the latter approach, it was illustrated that modified human IgG1 variants that lack FcRn binding were not transferred into the fetal circulation, whereas another IgG1 variant (H433K/N434F) with enhanced engagement to FcRn was transported more efficiently108,113,114. Importantly, FcRn antagonism with an anti-FcRn monoclonal antibody in this setting showed fast receptor blockade with almost complete inability to transfer a model IgG1 antibody115.
a, In humans, maternal and fetal circulations are separated by a single layer of polarized epithelium called the syncytiotrophoblast, which the antibody must intially pass to reach the fetus. b, Transport of IgGs is largely mediated through the presence of neonatal Fc receptor (FcRn) at this site. The initial step of internalization of maternal IgGs is thought to occur via fluid-phase pinocytosis. The formed vesicles containing IgGs then fuse with endosomes, where at a mildly acidic pH, the interaction with FcRn allows transport of the antibody to the basolateral membrane and release into the stroma at neutral pH. From there, IgG is hypothesized to passively diffuse and reach fetal endothelial cells; whether a similar FcRn-dependent transcytosis of IgG across fetal endothelium occurs in vivo is currently unknown. RBC, red blood cell.
Active immune functions
Innate immunity
FcRn is expressed at high levels, along with FcγRs, at the cell surface and intracellularly in myeloid cells, where it participates directly in innate responses to IgG-ICs in a manner that is independent of its roles in recycling and transcytosis20,23 (Figs. 2 and 3). For example, the ability of IgG-ICs to promote pro-inflammatory cytokine production by innate immune cells involves FcRn (Fig. 4a). IL-12p35 mRNA production, phosphorylation of STAT1 and translocation of IRF1 and NF-κB subunit p65 to the nucleus in response to IgG-ICs depend on FcRn in mouse DCs and human monocyte-derived DCs116. Similarly, induction of IL-6 and TNF production by whole human blood exposed to IgG-ICs is FcRn dependent as it requires IgG binding to FcRn and can be pharmacologically blocked by an FcRn antagonist20. Further, FcRn cooperates with FcγRIIA, including its high-affinity (FcγRIIAH) and low-affinity (FcγRIIAR) allelic variants, in inducing these innate immune activities. Optimal responses necessitate the presence of both FcRn and FcγRIIA, which are presumed to function in a ternary complex that is bridged by an IgG-IC43.
a, IgG immune complexes (IgG-ICs) bind Fc receptors for IgG (FcγRs) on the cell surface at neutral pH. As the IgG-ICs are taken up into endosomes, they engage neonatal Fc receptor (FcRn) at a slightly acidic pH. In response to IgG-ICs, FcRn actively induces the production of pro-inflammatory cytokines IL-12, IL-23, tumour necrosis factor (TNF) and IL-6 by neutrophils, monocytes, macrophages and dendritic cells and the induction of tissue factor expression in monocytes and macrophages, through co-operation with FcγRs. b, FcRn promotes phagocytosis of IgG-coated Streptococcus pneumoniae in neutrophils. The IgG-opsonized bacteria bind to the neutrophil cell surface at neutral pH, likely by FcγRs, whereas FcRn binds to the IgGs at a slightly acidic pH and actively enhances phagocytosis. c, Once IgG-ICs are taken up by FcγR-expressing cells, FcRn enhances both antigen presentation to CD4+ T cells by dendritic cells and macrophages, and antigen cross-presentation to CD8+ T cells by dendritic cells. FcRn-associated antigen presentation by MHC class II occurs via degradation and peptide loading within the acidic endosome, whereas antigen cross-presentation by MHC class I occurs via a separate cytoplasmic and proteasomal processing pathway. The active participation of FcRn in these antigen-presenting pathways results in greatly enhanced T cell activation, expansion and production of IL-2 and interferon-γ (IFNγ) by the interacting immune cells, which probably further amplifies the immune response. TCR, T cell receptor.
Tissue factor production by monocytes is required for the initiation of coagulation and is involved in thromboembolic diseases that are associated with IgG-ICs in many IgG-mediated autoimmune diseases117,118, such as warm autoimmune haemolytic anaemia119. Whereas FcγRIIA and Toll-like receptors are known to promote tissue factor production, the role played by FcRn in this process has only recently been discovered120 (Fig. 4a). IgG-ICs, including those derived from clinically relevant pathogenic antibodies, can induce primary monocytes to produce tissue factor and tissue factor-dependent factor Xa; this activity is disabled if the IgG-IC is unable to bind FcRn or FcγR and if FcRn is blocked120. Similarly, blockade of FcRn prevents human platelet factor 4-mediated antibody induction of pathogenic fibrin (clot) accumulation in a mouse model of heparin-induced thrombocytopenia that depends upon FcγRIIA120,121.
Traditionally, activating FcγRs are well known to facilitate endocytosis and phagocytosis of IgG-ICs. It is therefore of interest that FcRn promotes the phagocytic uptake of IgG-opsonized Streptococcus pneumoniae, as shown in mouse Fcgrt−/− neutrophils and using a human IgG1H435A variant with diminished FcRn binding24 (Fig. 4b). These observations, along with the cytokine and tissue factor induction studies, illustrate that FcRn can work in collaboration with FcγRs in conducting various innate immune-related activities.
Adaptive immune interactions
IgG-bound antigen that is diverted by FcRn to the lysosome for degradation also promotes MHC class II antigen presentation to CD4+ T cells, both in vitro and in vivo77 (Fig. 4c). Macrophage-associated MHC class II presentation of a model antigen ovalbumin (OVA) as either soluble IgG-ICs or as larger latex bead–IgG-ICs to OVA-specific CD4+ T cells also depends on FcRn; this suggests that endocytic (soluble IgG-ICs) or phagocytic (latex bead–IgG-ICs) uptake of antigen is regulated by FcRn122. Likewise, FcRn blockade with a therapeutic antibody can inhibit the presentation of OVA within IgG-ICs to CD4+ T cells by mouse DCs expressing human FcRn, indicating that these pathways are amenable to pharmacological blockade20. This has clinical relevance, as the ability of human monocyte-derived DCs to present a disease-related antigen (gliadin) associated with coeliac disease as an IgG-IC also depends on FcRn77. Further, FcRn in monocytic cells also determines the ability of FcγRIIA to mediate antigen presentation, as the levels of CD4+ T cell stimulation are significantly decreased if the IgG-IC is unable to bind FcRn irrespective of the FcγRIIA allelic variant, further indicating co-operation with FcRn, as observed with innate immune responses43.
Some DC subsets are specialized in delivering extracellular antigens to CD8+ T cells in a process called cross-presentation123. FcRn enhances the ability of specific types of mouse DCs to cross-present antigen contained within an IgG-IC to CD8+ T cells relative to that observed with the soluble antigen alone78 (Fig. 4c). This allows the DC to robustly respond to low amounts of antigen bound by IgGs. FcRn enables the IgG-associated antigen to enter endosomal compartments that possess the proper conditions for conducting cross-presentation, including optimal acidification and oxidation and the presence of distinct proteins participating in these processes such as transporter associated with antigen processing (TAP)78. Such activities also involve prolonged retention of IgG-ICs within these intracellular organelles. Human FcRn-mediated regulation of cross-presentation by DCs can be inhibited by a therapeutic anti-FcRn antibody20. In a colorectal cancer model, FcRn-dependent cross-presentation by DCs is highly protective (see later)116. Interestingly, FcRn can mediate IgG-IC-induced cross-presentation in the absence of FcγRs if the extracellular pH is acidic and thus permissive for IgG binding to FcRn on the cell surface, as might occur in certain disease states such as cancer and infection43. However, optimal cross-presentation occurs if both FcRn and FcγR are engaged43. By demonstrating the role of FcRn in promoting cytokine production or antigen processing and presentation pathways, these studies support an important role for FcRn in innate and adaptive immunity.
Pathophysiological functions of FcRn
FcRn–IgG interactions can either be beneficial or detrimental to the host: they offer the necessary protection from most infectious diseases and may participate in antitumour responses, yet FcRn interactions with pathogenic and self-reactive IgGs can promote autoimmune diseases.
Infectious diseases
FcRn participates in immune responses to several bacterial and viral infections, for which the direct evidence mainly comes from animal studies. For instance, in a mouse Citrobacter rodentium infectious colitis model, the presence of FcRn limited clinicopathological damage85,124. In the gastrointestinal tract, FcRn has a dual function wherein it is involved in the transcytosis of IgGs and also delivers antigen in the form of IgG-ICs from the intestinal lumen to myeloid cells for the induction of regional and systemic immune responses84,85. Similarly, FcRn dramatically lessens the severity of intestinal Clostridioides difficile infection in mice, but only when mice are first immunized with the toxin B carboxy-terminal domain, which is necessary for the generation of protective IgGs125. The levels of faecal, but not serum, IgGs specific for the carboxy-terminal domain were much higher in immunized mice that expressed FcRn, and antibody transfer to the lumen of the intestine is likely to be responsible for these effects125. In mice, infections by Helicobacter heilmannii and Helicobacter pylori, which are causative agents of stomach ulcers, are limited by FcRn126. The levels of both H. heilmannii-specific IgG and H. pylori-specific IgG antibodies were higher in the gastric juice of wild type mice than in Fcgrt−/− mice, whereas no differences in circulating antigen-specific IgG levels were seen. This suggests that FcRn in epithelial cells mediates local protection via its transport functions126. FcRn also plays a role in protection from Lyme disease-associated arthritis, caused by Borrelia burgdorferi. Specifically, FcRn-deficient mice exhibited increased joint histopathology and ankle-swelling post-intradermal infection, and had lower levels of serum B. burgdorferi-specific antibodies127.
IgGs are the major subtype of antibody in vaginal secretions and are important for protection against viral sexually transmitted diseases, through FcRn-mediated transcytosis128. Herpes simplex virus type 2 (HSV-2) infection in mice can be prevented by passive transfer of anti-HSV-2-specific IgGs in wild type mice but not in Fcgrt−/− mice, probably through FcRn-mediated transport of antibodies across the vaginal epithelium129. FcRn plays a role in preventing Zika virus infection130, as serum IgGs from infected (but not uninfected) mice injected intraperitoneally can confer protection from intravaginal Zika virus infection, and the virus-specific antibodies were found within the vaginal lumen130. FcRn transport of influenza virus haemagglutinin (HA)-specific antibodies may play a role in the neutralization of this virus as well in the lung, another organ that is a major site of IgG transport131. Interestingly, fusion proteins comprising Fc and viral-derived antigens, such as HA or HSV-2 glycoprotein, used in models of mouse vaccination were successful in enhancing transport of the antigen across the nasal epithelium, and might provide a novel FcRn-based immunization strategy94,132.
In the infectious disease setting, the role of FcRn can also be detrimental depending on the specificity of the antimicrobial IgGs. In the case of Chlamydia muridarum infection, IgGs recognizing chlamydial extracellular antigens enhanced infection in a FcRn-dependent manner, whereas IgGs recognizing intracellular determinants were protective133. Indeed, accumulating data indicate that certain pathogens have evolved to use FcRn to their advantage (Box 4).
Cancer
FcRn is expressed by both tumours and tumour-infiltrating immune cells, where it can engage IgGs and albumin, affecting the outcome of disease in both mouse models and humans105,134,135. Compared with wild type mice, Fcgrt−/− mice develop more tumour lesions in a melanoma lung metastasis model in association with defects in NK cell development, maturation and impaired ability to degranulate and secrete IFNγ136,137. This is interesting as FcRn is not expressed by NK cells, so the observed phenotype might indirectly depend on interactions with other FcRn+ immune cells. FcRn expression also confers protection in both colorectal cancer and melanoma lung metastasis models in mice through activation of CD8+ cytotoxic T cells by FcRn-dependent cross-presentation of IgG-complexed antigen by DCs, which also secrete high amounts of IL-12116. Remarkably, in humans, high FcRn expression by CD11c+ DCs in colorectal cancer tissue is predictive of long-term survival and, as in mouse studies in vivo, FcRn expression by CD11c+ cells is positively correlated with the infiltration of CD8+ T cells into the tumour site116. These results are consistent with the survival analysis of patients with non-small-cell lung cancer wherein the average survival of FCGRT high-expressing patients in one of the cohorts tested was 62.0 months compared with 37.3 months in FCGRT low-expressing patients, with the majority of the FCGRT mRNA expression detected in immune cells138.
Our understanding of the role that FcRn expression plays in the tumour cells themselves is still emerging. For instance, some tumours have been shown to downregulate FcRn expression139,140, whereas others upregulate it134. Given that, besides IgGs, FcRn also engages albumin, both immune and non-immune activities of FcRn can be involved58. In this regard, FcRn downregulation might lead to reduced recycling and increased intracellular accumulation of albumin or albumin-carried cargo, which can provide an alternative source of energy to the tumour139,141. Understanding FcRn functions within the context of cancer biology is also leading to the development of new antitumour therapies or improved theranostics142,143. For example, engineered albumin that exhibits increased FcRn binding can be used to deliver cytotoxic drugs to tumour cells, such as doxorubicin140. Others have developed engineered antibodies with enhanced FcRn binding (Abdeg based) known as Seldegs (selective degradation of antigen-specific antibodies)144 that when coupled to tumour antigens can be deployed to improve diagnostic imaging145. This approach showed promise in mouse models whereby excess levels of unbound radiolabelled diagnostic antibodies were reduced, resulting in decreased imaging background.
Autoimmunity
IgG-mediated autoimmune diseases represent a broad class of clinical conditions that result in chronic, incurable symptoms that potentially affect nearly every organ in the body. The autoantibodies that cause these diseases do so through several complex mechanisms, such as by direct cell lysis or by induction of pro-inflammatory mediators, which have been elegantly reviewed elsewhere146. IgG-mediated autoimmune diseases can be classified into two groups: the first includes diseases in which the specificity of the autoantibodies has been clearly identified and is directly involved in the pathogenesis of the disorder, such as myasthenia gravis (MG) and pemphigus-related disorders. The second encompasses complex autoimmune diseases such as inflammatory bowel disease (IBD), rheumatoid arthritis (RA) and multiple sclerosis (MS), in which the IgG antibodies are involved in a much broader range of immunological pathways147,148.
The role of FcRn in these disorders was initially recognized in the 1990s through the use of B2m−/− mice, in which the absence of β2m results in functional deficiency in FcRn, and ultimately in 2003 with the development of Fcgrt−/− animals62,63,64,65,111,149,150. In this way, it was shown that autoimmune diseases such as pemphigus-related disorders required FcRn for the ability of autoantibody to cause disease150,151. Importantly, these studies also showed that FcRn was required for evincing the phenotype associated with complex diseases such as IBD and RA152,153. These pioneering studies led to the development of therapeutic approaches that impede FcRn function, which fall into three broad classes: engineered Fc fragments, antibodies and peptides. Here, we summarize some of the preclinical, proof-of-concept studies that represent the forerunners of current clinical approaches by focusing on a select group of classical and complex IgG-mediated autoimmune diseases.
Autoantibody-mediated diseases of the skin, such as epidermolysis bullosa acquisita (EBA), bullous pemphigoid and pemphigus, involve FcRn. FcRn-deficient mice were protected from blistering in type VII collagen-immunization or passive antibody transfer EBA models, and these mice had lower levels of type VII collagen-specific serum antibodies154. Mice that develop EBA can be successfully treated with FcRn blockade, causing a reduction in circulating pathogenic anti-type VII collagen IgGs and IgG deposition in the skin155. Fcgrt−/− mice were also highly resistant to developing the blistering and pathological damage of pemphigus after treatment with rabbit anti-BP180, or with human anti-desmoglein 1 and anti-desmoglein 3 IgG antibodies, showing reduced neutrophil infiltration in the bullous pemphigoid model along with the expected reduction of pathogenic antibodies in the serum151.
FcRn promotes the development and progression of diseases of the nervous system, including Guillain–Barré syndrome (GBS), MS and MG. In an antibody-mediated model of axonal GBS, reduced levels of pathogenic anti-glycan/ganglioside antibodies were found both in wild type mice therapeutically treated with IgG1MST-HN (or Abdeg) and in Fcgrt−/− mice, and there was improved nerve regeneration156. In experimental autoimmune encephalomyelitis (EAE) or antibody-mediated EAE models of human MS, Abdegs caused degradation of total IgGs, including disease-specific antibodies in the brain and spinal cord, and reduced disease activity. In addition, using the previously mentioned Seldeg approach, which consisted of an Abdeg Fc mutant fused with myelin oligodendrocyte glycoprotein (MOG), also reduced disease activity by exclusive degradation of pathogenic autoantibodies157,158. FcRn blockade also limited optomotor defects in a similar IgG-mediated EAE model of MS, reduced spinal demyelination and specifically altered macrophage infiltration into the spinal cord, with no differences in B cells, T cells or complement deposition159. In a passive transfer model of anti-muscle-specific kinase IgG4 from patients with MG, IgG1MST-HN effectively ameliorated muscle weakness, weight loss and improved calf compound muscle action potentials, which correlated with lowering of serum pathogenic antibodies160. Acetylcholine receptor-specific antibody-mediated MG was also ameliorated by FcRn blockade in both immunization and passive transfer models in rats, which coincided with a decrease in inflammatory macrophages161.
Autoimmune haematological diseases, such as experimental immune thrombocytopenic purpura (ITP), can be therapeutically ameliorated through FcRn blockade. Prophylactic or therapeutic use of a mouse anti-FcRn antibody restored platelet numbers in the anti-CD41 passive transfer model of ITP and prophylactic blockade with an engineered Fc construct targeting both FcRn and FcγRs prevented the short-term loss of platelets in an ITP model involving passive transfer of a human anti-platelet antibody121,162.
In the K/BxN passive serum transfer model of RA, which relies on mouse anti-glucose 6-phosphate isomerase (GPI) antibodies, FcRn is required for the development of disease152. Total serum antibodies and anti-GPI-specific IgG antibodies were substantially lower in Fcgrt−/− mice, which indicates that the lowering of pathogenic antibodies plays a major role in this disease model152. Abdegs, or IgG1MST-HN, enhanced degradation of IgGs and dramatically lowered ankle swelling and histological joint damage in the K/BxN model162,163. Low-dose antibody blockade of mouse FcRn also ameliorated disease severity in mice expressing the low-affinity human FcγRIIAR variant in the K/BxN model, but without lowering circulating total or pathogenic IgGs; this suggests that FcRn may promote RA through multiple mechanisms that potentially include cooperation with FcγRs in myeloid cells in addition to effects on IgG recycling43. Consistent with this, disease burden is also reduced by simultaneously targeting FcRn and FcγRs in the K/BxN and collagen-induced arthritis models, which show the important roles that each of these receptors have in promoting RA162.
FcRn contributes to autoimmune kidney damage. In mice immunized with the non-collagenous domain of the α3 chain of type IV collagen, subepithelial ICs caused glomerular pathology and proteinuria, and an FcRn-inhibitor peptide was able to effectively limit disease164. Podocyte-specific FcRn promoted glomerulosclerosis and glomerular crescents in a nephrotoxic serum nephritis model, whereas it did not affect disease in an acute anti-glomerular basement membrane nephritis model165. Serum from patients with lupus nephritis or transplant glomerulopathy166, but not from healthy donors, induced expression of calcium/calmodulin-dependent protein kinase 4 and CD86 in human podocytes in vitro, and this activation pathway was confirmed to cause lupus nephritis-associated damage and proteinuria in vivo167,168, in an FcRn-dependent manner.
FcRn is also involved in the pathogenesis of IBD, as IgGs against commensal microorganisms and potentially autoantibodies can contribute to this disease169,170. A colitis model induced by bacterial flagellin immunization and dextran sulfate sodium treatment was more severe in wild type mice, with greater clinicopathological damage, than in Fcgrt−/− mice153. These differences were associated with the haematopoietic rather than the non-haematopoietic compartment in a study using bone marrow chimeras, although whether the effects observed were due to their role in extending IgG half-life versus regulation of a direct immune response was not assessed153.
Altogether, these studies have clearly established a role for FcRn in the pathogenesis of infectious, neoplastic and autoimmune diseases. Moreover, it is likely that FcRn’s involvement in these disorders occurs at many levels, including its activities in half-life extension (recycling), the delivery of IgG and/or IgG-ICs across tissues (transcytosis), the regulation of immune effector functions and its relationship with classical FcγRs. In addition, it is possible that FcRn also mediates its disease-related effects through expression in specific cell types at the site of tissue damage171.
FcRn blockade in the clinic
Currently, several strategies are used to address the damage provoked by the presence of pathogenic IgGs and IgG-ICs, such as corticosteroids, immunosuppressants, B cell depletion (with rituximab), high doses of intravenous immunoglobulin and plasmapheresis146. Unfortunately, a large proportion of the patients affected by autoimmunity still have unmet clinical needs in addition to the high cost, broad effects on the immune system, and drug shortages associated with some of these treatments (such as plasma donations for intravenous immunoglobulin)172. More recently, an approach to prevent FcRn–IgG interactions has gained momentum. Five antibody-based drugs (batoclimab, efgartigimod, nipocalimab, orilanolimab and rozanolixizumab) have successfully passed through phase I clinical trials and have demonstrated their ability to reduce total circulating IgG levels (Supplementary Table 1), but not other types of antibodies, in healthy participants20,173,174,175,176. Most of these drugs have advanced to phase II/III trials for treatment of several classical IgG-mediated autoimmune diseases in which pathogenic IgGs are clearly involved, with published data in patients with ITP, MG or pemphigus (Table 1). Altogether, the available data from clinical trials in healthy subjects and patients with severe generalized MG, primary ITP and pemphigus indicate that blocking FcRn–IgG interactions in humans is well tolerated and results in disease amelioration, with reductions in circulating pathogenic IgGs, total IgGs and circulating ICs20,79,173,174,175,176,177,178,179,180,181,182,183. For example, in the largest study so far, efgartigimod treatment of people with generalized MG reduced pathogenic antibodies and significantly decreased disease severity (Table 1). There are indications emerging that these therapies may also be disease modifying by mechanisms that are yet to be understood but are probably linked to the cellular effects that FcRn blockade has on disease-promoting immune cells80. Consistently, the observed treatment-emergent adverse events have been mild to moderate and generally comparable between patients in placebo and drug treatment groups, with the most frequent adverse event being headache. In December 2021, the first FcRn blocker was approved in the USA by the FDA, followed by similar approval in Japan, for the treatment of MG.
Blockade of FcRn–IgG interactions in humans is currently being evaluated in children with generalized MG (NCT05374590, NCT04833894); in pregnant women, to prevent transfer of pathogenic antibodies to the fetus (NCT03842189, NCT03755128, Box 6); and to treat numerous other autoimmune diseases (Table 1). All drugs in this class are associated with prolonged hypogammaglobulinemia and thus concurrent depletion of protective antibodies alongside the pathogenic ones, which could result in increased susceptibility to infections. The ongoing phase III trials with greater numbers of patients and longer exposure to the FcRn antagonists will provide a much clearer and needed understanding of the impact of FcRn blockade in humans. Nonetheless, FcRn blockade is now demonstrated to be a novel, effective therapeutic strategy to curtail autoimmune diseases associated with the presence of pathogenic IgGs.
Conclusions
Since the pioneering predictions of a transport and protection receptor by F.W. Rogers Brambell (Supplementary Fig. 1) in the 1960s, the studies over the past 30 years have allowed FcRn to gain a prominent place in numerous therapeutic approaches that involve leveraging its relationship with its two ligands: IgG and albumin. The translation of these insights includes the engineering of therapeutic antibodies and Fc fusion proteins, the development of engineered albumin molecules as carrier proteins and now the successful development of FcRn blockers. As the scientific community extends its understanding of FcRn biology and expands the use of these current approaches, many other therapeutic opportunities are likely to arise in this field.
References
Akula, S., Mohammadamin, S. & Hellman, L. Fc receptors for immunoglobulins and their appearance during vertebrate evolution. PLoS ONE 9, e96903 (2014).
Delidakis, G., Kim, J. E., George, K. & Georgiou, G. Improving antibody therapeutics by manipulating the Fc domain: immunological and structural considerations. Annu. Rev. Biomed. Eng. 24, 249–274 (2022).
Ward, E. S. et al. Clinical significance of serum albumin and implications of FcRn inhibitor treatment in IgG-mediated autoimmune disorders. Front. Immunol. 13, 892534 (2022).
Bern, M., Sand, K. M., Nilsen, J., Sandlie, I. & Andersen, J. T. The role of albumin receptors in regulation of albumin homeostasis: implications for drug delivery. J. Control. Rel. 211, 144–162 (2015).
Kandil, E. et al. The human gene encoding the heavy chain of the major histocompatibility complex class I-like Fc receptor (FCGRT) maps to 19q13.3. Cytogenetics Cell Genet. 73, 97–98 (1996).
Mikulska, J. E., Pablo, L., Canel, J. & Simister, N. E. Cloning and analysis of the gene encoding the human neonatal Fc receptor. Eur. J. Immunogenetics 27, 231–240 (2000).
Catunda Lemos, A. P. et al. Characterization of the rabbit neonatal Fc receptor (FcRn) and analyzing the immunophenotype of the transgenic rabbits that overexpresses FcRn. PLoS ONE 7, e28869 (2012).
Simister, N. E. & Mostov, K. E. An Fc receptor structurally related to MHC class I antigens. Nature 337, 184–187 (1989). This study reports the first purification and cloning of the rat FcRn heterodimer (β2m light chain and the MHC class I-related heavy chain).
Simister, N. E. & Rees, A. R. Isolation and characterization of an Fc receptor from neonatal rat small intestine. Eur. J. Immunol. 15, 733–738 (1985).
Burmeister, W., Gastinel, L., Simister, N., Blum, M. & Bjorkman, P. Crystal structure at 2.2 A resolution of the MHC-related neonatal Fc receptor. Nature 372, 336–343 (1994). This paper reports the first crystal structure of FcRn and an IgG Fc–FcRn complex.
Burmeister, W., Huber, A. & Bjorkman, P. Crystal structure of the complex of rat neonatal Fc receptor with Fc. Nature 372, 379–383 (1994).
Sachs, U. J. et al. A variable number of tandem repeats polymorphism influences the transcriptional activity of the neonatal Fc receptor α-chain promoter. Immunology 119, 83–89 (2006).
Raghavan, M., Gastinel, L. N. & Bjorkman, P. J. The class I major histocompatibility complex related Fc receptor shows pH-dependent stability differences correlating with immunoglobulin binding and release. Biochemistry 32, 8654–8660 (1993).
Ye, L. et al. The MHC class II-associated invariant chain interacts with the neonatal Fcγ receptor and modulates its trafficking to endosomal/lysosomal compartments. J. Immunol. 181, 2572–2585 (2008).
Zhu, X. et al. The heavy chain of neonatal Fc receptor for IgG is sequestered in endoplasmic reticulum by forming oligomers in the absence of β2-microglobulin association. Biochem. J. 367, 703–714 (2002).
Israel, E. J. et al. Expression of the neonatal Fc receptor, FcRn, on human intestinal epithelial cells. Immunology 92, 69–74 (1997).
Akilesh, S., Christianson, G. J., Roopenian, D. C. & Shaw, A. S. Neonatal FcR expression in bone marrow-derived cells functions to protect serum IgG from catabolism. J. Immunol. 179, 4580–4588 (2007).
Uhlén, M. et al. Proteomics. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Latvala, S., Jacobsen, B., Otteneder, M. B., Herrmann, A. & Kronenberg, S. Distribution of FcRn across species and tissues. J. Histochem. Cytochem. 65, 321–333 (2017).
Blumberg, L. J. et al. Blocking FcRn in humans reduces circulating IgG levels and inhibits IgG immune complex–mediated immune responses. Sci. Adv. 5, eaax9586 (2019). This study provides evidence that therapeutic blockade of FcRn in humans reduces serum IgGs and IgG-ICs, whereas it also inhibits innate and adaptive immune responses to IgG-ICs in human cells in vitro.
Karlsson, M. et al. A single-cell type transcriptomics map of human tissues. Sci. Adv. 7, eabh2169 (2021).
Kiskova, T. et al. Expression of the neonatal Fc-receptor in placental-fetal endothelium and in cells of the placental immune system. Placenta 78, 36–43 (2019).
Zhu, X. et al. MHC class I-related neonatal Fc receptor for IgG is functionally expressed in monocytes, intestinal macrophages, and dendritic cells. J. Immunol. 166, 3266–3276 (2001). This article shows for the first time that FcRn is expressed in myeloid cells, including monocytes, macrophages and dendritic cells.
Vidarsson, G. et al. FcRn: an IgG receptor on phagocytes with a novel role in phagocytosis. Blood 108, 3573–3579 (2006). These experiments provide evidence that FcRn plays a role in phagocytosis of IgG-ICs by neutrophils.
Liu, X. et al. NF-κB signaling regulates functional expression of the MHC class I-related neonatal Fc receptor for IgG via intronic binding sequences. J. Immunol. 179, 2999–3011 (2007).
Qian, S. et al. Activation of the JNK/MAPK signaling pathway by TGF-β1 enhances neonatal Fc receptor expression and IgG transcytosis. Microorganisms 9, 879 (2021).
Guo, J. et al. TGEV infection up-regulates FcRn expression via activation of NF-κB signaling. Sci. Rep. 6, 32154 (2016).
Rathore, A. P. S., Saron, W. A. A., Lim, T., Jahan, N. & St John, A. L. Maternal immunity and antibodies to dengue virus promote infection and Zika virus-induced microcephaly in fetuses. Sci. Adv. 5, eaav3208 (2019).
Liu, X. et al. Activation of the JAK/STAT-1 signaling pathway by IFN-γ can down-regulate functional expression of the MHC class I-related neonatal Fc receptor for IgG. J. Immunol. 181, 449–463 (2008).
Schmidt, M. M. et al. Crystal structure of an HSA/FcRn complex reveals recycling by competitive mimicry of HSA ligands at a pH-dependent hydrophobic interface. Structure 21, 1966–1978 (2013). This study shows the structural mechanism by which FcRn is able to recycle albumin and the development of high-affinity albumin mutants that can be used for the development of therapeutics with increased half-life.
West, A. P. Jr & Bjorkman, P. J. Crystal structure and immunoglobulin G binding properties of the human major histocompatibility complex-related Fc receptor. Biochemistry 39, 9698–9708 (2000).
Martin, W. L., West, A. P., Gan, L. & Bjorkman, P. J. Crystal structure at 2.8 Å of an FcRn/heterodimeric Fc complex: mechanism of pH-dependent binding. Mol. Cell 7, 867–877 (2001).
Oganesyan, V. et al. Structural insights into neonatal Fc receptor-based recycling mechanisms. J. Biol. Chem. 289, 7812–7824 (2014).
Raghavan, M., Bonagura, V. R., Morrison, S. L. & Bjorkman, P. J. Analysis of the pH dependence of the neonatal Fc receptor/immunoglobulin G interaction using antibody and receptor variants. Biochemistry 34, 14649–14657 (1995).
Kim, J. K. et al. Mapping the site on human IgG for binding of the MHC class I-related receptor, FcRn. Eur. J. Immunol. 29, 2819–2825 (1999).
Ober, R. J., Radu, C. G., Ghetie, V. & Ward, E. S. Differences in promiscuity for antibody–FcRn interactions across species: implications for therapeutic antibodies. Int. Immunol. 13, 1551–1559 (2001).
Andersen, J. T., Daba, M. B., Berntzen, G., Michaelsen, T. E. & Sandlie, I. Cross-species binding analyses of mouse and human neonatal Fc receptor show dramatic differences in immunoglobulin G and albumin binding. J. Biol. Chem. 285, 4826–4836 (2010).
Neuber, T. et al. Characterization and screening of IgG binding to the neonatal Fc receptor. mAbs 6, 928–942 (2014).
Stapleton, N. M. et al. Competition for FcRn-mediated transport gives rise to short half-life of human IgG3 and offers therapeutic potential. Nat. Commun. 2, 599 (2011).
Keeble, A. H., Khan, Z., Forster, A. & James, L. C. TRIM21 is an IgG receptor that is structurally, thermodynamically, and kinetically conserved. Proc. Natl Acad. Sci. USA. 105, 6045–6050 (2008).
Tao, M. H. & Morrison, S. L. Studies of aglycosylated chimeric mouse-human IgG. Role of carbohydrate in the structure and effector functions mediated by the human IgG constant region. J. Immunol. 143, 2595–2601 (1989).
Wines, B. D., Powell, M. S., Parren, P. W., Barnes, N. & Hogarth, P. M. The IgG Fc contains distinct Fc receptor (FcR) binding sites: the leukocyte receptors FcγRI and FcγRIIa bind to a region in the Fc distinct from that recognized by neonatal FcR and protein A. J. Immunol. 164, 5313–5318 (2000).
Hubbard, J. J. et al. FcRn is a CD32a coreceptor that determines susceptibility to IgG immune complex-driven autoimmunity. J. Exp. Med. 217, e20200359 (2020).
Ko, S., Jo, M. & Jung, S. T. Recent achievements and challenges in prolonging the serum half-lives of therapeutic IgG antibodies through Fc engineering. BioDrugs 35, 147–157 (2021).
Vaccaro, C., Zhou, J., Ober, R. J. & Ward, E. S. Engineering the Fc region of immunoglobulin G to modulate in vivo antibody levels. Nat. Biotechnol. 23, 1283–1288 (2005). This is the first report of an FcRn-blocking therapeutic that lowers IgG levels in vivo.
Martin, W. L. & Bjorkman, P. J. Characterization of the 2:1 complex between the class I MHC-related Fc receptor and its Fc ligand in solution. Biochemistry 38, 12639–12647 (1999).
Popov, S. et al. The stoichiometry and affinity of the interaction of murine Fc fragments with the MHC class I-related receptor, FcRn. Mol. Immunol. 33, 521–530 (1996).
Tesar, D. B., Tiangco, N. E. & Bjorkman, P. J. Ligand valency affects transcytosis, recycling and intracellular trafficking mediated by the neonatal Fc receptor. Traffic 7, 1127–1142 (2006).
Abdiche, Y. N. et al. The neonatal Fc receptor (FcRn) binds independently to both sites of the IgG homodimer with identical affinity. mAbs 7, 331–343 (2015).
Sun, Y., Estevez, A., Schlothauer, T. & Wecksler, A. T. Antigen physiochemical properties allosterically effect the IgG Fc-region and Fc neonatal receptor affinity. mAbs 12, 1802135 (2020).
Wang, W. et al. Monoclonal antibodies with identical Fc sequences can bind to FcRn differentially with pharmacokinetic consequences. Drug Metab. Dispos. 39, 1469–1477 (2011).
Schlothauer, T. et al. Analytical FcRn affinity chromatography for functional characterization of monoclonal antibodies. mAbs 5, 576–586 (2013).
Piche-Nicholas, N. M. et al. Changes in complementarity-determining regions significantly alter IgG binding to the neonatal Fc receptor (FcRn) and pharmacokinetics. mAbs 10, 81–94 (2018).
Jensen, P. F. et al. Investigating the interaction between the neonatal Fc receptor and monoclonal antibody variants by hydrogen/deuterium exchange mass spectrometry. Mol. Cell Proteom. 14, 148–161 (2015).
Rossini, S. et al. V region of IgG controls the molecular properties of the binding site for neonatal Fc receptor. J. Immunol. 205, 2850–2860 (2020).
Grevys, A. et al. Antibody variable sequences have a pronounced effect on cellular transport and plasma half-life. iScience 25, 103746 (2022).
Schoch, A. et al. Charge-mediated influence of the antibody variable domain on FcRn-dependent pharmacokinetics. Proc. Natl Acad. Sci. USA 112, 5997–6002 (2015).
Chaudhury, C. et al. The major histocompatibility complex-related Fc receptor for IgG (FcRn) binds albumin and prolongs its lifespan. J. Exp. Med. 197, 315–322 (2003). This study shows for the first time that albumin is a ligand for FcRn.
Morosky, S. et al. The neonatal Fc receptor is a pan-echovirus receptor. Proc. Natl Acad. Sci. USA 116, 3758–3763 (2019). This article illustrates that FcRn is a pan-echovirus receptor.
Zhao, X. et al. Human neonatal Fc receptor is the cellular uncoating receptor for Enterovirus B. Cell 177, 1553–1565 (2019). This study shows that FcRn is a receptor for Enterovirus B, which allows for its uncoating within cells.
Wang, K. et al. Structures of echovirus 30 in complex with its receptors inform a rational prediction for enterovirus receptor usage. Nat. Commun. 11, 4421 (2020).
Christianson, G. J. et al. β2-microglobulin-deficient mice are protected from hypergammaglobulinemia and have defective antibody responses because of increased IgG catabolism. J. Immunol. 159, 4781–4792 (1997).
Israel, E. J., Wilsker, D. F., Hayes, K. C., Schoenfeld, D. & Simister, N. E. Increased clearance of IgG in mice that lack β2-microglobulin: possible protective role of FcRn. Immunology 89, 573–578 (1996).
Ghetie, V. et al. Abnormally short serum half-lives of IgG in β2-microglobulin-deficient mice. Eur. J. Immunol. 26, 690–696 (1996).
Roopenian, D. C. et al. The MHC class I-like IgG receptor controls perinatal IgG transport, IgG homeostasis, and fate of IgG-Fc-coupled drugs. J. Immunol. 170, 3528–3533 (2003). This is the first report of Fcgrt−/− mice, which were critical to uncover FcRn as a receptor that controls homeostasis and perinatal transport of IgGs, along with controlling the fate of IgG Fc drugs.
Morell, A., Terry, W. D. & Waldmann, T. A. Metabolic properties of IgG subclasses in man. J. Clin. Invest. 49, 673–680 (1970).
Wani, M. A. et al. Familial hypercatabolic hypoproteinemia caused by deficiency of the neonatal Fc receptor, FcRn, due to a mutant β2-microglobulin gene. Proc. Natl Acad. Sci. USA 103, 5084–5089 (2006). This report provides evidence in humans that FcRn maintains serum persistence of IgGs and albumin, through the report of a human mutation in the β2m light chain of FcRn.
Montoyo, H. P. et al. Conditional deletion of the MHC class I-related receptor FcRn reveals the sites of IgG homeostasis in mice. Proc. Natl Acad. Sci. Usa. 106, 2788–2793 (2009).
Challa, D. K. et al. Neonatal Fc receptor expression in macrophages is indispensable for IgG homeostasis. mAbs 11, 848–860 (2019).
Junghans, R. P. & Anderson, C. L. The protection receptor for IgG catabolism is the β2-microglobulin-containing neonatal intestinal transport receptor. Proc. Natl Acad. Sci. USA 93, 5512–5516 (1996).
Ward, E. S., Zhou, J., Ghetie, V. & Ober, R. J. Evidence to support the cellular mechanism involved in serum IgG homeostasis in humans. Int. Immunol. 15, 187–195 (2003).
Ober, R. J., Martinez, C., Lai, X., Zhou, J. & Ward, E. S. Exocytosis of IgG as mediated by the receptor, FcRn: an analysis at the single-molecule level. Proc. Natl Acad. Sci. USA. 101, 11076–11081 (2004).
Prabhat, P. et al. Elucidation of intracellular recycling pathways leading to exocytosis of the Fc receptor, FcRn, by using multifocal plane microscopy. Proc. Natl Acad. Sci. USA 104, 5889–5894 (2007).
Weflen, A. W. et al. Multivalent immune complexes divert FcRn to lysosomes by exclusion from recycling sorting tubules. Mol. Biol. Cell 24, 2398–2405 (2013).
Tzaban, S. et al. The recycling and transcytotic pathways for IgG transport by FcRn are distinct and display an inherent polarity. J. Cell Biol. 185, 673–684 (2009).
Toh, W. H. et al. FcRn mediates fast recycling of endocytosed albumin and IgG from early macropinosomes in primary macrophages. J. Cell Sci. 133, jcs235416 (2019).
Qiao, S. W. et al. Dependence of antibody-mediated presentation of antigen on FcRn. Proc. Natl Acad. Sci. USA 105, 9337–9342 (2008). This paper outlines the discovery of the role of FcRn in the presentation of antigens, which are complexed with IgGs, by dendritic cells to CD4+ T cells.
Baker, K. et al. Neonatal Fc receptor for IgG (FcRn) regulates cross-presentation of IgG immune complexes by CD8−CD11b+ dendritic cells. Proc. Natl Acad. Sci. Usa. 108, 9927–9932 (2011).
Werth, V. P. et al. Safety, tolerability, and activity of ALXN1830 targeting the neonatal Fc receptor in chronic pemphigus. J. Investig. Dermatol. 141, 2858–2865 (2021).
Maho-Vaillant, M. et al. FcRn antagonism leads to a decrease of desmoglein-specific B cells: secondary analysis of a phase 2 study of efgartigimod in pemphigus vulgaris and pemphigus foliaceus. Front. Immunol. 13, 863095 (2022).
Jones, E. A. & Waldmann, T. A. The mechanism of intestinal uptake and transcellular transport of IgG in the neonatal rat. J. Clin. Invest. 51, 2916–2927 (1972).
Rodewald, R. Selective antibody transport in the proximal small intestine of the neonatal rat. J. Cell Biol. 45, 635–640 (1970). This report describes the discovery that IgGs are transported into the proximal small intestine of neonatal rats.
Dickinson, B. L. et al. Bidirectional FcRn-dependent IgG transport in a polarized human intestinal epithelial cell line. J. Clin. Invest. 104, 903–911 (1999).
Yoshida, M. et al. Human neonatal Fc receptor mediates transport of IgG into luminal secretions for delivery of antigens to mucosal dendritic cells. Immunity 20, 769–783 (2004).
Yoshida, M. et al. Neonatal Fc receptor for IgG regulates mucosal immune responses to luminal bacteria. J. Clin. Invest. 116, 2142–2151 (2006).
Qi, T. & Cao, Y. In translation: FcRn across the therapeutic spectrum. Int. J. Mol. Sci. 22, 3048 (2021).
Kobayashi, N. et al. FcRn-mediated transcytosis of immunoglobulin G in human renal proximal tubular epithelial cells. Am. J. Physiol. Ren. Physiol. 282, 65 (2002).
Sarav, M. et al. Renal FcRn reclaims albumin but facilitates elimination of IgG. J. Am. Soc. Nephrol. 20, 1941–1952 (2009).
Cooper, P. R. et al. Efflux of monoclonal antibodies from rat brain by neonatal Fc receptor, FcRn. Brain Res. 1534, 13–21 (2013).
Deane, R. et al. IgG-assisted age-dependent clearance of Alzheimer’s amyloid β peptide by the blood–brain barrier neonatal Fc receptor. J. Neurosci. 25, 11495–11503 (2005).
Abuqayyas, L. & Balthasar, J. P. Investigation of the role of FcγR and FcRn in mAb distribution to the brain. Mol. Pharm. 10, 1505–1513 (2013).
Ruano-Salguero, J. S. & Lee, K. H. Antibody transcytosis across brain endothelial-like cells occurs nonspecifically and independent of FcRn. Sci. Rep. 10, 3685 (2020).
Zhang, Y. & Pardridge, W. M. Mediated efflux of IgG molecules from brain to blood across the blood-brain barrier. J. Neuroimmunol. 114, 168–172 (2001).
Ye, L., Zeng, R., Bai, Y., Roopenian, D. C. & Zhu, X. Efficient mucosal vaccination mediated by the neonatal Fc receptor. Nat. Biotechnol. 29, 158–163 (2011).
Lu, L. et al. A neonatal Fc receptor-targeted mucosal vaccine strategy effectively induces HIV-1 antigen-specific immunity to genital infection. J. Virol. 85, 10542–10553 (2011).
West, A. P. Jr, Herr, A. B. & Bjorkman, P. J. The chicken yolk sac IgY receptor, a functional equivalent of the mammalian MHC-related Fc receptor, is a phospholipase A2 receptor homolog. Immunity 20, 601–610 (2004).
Malek, A., Sager, R. & Schneider, H. Maternal-fetal transport of immunoglobulin G and its subclasses during the third trimester of human pregnancy. Am. J. Reprod. Immunol. 32, 8–14 (1994).
Jauniaux, E. et al. Materno-fetal immunoglobulin transfer and passive immunity during the first trimester of human pregnancy. Hum. Reprod. 10, 3297–3300 (1995).
Einarsdottir, H. K. et al. Comparison of the Fc glycosylation of fetal and maternal immunoglobulin G. Glycoconj. J. 30, 147–157 (2013).
Clements, T. et al. Update on transplacental transfer of IgG subclasses: impact of maternal and fetal factors. Front. Immunol. 11, 1920 (2020).
DeSesso, J. M., Williams, A. L., Ahuja, A., Bowman, C. J. & Hurtt, M. E. The placenta, transfer of immunoglobulins, and safety assessment of biopharmaceuticals in pregnancy. Crit. Rev. Toxicol. 42, 185–210 (2012).
Leach, J. L. et al. Isolation from human placenta of the IgG transporter, FcRn, and localization to the syncytiotrophoblast: implications for maternal-fetal antibody transport. J. Immunol. 157, 3317–3322 (1996).
Simister, N. E., Story, C. M., Chen, H. L. & Hunt, J. S. An IgG‐transporting Fc receptor expressed in the syncytiotrophoblast of human placenta. Eur. J. Immunol. 26, 1527–1531 (1996).
Kristoffersen, E. K. & Matre, R. Co-localization of the neonatal Fcγ receptor and IgG in human placental term syncytiotrophoblasts. Eur. J. Immunol. 26, 1668–1671 (1996).
Cianga, P., Cianga, C., Cozma, L., Ward, E. S. & Carasevici, E. The MHC class I related Fc receptor, FcRn, is expressed in the epithelial cells of the human mammary gland. Hum. Immunol. 64, 1152–1159 (2003).
Szlauer, R. et al. Functional expression of the human neonatal Fc-receptor, hFcRn, in isolated cultured human syncytiotrophoblasts. Placenta 30, 507–515 (2009).
Ellinger, I., Schwab, M., Stefanescu, A., Hunziker, W. & Fuchs, R. IgG transport across trophoblast-derived BeWo cells: a model system to study IgG transport in the placenta. Eur. J. Immunol. 29, 733–744 (1999).
Firan, M. et al. The MHC class I-related receptor, FcRn, plays an essential role in the maternofetal transfer of γ-globulin in humans. Int. Immunol. 13, 993–1002 (2001). This study uncovered the role of FcRn in the transfer of IgGs from mother to offspring, using an ex vivo human placental model.
Antohe, F., Radulescu, L., Gafencu, A., Ghetie, V. & Simionescu, M. Expression of functionally active FcRn and the differentiated bidirectional transport of IgG in human placental endothelial cells. Hum. Immunol. 62, 93–105 (2001).
Radulescu, L., Antohe, F., Jinga, V., Ghetie, V. & Simionescu, M. Neonatal Fc receptors discriminates and monitors the pathway of native and modified immunoglobulin G in placental endothelial cells. Hum. Immunol. 65, 578–585 (2004).
Israel, E. J., Patel, V. K., Taylor, S. F., Marshak-Rothstein, A. & Simister, N. E. Requirement for a β 2-microglobulin-associated Fc receptor for acquisition of maternal IgG by fetal and neonatal mice. J. Immunol. 154, 6246–6251 (1995).
Kim, J. et al. FcRn in the yolk sac endoderm of mouse is required for IgG transport to fetus. J. Immunol. 182, 2583–2589 (2009).
Stapleton, N. M. et al. Human IgG lacking effector functions demonstrate lower FcRn-binding and reduced transplacental transport. Mol. Immunol. 95, 1–9 (2018).
Vaccaro, C., Bawdon, R., Wanjie, S., Ober, R. J. & Ward, E. S. Divergent activities of an engineered antibody in murine and human systems have implications for therapeutic antibodies. Proc. Natl Acad. Sci. USA 103, 18709–18714 (2006).
Roy, S. et al. M281, an anti-FcRn antibody, inhibits IgG transfer in a human ex vivo placental perfusion model. Am. J. Obstet. Gynecol. 220, 498.e1–498.e9 (2019).
Baker, K. et al. Neonatal Fc receptor expression in dendritic cells mediates protective immunity against colorectal cancer. Immunity 39, 1095–1107 (2013). This study discovered the role of FcRn in dendritic cell-mediated antitumour responses, through enhanced cross-presentation of antigen, which is complexed to IgGs, to CD8+ T cells.
Greinacher, A. Clinical practice. Heparin-induced thrombocytopenia. N. Engl. J. Med. 373, 252–261 (2015).
Chaturvedi, S. & McCrae, K. R. Diagnosis and management of the antiphospholipid syndrome. Blood Rev. 31, 406–417 (2017).
Ruggeri, M. & Rodeghiero, F. Thrombotic risk in patients with immune haemolytic anaemia. Br. J. Haematol. 172, 144–146 (2016).
Cines, D. B. et al. FcRn augments induction of tissue factor activity by IgG-containing immune complexes. Blood 135, 2085–2093 (2020).
Smith, B. et al. Generation of two high affinity anti-mouse FcRn antibodies: Inhibition of IgG recycling in wild type mice and effect in a mouse model of immune thrombocytopenia. Int. Immunopharmacol. 66, 362–365 (2019).
Liu, X. et al. The neonatal FcR-mediated presentation of immune-complexed antigen is associated with endosomal and phagosomal pH and antigen stability in macrophages and dendritic cells. J. Immunol. 186, 4674–4686 (2011).
Embgenbroich, M. & Burgdorf, S. Current concepts of antigen cross-presentation. Front. Immunol. 9, 1643 (2018).
Bhinder, G. et al. The Citrobacter rodentium mouse model: studying pathogen and host contributions to infectious colitis. J. Vis. Exp. 19, e50222 (2013).
Amadou Amani, S., Lang, G. A., Ballard, J. D. & Lang, M. L. The murine neonatal Fc receptor is required for transport of immunization-induced C. difficile-specific IgG to the gut and protection against disease but does not affect disease susceptibility. Infect. Immun. 89, e0027421 (2021).
Ben Suleiman, Y. et al. Neonatal Fc receptor for IgG (FcRn) expressed in the gastric epithelium regulates bacterial infection in mice. Mucosal Immunol. 5, 87–98 (2012).
Crowley, H., Alroy, J., Sproule, T. J., Roopenian, D. & Huber, B. T. The MHC class I-related FcRn ameliorates murine Lyme arthritis. Int. Immunol. 18, 409–414 (2006).
Kumamoto, Y. & Iwasaki, A. Unique features of antiviral immune system of the vaginal mucosa. Curr. Opin. Immunol. 24, 411–416 (2012).
Li, Z. et al. Transfer of IgG in the female genital tract by MHC class I-related neonatal Fc receptor (FcRn) confers protective immunity to vaginal infection. Proc. Natl Acad. Sci. Usa. 108, 4388–4393 (2011).
Scott, J. M. et al. Cellular and humoral immunity protect against vaginal Zika virus infection in mice. J. Virol. 92, e00038-18 (2018).
Bai, Y. et al. Intracellular neutralization of viral infection in polarized epithelial cells by neonatal Fc receptor (FcRn)-mediated IgG transport. Proc. Natl Acad. Sci. USA 108, 18406–18411 (2011).
Ochsner, S. P. et al. FcRn-targeted mucosal vaccination against influenza virus infection. J. Immunol. 207, 1310–1321 (2021).
Armitage, C. W. et al. Divergent outcomes following transcytosis of IgG targeting intracellular and extracellular chlamydial antigens. Immunol. Cell Biol. 92, 417–426 (2014).
Larsen, M. T. et al. FcRn overexpression in human cancer drives albumin recycling and cell growth; a mechanistic basis for exploitation in targeted albumin-drug designs. J. Control. Rel. 322, 53–63 (2020).
Uhlen, M. et al. A pathology atlas of the human cancer transcriptome. Science 357, eaan2507 (2017).
Castaneda, D. C. et al. Lack of FcRn impairs natural killer cell development and functions in the tumor microenvironment. Front. Immunol. 9, 2259 (2018).
Pasero, C. et al. Highly effective NK cells are associated with good prognosis in patients with metastatic prostate cancer. Oncotarget 6, 14360–14373 (2015).
Dalloneau, E. et al. Downregulation of the neonatal Fc receptor expression in non-small cell lung cancer tissue is associated with a poor prognosis. Oncotarget 7, 54415–54429 (2016).
Swiercz, R. et al. Loss of expression of the recycling receptor, FcRn, promotes tumor cell growth by increasing albumin consumption. Oncotarget 8, 3528–3541 (2017).
Liu, H. et al. KRAS-enhanced macropinocytosis and reduced FcRn-mediated recycling sensitize pancreatic cancer to albumin-conjugated drugs. J. Control. Rel. 296, 40–53 (2019).
Kamphorst, J. J. et al. Human pancreatic cancer tumors are nutrient poor and tumor cells actively scavenge extracellular protein. Cancer Res. 75, 544–553 (2015).
Jaggi, J. S. et al. Improved tumor imaging and therapy via i.v. IgG-mediated time-sequential modulation of neonatal Fc receptor. J. Clin. Invest. 117, 2422–2430 (2007).
Vilhelmsson Timmermand, O. et al. A conjugation strategy to modulate antigen binding and FcRn interaction leads to improved tumor targeting and radioimmunotherapy efficacy with an antibody targeting prostate-specific antigen. Cancers 13, 3469 (2021).
Devanaboyina, S. C., Khare, P., Challa, D. K., Ober, R. J. & Ward, E. S. Engineered clearing agents for the selective depletion of antigen-specific antibodies. Nat. Commun. 8, 15314 (2017).
Khare, P. et al. Selective depletion of radiolabeled HER2-specific antibody for contrast improvement during PET. mAbs 13, 1976705 (2021).
Ludwig, R. J. et al. Mechanisms of autoantibody-induced pathology. Front. Immunol. 8, 603 (2017).
Riedhammer, C. & Weissert, R. Antigen presentation, autoantigens, and immune regulation in multiple sclerosis and other autoimmune diseases. Front. Immunol. 6, 322 (2015).
Mitsuyama, K. et al. Antibody markers in the diagnosis of inflammatory bowel disease. World J. Gastroenterol. 22, 1304–1310 (2016).
Christianson, G. J. et al. β2-microglobulin dependence of the lupus-like autoimmune syndrome of MRL-lpr mice. J. Immunol. 156, 4932–4939 (1996).
Liu, Z. et al. β2-microglobulin-deficient mice are resistant to bullous pemphigoid. J. Exp. Med. 186, 777–783 (1997).
Li, N. et al. Complete FcRn dependence for intravenous Ig therapy in autoimmune skin blistering diseases. J. Clin. Invest. 115, 3440–3450 (2005).
Akilesh, S. et al. The MHC class I-like Fc receptor promotes humorally mediated autoimmune disease. J. Clin. Invest. 113, 1328–1333 (2004).
Kobayashi, K. et al. An FcRn-dependent role for anti-flagellin immunoglobulin G in pathogenesis of colitis in mice. Gastroenterology 137, 1746–1756.e1 (2009).
Sesarman, A., Sitaru, A. G., Olaru, F., Zillikens, D. & Sitaru, C. Neonatal Fc receptor deficiency protects from tissue injury in experimental epidermolysis bullosa acquisita. J. Mol. Med. 86, 951–959 (2008).
Kasprick, A. et al. Treatment with anti-neonatal Fc receptor (FcRn) antibody ameliorates experimental epidermolysis bullosa acquisita in mice. Br. J. Pharmacol. 177, 2381–2392 (2020).
Zhang, G., Lin, J., Ghauri, S. & Sheikh, K. A. Modulation of IgG–FcRn interactions to overcome antibody-mediated inhibition of nerve regeneration. Acta Neuropathol. 134, 321–324 (2017).
Challa, D. K. et al. Autoantibody depletion ameliorates disease in murine experimental autoimmune encephalomyelitis. mAbs 5, 655–659 (2013).
Sun, W. et al. Selective depletion of antigen-specific antibodies for the treatment of demyelinating disease. Mol. Ther. 29, 1312–1323 (2020).
Remlinger, J. et al. Antineonatal Fc receptor antibody treatment ameliorates MOG-IgG-associated experimental autoimmune encephalomyelitis. Neurol. Neuroimmunol. Neuroinflamm. 9, e1134 (2022).
Huijbers, M. G. et al. Efgartigimod improves muscle weakness in a mouse model for muscle-specific kinase myasthenia gravis. Exp. Neurol. 317, 133–143 (2019).
Liu, L. et al. Amelioration of experimental autoimmune myasthenia gravis in rats by neonatal FcR blockade. J. Immunol. 178, 5390–5398 (2007).
Monnet, C. et al. The dual targeting of FcRn and FcγRs via monomeric Fc fragments results in strong inhibition of IgG-dependent autoimmune pathologies. Front. Immunol. 12, 728322 (2021).
Patel, D. A. et al. Neonatal Fc receptor blockade by Fc engineering ameliorates arthritis in a murine model. J. Immunol. 187, 1015–1022 (2011).
Olaru, F. et al. Neonatal Fc receptor promotes immune complex-mediated glomerular disease. J. Am. Soc. Nephrol. 25, 918–925 (2014).
Dylewski, J. F., Tonsawan, P., Garcia, G., Lewis, L. & Blaine, J. Podocyte-specific knockout of the neonatal Fc receptor (FcRn) results in differential protection depending on the model of glomerulonephritis. PLoS ONE 15, e0230401 (2020).
Bhargava, R. et al. N-glycosylated IgG in patients with kidney transplants increases calcium/calmodulin kinase IV in podocytes and causes injury. Am. J. Transpl. 21, 148–160 (2021).
Ichinose, K. et al. Lupus nephritis IgG induction of calcium/calmodulin-dependent protein kinase IV expression in podocytes and alteration of their function. Arthritis Rheumatol. 68, 944–952 (2016).
Maeda, K. et al. CaMK4 compromises podocyte function in autoimmune and nonautoimmune kidney disease. J. Clin. Invest. 128, 3445–3459 (2018).
Castro-Dopico, T. & Clatworthy, M. R. Mucosal IgG in inflammatory bowel disease — a question of (sub)class? Gut Microbes 12, 1–9 (2020).
Dabritz, J. et al. Granulocyte macrophage colony-stimulating factor auto-antibodies and disease relapse in inflammatory bowel disease. Am. J. Gastroenterol. 108, 1901–1910 (2013).
Zakrzewicz, A. et al. Stabilization of keratinocyte monolayer integrity in the presence of anti-desmoglein-3 antibodies through FcRn blockade with efgartigimod: novel treatment paradigm for pemphigus? Cells 11, 942 (2022).
Hartmann, J. & Klein, H. G. Supply and demand for plasma-derived medicinal products - A critical reassessment amid the COVID-19 pandemic. Transfusion 60, 2748–2752 (2020).
Ulrichts, P. et al. Neonatal Fc receptor antagonist efgartigimod safely and sustainably reduces IgGs in humans. J. Clin. Invest. 128, 4372–4386 (2018). This study shows that blockade of FcRn with efgartigimod is safe and reduces serum IgGs in healthy humans.
Kiessling, P. et al. The FcRn inhibitor rozanolixizumab reduces human serum IgG concentration: a randomized phase 1 study. Sci. Transl. Med. 9, eaan1208 (2017). This paper reports that rozanolixizumab, an FcRn-blocking antibody, is safe and reduces serum IgGs in healthy humans.
Ling, L. et al. M281, an anti-FcRn antibody: pharmacodynamics, pharmacokinetics, and safety across the full range of IgG reduction in a first-in-human study. Clin. Pharmacol. Ther. 105, 1031–1039 (2018). This is a report that M281 (nipocalimab), an FcRn-blocking antibody, is safe in healthy humans and reduces total serum IgGs.
Yap, D. Y. H. et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of HBM9161, a novel FcRn inhibitor, in a phase I study for healthy Chinese volunteers. Clin. Transl. Sci. 14, 1769–1779 (2021). This article shows that HBM9161 (batoclimab) is a safe FcRn-blocking antibody that reduces serum IgGs in healthy humans.
Bril, V. et al. Efficacy and safety of rozanolixizumab in moderate to severe generalized myasthenia gravis: a phase 2 randomized control trial. Neurology 96, e853–e865 (2021).
Howard, J. F. Jr et al. Randomized phase 2 study of FcRn antagonist efgartigimod in generalized myasthenia gravis. Neurology 92, e2661–e2673 (2019).
Howard, J. F. Jr et al. Safety, efficacy, and tolerability of efgartigimod in patients with generalised myasthenia gravis (ADAPT): a multicentre, randomised, placebo-controlled, phase 3 trial. Lancet Neurol. 20, 526–536 (2021). This is a report of the largest study to date of an FcRn-blocking therapeutic, which has led to the approval of efgartigimod for the treatment of MG.
Robak, T. et al. Phase 2 multiple-dose study of an FcRn inhibitor, rozanolixizumab, in patients with primary immune thrombocytopenia. Blood Adv. 4, 4136–4146 (2020).
Newland, A. C. et al. Phase 2 study of efgartigimod, a novel FcRn antagonist, in adult patients with primary immune thrombocytopenia. Am. J. Hematol. 95, 178–187 (2020).
Goebeler, M. et al. Treatment of pemphigus vulgaris and foliaceus with efgartigimod, a neonatal Fc receptor inhibitor: a phase II multicentre, open-label feasibility trial. Br. J. Dermatol. 186, 429–439 (2021).
Yan, C. et al. Therapeutic effects of batoclimab in Chinese patients with generalized myasthenia gravis: a double-blinded, randomized, placebo-controlled phase II study. Neurol. Ther. 11, 815–834 (2022).
Gilhus, N. E. et al. Myasthenia gravis. Nat. Rev. Dis. Prim. 5, 30 (2019).
Schmidt, E., Kasperkiewicz, M. & Joly, P. Pemphigus. Lancet 394, 882–894 (2019).
Cooper, N. & Ghanima, W. Immune thrombocytopenia. N. Engl. J. Med. 381, 945–955 (2019).
Ishii-Watabe, A. et al. Genetic polymorphisms of FCGRT encoding FcRn in a Japanese population and their functional analysis. Drug. Metab. Pharmacokinet. 25, 578–587 (2010).
Passot, C. et al. Influence of FCGRT gene polymorphisms on pharmacokinetics of therapeutic antibodies. mAbs 5, 614–619 (2013).
O’Shannessy, D. J. et al. Correlation of FCGRT genomic structure with serum immunoglobulin, albumin and farletuzumab pharmacokinetics in patients with first relapsed ovarian cancer. Genomics 109, 251–257 (2017).
Ferguson, D. C. & Blanco, J. G. Regulation of the human Fc-neonatal receptor alpha-chain gene FCGRT by microRNA-3181. Pharm. Res. 35, 15 (2018).
Cejas, R. B., Ferguson, D. C., Quiñones-Lombraña, A., Bard, J. E. & Blanco, J. G. Contribution of DNA methylation to the expression of FCGRT in human liver and myocardium. Sci. Rep. 9, 8674 (2019).
Yeung, Y. A. et al. Engineering human IgG1 affinity to human neonatal Fc receptor: impact of affinity improvement on pharmacokinetics in primates. J. Immunol. 182, 7663–7671 (2009).
Deng, R. et al. Pharmacokinetics of humanized monoclonal anti-tumor necrosis factor-α antibody and its neonatal Fc receptor variants in mice and cynomolgus monkeys. Drug Metab. Dispos. 38, 600–605 (2010).
Ghetie, V. et al. Increasing the serum persistence of an IgG fragment by random mutagenesis. Nat. Biotechnol. 15, 637–640 (1997). This is the first discovery of mutations to the Fc region of an IgG fragment that can confer an enhanced serum half-life.
Dall’Acqua, W. F., Kiener, P. A. & Wu, H. Properties of human IgG1s engineered for enhanced binding to the neonatal Fc receptor (FcRn). J. Biol. Chem. 281, 23514–23524 (2006).
Zalevsky, J. et al. Enhanced antibody half-life improves in vivo activity. Nat. Biotechnol. 28, 157–159 (2010).
Lee, C.-H. et al. An engineered human Fc domain that behaves like a pH-toggle switch for ultra-long circulation persistence. Nat. Commun. 10, 5031 (2019).
Robbie, G. J. et al. A novel investigational Fc-modified humanized monoclonal antibody, motavizumab-YTE, has an extended half-life in healthy adults. Antimicrob. Agents Chemother. 57, 6147–6153 (2013).
Griffin, M. P. et al. Safety, tolerability, and pharmacokinetics of MEDI8897, the respiratory syncytial virus prefusion F-targeting monoclonal antibody with an extended half-life, in healthy adults. Antimicrob. Agents Chemother. 61, e01714–16 (2017).
Griffin, M. P. et al. Single-dose nirsevimab for prevention of RSV in preterm infants. N. Engl. J. Med. 383, 415–425 (2020).
Moreland, L. W. et al. Treatment of rheumatoid arthritis with a recombinant human tumor necrosis factor receptor (p75)–Fc fusion protein. N. Engl. J. Med. 337, 141–147 (1997).
Chaudhury, C., Brooks, C. L., Carter, D. C., Robinson, J. M. & Anderson, C. L. Albumin binding to FcRn: distinct from the FcRn-IgG interaction. Biochemistry 45, 4983–4990 (2006).
Andersen, J. T., Dee Qian, J. & Sandlie, I. The conserved histidine 166 residue of the human neonatal Fc receptor heavy chain is critical for the pH-dependent binding to albumin. Eur. J. Immunol. 36, 3044–3051 (2006).
Sand, K. M. et al. Dissection of the neonatal Fc receptor (FcRn)-albumin interface using mutagenesis and anti-FcRn albumin-blocking antibodies. J. Biol. Chem. 289, 17228–17239 (2014).
Andersen, J. T. et al. Structure-based mutagenesis reveals the albumin-binding site of the neonatal Fc receptor. Nat. Commun. 3, 610 (2012). This report shows the albumin binding site of FcRn, through mutagenesis experiments.
Nilsen, J. et al. Human and mouse albumin bind their respective neonatal Fc receptors differently. Sci. Rep. 8, 14648 (2018).
Tenten, V. et al. Albumin is recycled from the primary urine by tubular transcytosis. J. Am. Soc. Nephrol. 24, 1966–1980 (2013).
Pyzik, M. et al. Hepatic FcRn regulates albumin homeostasis and susceptibility to liver injury. Proc. Natl Acad. Sci. USA 114, E2862–E2871 (2017).
Eshbach, M. L. & Weisz, O. A. Receptor-mediated endocytosis in the proximal tubule. Annu. Rev. Physiol. 79, 425–448 (2017).
Richter, W. F. et al. Hematopoietic cells as site of first-pass catabolism after subcutaneous dosing and contributors to systemic clearance of a monoclonal antibody in mice. mAbs 10, 803–813 (2018).
Escobar, M. et al. IDELVION: a comprehensive review of clinical trial and real-world data. J. Clin. Med. https://doi.org/10.3390/jcm11041071 (2022).
van der Wal, F. J., Kikkert, M. & Wiertz, E. The HCMV gene products US2 and US11 target MHC class I molecules for degradation in the cytosol. Curr. Top. Microbiol. Immunol. 269, 37–55 (2002).
Liu, X. et al. Human cytomegalovirus evades antibody-mediated immunity through endoplasmic reticulum-associated degradation of the FcRn receptor. Nat. Commun. 10, 3020 (2019).
Gupta, S. et al. The neonatal Fc receptor (FcRn) enhances human immunodeficiency virus type 1 (HIV-1) transcytosis across epithelial cells. PLoS Pathog. 9, e1003776 (2013).
Chen, X., Schneewind, O. & Missiakas, D. Engineered human antibodies for the opsonization and killing of Staphylococcus aureus. Proc. Natl Acad. Sci. USA 119, e2114478119 (2022).
Kim, J. K., Tsen, M. F., Ghetie, V. & Ward, E. S. Identifying amino acid residues that influence plasma clearance of murine IgG1 fragments by site-directed mutagenesis. Eur. J. Immunol. 24, 542–548 (1994).
Sauer-Eriksson, A. E., Kleywegt, G. J., Uhlen, M. & Jones, T. A. Crystal structure of the C2 fragment of streptococcal protein G in complex with the Fc domain of human IgG. Structure 3, 265–278 (1995).
Martinez, D. R. et al. Fc characteristics mediate selective placental transfer of IgG in HIV-infected women. Cell 178, 190–201.e11 (2019).
Jennewein, M. F. et al. Fc glycan-mediated regulation of placental antibody transfer. Cell 178, 202–215.e14 (2019).
Mathiesen, L. et al. Maternofetal transplacental transport of recombinant IgG antibodies lacking effector functions. Blood 122, 1174–1181 (2013).
Borghi, S. et al. FcRn, but not FcγRs, drives maternal-fetal transplacental transport of human IgG antibodies. Proc. Natl Acad. Sci. USA 117, 12943–12951 (2020).
Tsao, N. W., Lynd, L. D., Sadatsafavi, M., Hanley, G. & De Vera, M. A. Patterns of biologics utilization and discontinuation before and during pregnancy in women with autoimmune diseases: a population-based cohort study. Arthritis Care Res. 70, 979–986 (2018).
De Felice, K. M. & Kane, S. Safety of anti-TNF agents in pregnancy. J. Allergy Clin. Immunol. 148, 661–667 (2021).
Verhasselt, V. et al. Breast milk-mediated transfer of an antigen induces tolerance and protection from allergic asthma. Nat. Med. 14, 170–175 (2008).
Mosconi, E. et al. Breast milk immune complexes are potent inducers of oral tolerance in neonates and prevent asthma development. Mucosal Immunol. 3, 461–474 (2010).
Culina, S. et al. Materno-fetal transfer of preproinsulin through the neonatal Fc receptor prevents autoimmune diabetes. Diabetes 64, 3532–3542 (2015).
Gupta, N. et al. Regulation of immune responses to protein therapeutics by transplacental induction of T cell tolerance. Sci. Transl. Med. 7, 275ra221 (2015).
Ohsaki, A. et al. Maternal IgG immune complexes induce food allergen-specific tolerance in offspring. J. Exp. Med. 215, 91–113 (2018).
Marchand, G. et al. Systematic review and meta-analysis of COVID-19 maternal and neonatal clinical features and pregnancy outcomes up to June 3, 2021. AJOG Glob. Rep. 2, 100049 (2022).
Male, V. SARS-CoV-2 infection and COVID-19 vaccination in pregnancy. Nat. Rev. Immunol. 22, 277–282 (2022).
de Moraes-Pinto, M. I. et al. Placental transfer and maternally acquired neonatal IgG immunity in human immunodeficiency virus infection. J. Infect. Dis. 173, 1077–1084 (1996).
Dechavanne, C. et al. Associations between an IgG3 polymorphism in the binding domain for FcRn, transplacental transfer of malaria-specific IgG3, and protection against Plasmodium falciparum malaria during infancy: a birth cohort study in Benin. PLoS Med. 14, e1002403 (2017).
de Moraes-Pinto, M. I. et al. Placental antibody transfer: influence of maternal HIV infection and placental malaria. Arch. Dis. Child. Fetal Neonatal Ed. 79, F202–F205 (1998).
Jones, C. E. et al. Maternal HIV infection and antibody responses against vaccine-preventable diseases in uninfected infants. JAMA 305, 576–584 (2011).
Singh, T. et al. Efficient transplacental IgG transfer in women infected with Zika virus during pregnancy. PLoS Negl. Trop. Dis. 13, e0007648 (2019).
Chen, P. et al. Animal model of fetal and neonatal immune thrombocytopenia: role of neonatal Fc receptor in the pathogenesis and therapy. Blood 116, 3660–3668 (2010).
Li, C. et al. The maternal immune response to fetal platelet GPIbα causes frequent miscarriage in mice that can be prevented by intravenous IgG and anti-FcRn therapies. J. Clin. Invest. 121, 4537–4547 (2011).
Garcia-Serra, A. et al. Blocking placental class G immunoglobulin transfer prevents NMDA receptor antibody effects in newborn mice. Neurol. Neuroimmunol. Neuroinflamm. 8, e1061 (2021).
Coutinho, E. et al. Inhibition of maternal-to-fetal transfer of IgG antibodies by FcRn blockade in a mouse model of arthrogryposis multiplex congenita. Neurol. Neuroimmunol. Neuroinflamm. 8, e1011 (2021).
Acknowledgements
We thank T. Hanley for assistance with revisions of the manuscript and D. Humphries for critical discussions. This work was funded by National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant DK053056, Harvard Digestive Diseases Center (HDDC) grant DK034854 and a Canadian Institutes of Health Research (CIHR) fellowship grant (L.K.K). Finally, we apologize to all colleagues whose work has not been included in this review owing to space limitations.
Author information
Authors and Affiliations
Contributions
M.P., L.K.K. and A.G. researched data for the article and together with R.S.B. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
R.S.B. had equity interests in Syntimmune Inc., a company developing therapeutic agents to target FcRn. Syntimmune Inc. was a wholly owned subsidiary of Alexion Pharmaceuticals Inc., which was acquired by AstraZeneca. M.P., L.K.K. and A.G. declare no competing interests.
Peer review
Peer review information
Nature Reviews Immunology thanks D. Roopenian and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
The Human Protein Atlas: https://www.proteinatlas.org/ENSG00000104870-FCGRT/single+cell+type
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pyzik, M., Kozicky, L.K., Gandhi, A.K. et al. The therapeutic age of the neonatal Fc receptor. Nat Rev Immunol 23, 415–432 (2023). https://doi.org/10.1038/s41577-022-00821-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41577-022-00821-1
This article is cited by
-
Non-specific irreversible 89Zr-mAb uptake in tumours: evidence from biopsy-proven target-negative tumours using 89Zr-immuno-PET
EJNMMI Research (2024)
-
The proteome of the blood–brain barrier in rat and mouse: highly specific identification of proteins on the luminal surface of brain microvessels by in vivo glycocapture
Fluids and Barriers of the CNS (2024)
-
The present and future of bispecific antibodies for cancer therapy
Nature Reviews Drug Discovery (2024)
-
Engineered serum markers for non-invasive monitoring of gene expression in the brain
Nature Biotechnology (2024)
-
FcRn regulates antigen presentation in dendritic cells downstream of DEC205-targeted vaccines
npj Vaccines (2024)