Abstract
Depression is one of the most common comorbidities of many chronic medical diseases including cancer and cardiovascular, metabolic, inflammatory and neurological disorders. Indeed, the prevalence of depression in these patient groups is often substantially higher than in the general population, and depression accounts for a substantial part of the psychosocial burden of these disorders. Many factors can contribute to the occurrence of comorbid depression, such as shared genetic factors, converging biological pathways, social factors, health behaviours and psychological factors. Diagnosis of depression in patients with a medical disorder can be particularly challenging owing to symptomatic overlap. Although pharmacological and psychological treatments can be effective, adjustments may need to be made for patients with a comorbid medical disorder. In addition, symptoms or treatments of medical disorders may interfere with the treatment of depression. Conversely, symptoms of depression may decrease adherence to treatment of both disorders. Thus, comprehensive treatment plans are necessary to optimize care.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Otte, C. et al. Major depressive disorder. Nat. Rev. Dis. Prim. 2, 16065 (2016). This paper provides a current overview of epidemiology, pathophysiology, diagnosis and management of MDD.
Whiteford, H. A. et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet 382, 1575–1586 (2013).
Moussavi, S. et al. Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet 370, 851–858 (2007). This paper describes the impact of comorbid depression on overall health in patients with medical disorders in a very large sample from 60 countries.
Puyat, J. H., Kazanjian, A., Wong, H. & Goldner, E. Comorbid chronic general health conditions and depression care: a population-based analysis. Psychiatr. Serv. 68, 907–915 (2017).
Gonzalez, J. S. et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care 31, 2398–2403 (2008).
Pelletier, G., Verhoef, M. J., Khatri, N. & Hagen, N. Quality of life in brain tumor patients: the relative contributions of depression, fatigue, emotional distress, and existential issues. J. Neurooncol. 57, 41–49 (2002).
Suppli, N. P. et al. Survival after early-stage breast cancer of women previously treated for depression: a nationwide Danish cohort study. J. Clin. Oncol. 35, 334–342 (2017).
Rutledge, T., Reis, V. A., Linke, S. E., Greenberg, B. H. & Mills, P. J. Depression in heart failure. J. Am. Coll. Cardiol. 48, 1527–1537 (2006).
Koyanagi, A. et al. Mortality in unipolar depression preceding and following chronic somatic diseases. Acta Psychiatr. Scand. 138, 500–508 (2018).
Cai, W., Mueller, C., Li, Y.-J., Shen, W.-D. & Stewart, R. Post stroke depression and risk of stroke recurrence and mortality: a systematic review and meta-analysis. Ageing Res. Rev. 50, 102–109 (2019).
Momen, N. C. et al. Association between mental disorders and subsequent medical conditions. N. Engl. J. Med. 382, 1721–1731 (2020).
Plana-Ripoll, O. et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet 394, 1827–1835 (2019).
Plana-Ripoll, O. et al. Changes over time in the differential mortality gap in individuals with mental disorders. JAMA Psychiatry 77, 648–650 (2020).
Machado, M. O. et al. The association of depression and all-cause and cause-specific mortality: an umbrella review of systematic reviews and meta-analyses. BMC Med. 16, 112 (2018).
Roest, A. M. & de Jonge, P. The heart of the matter: in search of causal effects of depression on somatic diseases. BMC Med. 16, 147 (2018).
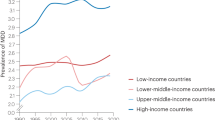
Ferrari, A. J. et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol. Med. 43, 471–481 (2013).
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259 (2017).
Pedersen, C. B. et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry 71, 573–581 (2014).
Salk, R. H., Hyde, J. S. & Abramson, L. Y. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol. Bull. 143, 783–822 (2017).
Luppa, M. et al. Age- and gender-specific prevalence of depression in latest-life – systematic review and meta-analysis. J. Affect. Disord. 136, 212–221 (2012).
Sjöberg, L. et al. Prevalence of depression: comparisons of different depression definitions in population-based samples of older adults. J. Affect. Disord. 221, 123–131 (2017).
Walker, J. et al. The prevalence of depression in general hospital inpatients: a systematic review and meta-analysis of interview-based studies. Psychol. Med. 48, 2285–2298 (2018). This paper gives an overview of the prevalence of depression among general medical and surgical inpatients, suggesting a prevalence high enough to make it worthwhile screening hospital inpatients for depression and initiating treatment where appropriate.
Wang, J. et al. Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ Open 7, e017173 (2017).
Mitchell, A. J. et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 12, 160–174 (2011).
Krebber, A. M. H. et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology 23, 121–130 (2013).
Watts, S. et al. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 4, e003901 (2014).
Watts, S., Prescott, P., Mason, J., McLeod, N. & Lewith, G. Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 5, e007618 (2015).
Huang, J. et al. Association between depression and brain tumor: a systematic review and meta-analysis. Oncotarget 8, 94932–94943 (2017).
Mehnert, A. et al. Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J. Clin. Oncol. 32, 3540–3546 (2014).
Secinti, E., Thompson, E. J., Richards, M. & Gaysina, D. Research review: childhood chronic physical illness and adult emotional health – a systematic review and meta-analysis. J. Child. Psychol. Psychiatry 58, 753–769 (2017).
Freedland, K. E. et al. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom. Med. 65, 119–128 (2003).
Brostow, D. P., Petrik, M. L., Starosta, A. J. & Waldo, S. W. Depression in patients with peripheral arterial disease: a systematic review. Eur. J. Cardiovasc. Nurs. 16, 181–193 (2017).
Feng, L. et al. Prevalence of depression in myocardial infarction. Medicine 98, e14596 (2019).
Doyle, F. et al. Systematic review and individual patient data meta-analysis of sex differences in depression and prognosis in persons with myocardial infarction. Psychosom. Med. 77, 419–428 (2015).
Khaledi, M., Haghighatdoost, F., Feizi, A. & Aminorroaya, A. The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. 56, 631–650 (2019).
Barnard, K. D., Skinner, T. C. & Peveler, R. The prevalence of co-morbid depression in adults with type 1 diabetes: systematic literature review. Diabet. Med. 23, 445–448 (2006).
Buchberger, B. et al. Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Psychoneuroendocrinology 70, 70–84 (2016).
Cooney, L. G., Lee, I., Sammel, M. D. & Dokras, A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum. Reprod. 32, 1075–1091 (2017).
Mitchell, A. J. et al. Prevalence and predictors of post-stroke mood disorders: a meta-analysis and meta-regression of depression, anxiety and adjustment disorder. Gen. Hosp. Psychiatry 47, 48–60 (2017).
Ayerbe, L., Ayis, S., Wolfe, C. D. A. & Rudd, A. G. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br. J. Psychiatry 202, 14–21 (2013).
Boeschoten, R. E. et al. Prevalence of depression and anxiety in multiple sclerosis: a systematic review and meta-analysis. J. Neurol. Sci. 372, 331–341 (2017).
Marrie, R. A. et al. Differences in the burden of psychiatric comorbidity in MS vs the general population. Neurology 85, 1972–1979 (2015).
McKay, K. A. et al. Psychiatric comorbidity is associated with disability progression in multiple sclerosis. Neurology 90, e1316–e1323 (2018).
Binzer, S., McKay, K. A., Brenner, P., Hillert, J. & Manouchehrinia, A. Disability worsening among persons with multiple sclerosis and depression: a Swedish cohort study. Neurology 93, e2216–e2223 (2019).
Kim, M., Kim, Y.-S., Kim, D.-H., Yang, T.-W. & Kwon, O.-Y. Major depressive disorder in epilepsy clinics: a meta-analysis. Epilepsy Behav. 84, 56–69 (2018).
Goodarzi, Z. et al. Detecting depression in Parkinson disease. Neurology 87, 426–437 (2016).
Chi, S. et al. The prevalence of depression in Alzheimer’s disease: a systematic review and meta-analysis. Curr. Alzheimer Res. 12, 189–198 (2015).
Zhang, L., Fu, T., Yin, R., Zhang, Q. & Shen, B. Prevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. BMC Psychiatry 17, 70 (2017).
Dowlatshahi, E. A., Wakkee, M., Arends, L. R. & Nijsten, T. The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J. Investig. Dermatol. 134, 1542–1551 (2014).
Matcham, F., Rayner, L., Steer, S. & Hotopf, M. The prevalence of depression in rheumatoid arthritis: a systematic review and meta-analysis. Rheumatology 52, 2136–2148 (2013).
Neuendorf, R., Harding, A., Stello, N., Hanes, D. & Wahbeh, H. Depression and anxiety in patients with inflammatory bowel disease: a systematic review. J. Psychosom. Res. 87, 70–80 (2016).
Mulugeta, A., Zhou, A., King, C. & Hyppönen, E. Association between major depressive disorder and multiple disease outcomes: a phenome-wide Mendelian randomisation study in the UK Biobank. Mol. Psychiatry 25, 1469–1476 (2019).
Tylee, D. S. et al. Genetic correlations among psychiatric and immune-related phenotypes based on genome-wide association data. Am. J. Med. Genet. B Neuropsychiatr. Genet. 177, 641–657 (2018).
Tyrrell, J. et al. Using genetics to understand the causal influence of higher BMI on depression. Int. J. Epidemiol. 48, 834–848 (2019).
Milaneschi, Y. et al. Genetic association of major depression with atypical features and obesity-related immunometabolic dysregulations. JAMA Psychiatry 74, 1214–1225 (2017). This study clearly demonstrates a genetic link between depression and obesity and illustrates the possibility of using genetics to explore potential biological pathways connecting depression and medical disorders.
Haljas, K. et al. Bivariate genome-wide association study of depressive symptoms with type 2 diabetes and quantitative glycemic traits. Psychosom. Med. 80, 242–251 (2018).
Samaan, Z. et al. Lack of association between type 2 diabetes and major depression: epidemiologic and genetic evidence in a multiethnic population. Transl Psychiatry 5, e618 (2015).
Clarke, T.-K. et al. Investigating shared aetiology between type 2 diabetes and major depressive disorder in a population based cohort. Am. J. Med. Genet. B Neuropsychiatr. Genet. 174, 227–234 (2016).
Khandaker, G. M. et al. Shared mechanisms between coronary heart disease and depression: findings from a large UK general population-based cohort. Mol. Psychiatry 25, 1477–1486 (2020).
Brainstorm Consortium. et al. Analysis of shared heritability in common disorders of the brain. Science 360, eaap8757 (2018).
Wang, J. S. et al. Examining the effect of 5-HTTLPR on depressive symptoms in postmenopausal women 1 year after initial breast cancer treatment. Support. Care Cancer 27, 513–519 (2019).
Ogrodnik, M. et al. Obesity-induced cellular senescence drives anxiety and impairs neurogenesis. Cell Metab. 29, 1061–1077 (2019).
Kennis, M. et al. Prospective biomarkers of major depressive disorder: a systematic review and meta-analysis. Mol. Psychiatry 25, 321–338 (2019).
Otte, C., Neylan, T. C., Pipkin, S. S., Browner, W. S. & Whooley, M. A. Depressive symptoms and 24-hour urinary norepinephrine excretion levels in patients with coronary disease: findings from the Heart and Soul study. Am. J. Psychiatry 162, 2139–2145 (2005).
Otte, C. et al. Depression and 24-hour urinary cortisol in medical outpatients with coronary heart disease: the Heart and Soul study. Biol. Psychiatry 56, 241–247 (2004).
Enache, D., Pariante, C. M. & Mondelli, V. Markers of central inflammation in major depressive disorder: a systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain Behav. Immun. 81, 24–40 (2019).
Köhler, C. A. et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr. Scand. 135, 373–387 (2017).
Osimo, E. F., Baxter, L. J., Lewis, G., Jones, P. B. & Khandaker, G. M. Prevalence of low-grade inflammation in depression: a systematic review and meta-analysis of CRP levels. Psychol. Med. 49, 1958–1970 (2019).
Orlovska-Waast, S. et al. Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Mol. Psychiatry 24, 869–887 (2018).
Hodes, G. E., Kana, V., Menard, C., Merad, M. & Russo, S. J. Neuroimmune mechanisms of depression. Nat. Neurosci. 18, 1386–1393 (2015).
Nerurkar, L., Siebert, S., McInnes, I. B. & Cavanagh, J. Rheumatoid arthritis and depression: an inflammatory perspective. Lancet Psychiatry 6, 164–173 (2019).
Kappelmann, N., Lewis, G., Dantzer, R., Jones, P. B. & Khandaker, G. M. Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol. Psychiatry 23, 335–343 (2016).
Wittenberg, G. M. et al. Effects of immunomodulatory drugs on depressive symptoms: a mega-analysis of randomized, placebo-controlled clinical trials in inflammatory disorders. Mol. Psychiatry 25, 1275–1285 (2019).
Duivis, H. E. et al. Depressive symptoms, health behaviors, and subsequent inflammation in patients with coronary heart disease: prospective findings from the Heart and Soul study. Am. J. Psychiatry 168, 913–920 (2011).
Laake, J.-P. S. et al. The association between depressive symptoms and systemic inflammation in people with type 2 diabetes: findings from the South London Diabetes Study. Diabetes Care 37, 2186–2192 (2014).
Hayashino, Y., Mashitani, T., Tsujii, S. & Ishii, H. Elevated levels of hs-CRP are associated with high prevalence of depression in Japanese patients with type 2 diabetes: the Diabetes Distress and Care Registry at Tenri (DDCRT 6). Diabetes Care 37, 2459–2465 (2014).
Moulton, C. D., Pickup, J. C. & Ismail, K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 3, 461–471 (2015).
Carson, A. J. et al. Depression after stroke and lesion location: a systematic review. Lancet 356, 122–126 (2000).
Wei, N. et al. Post-stroke depression and lesion location: a systematic review. J. Neurol. 262, 81–90 (2014).
Padmanabhan, J. L. et al. A human depression circuit derived from focal brain lesions. Biol. Psychiatry 86, 749–758 (2019).
Allida, S. et al. Pharmacological, psychological, and non-invasive brain stimulation interventions for treating depression after stroke. Cochrane Database Syst. Rev. 1, CD0033437 (2020).
Gold, S. M. et al. Detection of altered hippocampal morphology in multiple sclerosis-associated depression using automated surface mesh modeling. Hum. Brain Mapp. 35, 30–37 (2012).
Rossi, S. et al. Neuroinflammation drives anxiety and depression in relapsing-remitting multiple sclerosis. Neurology 89, 1338–1347 (2017).
Corallo, F. et al. A complex relation between depression and multiple sclerosis: a descriptive review. Neurol. Sci. 40, 1551–1558 (2019).
Qato, D. M., Ozenberger, K. & Olfson, M. Prevalence of prescription medications with depression as a potential adverse effect among adults in the United States. JAMA 319, 2289–2298 (2018).
Verbeek, D. E. P., van Riezen, J., de Boer, R. A., van Melle, J. P. & de Jonge, P. A review on the putative association between beta-blockers and depression. Heart Fail. Clin. 7, 89–99 (2011).
Salagre, E., Fernandes, B. S., Dodd, S., Brownstein, D. J. & Berk, M. Statins for the treatment of depression: a meta-analysis of randomized, double-blind, placebo-controlled trials. J. Affect. Disord. 200, 235–242 (2016).
Kovacs, D., Kovacs, P., Eszlari, N., Gonda, X. & Juhasz, G. Psychological side effects of immune therapies: symptoms and pathomechanism. Curr. Opin. Pharmacol. 29, 97–103 (2016).
Udina, M. et al. Interferon-induced depression in chronic hepatitis C. J. Clin. Psychiatry 73, 1128–1138 (2012).
Schaefer, M. et al. Escitalopram for the prevention of peginterferon-α2a-associated depression in hepatitis C virus-infected patients without previous psychiatric disease: a randomized trial. Ann. Intern. Med. 157, 94–103 (2012).
Mann, T. K., Dail, R. B. & Bailey, D. E. Cognitive and affective symptoms experienced by cancer patients receiving high-dose intravenous interleukin 2 therapy: an integrative literature review. Cancer Nurs. 39, 349–357 (2016).
DellaGioia, N. & Hannestad, J. A critical review of human endotoxin administration as an experimental paradigm of depression. Neurosci. Biobehav. Rev. 34, 130–143 (2010).
Weinberger, A. H. et al. Depression and cigarette smoking behavior: a critical review of population-based studies. Am. J. Drug. Alcohol. Abuse 43, 416–431 (2016).
Forouzanfar, M. H. et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1659–1724 (2016).
Chauhan, G. et al. Genetic and lifestyle risk factors for MRI-defined brain infarcts in a population-based setting. Neurology 92, e486–e503 (2019).
Belbasis, L., Bellou, V., Evangelou, E., Ioannidis, J. P. A. & Tzoulaki, I. Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta-analyses. Lancet Neurol. 14, 263–273 (2015).
Chaiton, M. O., Cohen, J. E., OtextquotesingleLoughlin, J. & Rehm, J. A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public. Health 9, 356 (2009).
Ho, S. Y., Alnashri, N., Rohde, D., Murphy, P. & Doyle, F. Systematic review and meta-analysis of the impact of depression on subsequent smoking cessation in patients with chronic respiratory conditions. Gen. Hosp. Psychiatry 37, 399–407 (2015).
Patten, S. B., Williams, J. V. & Bulloch, A. G. Major depressive episodes and mortality in the Canadian household population. J. Affect. Disord. 242, 165–171 (2019).
Choi, K. W. et al. Assessment of bidirectional relationships between physical activity and depression among adults. JAMA Psychiatry 76, 399–408 (2019).
Whooley, M. A. et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA 300, 2379–2388 (2008). This study demonstrates that the association between depressive symptoms and adverse cardiovascular events in patients with coronary heart disease is largely explained by behavioural factors, particularly physical inactivity.
Boden, J. M. & Fergusson, D. M. Alcohol and depression. Addiction 106, 906–914 (2011).
Lassale, C. et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol. Psychiatry 24, 965–986 (2018).
Molendijk, M., Molero, P., Ortuño Sánchez-Pedreño, F., Van der Does, W. & Angel Martínez-González, M. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 226, 346–354 (2018).
Martínez-González, M. A., Gea, A. & Ruiz-Canela, M. The Mediterranean diet and cardiovascular health. Circulation Res. 124, 779–798 (2019).
Bot, M. et al. Effect of multinutrient supplementation and food-related behavioral activation therapy on prevention of major depressive disorder among overweight or obese adults with subsyndromal depressive symptoms. JAMA 321, 858–868 (2019).
Mausbach, B. T., Schwab, R. B. & Irwin, S. A. Depression as a predictor of adherence to adjuvant endocrine therapy (AET) in women with breast cancer: a systematic review and meta-analysis. Breast Cancer Res. Treat. 152, 239–246 (2015).
Kessing, D., Denollet, J., Widdershoven, J. & Kupper, N. Psychological determinants of heart failure self-care. Psychosom. Med. 78, 412–431 (2016).
Brown, S. A. et al. Biobehavioral determinants of glycemic control in type 2 diabetes: a systematic review and meta-analysis. Patient Educ. Couns. 99, 1558–1567 (2016).
Rieckmann, N. et al. Course of depressive symptoms and medication adherence after acute coronary syndromes. J. Am. Coll. Cardiol. 48, 2218–2222 (2006).
Folkman, S. in Encyclopedia of Behavioral Medicine (eds Gellman, M. D. & Turner, J. R.) 1913–1915 (Springer, 2013).
Heijmans, M. et al. The stress of being chronically ill: from disease-specific to task-specific aspects. J. Behav. Med. 27, 255–271 (2004).
Moss-Morris, R. Adjusting to chronic illness: time for a unified theory. Br. J. Health Psychol. 18, 681–686 (2013).
Clarke, D. M. & Currie, K. C. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med. J. Aust. 190, S54–S60 (2009).
Detweiler-Bedell, J. B., Friedman, M. A., Leventhal, H., Miller, I. W. & Leventhal, E. A. Integrating co-morbid depression and chronic physical disease management: identifying and resolving failures in self-regulation. Clin. Psychol. Rev. 28, 1426–1446 (2008).
Sirois, F. M., Kitner, R. & Hirsch, J. K. Self-compassion, affect, and health-promoting behaviors. Health Psychol. 34, 661–669 (2015).
Schiavon, C. C., Marchetti, E., Gurgel, L. G., Busnello, F. M. & Reppold, C. T. Optimism and hope in chronic disease: a systematic review. Front. Psychol. 7, 2022 (2016).
Leventhal, H., Diefenbach, M. & Leventhal, E. A. Illness cognition: using common sense to understand treatment adherence and affect cognition interactions. Cognit. Ther. Res. 16, 143–163 (1992).
Trudel-Fitzgerald, C. et al. The relationship of perfectionism with psychological symptoms in cancer patients and the contributing role of hyperarousability and coping. Psychol. Health 32, 381–401 (2017).
Leventhal, H., Brissette, I. & Leventhal, E. A. in The Self-regulation of Health and Illness Behaviour (eds Cameron, L. D. & Leventhal, H.) 42–65 (Psychology Press, 2003).
Hagger, M. S., Koch, S., Chatzisarantis, N. L. D. & Orbell, S. The common sense model of self-regulation: meta-analysis and test of a process model. Psychol. Bull. 143, 1117–1154 (2017).
Uhlenbusch, N. et al. Depression and anxiety in patients with different rare chronic diseases: a cross-sectional study. PLoS ONE 14, e0211343 (2019).
Edwards, R. R., Cahalan, C., Mensing, G., Smith, M. & Haythornthwaite, J. A. Pain, catastrophizing, and depression in the rheumatic diseases. Nat. Rev. Rheumatol. 7, 216–224 (2011).
Edwards, R. R., Bingham, C. O., Bathon, J. & Haythornthwaite, J. A. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Rheum. 55, 325–332 (2006).
Hudson, J. L. & Moss-Morris, R. Treating illness distress in chronic illness. Eur. Psychol. 24, 26–37 (2019).
Neff, K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity 2, 85–101 (2003).
Pinto-Gouveia, J., Duarte, C., Matos, M. & Fráguas, S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clin. Psychol. Psychother. 21, 311–323 (2013).
Przezdziecki, A. et al. My changed body: breast cancer, body image, distress and self-compassion. Psychooncology 22, 1872–1879 (2012).
Sirois, F. M. & Rowse, G. The role of self-compassion in chronic illness care. J. Clin. Outcome Manag. 23, 521–527 (2016).
Stange, J. P., Alloy, L. B. & Fresco, D. M. Inflexibility as a vulnerability to depression: a systematic qualitative review. Clin. Psychol. Sci. Pract. 24, 245–276 (2017).
Gentili, C. et al. Psychological flexibility as a resilience factor in individuals with chronic pain. Front. Psychol. 10, 2016 (2019).
Dimidjian, S., Barrera, M., Martell, C., Muñoz, R. F. & Lewinsohn, P. M. The origins and current status of behavioral activation treatments for depression. Annu. Rev. Clin. Psychol. 7, 1–38 (2011).
Shear, M. K. et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry 73, 685–694 (2016).
Whooley, M. A., Avins, A. L., Miranda, J. & Browner, W. S. Case-finding instruments for depression. J. Gen. Intern. Med. 12, 439–445 (1997).
Bosanquet, K. et al. Diagnostic accuracy of the Whooley questions for the identification of depression: a diagnostic meta-analysis. BMJ Open 5, e008913 (2015). This paper provides a quantitative overview of the diagnostic accuracy of screening for depression.
Colquhoun, D. M. et al. Screening, referral and treatment for depression in patients with coronary heart disease. Med. J. Aust. 198, 483–484 (2013).
World Health Organization. mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings – version 2 (WHO, 2016).
Shepard, N. & Parker, C. Depression in adults: recognition and management. Clin. Pharm. https://doi.org/10.1211/cp.2017.20202439 (2017).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The patient health questionnaire-2. Med. Care 41, 1284–1292 (2003).
Manea, L. et al. Identifying depression with the PHQ-2: a diagnostic meta-analysis. J. Affect. Disord. 203, 382–395 (2016).
Whooley, M. A. Screening for depression — a tale of two questions. JAMA Intern. Med. 176, 436–438 (2016).
Levis, B. et al. Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: systematic review and meta-analysis. JAMA 323, 2290–2300 (2020).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9. J. Gen. Intern. Med. 16, 606–613 (2001).
Gilbody, S., Richards, D., Brealey, S. & Hewitt, C. Screening for depression in medical settings with the patient health questionnaire (PHQ): a diagnostic meta-analysis. J. Gen. Intern. Med. 22, 1596–1602 (2007).
Mitchell, A. J., Yadegarfar, M., Gill, J. & Stubbs, B. Case finding and screening clinical utility of the patient health questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open 2, 127–138 (2016).
Archer, J. et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst. Rev. 10, CD006525 (2012).
Panagioti, M. et al. Association between chronic physical conditions and the effectiveness of collaborative care for depression: an individual participant data meta-analysis. JAMA Psychiatry 73, 978–989 (2016).
Cipriani, A. et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet 391, 1357–1366 (2018).
Rayner, L. et al. Antidepressants for depression in physically ill people. Cochrane Database Syst. Rev. 391, CD007503 (2010). This paper provides a comprehensive, quantitative summary of the efficacy of antidepressants in patients with comorbid medical disorders.
Ostuzzi, G. et al. Efficacy and acceptability of antidepressants in patients with ischemic heart disease. Int. Clin. Psychopharmacol. 34, 65–75 (2019).
Ostuzzi, G., Benda, L., Costa, E. & Barbui, C. Efficacy and acceptability of antidepressants on the continuum of depressive experiences in patients with cancer: systematic review and meta-analysis. Cancer Treat. Rev. 41, 714–724 (2015).
Baumeister, H., Hutter, N. & Bengel, J. Psychological and pharmacological interventions for depression in patients with diabetes mellitus: an abridged Cochrane review. Diabet. Med. 31, 773–786 (2014).
Price, A. et al. Antidepressants for the treatment of depression in neurological disorders: a systematic review and meta-analysis of randomised controlled trials. J. Neurol. Neurosurg. Psychiatry 82, 914–923 (2011).
Xu, X. et al. Efficacy and feasibility of antidepressant treatment in patients with post-stroke depression. Medicine 95, e5349 (2016).
Bomasang-Layno, E., Fadlon, I., Murray, A. N. & Himelhoch, S. Antidepressive treatments for Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat. Disord. 21, 833–842 (2015).
Fiest, K. M. et al. Systematic review and meta-analysis of interventions for depression and anxiety in persons with multiple sclerosis. Mult. Scler. Relat. Disord. 5, 12–26 (2016).
Ostuzzi, G., Matcham, F., Dauchy, S., Barbui, C. & Hotopf, M. Antidepressants for the treatment of depression in people with cancer. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.cd011006.pub3 (2018).
Fiest, K. M. et al. Systematic review and meta-analysis of interventions for depression and anxiety in persons with rheumatoid Arthritis. J. Clin. Rheumatol. 23, 425–434 (2017).
Fiest, K. M. et al. Systematic review of interventions for depression and anxiety in persons with inflammatory bowel disease. BMC Res. Notes 9, 404 (2016).
Madhusoodanan, S., Velama, U., Parmar, J., Goia, D. & Brenner, R. A current review of cytochrome P450 interactions of psychotropic drugs. Ann. Clin. Psychiatry 26, 120–138 (2014).
Rosenblat, J. D., Lee, Y. & McIntyre, R. S. The effect of pharmacogenomic testing on response and remission rates in the acute treatment of major depressive disorder: a meta-analysis. J. Affect. Disord. 241, 484–491 (2018).
Kim, B. Y., Sharafoddini, A., Tran, N., Wen, E. Y. & Lee, J. Consumer mobile apps for potential drug-drug interaction check: systematic review and content analysis using the mobile app rating scale (MARS). JMIR Mhealth Uhealth 6, e74 (2018).
Apidi, N. A. et al. Mobile medical applications for dosage recommendation, drug adverse reaction, and drug interaction. Ther. Innov. Regul. Sci. 51, 480–485 (2017).
Eshun-Wilson, I. et al. Antidepressants for depression in adults with HIV infection. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.cd008525.pub3 (2018).
Zimmermann-Viehoff, F., Kuehl, L. K., Danker-Hopfe, H., Whooley, M. A. & Otte, C. Antidepressants, autonomic function and mortality in patients with coronary heart disease: data from the heart and soul study. Psychol. Med. 44, 2975–2984 (2014).
Taylor, D. Antidepressant drugs and cardiovascular pathology: a clinical overview of effectiveness and safety. Acta Psychiatr. Scand. 118, 434–442 (2008).
Pizzi, C. et al. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am. J. Cardiol. 107, 972–979 (2011).
Beach, S. R. et al. Meta-analysis of selective serotonin reuptake inhibitor–associated QTc prolongation. J. Clin. Psychiatry 75, e441–e449 (2014).
Assimon, M. M., Brookhart, M. A. & Flythe, J. E. Comparative cardiac safety of selective serotonin reuptake inhibitors among individuals receiving maintenance hemodialysis. J. Am. Soc. Nephrol. 30, 611–623 (2019).
Bahar, M. A., Kamp, J., Borgsteede, S. D., Hak, E. & Wilffert, B. The impact of CYP2D6 mediated drug-drug interaction: a systematic review on a combination of metoprolol and paroxetine/fluoxetine. Br. J. Clin. Pharmacol. 84, 2704–2715 (2018).
Köhler-Forsberg, O. et al. Efficacy of anti-inflammatory treatment on major depressive disorder or depressive symptoms: meta-analysis of clinical trials. Acta Psychiatri. Scand. 139, 404–419 (2019).
Bu, D., Griffin, G. & Lichtman, A. H. Mechanisms for the anti-inflammatory effects of statins. Curr. Opin. Lipidol. 22, 165–170 (2011).
Abajo, F. J. de & García-Rodríguez, L. A. Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy. Arch. Gen. Psychiatry 65, 795–803 (2008).
Spina, E., Barbieri, M. A., Cicala, G., Bruno, A. & de Leon, J. Clinically relevant drug interactions between newer antidepressants and oral anticoagulants. Expert. Opin. Drug. Metab. Toxicol. 16, 31–44 (2020).
Yoon, J. M., Cho, E.-G., Lee, H.-K. & Park, S. M. Antidepressant use and diabetes mellitus risk: a meta-analysis. Korean J. Fam. Med. 34, 228–240 (2013).
Domecq, J. P. et al. Drugs commonly associated with weight change: a systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 100, 363–370 (2015).
Roopan, S. & Larsen, E. R. Use of antidepressants in patients with depression and comorbid diabetes mellitus: a systematic review. Acta Neuropsychiatr. 29, 127–139 (2016).
Williams, L. J. et al. Selective serotonin reuptake inhibitors (SSRIs) and markers of bone turnover in men. Calcif. Tissue Int. 103, 125–130 (2018).
Brännström, J., Lövheim, H., Gustafson, Y. & Nordström, P. Association between antidepressant drug use and hip fracture in older people before and after treatment initiation. JAMA Psychiatry 76, 172–179 (2019).
Maguire, M. J., Weston, J., Singh, J. & Marson, A. G. Antidepressants for people with epilepsy and depression. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD010682.pub2 (2014).
Monaco, F. & Cicolin, A. Interactions between anticonvulsant and psychoactive drugs. Epilepsia 40, s71–s76 (1999).
Ogawa, Y. et al. Antidepressants plus benzodiazepines for adults with major depression. Cochrane Database Syst. Rev. 6, CD001026 (2019).
Gasim, M. et al. Adverse psychiatric effects of disease-modifying therapies in multiple sclerosis: a systematic review. Mult. Scler. Relat. Disord. 26, 124–156 (2018).
Deutsche Gesellschaft für Neurologie. Idiopathisches Parkinson-Syndrom in Leitlinien für Diagnostik und Therapie in der Neurologie (DGN, 2016).
Lederberg, M. S. & Holland, J. C. in Handbook of Psychotherapy in Cancer Care Ch. 1 (Watson, M. & Kissane, D. W.) 1–14 (John Wiley & Sons, Ltd, 2011).
Faller, H. et al. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J. Clin. Oncol. 31, 782–793 (2013).
Okuyama, T., Akechi, T., Mackenzie, L. & Furukawa, T. A. Psychotherapy for depression among advanced, incurable cancer patients: a systematic review and meta-analysis. Cancer Treat. Rev. 56, 16–27 (2017).
Bortolato, B. et al. Depression in cancer: The many biobehavioral pathways driving tumor progression. Cancer Treat. Rev. 52, 58–70 (2017).
Lutgendorf, S. K. & Andersen, B. L. Biobehavioral approaches to cancer progression and survival: mechanisms and interventions. Am. Psychologist 70, 186–197 (2015).
Hartung, T. J. et al. The hospital anxiety and depression scale (HADS) and the 9-item patient health questionnaire (PHQ-9) as screening instruments for depression in patients with cancer: depression screening in oncology. Cancer 123, 4236–4243 (2017).
Wang, S.-B. et al. Cognitive behavioral therapy for post-stroke depression: a meta-analysis. J. Affect. Disord. 235, 589–596 (2018).
Hackett, M. L., Anderson, C. S., House, A. & Xia, J. Interventions for treating depression after stroke. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.cd003437.pub3 (2008).
Ghielen, I. et al. The effects of cognitive behavioral and mindfulness-based therapies on psychological distress in patients with multiple sclerosis, Parkinson’s disease and Huntington’s disease: two meta-analyses. J. Psychosom. Res. 122, 43–51 (2019).
Hind, D. et al. Cognitive behavioural therapy for the treatment of depression in people with multiple sclerosis: a systematic review and meta-analysis. BMC Psychiatry 14, 5 (2014).
Reavell, J., Hopkinson, M., Clarkesmith, D. & Lane, D. A. Effectiveness of cognitive behavioral therapy for depression and anxiety in patients with cardiovascular disease. Psychosom. Med. 80, 742–753 (2018).
Li, C. et al. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for patients with diabetes and depression. J. Psychosom. Res. 95, 44–54 (2017).
Chew, B. H., Vos, R. C., Metzendorf, M.-I., Scholten, R. J. & Rutten, G. E. Psychological interventions for diabetes-related distress in adults with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 9, CD011469 (2017).
Graham, C. D., Gouick, J., Krahé, C. & Gillanders, D. A systematic review of the use of acceptance and commitment therapy (ACT) in chronic disease and long-term conditions. Clin. Psychol. Rev. 46, 46–58 (2016).
Gold, S. M. et al. Control conditions for randomised trials of behavioural interventions in psychiatry: a decision framework. Lancet Psychiatry 4, 725–732 (2017).
UK ECT Review Group. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet 361, 799–808 (2003).
Meyer, J. P., Swetter, S. K. & Kellner, C. H. Electroconvulsive therapy in geriatric psychiatry: a selective review. Psychiatr. Clin. North. Am. 41, 79–93 (2018).
van Diermen, L. et al. Prediction of electroconvulsive therapy response and remission in major depression: meta-analysis. Br. J. Psychiatry 212, 71–80 (2018).
Semkovska, M. & McLoughlin, D. M. Objective cognitive performance associated with electroconvulsive therapy for depression: a systematic review and meta-analysis. Biol. Psychiatry 68, 568–577 (2010).
Mutz, J. et al. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ 364, l1079 (2019).
Academy of Medical Sciences. Multimorbidity: a priority for global health research (Academy of Medical Sciences, 2018).
Beran, D., Perel, P. & Miranda, J. J. Forty years since Alma-Ata: do we need a new model for noncommunicable diseases? J. Glob. Health 9, 010316 (2019).
Brandt, L. R. et al. Addressing depression comorbid with diabetes or hypertension in resource-poor settings: a qualitative study about user perception of a nurse-supported smartphone app in Peru. JMIR Ment. Health 6, e11701 (2019).
Menezes, P. et al. Use of a mobile phone app to treat depression comorbid with hypertension or diabetes: a pilot study in Brazil and Peru. JMIR Ment. Health 6, e11698 (2019).
Gellis, Z. D., Kenaley, B. L. & Have, T. T. Integrated telehealth care for chronic illness and depression in geriatric home care patients: the Integrated Telehealth Education and Activation of Mood (I-TEAM) study. J. Am. Geriatr. Soc. 62, 889–895 (2014).
Butow, P. et al. Comparison of implementation strategies to influence adherence to the clinical pathway for screening, assessment and management of anxiety and depression in adult cancer patients (ADAPT CP): study protocol of a cluster randomised controlled trial. BMC Cancer 18, 1077 (2018).
Woltmann, E. et al. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am. J. Psychiatry 169, 790–804 (2012).
Stein, D. J. et al. Integrating mental health with other non-communicable diseases. BMJ 364, l295 (2019).
Firth, J. et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry 6, 675–712 (2019).
Labrique, A., Vasudevan, L., Mehl, G., Rosskam, E. & Hyder, A. A. Digital health and health systems of the future. Glob. Health Sci. Pract. 6, S1–S4 (2018).
Peiris, D., Miranda, J. J. & Mohr, D. C. Going beyond killer apps: building a better mHealth evidence base. BMJ Glob. Health 3, e000676 (2018).
Chandrashekar, P. Do mental health mobile apps work: evidence and recommendations for designing high-efficacy mental health mobile apps. mHealth 4, 6 (2018).
Hoermann, S., McCabe, K. L., Milne, D. N. & Calvo, R. A. Application of synchronous text-based dialogue systems in mental health interventions: systematic review. J. Med. Internet Res. 19, e267 (2017).
Kroenke, K. et al. Effect of telecare management on pain and depression in patients with cancer. JAMA 304, 163–171 (2010).
Diez-Canseco, F. et al. Integration of a technology-based mental health screening program into routine practices of primary health care services in Peru (the Allillanchu Project): development and implementation. J. Med. Internet Res. 20, e100 (2018).
Cavero, V. et al. Provision of mental health care within primary care in Peru: a qualitative study exploring the perspectives of psychologists, primary health care providers, and patients. Wellcome Open. Res. 3, 9 (2018).
Nobis, S. et al. Efficacy of a web-based intervention with mobile phone support in treating depressive symptoms in adults with type 1 and type 2 diabetes: a randomized controlled trial. Diabetes Care 38, 776–783 (2015).
Nobis, S. et al. Web-based intervention for depressive symptoms in adults with types 1 and 2 diabetes mellitus: a health economic evaluation. Br. J. Psychiatry 212, 199–206 (2018).
Yoo, S. J. C., Nyman, J. A., Cheville, A. L. & Kroenke, K. Cost effectiveness of telecare management for pain and depression in patients with cancer: results from a randomized trial. Gen. Hosp. Psychiatry 36, 599–606 (2014).
Chibanda, D. et al. Effect of a primary care-based psychological intervention on symptoms of common mental disorders in Zimbabwe. JAMA 316, 2618–2626 (2016). This study demonstrates the feasibility and effectiveness of task-shifting treatment strategies to non-health professionals, augmenting possibilities for reach and adoption of treatment efforts in low-resource settings.
Mehta, S., Peynenburg, V. A. & Hadjistavropoulos, H. D. Internet-delivered cognitive behaviour therapy for chronic health conditions: a systematic review and meta-analysis. J. Behav. Med. 42, 169–187 (2018).
Fischer, A. et al. An online programme to reduce depression in patients with multiple sclerosis: a randomised controlled trial. Lancet Psychiatry 2, 217–223 (2015).
Schröder, J. et al. Efficacy of a psychological online intervention for depression in people with epilepsy: a randomized controlled trial. Epilepsia 55, 2069–2076 (2014).
Herring, M. P., Puetz, T. W., O’Connor, P. J. & Dishman, R. K. Effect of exercise training on depressive symptoms among patients with a chronic illness. Arch. Intern. Med. 172, 101–111 (2012).
Blumenthal, J. A. et al. Exercise and pharmacological treatment of depressive symptoms in patients with coronary heart disease. J. Am. Coll. Cardiol. 60, 1053–1063 (2012).
Blumenthal, J. A. et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure. JAMA 308, 465–474 (2012).
Dalgas, U., Stenager, E., Sloth, M. & Stenager, E. The effect of exercise on depressive symptoms in multiple sclerosis based on a meta-analysis and critical review of the literature. Eur. J. Neurol. 22, e34 (2015).
Kelley, G. A., Kelley, K. S. & Hootman, J. M. Effects of exercise on depression in adults with arthritis: a systematic review with meta-analysis of randomized controlled trials. Arthritis Res. Ther. 17, 21 (2015).
Fang, F. et al. Suicide and cardiovascular death after a cancer diagnosis. N. Engl. J. Med. 366, 1310–1318 (2012).
Zaorsky, N. G. et al. Suicide among cancer patients. Nat. Commun. 10, 207 (2019).
Bolton, J. M., Walld, R., Chateau, D., Finlayson, G. & Sareen, J. Risk of suicide and suicide attempts associated with physical disorders: a population-based, balancing score-matched analysis. Psychol. Med. 45, 495–504 (2014).
Wang, B., An, X., Shi, X. & Zhang, J.-A. Management of endocrine disease: suicide risk in patients with diabetes: a systematic review and meta-analysis. Eur. J. Endocrinol. 177, R169–R181 (2017).
Pompili, M. et al. Suicide risk in type 1 diabetes mellitus: a systematic review. J. Psychosom. Res. 76, 352–360 (2014).
Erlangsen, A. et al. Association between neurological disorders and death by suicide in Denmark. JAMA 323, 444–454 (2020).
Ahmedani, B. K. et al. Health care contacts in the year before suicide death. J. Gen. Intern. Med. 29, 870–877 (2014).
Katon, W. J. et al. Collaborative care for patients with depression and chronic illnesses. N. Engl. J. Med. 363, 2611–2620 (2010).
Li, M. et al. Systematic review and meta-analysis of collaborative care interventions for depression in patients with cancer. Psychooncology 26, 573–587 (2016).
Atlantis, E., Fahey, P. & Foster, J. Collaborative care for comorbid depression and diabetes: a systematic review and meta-analysis. BMJ Open 4, e004706 (2014).
Tully, P. J. & Baumeister, H. Collaborative care for comorbid depression and coronary heart disease: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 5, e009128 (2015).
Bullinger, M. & Quitmann, J. Quality of life as patient-reported outcomes: principles of assessment. Dialogues Clin. Neurosci. 16, 137–145 (2014).
Bullinger, M. in Advances in Experimental Medicine and Biology 113–122 (Kluwer Academic Publishers, 2003).
John, E. Ware, Jr. & Gandek, B. The SF-36 health survey: development and use in mental health research and the IQOLA project. Int. J. Ment. Health 23, 49–73 (1994).
Skevington, S. M., Lotfy, M. & O’Connell, K. A. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 13, 299–310 (2004).
Devlin, N. J. & Brooks, R. EQ-5D and the EuroQol group: past, present and future. Appl. Health Econ. Health Policy 15, 127–137 (2017).
Cocks, K., King, M. T., Velikova, G., Fayers, P. M. & Brown, J. M. Quality, interpretation and presentation of European Organisation for Research and Treatment of Cancer quality of life questionnaire core 30 data in randomised controlled trials. Eur. J. Cancer 44, 1793–1798 (2008).
Liao, S.-C., Ma, H.-M., Lin, Y.-L. & Huang, W.-L. Functioning and quality of life in patients with somatic symptom disorder: the association with comorbid depression. Compr. Psychiatry 90, 88–94 (2019).
Gao, K., Su, M., Sweet, J. & Calabrese, J. R. Correlation between depression/anxiety symptom severity and quality of life in patients with major depressive disorder or bipolar disorder. J. Affect. Disord. 244, 9–15 (2019).
DeJean, D., Giacomini, M., Vanstone, M. & Brundisini, F. Patient experiences of depression and anxiety with chronic disease: a systematic review and qualitative meta-synthesis. Ont. Health Technol. Assess. Ser. 13, 1–33 (2013).
Sluijs, J. F. et al. Illness burden and physical outcomes associated with collaborative care in patients with comorbid depressive disorder in chronic medical conditions: a systematic review and meta-analysis. Gen. Hosp. Psychiatry 50, 1–14 (2018).
Schwartz, C. E. et al. The clinical significance of adaptation to changing health: a meta-analysis of response shift. Qual. Life Res. 15, 1533–1550 (2006).
Kristofferzon, M.-L., Engström, M. & Nilsson, A. Coping mediates the relationship between sense of coherence and mental quality of life in patients with chronic illness: a cross-sectional study. Qual. Life Res. 27, 1855–1863 (2018).
Park, S. J., Rim, S. J., Kim, C. E. & Park, S. Effect of comorbid depression on health-related quality of life of patients with chronic diseases: a South Korean nationwide study (2007–2015). J. Psychosom. Res. 116, 17–21 (2019).
Kang, H.-J. et al. Comorbidity of depression with physical disorders: research and clinical implications. Chonnam Med. J. 51, 8–18 (2015).
Egede, L. E. & Hernández-Tejada, M. A. Effect of comorbid depression on quality of life in adults with type 2 diabetes. Expert. Rev. Pharmacoeconomics Outcomes Res. 13, 83–91 (2013).
Amoozegar, F. Depression comorbidity in migraine. Int. Rev. Psychiatry 29, 504–515 (2017).
Shin, D. W. et al. Health-related quality of life, perceived social support, and depression in disease-free survivors who underwent curative surgery only for prostate, kidney and bladder cancer: comparison among survivors and with the general population. Cancer Res. Treat. 51, 289–299 (2019).
Rodrigues, K. C. et al. Assessment of depression, anxiety, quality of life, and coping in long-standing multiple endocrine neoplasia type 2 patients. Thyroid 27, 693–706 (2017).
Lemmens, L. C., Molema, C. C. M., Versnel, N., Baan, C. A. & de Bruin, S. R. Integrated care programs for patients with psychological comorbidity: a systematic review and meta-analysis. J. Psychosom. Res. 79, 580–594 (2015).
Vyas, A., Babcock, Z. & Kogut, S. Impact of depression treatment on health-related quality of life among adults with cancer and depression: a population-level analysis. J. Cancer Surviv. 11, 624–633 (2017).
Alenzi, E. O. & Sambamoorthi, U. Depression treatment and health-related quality of life among adults with diabetes and depression. Qual. Life Res. 25, 1517–1525 (2015).
Shah, D., Rai, P., Dwibedi, N. & Sambamoorthi, U. Treatment for depression and health-related quality of life among adults with arthritis. Psychiatr. Q. 89, 129–140 (2017).
Baumeister, H., Hutter, N. & Bengel, J. Psychological and pharmacological interventions for depression in patients with coronary artery disease. Cochrane Database Syst. Rev. 9, CD008012 (2011).
Kearns, B. et al. The cost-effectiveness of changes to the care pathway used to identify depression and provide treatment amongst people with diabetes in England: a model-based economic evaluation. BMC Health Serv. Res. 17, 78 (2017).
Committee for Medicinal Products for Human Use (CHMP). Reflection paper on the regulatory guidance for the use of health-related quality of life (HRQL) measures in the evaluation of medicinal products. EMA https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-regulatory-guidance-use-healthrelated-quality-life-hrql-measures-evaluation_en.pdf (2005).
FDA. Patient-reported outcome measures: use in medical product development to support labeling claims. FDA https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-reported-outcome-measures-use-medical-product-development-support-labeling-claims (2009).
Minden, S. L. et al. Evidence-based guideline: assessment and management of psychiatric disorders in individuals with MS: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 82, 174–181 (2013).
Siu, A. L. et al. Screening for depression in adults: US preventive services task force recommendation statement. JAMA 315, 380–387 (2016).
Canadian Task Force on Preventive Health Care. et al. Recommendations on screening for depression in adults. Can. Med. Assoc. J. 185, 775–782 (2013).
Thombs, B. D. & Ziegelstein, R. C. Does depression screening improve depression outcomes in primary care? BMJ 348, g1253–g1253 (2014).
Ferrari, F. & Villa, R. F. The neurobiology of depression: an integrated overview from biological theories to clinical evidence. Mol. Neurobiol. 54, 4847–4865 (2016).
Pilevarzadeh, M. et al. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res. Treat. 176, 519–533 (2019).
Walker, J. et al. Prevalence, associations, and adequacy of treatment of major depression in patients with cancer: a cross-sectional analysis of routinely collected clinical data. Lancet Psychiatry 1, 343–350 (2014).
Li, Z., Li, Y., Chen, L., Chen, P. & Hu, Y. Prevalence of depression in patients with hypertension: a systematic review and meta-analysis. Medicine 94, e1317 (2015).
Ormel, J., Oldehinkel, A. J., Nolen, W. A. & Vollebergh, W. Psychosocial disability before, during, and after a major depressive episode: a 3-wave population-based study of state, scar, and trait effects. Arch. Gen. Psychiatry 61, 387–392 (2004).
Marmot, M. et al. WHO European review of social determinants of health and the health divide. Lancet 380, 1011–1029 (2012).
Hughes, K. et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2, e356–e366 (2017).
Cuijpers, P., Stringaris, A. & Wolpert, M. Treatment outcomes for depression: challenges and opportunities. Lancet Psychiatry 17, 30036–30045 (2020).
Suglia, S. F. et al. Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. Circulation 137, e15–e28 (2018).
Heim, C. M., Entringer, S. & Buss, C. Translating basic research knowledge on the biological embedding of early-life stress into novel approaches for the developmental programming of lifelong health. Psychoneuroendocrinology 105, 123–137 (2019).
Stringhini, S. et al. Socioeconomic status and the 25×25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet 389, 1229–1237 (2017).
Lorant, V. et al. Socioeconomic inequalities in depression: a meta-analysis. Am. J. Epidemiol. 157, 98–112 (2003).
Saraceno, B., Levav, I. & Kohn, R. The public mental health significance of research on socio-economic factors in schizophrenia and major depression. World Psychiatry 4, 181–185 (2005).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Scottish Government Polypharmacy Model of Care Group. Polypharmacy Guidance, Realistic Prescribing 3rd edn (Scottish Government, 2018).
van den Beuken-van Everdingen, M. H. J., Hochstenbach, L. M. J., Joosten, E. A. J., Tjan-Heijnen, V. C. G. & Janssen, D. J. A. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J. Pain. Symptom Manage 51, 1070–1090.e9 (2016).
Drewes, A. M. et al. Gastrointestinal pain. Nat. Rev. Dis. Prim. 6, 1 (2020).
Bair, M. J. et al. Prevalence of pain and association with quality of life, depression and glycaemic control in patients with diabetes. Diabet. Med. 27, 578–584 (2010).
Antonini, A. et al. Pain in Parkinson’s disease: facts and uncertainties. Eur. J. Neurol. 25, 917-e69 (2018).
Means-Christensen, A. J., Roy-Byrne, P. P., Sherbourne, C. D., Craske, M. G. & Stein, M. B. Relationships among pain, anxiety, and depression in primary care. Depress. Anxiety 25, 593–600 (2008).
Gerrits, M. M. J. G., van Oppen, P., van Marwijk, H. W. J., Penninx, B. W. J. H. & van der Horst, H. E. Pain and the onset of depressive and anxiety disorders. Pain 155, 53–59 (2014).
Stubbs, B. et al. Depression and pain: primary data and meta-analysis among 237 952 people across 47 low- and middle-income countries. Psychol. Med. 47, 2906–2917 (2017).
DeVeaugh-Geiss, A. M. et al. The adverse effects of comorbid pain on depression outcomes in primary care patients: results from the ARTIST trial. Pain Med. 11, 732–741 (2010).
Gerrits, M. M. J. G. et al. Pain, not chronic disease, is associated with the recurrence of depressive and anxiety disorders. BMC Psychiatry 14, 187 (2014).
World Health Organization. Guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents (WHO, 2018).
Chou, R. et al. Systemic pharmacologic therapies for low back pain: a systematic review for an American College of Physicians Clinical Practice Guideline. Ann. Intern. Med. 166, 480–492 (2017).
Acknowledgements
S.M.G. receives funding from the Deutsche Forschungsgemeinschaft (GO1357/5-2; 8-2), the European Commission (IMI2 859366), the German Federal Ministry of Health (BMG-BVA 2520FSB431) and the National MS Society (MB-1707-28359; RG-1507-05418). J.J.M. has received support from the Alliance for Health Policy and Systems Research (HQHSR1206660), the Bernard Lown Scholars in Cardiovascular Health Program at Harvard T.H. Chan School of Public Health (BLSCHP-1902), Bloomberg Philanthropies, FONDECYT via CIENCIACTIVA/CONCYTEC, British Council, British Embassy and the Newton-Paulet Fund (223-2018, 224-2018), DFID/MRC/Wellcome Global Health Trials (MR/M007405/1), Fogarty International Center (R21TW009982, D71TW010877), Grand Challenges Canada (0335-04), Inter-American Institute for Global Change Research (IAI CRN3036), International Development Research Center Canada (IDRC 106887, 108167), Medical Research Council (MR/P008984/1, MR/P024408/1, MR/P02386X/1), National Cancer Institute (1P20CA217231), National Heart, Lung and Blood Institute (HHSN268200900033C, 5U01HL114180, 1UM1HL134590), National Institute of Mental Health (1U19MH098780), Swiss National Science Foundation (40P740-160366), Wellcome Trust (074833/Z/04/Z, 093541/Z/10/Z, 103994/Z/14/Z, 107435/Z/15/Z, 205177/Z/16/Z, 214185/Z/18/Z, 218743/Z/19/Z) and the World Diabetes Foundation (WDF15-1224). C.O. has received funding from the Deutsche Forschungsgemeinschaft (OT 209/7-3; 14-1), the European Commission (IMI2 859366) and the German Federal Ministry of Education and Research (KS2017-067). The authors thank V. Stiglbauer (Charité – Universitätsmedizin Berlin) for help with formatting of the manuscript draft.
Author information
Authors and Affiliations
Contributions
Introduction (S.M.G. and C.O.); Epidemiology (O.K.-F. and M.A.W.); Mechanisms/pathophysiology (S.M.G., O.K.-F., R.M.-M. and A.S.); Diagnosis, screening and prevention (M.A.W. and C.O.); Management (S.M.G., O.K.-F., A.M., J.J.M. and C.O.); Quality of life (M.B.); Outlook (S.M.G.); Overview of Primer (S.M.G. and C.O.).
Corresponding author
Ethics declarations
Competing interests
S.M.G. reports personal fees from Almirall SA, Celgene, Forum für Medizinische Fortbildung (FomF) and Mylan GmbH, and in-kind research contributions from GAIA Group. R.M.-M. reports personal fees from Mahana Therapeutics and is a beneficiary of a license agreement between Mahana Therapeutics and King’s College London. C.O. reports personal fees from Allergan, Ferring, Fortbildungskolleg, Limes Kliniken, Medical Tribune, MedOnline, Neuraxpharm, Sage Therapeutics and Stillachhaus. All other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks C. Caltagirone, C. Pae, S. Patten, P. De Jonge, Y. Uchitomi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Drug interactions checker: https://www.drugs.com/drug_interactions.html
Rights and permissions
About this article
Cite this article
Gold, S.M., Köhler-Forsberg, O., Moss-Morris, R. et al. Comorbid depression in medical diseases. Nat Rev Dis Primers 6, 69 (2020). https://doi.org/10.1038/s41572-020-0200-2
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-020-0200-2
This article is cited by
-
Dynamic and accessible pharmacogenomic results: a response to pharmacogenomic testing for antidepressant treatment selection
Neuropsychopharmacology (2024)
-
Das Deutsche Zentrum für Psychische Gesundheit
Der Nervenarzt (2024)
-
Prospective trajectories of depression predict mortality in cancer patients
Journal of Behavioral Medicine (2024)
-
Antidepressants and type 2 diabetes: highways to knowns and unknowns
Diabetology & Metabolic Syndrome (2023)
-
Major depressive disorder
Nature Reviews Disease Primers (2023)