Abstract
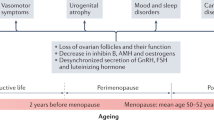
The menopausal transition period spans, on average, 2–8 years before the final menstrual period and is associated with an increase in clinical and subclinical cardiovascular risk. In this Review, we discuss the metabolic and cardiovascular changes that occur during the menopausal transition period and the role of ovarian ageing, chronological ageing and other ageing-related risk factors in mediating these changes. Disentangling the relative contributions of chronological and reproductive ageing to cardiovascular risk is challenging, but data from longitudinal studies in women transitioning from premenopause to post-menopause have provided valuable insights. We also discuss evidence on how cardiovascular risk is altered by premature or early menopause, surgical menopause, and vasomotor and other menopausal symptoms. Whether targeted interventions can slow the progression of atherosclerosis and subclinical disease during the menopausal transition, thus delaying or preventing the onset of cardiovascular events, remains to be determined. Furthermore, we consider the recommended strategies for cardiovascular risk reduction in women undergoing menopausal transition using the framework of the American Heart Association’s Life’s Essential 8 key measures for improving and maintaining cardiovascular health, and discuss the cardiovascular risks and benefits of menopausal hormone therapy. Finally, we also discuss novel therapies that might benefit this population in reducing cardiovascular risk.
Key points
-
The menopausal transition period heralds a dynamic change in a woman’s reproductive lifespan and is associated with substantial hormonal, metabolic and cardiovascular changes.
-
Some of the cardiometabolic changes that occur throughout the menopausal transition period are independent of chronological ageing and are instead largely driven by reproductive ageing.
-
Individuals who undergo premature menopause, early menopause or surgically induced menopause have an increased risk of adverse cardiometabolic changes.
-
Strategies to reduce the cardiometabolic risk during the menopausal transition period include lifestyle modifications and pharmacological therapy.
-
Depending on the timing of initiation, menopausal hormone therapy might portend neutral-to-beneficial cardiometabolic effects during the menopausal transition period.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
El Khoudary, S. R. et al. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation 142, e506–e532 (2020).
Kochanek, K. D., Murphy, S. L., Xu, J. & Tejada-Vera, B. Deaths: final data for 2014. Natl. Vital. Stat. Rep. 65, 1–122 (2016).
Manson J. E. & Bassuk, S. S. in Harrison’s Principles of Internal Medicine 21st edn (eds Loscalzo, J. et al.) (McGraw Hill, 2022).
Thurston, R. C. & Joffe, H. Vasomotor symptoms and menopause: findings from the Study of Women’s Health Across the Nation. Obstet. Gynecol. Clin. North. Am. 38, 489–501 (2011).
Gold, E. B. et al. Longitudinal analysis of the association between VMS and race/ethnicity across the menopausal transition: Study of Women’s Health Across the Nation. Am. J. Public. Health 96, 1226–1235 (2006).
Politi, M. C., Schleinitz, M. D. & Col, N. F. Revisiting the duration of VMS of menopause: a meta-analysis. J. Gen. Intern. Med. 23, 1507–1513 (2008).
Mishra, G. D. & Dobson, A. J. Using longitudinal profiles to characterize women’s symptoms through midlife: results from a large prospective study. Menopause 19, 549–555 (2012).
El Khoudary, S. R. Gaps, limitations and new insights on endogenous estrogen and follicle stimulating hormone as related to risk of cardiovascular disease in women traversing the menopause: a narrative review. Maturitas 104, 44–53 (2017).
Santoro, N. & Randolph, J. F. Reproductive hormones and the menopause transition. Obstet. Gynecol. Clin. North. Am. 38, 455–466 (2011).
Harlow, S. D. et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. Fertil. Steril. 97, 843–851 (2012).
Crandall, C. J., Mehta, J. M. & Manson, J. E. Management of menopausal symptoms: a review. JAMA 329, 405–420 (2023).
Avis, N. E., Crawford, S. L. & Green, R. Vasomotor symptoms across the menopause transition: differences among women. Obstet. Gynecol. Clin. North. Am. 45, 629–640 (2018).
El Khoudary, S. R. et al. The menopause transition and women’s health at midlife: a progress report from the Study of Women’s Health Across the Nation (SWAN). Menopause 26, 1213–1227 (2019).
Bromberger, J. T. & Epperson, C. N. Depression during and after the perimenopause: impact of hormones, genetics, and environmental determinants of disease. Obstet. Gynecol. Clin. North. Am. 45, 663–678 (2018).
Kravitz, H. M. et al. Trajectory analysis of sleep maintenance problems in midlife women before and after surgical menopause: the Study of Women’s Health Across the Nation (SWAN). Menopause 27, 278–288 (2020).
Guthrie, J. R., Dennerstein, L., Taffe, J. R., Lehert, P. & Burger, H. G. The menopausal transition: a 9-year prospective population-based study. The Melbourne Women’s Midlife Health Project. Climacteric 7, 375–389 (2004).
Dennerstein, L., Dudley, E. C., Hopper, J. L., Guthrie, J. R. & Burger, H. G. A prospective population-based study of menopausal symptoms. Obstet. Gynecol. 96, 351–358 (2000).
Davis, S. R. et al. Understanding weight gain at menopause. Climacteric 15, 419–429 (2012).
Freeman, E. W. & Sammel, M. D. Methods in a longitudinal cohort study of late reproductive age women: the Penn Ovarian Aging Study (POAS). Women’s Midlife Health 2, 1 (2016).
Thomas, A. J., Mitchell, E. S. & Woods, N. F. The challenges of midlife women: themes from the Seattle Midlife Women’s Health Study. Women’s Midlife Health 4, 8 (2018).
Samargandy, S. et al. Abdominal visceral adipose tissue over the menopause transition and carotid atherosclerosis: the SWAN heart study. Menopause 28, 626–633 (2021).
Greendale, G. A. et al. Changes in regional fat distribution and anthropometric measures across the menopause transition. J. Clin. Endocrinol. Metab. 106, 2520–2534 (2021).
Greendale, G. A. et al. Changes in body composition and weight during the menopause transition. JCI Insight 4, e124865 (2019).
Mao, L., Wang, L., Bennett, S., Xu, J. & Zou, J. Effects of follicle-stimulating hormone on fat metabolism and cognitive impairment in women during menopause. Front. Physiol. 13, 1043237 (2022).
Iacobellis, G., Gao, Y. J. & Sharma, A. M. Do cardiac and perivascular adipose tissue play a role in atherosclerosis? Curr. Diab. Rep. 8, 20–24 (2008).
Rosito, G. A. et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample the Framingham Heart Study. Circulation 117, 605–613 (2008).
Stanhewicz, A. E., Wenner, M. M. & Stachenfeld, N. S. Sex differences in endothelial function important to vascular health and overall cardiovascular disease risk across the lifespan. Am. J. Physiol. Heart Circ. Physiol. 315, H1569–H1588 (2018).
El Khoudary, S. R. et al. Progression rates of carotid intima-media thickness and adventitial diameter during the menopausal transition. Menopause 20, 8–14 (2013).
Samargandy, S. et al. Arterial stiffness accelerates within 1 year of the final menstrual period: the SWAN heart study. Arterioscler. Thromb. Vasc. Biol. 40, 1001–1008 (2020).
Anagnostis, P., Lambrinoudaki, I., Stevenson, J. C. & Goulis, D. G. Menopause-associated risk of cardiovascular disease. Endocr. Connect. 11, e210537 (2022).
Thurston, R. C. et al. Menopause versus chronologic aging: their roles in women’s health. Menopause 25, 849–854 (2018).
Matthews, K. A. et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J. Am. Coll. Cardiol. 54, 2366–2373 (2009).
El Khoudary, S. R. HDL and the menopause. Curr. Opin. Lipidol. 28, 328–336 (2017).
El Khoudary, S. R. et al. Increase HDL-C level over the menopausal transition is associated with greater atherosclerotic progression. J. Clin. Lipidol. 10, 962–969 (2016).
Rosenson, R. S. et al. HDL measures, particle heterogeneity, proposed nomenclature, and relation to atherosclerotic cardiovascular events. Clin. Chem. 57, 392–410 (2011).
Gurka, M. J., Vishnu, A., Santen, R. J. & Deboer, M. D. Progression of metabolic syndrome severity during the menopausal transition. J. Am. Heart Assoc. 5, e003609 (2016).
Lejsková, M., Aluší, Š., Valenta, Z., Adámková, S. & Piťha, J. Natural postmenopause is associated with an increase in combined cardiovascular risk factors. Physiol. Res. 61, 587–596 (2012).
Janssen, I., Powell, L. H., Crawford, S., Lasley, B. & Sutton-Tyrrell, K. Menopause and the metabolic syndrome: the Study of Women’s Health Across the Nation. Arch. Intern. Med. 168, 1568–1575 (2008).
Li, Q. et al. High circulating follicle-stimulating hormone level is a potential risk factor for renal dysfunction in post-menopausal women. Front. Endocrinol. 12, 627903 (2021).
Zhang, X. et al. High follicle-stimulating hormone level associated with risk of rheumatoid arthritis and disease activity. Front. Endocrinol. 13, 862849 (2022).
Thurston, R. C. et al. Menopausal vasomotor symptoms and risk of incident cardiovascular disease events in SWAN. J. Am. Heart Assoc. 10, e017416 (2021).
Zhu, D. et al. Vasomotor menopausal symptoms and risk of cardiovascular disease: a pooled analysis of six prospective studies. Am. J. Obstet. Gynecol. 223, e1–e16 (2020).
Thurston, R. C. et al. Trajectories of vasomotor symptoms and carotid intima media thickness in the Study of Women’s Health Across the Nation. Stroke 47, 12–17 (2016).
Thurston, R. C., Sutton-Tyrrell, K., Everson-Rose, S. A., Hess, R. & Matthews, K. A. Hot flashes and subclinical cardiovascular disease: findings from the Study of Women’s Health Across the Nation Heart Study. Circulation 118, 1234–1240 (2008).
Bechlioulis, A. et al. Endothelial function, but not carotid intima-media thickness, is affected early in menopause and is associated with severity of hot flushes. J. Clin. Endocrinol. Metab. 95, 2009–2262 (2010).
Thurston, R. C. et al. Menopausal symptoms and cardiovascular disease mortality in the Women’s Ischemia Syndrome Evaluation (WISE). Menopause 24, 126–132 (2017).
Thurston, R. C. et al. Physiologically assessed hot flashes and endothelial function among midlife women. Menopause 24, 886–893 (2017).
Herber-Gast, G. C. M. & Mishra, G. D. Early severe vasomotor menopausal symptoms are associated with diabetes. Menopause 21, 855–860 (2014).
Stuenkel, C. A. Menopause, hormone therapy and diabetes. Climacteric 20, 11–21 (2017).
Honigberg, M. C. et al. Association of premature natural and surgical menopause with incident cardiovascular disease. JAMA 322, 2411–2421 (2019).
Nudy, M. et al. The severity of vasomotor symptoms and number of menopausal symptoms in postmenopausal women and select clinical health outcomes in the Women’s Health Initiative Calcium and Vitamin D Randomized Clinical Trial. Menopause 27, 1265–1273 (2020).
Thurston, R. C. et al. Sleep characteristics and carotid atherosclerosis among midlife women. Sleep 40, zsw052 (2017).
Hall, M. H. et al. Sleep is associated with the metabolic syndrome in a multi-ethnic cohort of midlife women: the SWAN Sleep Study. Sleep 35, 783–790 (2012).
Matthews, K. A. et al. Do reports of sleep disturbance relate to coronary and aortic calcification in healthy middle-aged women?: study of Women’s Health Across the Nation. Sleep. Med. 14, 282–287 (2013).
Zhou, Y., Yang, R., Li, C. & Tao, M. Sleep disorder, an independent risk associated with arterial stiffness in menopause. Sci. Rep. 7, 1904 (2017).
Makarem, N., St-Onge, M. P., Liao, M., Lloyd-Jones, D. M. & Aggarwal, B. Association of sleep characteristics with cardiovascular health among women and differences by race/ethnicity and menopausal status: findings from the American Heart Association Go Red for Women Strategically Focused Research Network. Sleep. Health 5, 501–508 (2019).
Janssen, I. et al. Depressive symptoms are related to progression of coronary calcium in midlife women: the Study of Women’s Health Across the Nation (SWAN) heart study. Am. Heart J. 161, 1186–1191 (2011).
Janssen, I. et al. Relation of persistent depressive symptoms to coronary artery calcification in women aged 46 to 59 years. Am. J. Cardiol. 117, 1884–1889 (2016).
Wassertheil-Smoller, S. et al. Depression and cardiovascular sequelae in postmenopausal women. Arch. Intern. Med. 164, 289–298 (2004).
Muka, T. et al. Association of vasomotor and other menopausal symptoms with risk of cardiovascular disease: a systematic review and meta-analysis. PLoS ONE 11, e0157417 (2016).
Muka, T. et al. Association of age at onset of menopause and time since onset of menopause with cardiovascular outcomes, intermediate vascular traits, and all-cause mortality: a systematic review and meta-analysis. JAMA Cardiol. 1, 767–776 (2016).
Zhu, D. et al. Age at natural menopause and risk of incident cardiovascular disease: a pooled analysis of individual patient data. Lancet Public. Health 4, e553–e564 (2019).
Yoshida, Y. et al. Early menopause and cardiovascular disease risk in women with or without type 2 diabetes: a pooled analysis of 9,374 postmenopausal women. Diabetes Care 44, 2564–2572 (2021).
Shin, J. et al. Age at menopause and risk of heart failure and atrial fibrillation: a nationwide cohort study. Eur. Heart J. 43, 4148–4157 (2022).
Freaney, P. M. et al. Premature menopause and 10-year risk prediction of atherosclerotic cardiovascular disease. JAMA Cardiol. 6, 1463–1465 (2021).
Lloyd-Jones, D. M. et al. The coronary artery risk development in young adults (CARDIA) study: JACC focus seminar 8/8. J. Am. Coll. Cardiol. 78, 260–277 (2021).
Ardissino, M. et al. Sex-specific reproductive factors augment cardiovascular disease risk in women: a Mendelian randomization study. J. Am. Heart Assoc. 12, e027933 (2023).
Kok, H. S. et al. Heart disease risk determines menopausal age rather than the reverse. J. Am. Coll. Cardiol. 47, 1976–1983 (2006).
Zhu, D. et al. Premenopausal cardiovascular disease and age at natural menopause: a pooled analysis of over 170,000 women. Eur. J. Epidemiol. 34, 235–246 (2019).
Rivera, C. M. et al. Increased cardiovascular mortality after early bilateral oopherectomy. Menopause 16, 15–23 (2009).
Atsma, F., Bartelink, M. L. E. L., Grobbee, D. E. & Van Der Schouw, Y. T. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause 13, 265–279 (2006).
Parker, W. H. et al. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the Nurses’ Health Study. Obstet. Gynecol. 113, 1027–1037 (2009).
Ingelsson, E., Lundholm, C., Johansson, A. L. V. & Altman, D. Hysterectomy and risk of cardiovascular disease: a population-based cohort study. Eur. Heart J. 32, 745–750 (2011).
Sarrel, P. M., Sullivan, S. D. & Nelson, L. M. Hormone replacement therapy in young women with surgical primary ovarian insufficiency. Fertil. Steril. 106, 1580–1587 (2016).
Santoro, N., Worsley, R., Miller, K. K., Parish, S. J. & Davis, S. R. Role of estrogens and estrogen-like compounds in female sexual function and dysfunction. J. Sex. Med. 13, 305–316 (2016).
Faubion, S. S., Kuhle, C. L., Shuster, L. T. & Rocca, W. A. Long-term health consequences of premature or early menopause and considerations for management. Climacteric 18, 483–491 (2015).
Lloyd-Jones, D. M. et al. Life’s Essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation 146, e18–e43 (2022).
American Diabetes Association Professional Practice Committee. 3. Prevention or delay of type 2 diabetes and associated comorbidities: standards of medical care in diabetes – 2022. Diabetes Care 45, S39–S45 (2022).
Stampfer, M. J., Hu, F. B., Manson, J. E., Rimm, E. B. & Willett, M. C. Primary prevention of coronary heart disease in women through diet and lifestyle. N. Engl. J. Med. 343, 16–22 (2000).
Colpani, V. et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis. Eur. J. Epidemiol. 33, 831–845 (2018).
Shams-White, M. M., Brockton, N. T., Mitrou, P., Kahle, L. L. & Reedy, J. The 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) score and all-cause, cancer, and cardiovascular disease mortality risk: a longitudinal analysis in the NIH-AARP diet and health study. Curr. Dev. Nutr. 6, nzac096 (2022).
Hu, F. B. et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N. Engl. J. Med. 345, 790–797 (2001).
Wang, D. et al. Western dietary pattern derived by multiple statistical methods is prospectively associated with subclinical carotid atherosclerosis in midlife women. J. Nutr. 150, 579–591 (2020).
Wildman, R. P., Schott, L. L., Brockwell, S., Kuller, L. H. & Sutton-Tyrrell, K. A dietary and exercise intervention slows menopause-associated progression of subclinical atherosclerosis as measured by intima-media thickness of the carotid arteries. J. Am. Coll. Cardiol. 44, 579–585 (2004).
Karagkouni, I. et al. Dietary patterns are associated with arterial stiffness and carotid atherosclerosis in postmenopausal women. Endocrine 78, 57–67 (2022).
Chelmow, D. et al. Preventing obesity in midlife women: a recommendation from the Women’s Preventive Service Initiative. Ann. Intern. Med. 175, 1305–1309 (2022).
Mehta, J., Kling, J. M. & Manson, J. A. E. Risks, benefits, and treatment modalities of menopausal hormone therapy: current concepts. Front. Endocrinol. 12, 564781 (2021).
Stampfer, M. J. & Colditz, G. A. Estrogen replacement therapy and coronary heart disease: a quantitative assessment of the epidemiologic evidence. Prev. Med. 20, 47–63 (1991).
Schierbeck, L. L. et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ 345, e6409 (2012).
Gregersen, I. et al. Effect of hormone replacement therapy on atherogenic lipid profile in postmenopausal women. Thromb. Res. 184, 1–7 (2019).
Stampfer, M. J. et al. A prospective study of postmenopausal estrogen therapy and coronary heart disease. N. Engl. J. Med. 313, 1044–1049 (1985).
D’Alonzo, M., Bounous, V. E., Villa, M. & Biglia, N. Current evidence of the oncological benefit-risk profile of hormone replacement therapy. Medicina 55, 573 (2019).
Manson, J. A. E. et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Qomen’s Health Initiative randomized trials. JAMA 310, 1353–1368 (2013).
North American Menopause Society Estrogen and progestogen use in peri- and postmenopausal women: September 2003 position statement of the North American Menopause Society. Menopause 10, 497–506 (2003).
Miller, V. M. et al. Using basic science to design a clinical trial: baseline characteristics of women enrolled in the Kronos Early Estrogen Prevention Study (KEEPS). J. Cardiovasc. Transl. Res. 2, 228–239 (2009).
Mehta, J. M., Chester, R. C. & Kling, J. M. The timing hypothesis: hormone therapy for treating symptomatic women during menopause and its relationship to cardiovascular disease. J. Women’s Health 28, 705–711 (2019).
Ouyang, P., Michos, E. D. & Karas, R. H. Hormone replacement therapy and the cardiovascular system. lessons learned and unanswered questions. J. Am. Coll. Cardiol. 47, 1741–1753 (2006).
Moreau, K. L., Hildreth, K. L., Meditz, A. L., Deane, K. D. & Kohrt, W. M. Endothelial function is impaired across the stages of the menopause transition in healthy women. J. Clin. Endocrinol. Metab. 97, 4692–4700 (2012).
Wild, R. A. et al. Cardiovascular disease (CVD) risk scores, age, or years since menopause to predict cardiovascular disease in the Women’s Health Initiative. Menopause 28, 610–618 (2021).
Boardman, H. M. P. et al. Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochrane Database Syst. Rev. 2015, CD002229 (2015).
Pinkerton, J. A. V. et al. The 2017 hormone therapy position statement of the North American Menopause Society. Menopause 24, 728–753 (2017).
McNeil, M. Menopausal hormone therapy: understanding long-term risks and benefits. JAMA 318, 911–913 (2017).
Miller, V. M. et al. The Kronos Early Estrogen Prevention Study (KEEPS): what have we learned? Menopause 26, 1071–1084 (2019).
Hodis, H. N. & Mack, W. J. The timing hypothesis and hormone replacement therapy: a paradigm shift in the primary prevention of coronary heart disease in women. Part 2: comparative risks. J. Am. Geriatr. Soc. 61, 1011–1018 (2013).
Hodis, H. N. et al. Vascular effects of early versus late postmenopausal treatment with estradiol. N. Engl. J. Med. 374, 1221–1231 (2016).
Grossman, D. C. et al. Hormone therapy for the primary prevention of chronic conditions in postmenopausal women US Preventive Services Task Force recommendation statement. JAMA 318, 2224–2233 (2017).
Folsom, A. R. et al. Hormonal replacement therapy and morbidity and mortality in a prospective study of postmenopausal women. Am. J. Public. Health 85, 1128–1132 (1995).
Salpeter, S. R. et al. Meta-analysis: effect of hormone-replacement therapy on components of the metabolic syndrome in postmenopausal women. Diabetes Obes. Metab. 8, 538–554 (2006).
Xu, Y., Lin, J., Wang, S., Xiong, J. & Zhu, Q. Combined estrogen replacement therapy on metabolic control in postmenopausal women with diabetes mellitus. Kaohsiung J. Med. Sci. 30, 350–361 (2014).
Rossouw, J. E. et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. J. Am. Med. Assoc. 288, 321–333 (2002).
Anderson, G. L. & Limacher, M. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. J. Am. Med. Assoc. 291, 1701–1712 (2004).
Shufelt, C. L. et al. Hormone therapy dose, formulation, route of delivery, and risk of cardiovascular events in women: findings from the Women’s Health Initiative Observational Study. Menopause 21, 260–266 (2014).
Bassuk, S. S. & Manson, J. A. E. Oral contraceptives and menopausal hormone therapy: relative and attributable risks of cardiovascular disease, cancer, and other health outcomes. Ann. Epidemiol. 25, 193–200 (2015).
Madika, A. L. et al. Menopausal hormone therapy and risk of incident hypertension: role of the route of estrogen administration and progestogens in the E3N cohort. Menopause 28, 1204–1208 (2021).
O’Kelly, A. C. et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ. Res. 130, 652–672 (2022).
Mehta, P. K., Gaignard, S., Schwartz, A. & Manson, J. A. E. Traditional and emerging sex-specific risk factors for cardiovascular disease in women. Rev. Cardiovasc. Med. 23, 288 (2022).
Shifren, J. L. et al. The North American Menopause Society recommendations for clinical care of midlife women. Menopause 21, 1038–1062 (2014).
Baart, S. J. et al. Cardiovascular risk prediction models for women in the general population: a systematic review. PLoS ONE 14, e0210329 (2019).
Liu, P. et al. Blocking FSH induces thermogenic adipose tissue and reduces body fat. Nature 546, 107–112 (2017).
Kohrt, W. M. & Wierman, M. E. Preventing fat gain by blocking follicle-stimulating hormone. N. Engl. J. Med. 377, 293–295 (2017).
Kumar, P. & Sharma, A. Gonadotropin-releasing hormone analogs: understanding advantages and limitations. J. Hum. Reprod. Sci. 7, 170–174 (2014).
Bethel, M. A. et al. Cardiovascular outcomes with glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: a meta-analysis. Lancet Diabetes Endocrinol. 6, 105–113 (2018).
Rizzo, M. et al. GLP-1 receptor agonists and reduction of cardiometabolic risk: potential underlying mechanisms. Biochim. Biophys. Acta Mol. Basis Dis. 1864, 2814–2821 (2018).
Santoro, N. et al. Effect of the neurokinin 3 receptor antagonist fezolinetant on patient-reported outcomes in postmenopausal women with vasomotor symptoms: results of a randomized, placebo-controlled, double-blind, dose-ranging study (VESTA). Menopause 27, 1350–1356 (2020).
Manson, J. E. et al. Estrogen therapy and coronary-artery calcification. N. Engl. J. Med. 356, 2591–2602 (2007).
Author information
Authors and Affiliations
Contributions
The authors contributed substantially to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Eleni Armeni, Yvonne van der Schouw and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mehta, J.M., Manson, J.E. The menopausal transition period and cardiovascular risk. Nat Rev Cardiol 21, 203–211 (2024). https://doi.org/10.1038/s41569-023-00926-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-023-00926-7