Abstract
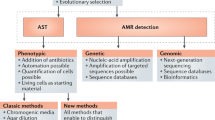
Antimicrobial resistance extracts high morbidity, mortality and economic costs yearly by rendering bacteria immune to antibiotics. Identifying and understanding antimicrobial resistance are imperative for clinical practice to treat resistant infections and for public health efforts to limit the spread of resistance. Technologies such as next-generation sequencing are expanding our abilities to detect and study antimicrobial resistance. This Review provides a detailed overview of antimicrobial resistance identification and characterization methods, from traditional antimicrobial susceptibility testing to recent deep-learning methods. We focus on sequencing-based resistance discovery and discuss tools and databases used in antimicrobial resistance studies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cosgrove, S. E. & Carmeli, Y. The impact of antimicrobial resistance on health and economic outcomes. Clin. Infect. Dis. 36, 1433–1437 (2003).
Hawkey, P. M. The growing burden of antimicrobial resistance. J. Antimicrob. Chemother. 62 (Suppl. 1), i1–i9 (2008).
Acar, J. F. Consequences of bacterial resistance to antibiotics in medical practice. Clin. Infect. Dis. 24 (Suppl. 1), 17–18 (1997).
Cosgrove, S. E. The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clin. Infect. Dis. 42 (Suppl. 2), 82–89 (2006).
Tillotson, G. S. & Zinner, S. H. Burden of antimicrobial resistance in an era of decreasing susceptibility. Expert Rev. Anti. Infect. Ther. 15, 663–676 (2017).
Poirel, L. & Nordmann, P. Carbapenem resistance in Acinetobacter baumannii: mechanisms and epidemiology. Clin. Microbiol. Infect. 12, 826–836 (2006).
Johnson, A. P. & Woodford, N. Global spread of antibiotic resistance: the example of New Delhi metallo-beta-lactamase (NDM)-mediated carbapenem resistance. J. Med. Microbiol. 62, 499–513 (2013).
Gupta, N., Limbago, B. M., Patel, J. B. & Kallen, A. J. Carbapenem-resistant enterobacteriaceae: epidemiology and prevention. Clin. Infect. Dis. 53, 60–67 (2011).
Liu, Y. Y. et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect. Dis. 16, 161–168 (2016).
Ventola, C. L. The antibiotic resistance crisis: part 1: causes and threats. P T 40, 277–283 (2015).
Centers for Disease Control and Prevention. Antibiotic/antimicrobial resistance (AR/AMR): biggest threats and data. CDC http://www.cdc.gov/drugresistance/threat-report-2013/ (updated 26 Nov 2018).
Smith, R. & Coast, J. The true cost of antimicrobial resistance. BMJ 346, f1493 (2013).
O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations (Review on Antimicrobial Resistance, 2016).
Cassini, A. et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet. Infect. Dis. 19, 56–66 (2019). This paper demonstrates the impact of antimicrobial resistance on the health-care system and identifies major priorities for future mitigation efforts.
World Health Organization. Global Action Plan on Antimicrobial Resistance 2015 (Report No. 9789241509763) (WHO, 2015).
Tacconelli, E. et al. Surveillance for control of antimicrobial resistance. Lancet. Infect. Dis. 18, e99–e106 (2018).
Wernli, D. et al. Mapping global policy discourse on antimicrobial resistance. BMJ Global Health 2, e000378 (2017).
Didelot, X., Bowden, R., Wilson, D. J., Peto, T. E. & Crook, D. W. Transforming clinical microbiology with bacterial genome sequencing. Nat. Rev. Genet. 13, 601–612 (2012).
D’Costa, V. M., McGrann, K. M., Hughes, D. W. & Wright, G. D. Sampling the antibiotic resistome. Science 311, 374–377 (2006). This article shows that soil bacteria are a reservoir for resistance determinants.
Wang, R. et al. The global distribution and spread of the mobilized colistin resistance gene mcr-1. Nat. Commun. 9, 1179 (2018).
Nordmann, P., Naas, T. & Poirel, L. Global spread of carbapenemase-producing Enterobacteriaceae. Emerg. Infect. Dis. 17, 1791–1798 (2011).
Canton, R. et al. Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin. Microbiol. Infect. 18, 413–431 (2012).
Potter, R. F., D’Souza, A. W. & Dantas, G. The rapid spread of carbapenem-resistant Enterobacteriaceae. Drug Resist. Updat. 29, 30–46 (2016).
Pesesky, M. W. et al. KPC and NDM-1 genes in related Enterobacteriaceae strains and plasmids from Pakistan and the United States. Emerg. Infect. Dis. 21, 1034–1037 (2015).
Pehrsson, E. C. et al. Interconnected microbiomes and resistomes in low-income human habitats. Nature 533, 212–216 (2016).
Gibson, M. K., Forsberg, K. J. & Dantas, G. Improved annotation of antibiotic resistance determinants reveals microbial resistomes cluster by ecology. ISME J. 9, 207–216 (2015). This paper describes the creation of a profile HMM-based resistance database and presents an application of this database showing that environmental-based and human-based samples have different resistance profiles.
Bankevich, A. et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 19, 455–477 (2012).
Zerbino, D. R. & Birney, E. Velvet: algorithms for de novo short read assembly using de Bruijn graphs. Genome Res. 18, 821–829 (2008).
Simpson, J. T. et al. ABySS: a parallel assembler for short read sequence data. Genome Res. 19, 1117–1123 (2009).
Luo, R. et al. SOAPdenovo2: an empirically improved memory-efficient short-read de novo assembler. Gigascience 1, 18 (2012).
Compeau, P. E., Pevzner, P. A. & Tesler, G. How to apply de Bruijn graphs to genome assembly. Nat. Biotechnol. 29, 987–991 (2011). This short paper explains how DBGs are used in genome assembly.
Ghurye, J. S., Cepeda-Espinoza, V. & Pop, M. Metagenomic assembly: overview, challenges and applications. Yale J. Biol. Med. 89, 353–362 (2016).
Miller, J. R., Koren, S. & Sutton, G. Assembly algorithms for next-generation sequencing data. Genomics 95, 315–327 (2010).
Antipov, D. et al. plasmidSPAdes: assembling plasmids from whole genome sequencing data. Bioinformatics 32, 3380–3387 (2016).
Rozov, R. et al. Recycler: an algorithm for detecting plasmids from de novo assembly graphs. Bioinformatics 33, 475–482 (2017).
Roosaare, M., Puustusmaa, M., Mols, M., Vaher, M. & Remm, M. PlasmidSeeker: identification of known plasmids from bacterial whole genome sequencing reads. PeerJ 6, e4588 (2018).
Lanza, V. F. et al. Plasmid flux in Escherichia coli ST131 sublineages, analyzed by plasmid constellation network (PLACNET), a new method for plasmid reconstruction from whole genome sequences. PLOS Genet. 10, e1004766 (2014).
Peng, Y., Leung, H. C., Yiu, S. M. & Chin, F. Y. IDBA-UD: a de novo assembler for single-cell and metagenomic sequencing data with highly uneven depth. Bioinformatics 28, 1420–1428 (2012).
Li, D., Liu, C. M., Luo, R., Sadakane, K. & Lam, T. W. MEGAHIT: an ultra-fast single-node solution for large and complex metagenomics assembly via succinct de Bruijn graph. Bioinformatics 31, 1674–1676 (2015).
Nurk, S., Meleshko, D., Korobeynikov, A. & Pevzner, P. A. metaSPAdes: a new versatile metagenomic assembler. Genome Res. 27, 824–834 (2017).
Namiki, T., Hachiya, T., Tanaka, H. & Sakakibara, Y. MetaVelvet: an extension of Velvet assembler to de novo metagenome assembly from short sequence reads. Nucleic Acids Res. 40, e155 (2012). Peng et al. (2012), Li et al. (2015), Nurk et al. (2017) and Namiki et al. (2012) are method papers of metagenomic assemblers developed to assemble complex metagenomics data sets with uneven sequencing depths.
Sczyrba, A. et al. Critical assessment of metagenome interpretation-a benchmark of metagenomics software. Nat. Methods 14, 1063–1071 (2017).
Bremges, A. & McHardy, A. C. Critical assessment of metagenome interpretation enters the second round. mSystems 3, e00103-18 (2018). Together with Sczyrba et al., this paper describes the CAMI project designed to evaluate the differences between different metagenomics tools for metagenomic assembly, taxonomic classification and assembled contig binning.
Altschul, S. F., Gish, W., Miller, W., Myers, E. W. & Lipman, D. J. Basic local alignment search tool. J. Mol. Biol. 215, 403–410 (1990).
Edgar, R. C. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26, 2460–2461 (2010).
Buchfink, B., Xie, C. & Huson, D. H. Fast and sensitive protein alignment using DIAMOND. Nat. Methods 12, 59–60 (2015).
Werner, J. J. et al. Impact of training sets on classification of high-throughput bacterial 16s rRNA gene surveys. ISME J. 6, 94–103 (2012).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Inouye, M. et al. SRST2: rapid genomic surveillance for public health and hospital microbiology labs. Genome Med. 6, 90 (2014).
Clausen, P. T., Zankari, E., Aarestrup, F. M. & Lund, O. Benchmarking of methods for identification of antimicrobial resistance genes in bacterial whole genome data. J. Antimicrob. Chemother. 71, 2484–2488 (2016).
Hunt, M. et al. ARIBA: rapid antimicrobial resistance genotyping directly from sequencing reads. Microb. Genom. 3, e000131 (2017).
Fu, L., Niu, B., Zhu, Z., Wu, S. & Li, W. CD-HIT: accelerated for clustering the next-generation sequencing data. Bioinformatics 28, 3150–3152 (2012).
Rowe, W. et al. Search engine for antimicrobial resistance: a cloud compatible pipeline and web interface for rapidly detecting antimicrobial resistance genes directly from sequence data. PLOS ONE 10, e0133492 (2015).
Munk, P. et al. A sampling and metagenomic sequencing-based methodology for monitoring antimicrobial resistance in swine herds. J. Antimicrob. Chemother. 72, 385–392 (2017).
Rowe, W. P. M. & Winn, M. D. Indexed variation graphs for efficient and accurate resistome profiling. Bioinformatics 34, 3601–3608 (2018).
Langmead, B., Trapnell, C., Pop, M. & Salzberg, S. L. Ultrafast and memory-efficient alignment of short DNA sequences to the human genome. Genome Biol. 10, R25 (2009).
Henson, J., Tischler, G. & Ning, Z. Next-generation sequencing and large genome assemblies. Pharmacogenomics 13, 901–915 (2012).
Carr, R. & Borenstein, E. Comparative analysis of functional metagenomic annotation and the mappability of short reads. PLOS ONE 9, e105776 (2014).
Quince, C., Walker, A. W., Simpson, J. T., Loman, N. J. & Segata, N. Shotgun metagenomics, from sampling to analysis. Nat. Biotechnol. 35, 833–844 (2017). This detailed review discusses the best strategies used in shotgun metagenomics studies.
Kaminski, J. et al. High-specificity targeted functional profiling in microbial communities with ShortBRED. PLOS Comput. Biol. 11, e1004557 (2015).
Gibson, M. K. et al. Developmental dynamics of the preterm infant gut microbiota and antibiotic resistome. Nat. Microbiol. 1, 16024 (2016).
Tsukayama, P. et al. Characterization of wild and captive baboon gut microbiota and their antibiotic resistomes. mSystems 3, e00016-18 (2018).
Hsu, T. et al. Urban transit system microbial communities differ by surface type and interaction with humans and the environment. mSystems 1, e00018-16 (2016).
Liu, B. & Pop, M. ARDB—antibiotic resistance genes database. Nucleic Acids Res 37, D443–D447 (2009). ARDB was one of the first general antimicrobial resistance gene databases, and this paper spawned several other efforts to compile resistance gene information across drug classes and bacterial species.
Gupta, S. K. et al. ARG-ANNOT, a new bioinformatic tool to discover antibiotic resistance genes in bacterial genomes. Antimicrob. Agents Chemother. 58, 212–220 (2014).
Jia, B. et al. CARD 2017: expansion and model-centric curation of the comprehensive antibiotic resistance database. Nucleic Acids Res. 45, D566–D573 (2017). This paper describes recent updates to the CARD and tools that are associated with the database.
Thai, Q. K. & Pleiss, J. SHV lactamase engineering database: a reconciliation tool for SHV beta-lactamases in public databases. BMC Genomics 11, 563 (2010).
Thai, Q. K., Bos, F. & Pleiss, J. The lactamase engineering database: a critical survey of TEM sequences in public databases. BMC Genomics 10, 390 (2009).
Bush, K. & Jacoby, G. A. Updated functional classification of β-lactamases. Antimicrob. Agents Chemother. 54, 969–976 (2010).
Srivastava, A., Singhal, N., Goel, M., Virdi, J. S. & Kumar, M. CBMAR: a comprehensive beta-lactamase molecular annotation resource. Database (Oxford) 2014, bau111 (2014).
Zankari, E. et al. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 67, 2640–2644 (2012). This article describes Resfinder, a widely used tool for the identification of acquired antimicrobial resistance genes in whole-genome data.
Zankari, E. et al. PointFinder: a novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. J. Antimicrob. Chemother. 72, 2764–2768 (2017).
Yin, X. et al. ARGs-OAP v2.0 with an expanded SARG database and hidden Markov models for enhancement characterization and quantification of antibiotic resistance genes in environmental metagenomes. Bioinformatics 34, 2263–2270 (2018).
Sandgren, A. et al. Tuberculosis drug resistance mutation database. PLOS Med. 6, e2 (2009).
Flandrois, J. P., Lina, G. & Dumitrescu, O. MUBII-TB-DB: a database of mutations associated with antibiotic resistance in Mycobacterium tuberculosis. BMC Bioinformatics 15, 107 (2014).
Cox, G. & Wright, G. D. Intrinsic antibiotic resistance: mechanisms, origins, challenges and solutions. Int. J. Med. Microbiol. 303, 287–292 (2013).
Gygli, S. M., Borrell, S., Trauner, A. & Gagneux, S. Antimicrobial resistance in Mycobacterium tuberculosis: mechanistic and evolutionary perspectives. FEMS Microbiol. Rev. 41, 354–373 (2017).
Allix-Beguec, C. et al. Prediction of susceptibility to first-line tuberculosis drugs by DNA sequencing. N. Engl. J. Med. 379, 1403–1415 (2018). This paper shows the effectiveness of a sequencing approach to phenotypic antimicrobial resistance predictions in M. tuberculosis.
McArthur, A. G. & Tsang, K. K. Antimicrobial resistance surveillance in the genomic age. Ann. NY Acad. Sci. 1388, 78–91 (2017).
Yelin, I. & Kishony, R. Antibiotic resistance. Cell 172, 1136–1136 (2018).
Eddy, S. R. Profile hidden Markov models. Bioinformatics 14, 755–763 (1998).
Wallace, J. C., Port, J. A., Smith, M. N. & Faustman, E. M. FARME DB: a functional antibiotic resistance element database. Database (Oxford) 2017, baw165 (2017). This paper compiles putative resistance determinants from functional antimicrobial selections in public databases to identify resistance determinants that are not well represented in databases built primarily from clinical bacterial isolates.
Munk, P. et al. Abundance and diversity of the faecal resistome in slaughter pigs and broilers in nine European countries. Nat. Microbiol. 3, 898–908 (2018). This article presents a new technique for identifying antimicrobial resistance determinants by including 3D information.
Ruppe, E. et al. Prediction of the intestinal resistome by a three-dimensional structure-based method. Nat. Microbiol. 4, 112–123 (2019).
Xavier, B. B. et al. Consolidating and exploring antibiotic resistance gene data resources. J. Clin. Microbiol. 54, 851–859 (2016).
Hall, R. M. & Schwarz, S. Resistance gene naming and numbering: is it a new gene or not? J. Antimicrob. Chemother. 71, 569–571 (2016).
Carnevali, C. et al. Occurrence of mcr-1 in colistin-resistant salmonella enterica isolates recovered from humans and animals in Italy, 2012 to 2015. Antimicrob. Agents Chemother. 60, 7532–7534 (2016).
Ortega-Paredes, D., Barba, P. & Zurita, J. Colistin-resistant Escherichia coli clinical isolate harbouring the mcr-1 gene in Ecuador. Epidemiol. Infect. 144, 2967–2970 (2016).
Teo, J. Q. et al. mcr-1 in multidrug-resistant blaKPC-2-producing clinical enterobacteriaceae isolates in Singapore. Antimicrob. Agents Chemother. 60, 6435–6437 (2016).
Fernandes, M. R. et al. First report of the globally disseminated IncX4 plasmid carrying the mcr-1 gene in a colistin-resistant Escherichia coli sequence type 101 isolate from a human infection in Brazil. Antimicrob. Agents Chemother. 60, 6415–6417 (2016).
Delgado-Blas, J. F., Ovejero, C. M., Abadia-Patino, L. & Gonzalez-Zorn, B. Coexistence of mcr-1 and blaNDM-1 in Escherichia coli from Venezuela. Antimicrob. Agents Chemother. 60, 6356–6358 (2016).
Kline, K. E. et al. Investigation of first identified mcr-1 gene in an isolate from a U. S. patient - Pennsylvania, 2016. MMWR Morb. Mortal. Wkly. Rep. 65, 977–978 (2016).
Wong, S. C. et al. Colistin-resistant enterobacteriaceae carrying the mcr-1 gene among patients in Hong Kong. Emerg. Infect. Dis. 22, 1667–1669 (2016).
Brauer, A. et al. Plasmid with colistin resistance gene mcr-1 in extended-spectrum-beta-lactamase-producing Escherichia coli strains isolated from pig slurry in Estonia. Antimicrob. Agents Chemother. 60, 6933–6936 (2016).
von Wintersdorff, C. J. et al. Detection of the plasmid-mediated colistin-resistance gene mcr-1 in faecal metagenomes of Dutch travellers. J. Antimicrob. Chemother. 71, 3416–3419 (2016).
Crofts, T. S., Gasparrini, A. J. & Dantas, G. Next-generation approaches to understand and combat the antibiotic resistome. Nat. Rev. Microbiol. 15, 422–434 (2017).
Riesenfeld, C. S. et al. Uncultured soil bacteria are a reservoir of new antibiotic resistance genes. Environ. Microbiol. 6, 981–989 (2015). This is one of the initial studies to demonstrate the application of functional metagenomic selections for discovering novel antibiotic resistance genes.
Pehrsson, E. C., Forsberg, K. J., Gibson, M. K., Ahmadi, S. & Dantas, G. Novel resistance functions uncovered using functional metagenomic investigations of resistance reservoirs. Front. Microbiol 4, 145 (2013).
Forsberg, K. J. et al. The shared antibiotic resistome of soil bacteria and human pathogens. Science 337, 1107–1111 (2012). This paper applies a functional metagenomics approach and assembly pipeline to show evidence of resistance gene exchange between human pathogens and soil bacteria.
de la Bastide, M. & McCombie, W. R. Assembling genomic DNA sequences with PHRAP. Curr. Protoc. Bioinformatics 17, 11.4.1–11.4.15 (2007).
Zhu, W., Lomsadze, A. & Borodovsky, M. Ab initio gene identification in metagenomic sequences. Nucleic Acids Res. 38, e132 (2010).
Torres-Cortes, G. et al. Characterization of novel antibiotic resistance genes identified by functional metagenomics on soil samples. Environ. Microbiol. 13, 1101–1114 (2011).
Forsberg, K. J., Patel, S., Wencewicz, T. A. & Dantas, G. The tetracycline destructases: a novel family of tetracycline-inactivating enzymes. Chem. Biol. 22, 888–897 (2015).
Martinez, A. et al. Genetically modified bacterial strains and novel bacterial artificial chromosome shuttle vectors for constructing environmental libraries and detecting heterologous natural products in multiple expression hosts. Appl. Environ. Microbiol. 70, 2452–2463 (2004).
Dantas, G. & Sommer, M. O. Context matters - the complex interplay between resistome genotypes and resistance phenotypes. Curr. Opin. Microbiol. 15, 577–582 (2012). This article covers the importance of genomic context in understanding how genotypic resistance determinants result in varied phenotypic antimicrobial susceptibility profiles.
Rishishwar, L., Petit, R. A. 3rd, Kraft, C. S. & Jordan, I. K. Genome sequence-based discriminator for vancomycin-intermediate Staphylococcus aureus. J. Bacteriol. 196, 940–948 (2014).
Bradley, P. et al. Rapid antibiotic-resistance predictions from genome sequence data for Staphylococcus aureus and Mycobacterium tuberculosis. Nat. Commun. 6, 10063 (2015).
Davis, J. J. et al. Antimicrobial resistance prediction in PATRIC and RAST. Sci. Rep. 6, 27930 (2016).
Arango-Argoty, G. et al. DeepARG: a deep learning approach for predicting antibiotic resistance genes from metagenomic data. Microbiome 6, 23 (2018).
LeCun, Y., Bengio, Y. & Hinton, G. Deep learning. Nature 521, 436–444 (2015).
Baroud, M. et al. Underlying mechanisms of carbapenem resistance in extended-spectrum beta-lactamase-producing Klebsiella pneumoniae and Escherichia coli isolates at a tertiary care centre in Lebanon: role of OXA-48 and NDM-1 carbapenemases. Int. J. Antimicrob. Agents 41, 75–79 (2013).
Shigemura, K. et al. Association of overexpression of efflux pump genes with antibiotic resistance in Pseudomonas aeruginosa strains clinically isolated from urinary tract infection patients. J. Antibiot. 68, 568–572 (2015).
Depardieu, F., Podglajen, I., Leclercq, R., Collatz, E. & Courvalin, P. Modes and modulations of antibiotic resistance gene expression. Clin. Microbiol. Rev. 20, 79–114 (2007).
Isenberg, H. D. Clinical microbiology: past, present, and future. J. Clin. Microbiol. 41, 917–918 (2003).
Bauer, A. W., Kirby, W. M., Sherris, J. C. & Turck, M. Antibiotic susceptibility testing by a standardized single disk method. Am. J. Clin. Pathol. 45, 493–496 (1966).
Brown, D. F. & Brown, L. Evaluation of the E test, a novel method of quantifying antimicrobial activity. J. Antimicrob. Chemother. 27, 185–190 (1991).
Jorgensen, J. H. & Ferraro, M. J. Antimicrobial susceptibility testing: a review of general principles and contemporary practices. Clin. Infect. Dis. 49, 1749–1755 (2009). This is a review of traditional microbiology techniques and of several automation innovations, including disc diffusion, microbroth dilution and a Vitek system.
Seng, P. et al. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin. Infect. Dis. 49, 543–551 (2009).
Nagy, E., Maier, T., Urban, E., Terhes, G. & Kostrzewa, M. Species identification of clinical isolates of Bacteroides by matrix-assisted laser-desorption/ionization time-of-flight mass spectrometry. Clin. Microbiol. Infect. 15, 796–802 (2009).
Eigner, U. et al. Performance of a matrix-assisted laser desorption ionization-time-of-flight mass spectrometry system for the identification of bacterial isolates in the clinical routine laboratory. Clin. Lab. 55, 289–296 (2009).
Vrioni, G. et al. MALDI-TOF mass spectrometry technology for detecting biomarkers of antimicrobial resistance: current achievements and future perspectives. Ann. Transl Med. 6, 240 (2018).
Kostrzewa, M., Sparbier, K., Maier, T. & Schubert, S. MALDI-TOF MS: an upcoming tool for rapid detection of antibiotic resistance in microorganisms. Proteomics Clin. Appl. 7, 767–778 (2013).
Sparbier, K., Schubert, S. & Kostrzewa, M. MBT-ASTRA: a suitable tool for fast antibiotic susceptibility testing? Methods 104, 48–54 (2016).
Yilmaz, O. & Demiray, E. Clinical role and importance of fluorescence in situ hybridization method in diagnosis of H pylori infection and determination of clarithromycin resistance in H pylori eradication therapy. World J. Gastroenterol. 13, 671–675 (2007).
Moter, A. & Gobel, U. B. Fluorescence in situ hybridization (FISH) for direct visualization of microorganisms. J. Microbiol. Methods 41, 85–112 (2000).
Juttner, S. et al. Reliable detection of macrolide-resistant Helicobacter pylori via fluorescence in situ hybridization in formalin-fixed tissue. Mod. Pathol. 17, 684–689 (2004).
Haas, M., Essig, A., Bartelt, E. & Poppert, S. Detection of resistance to macrolides in thermotolerant campylobacter species by fluorescence in situ hybridization. J. Clin. Microbiol. 46, 3842–3844 (2008).
Werner, G. et al. Detection of mutations conferring resistance to linezolid in Enterococcus spp. by fluorescence in situ hybridization. J. Clin. Microbiol. 45, 3421–3423 (2007).
Choi, J. et al. A rapid antimicrobial susceptibility test based on single-cell morphological analysis. Sci. Transl Med. 6, 267ra174 (2014).
Kalashnikov, M. et al. Rapid phenotypic stress-based microfluidic antibiotic susceptibility testing of Gram-negative clinical isolates. Sci. Rep. 7, 8031 (2017).
Mohan, R. et al. A multiplexed microfluidic platform for rapid antibiotic susceptibility testing. Biosens. Bioelectron. 49, 118–125 (2013).
Hou, H. W., Bhattacharyya, R. P., Hung, D. T. & Han, J. Direct detection and drug-resistance profiling of bacteremias using inertial microfluidics. Lab. Chip 15, 2297–2307 (2015).
Baltekin, O., Boucharin, A., Tano, E., Andersson, D. I. & Elf, J. Antibiotic susceptibility testing in less than 30 min using direct single-cell imaging. Proc. Natl Acad. Sci. USA 114, 9170–9175 (2017).
Choi, J. et al. Rapid drug susceptibility test of Mycobacterium tuberculosis using microscopic time-lapse imaging in an agarose matrix. Appl. Microbiol. Biotechnol. 100, 2355–2365 (2016).
Seki, M., Kim, C. K., Hayakawa, S. & Mitarai, S. Recent advances in tuberculosis diagnostics in resource-limited settings. Eur. J. Clin. Microbiol. Infect. Dis. 37, 1405–1410 (2018).
Wolfe, A. J. et al. Evidence of uncultivated bacteria in the adult female bladder. J. Clin. Microbiol. 50, 1376–1383 (2012).
Rudkjobing, V. B. et al. Comparing culture and molecular methods for the identification of microorganisms involved in necrotizing soft tissue infections. BMC Infect. Dis. 16, 652 (2016).
Fok, C. S. et al. Urinary symptoms are associated with certain urinary microbes in urogynecologic surgical patients. Int. Urogynecol. J. 29, 1765–1771 (2018).
Mowat, A. Commentary on: urinary symptoms are associated with certain urinary microbes in urogynecologic surgical patients. Int. Urogynecol. J. 29, 1773 (2018).
Patel, J. B., Tenover, F. C., Turnidge, J. D. & Jorgensen, J. H. in Manual of Clinical Microbiology 10th edn (eds Versalovic, J. et al.) (American Society for Microbiology, 2011).
Shetty, N., Hill, G. & Ridgway, G. L. The Vitek analyser for routine bacterial identification and susceptibility testing: protocols, problems, and pitfalls. J. Clin. Pathol. 51, 316–323 (1998).
Idelevich, E. A. et al. Evaluation of an automated system for reading and interpreting disk diffusion antimicrobial susceptibility testing of fastidious bacteria. PLOS ONE 11, e0159183 (2016).
Lutgring, J. D. et al. Evaluation of the accelerate pheno system: results from two academic medical centers. J. Clin. Microbiol. 56, e01672-17 (2018).
Marschal, M. et al. Evaluation of the accelerate pheno system for fast identification and antimicrobial susceptibility testing from positive blood cultures in bloodstream infections caused by gram-negative pathogens. J. Clin. Microbiol. 55, 2116–2126 (2017).
Florio, W., Morici, P., Ghelardi, E., Barnini, S. & Lupetti, A. Recent advances in the microbiological diagnosis of bloodstream infections. Crit. Rev. Microbiol. 44, 351–370 (2018).
Peker, N., Couto, N., Sinha, B. & Rossen, J. W. Diagnosis of bloodstream infections from positive blood cultures and directly from blood samples: recent developments in molecular approaches. Clin. Microbiol. Infect. 24, 944–955 (2018).
Fredborg, M. et al. Rapid antimicrobial susceptibility testing of clinical isolates by digital time-lapse microscopy. Eur. J. Clin. Microbiol. Infect. Dis. 34, 2385–2394 (2015).
Dekker, J., Rippe, K., Dekker, M. & Kleckner, N. Capturing chromosome conformation. Science 295, 1306–1311 (2002).
Hakim, O. & Misteli, T. SnapShot: chromosome confirmation capture. Cell 148, 1068–1068.e2 (2012).
Trussart, M. et al. Defined chromosome structure in the genome-reduced bacterium Mycoplasma pneumoniae. Nat. Commun. 8, 14665 (2017).
Yildirim, A. & Feig, M. High-resolution 3D models of Caulobacter crescentus chromosome reveal genome structural variability and organization. Nucleic Acids Res. 46, 3937–3952 (2018).
Marbouty, M., Baudry, L., Cournac, A. & Koszul, R. Scaffolding bacterial genomes and probing host-virus interactions in gut microbiome by proximity ligation (chromosome capture) assay. Sci. Adv. 3, e1602105 (2017).
Stewart, R. D. et al. Assembly of 913 microbial genomes from metagenomic sequencing of the cow rumen. Nat. Commun. 9, 870 (2018).
Press, M. O. et al. Hi-C deconvolution of a human gut microbiome yields high-quality draft genomes and reveals plasmid-genome interactions. Preprint at bioRxiv https://doi.org/10.1101/198713 (2017).
Eid, J. et al. Real-time DNA sequencing from single polymerase molecules. Science 323, 133–138 (2009).
Clarke, J. et al. Continuous base identification for single-molecule nanopore DNA sequencing. Nat. Nanotechnol. 4, 265–270 (2009).
Wick, R. R., Judd, L. M., Gorrie, C. L. & Holt, K. E. Completing bacterial genome assemblies with multiplex MinION sequencing. Microb. Genom. 3, e000132 (2017).
Liao, Y. C., Lin, S. H. & Lin, H. H. Completing bacterial genome assemblies: strategy and performance comparisons. Sci. Rep. 5, 8747 (2015).
Wick, R. R., Judd, L. M., Gorrie, C. L. & Holt, K. E. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLOS Comput. Biol. 13, e1005595 (2017).
Frank, J. A. et al. Improved metagenome assemblies and taxonomic binning using long-read circular consensus sequence data. Sci. Rep. 6, 25373 (2016).
Driscoll, C. B., Otten, T. G., Brown, N. M. & Dreher, T. W. Towards long-read metagenomics: complete assembly of three novel genomes from bacteria dependent on a diazotrophic cyanobacterium in a freshwater lake co-culture. Stand. Genomic. Sci. 12, 9 (2017).
Beaulaurier, J. et al. Metagenomic binning and association of plasmids with bacterial host genomes using DNA methylation. Nat. Biotechnol. 36, 61–69 (2018).
Bertrand, D. et al. Nanopore sequencing enables high-resolution analysis of resistance determinants and mobile elements in the human gut microbiome. Preprint at bioRxiv https://doi.org/10.1101/456905 (2018).
Břinda, K. et al. Lineage calling can identify antibiotic resistant clones within minutes. Preprint at bioRxiv https://doi.org/10.1101/403204 (2018).
Croucher, N. J. & Thomson, N. R. Studying bacterial transcriptomes using RNA-seq. Curr. Opin. Microbiol. 13, 619–624 (2010).
Wang, Z., Gerstein, M. & Snyder, M. RNA-Seq: a revolutionary tool for transcriptomics. Nat. Rev. Genet. 10, 57–63 (2009).
Dersch, P., Khan, M. A., Muhlen, S. & Gorke, B. Roles of regulatory RNAs for antibiotic resistance in bacteria and their potential value as novel drug targets. Front. Microbiol. 8, 803 (2017).
Khaledi, A. et al. Transcriptome profiling of antimicrobial resistance in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 60, 4722–4733 (2016).
Suzuki, S., Horinouchi, T. & Furusawa, C. Prediction of antibiotic resistance by gene expression profiles. Nat. Commun. 5, 5792 (2014). This paper uses expression profiles to help predict phenotypic resistance from genotypic data, showing the power of combining multiple omics techniques.
Qin, H. et al. Comparative transcriptomics of multidrug-resistant Acinetobacter baumannii in response to antibiotic treatments. Sci. Rep. 8, 3515 (2018).
Low, Y. M. et al. Elucidating the survival and response of carbapenem resistant Klebsiella pneumoniae after exposure to imipenem at sub-lethal concentrations. Pathog. Glob. Health 112, 378–386 (2018).
Cho, H. & Kim, K. S. Escherichia coli OxyS RNA triggers cephalothin resistance by modulating the expression of CRP-associated genes. Biochem. Biophys. Res. Commun. 506, 66–72 (2018).
Schniederjans, M., Koska, M. & Häussler, S. Transcriptional and mutational profiling of an aminoglycoside-resistant Pseudomonas aeruginosa small-colony variant. Antimicrob. Agents Chemother. 61, e01178-17 (2017).
Felden, B. & Cattoir, V. Bacterial adaptation to antibiotics through regulatory RNAs. Antimicrob. Agents Chemother. 62, e02503-17 (2018).
Antonopoulos, D. A. et al. PATRIC as a unique resource for studying antimicrobial resistance. Brief. Bioinform. https://doi.org/10.1093/bib/bbx083 (2017).
de Man, T. J. & Limbago, B. M. SSTAR, a stand-alone easy-to-use antimicrobial resistance gene predictor. mSphere 1, e00050-15 (2016).
Lakin, S. M. et al. MEGARes: an antimicrobial resistance database for high throughput sequencing. Nucleic Acids Res. 45, D574–D580 (2017).
Naas, T. et al. Beta-lactamase database (BLDB) - structure and function. J. Enzyme Inhib. Med. Chem. 32, 917–919 (2017).
Saha, S. B., Uttam, V. & Verma, V. u-CARE: user-friendly Comprehensive Antibiotic resistance Repository of Escherichia coli. J. Clin. Pathol. 68, 648–651 (2015).
Acknowledgements
The authors thank K. Sukhum and M. Pandey for reading through a draft of this paper. This work was supported in part by awards to G.D. through the National Institute of Allergy and Infectious Diseases (NIAID), the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the National Center for Complementary and Integrative Health of the US National Institutes of Health (NIH) under award numbers R01AI123394, R01HD092414 and R01AT009741, respectively. A.W.D. received support from the Institutional Program Unifying Population and Laboratory-Based Sciences Burroughs Wellcome Fund Grant to Washington University. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Reviewer information
Nature Reviews Genetics thanks J. Parkhill, E. Ruppé and other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
M.B. and A.W.D. researched the literature and wrote the article. All authors substantially contributed to discussions of the content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Antimicrobial resistance
-
Bacterial ability to survive or grow in otherwise lethal or inhibitory antimicrobial concentrations.
- Antimicrobial susceptibility testing
-
(AST). Challenge of bacteria with antimicrobials to determine whether they have phenotypic antimicrobial resistance.
- Horizontal gene transfer
-
(HGT). Passage of resistance genes from one bacterium to another when neither bacteria is the parent or daughter cell. This process usually occurs through transduction, conjugation or transformation.
- Metagenomes
-
Collections of genes from all organisms of a given habitat or sample.
- Resistance exchange networks
-
Interconnected groups of environments or bacteria that transfer resistance genes with each other.
- Phylogeny
-
The evolutionary ancestral relationships between organisms.
- Contigs
-
Contiguous sequences assembled from sequencing reads.
- De Bruijn graph
-
(DBG). Directional graphing algorithm commonly used for short-read assembly.
- Euler’s path
-
A walk through a directed graph that crosses each edge in the graph only once. Euler’s path is used to reconstruct genome sequences from De Bruijn graphs.
- Isolate assembly
-
Gathering of sequencing reads from a bacterial isolate into longer contiguous sequences representative of their state within the bacterium.
- Resistome
-
All antimicrobial resistance genes within a given sample of bacteria.
- Annotation
-
Identification and labelling of genes within a genome.
- Burrows–Wheeler transform
-
A reversible data transformation algorithm to organize text with repeated sequences for efficient compression. This algorithm is implemented in bioinformatics software owing to frequent repeated sequences in biological data.
- Metagenomic assembly
-
Deconvolution and assembly of sequencing reads from a metagenomic sample.
- Hidden Markov model
-
(HMM). A probabilistic model of antimicrobial resistance process where hidden states emit observable outputs. These models are commonly used for sequence annotation.
- Microbiota
-
A community of microorganisms from a given habitat or sample.
- Functional metagenomics
-
A biological assay in which a metagenomic library of DNA is expressed in a naive host and then the host is exposed to a selection pressure to select for DNA that confers a fitness advantage against the selection pressure.
- Biocuration
-
The collection and organization of biological data in a data structure useful for future analysis.
- Carbapenem resistance
-
Resistance against the broad-spectrum carbapenem class of β-lactam antimicrobials, which are often used as drugs of last resort.
- Methicillin resistance
-
Resistance against methicillin, a narrow-spectrum penicillin derivative. Methicillin resistance is often seen in the context of methicillin-resistant Staphylococcus aureus (MRSA), a common human pathogen. This resistance is commonly gained by horizontal transfer of a modified target protein (see Fig. 1b and 1c).
- Deep learning
-
An extension of representational machine learning methods where the algorithm uses multiple transformation layers between raw data and output rather than one layer. This often improves results for more complex machine learning tasks.
Rights and permissions
About this article
Cite this article
Boolchandani, M., D’Souza, A.W. & Dantas, G. Sequencing-based methods and resources to study antimicrobial resistance. Nat Rev Genet 20, 356–370 (2019). https://doi.org/10.1038/s41576-019-0108-4
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41576-019-0108-4
This article is cited by
-
Metagenomics reveals the temporal dynamics of the rumen resistome and microbiome in goat kids
Microbiome (2024)
-
Development of a novel integrated isothermal amplification system for detection of bacteria-spiked blood samples
AMB Express (2023)
-
Machine learning algorithm to characterize antimicrobial resistance associated with the International Space Station surface microbiome
Microbiome (2022)
-
Primary exploring the value of metagenomic next‐generation sequencing in detecting pathogenic bacteria of cholangitis with biliary atresia after Kasai operation
Pediatric Surgery International (2022)