Abstract
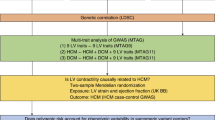
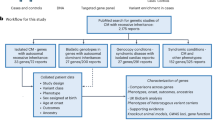
Hypertrophic cardiomyopathy (HCM) was traditionally described as an autosomal dominant Mendelian disease but is now increasingly recognized as having a complex genetic aetiology. Although eight core genes encoding sarcomeric proteins account for >90% of the pathogenic variants in patients with HCM, variants in several additional genes (ACTN2, ALPK3, CSRP3, FHOD3, FLNC, JPH2, KLHL24, PLN and TRIM63), encoding non-sarcomeric proteins with diverse functions, have been shown to be disease-causing in a small number of patients. Genome-wide association studies (GWAS) have identified numerous loci in cardiomyopathy case–control studies and biobank investigations of left ventricular functional traits. Genes associated with Mendelian cardiomyopathy are enriched in the putative causal gene lists at these loci. Intriguingly, many loci are associated with both HCM and dilated cardiomyopathy but with opposite directions of effect on left ventricular traits, highlighting a genetic basis underlying the contrasting pathophysiological effects observed in each condition. This overlap extends to rare Mendelian variants with distinct variant classes in several genes associated with HCM and dilated cardiomyopathy. In this Review, we appraise the complex contribution of the non-sarcomeric, HCM-associated genes to cardiomyopathies across a range of variant classes (from common non-coding variants of individually low effect size to complete gene knockouts), which provides insights into the genetic basis of cardiomyopathies, causal genes at GWAS loci and the application of clinical genetic testing.
Key points
-
Cardiomyopathies are often inherited diseases, but highly variable penetrance and the lack of Mendelian genetic variants in substantial numbers of patients increasingly suggests a complex genetic aetiology.
-
Genome-wide association studies have identified large overlaps in significant loci for cardiomyopathies and left ventricular traits, with opposite effects (risk or protective alleles) observed for hypertrophic and dilated cardiomyopathy.
-
Variants in genes encoding non-sarcomeric proteins account for a small proportion of patients with Mendelian hypertrophic cardiomyopathy but are the presumed causal genes at several genome-wide association study loci, expanding their role in cardiomyopathy genetics.
-
These genes have complex genotype–phenotype correlations across different variant classes (common regulatory and rare missense, truncating and biallelic loss-of-function variants), with distinct associations often observed for hypertrophic and dilated cardiomyopathy.
-
Understanding these complex, rare variant associations is essential for variant interpretation in patients with cardiomyopathies, with hypertrophic cardiomyopathy-associated minor gene variants probably more prevalent in understudied populations.
-
The shared genes and pathways identified by these rare and common variant studies provide new insights into cardiomyopathy pathophysiology and propose novel approaches for therapeutic intervention.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Seidman, C. E. & Seidman, J. G. Identifying sarcomere gene mutations in hypertrophic cardiomyopathy: a personal history. Circ. Res. 108, 743–750 (2011).
Walsh, R. et al. Reassessment of Mendelian gene pathogenicity using 7,855 cardiomyopathy cases and 60,706 reference samples. Genet. Med. 19, 192–203 (2017).
Ho, C. Y. et al. Genotype and lifetime burden of disease in hypertrophic cardiomyopathy: insights from the sarcomeric human cardiomyopathy registry (SHaRe). Circulation 138, 1387–1398 (2018).
Mazzarotto, F. et al. Reevaluating the genetic contribution of monogenic dilated cardiomyopathy. Circulation 141, 387–398 (2020).
Ingles, J. et al. Evaluating the clinical validity of hypertrophic cardiomyopathy genes. Circ. Genom. Precis. Med. 12, e002460 (2019).
Jordan, E. et al. An evidence-based assessment of genes in dilated cardiomyopathy. Circulation https://doi.org/10.1161/CIRCULATIONAHA.120.053033 (2021).
James, C. A. et al. International evidence based reappraisal of genes associated with arrhythmogenic right ventricular cardiomyopathy using the clinical genome resource framework. Circ. Genom. Precis. Med. 14, e003273 (2021).
Tadros, R. et al. Shared genetic pathways contribute to risk of hypertrophic and dilated cardiomyopathies with opposite directions of effect. Nat. Genet. 53, 128–134 (2021).
Harper, A. R. et al. Common genetic variants and modifiable risk factors underpin hypertrophic cardiomyopathy susceptibility and expressivity. Nat. Genet. 53, 135–142 (2021).
Pirruccello, J. P. et al. Analysis of cardiac magnetic resonance imaging in 36,000 individuals yields genetic insights into dilated cardiomyopathy. Nat. Commun. 11, 2254 (2020).
Ziane, R. et al. Cell membrane expression of cardiac sodium channel Na(v)1.5 is modulated by alpha-actinin-2 interaction. Biochemistry 49, 166–178 (2010).
Lu, L. et al. Molecular coupling of a Ca2+-activated K+ channel to L-type Ca2+ channels via alpha-actinin2. Circ. Res. 100, 112–120 (2007).
Chiu, C. et al. Mutations in alpha-actinin-2 cause hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 55, 1127–1135 (2010).
Girolami, F. et al. Novel α-actinin 2 variant associated with familial hypertrophic cardiomyopathy and juvenile atrial arrhythmias: a massively parallel sequencing study. Circ. Cardiovasc. Genet. 7, 741–750 (2014).
Bagnall, R. D., Molloy, L. K., Kalman, J. M. & Semsarian, C. Exome sequencing identifies a mutation in the ACTN2 gene in a family with idiopathic ventricular fibrillation, left ventricular noncompaction, and sudden death. BMC Med. Genet. 15, 99 (2014).
Prondzynski, M. et al. Disease modeling of a mutation in α-actinin 2 guides clinical therapy in hypertrophic cardiomyopathy. EMBO Mol. Med. 11, e11115 (2019).
Mazzarotto, F. et al. Systematic large-scale assessment of the genetic architecture of left ventricular noncompaction reveals diverse etiologies. Genet. Med. 23, 856–864 (2021).
Singer, E. S. et al. Characterization of clinically relevant copy-number variants from exomes of patients with inherited heart disease and unexplained sudden cardiac death. Genet. Med. 23, 86–93 (2021).
Lindholm, M. E. et al. Mono- and bi-allelic protein truncating variants in alpha-actinin 2 cause cardiomyopathy through distinct mechanisms. bioRxiv https://doi.org/10.1101/2020.11.19.389064 (2020).
Arvanitis, M. et al. Genome-wide association and multi-omic analyses reveal ACTN2 as a gene linked to heart failure. Nat. Commun. 11, 1122 (2020).
Almomani, R. et al. Biallelic truncating mutations in ALPK3 cause severe pediatric cardiomyopathy. J. Am. Coll. Cardiol. 67, 515–525 (2016).
Phelan, D. G. et al. ALPK3-deficient cardiomyocytes generated from patient-derived induced pluripotent stem cells and mutant human embryonic stem cells display abnormal calcium handling and establish that ALPK3 deficiency underlies familial cardiomyopathy. Eur. Heart J. 37, 2586–2590 (2016).
Çağlayan, A. O. et al. ALPK3 gene mutation in a patient with congenital cardiomyopathy and dysmorphic features. Cold Spring Harb. Mol. Case Stud. 3, a001859 (2017).
Jaouadi, H. et al. Novel ALPK3 mutation in a Tunisian patient with pediatric cardiomyopathy and facio-thoraco-skeletal features. J. Hum. Genet. 63, 1077–1082 (2018).
Al Senaidi, K. et al. Phenotypic spectrum of ALPK3-related cardiomyopathy. Am. J. Med. Genet. A 179, 1235–1240 (2019).
Jorholt, J. et al. Two new cases of hypertrophic cardiomyopathy and skeletal muscle features associated with ALPK3 homozygous and compound heterozygous variants. Genes 11, 1201 (2020).
Herkert, J. C. et al. Expanding the clinical and genetic spectrum of ALPK3 variants: phenotypes identified in pediatric cardiomyopathy patients and adults with heterozygous variants. Am. Heart J. 225, 108–119 (2020).
Lopes, L. R. et al. Alpha-protein kinase 3 (ALPK3) truncating variants are a cause of autosomal dominant hypertrophic cardiomyopathy. Eur. Heart J. https://doi.org/10.1093/eurheartj/ehab424 (2021).
Cheawsamoot, C. et al. A pathogenic variant in ALPK3 is associated with an autosomal dominant adult-onset hypertrophic cardiomyopathy. Circ. Genom. Precis. Med. 13, e003127 (2020).
Van Sligtenhorst, I. et al. Cardiomyopathy in α-kinase 3 (ALPK3)-deficient mice. Vet. Pathol. 49, 131–141 (2012).
Vafiadaki, E., Arvanitis, D. A. & Sanoudou, D. Muscle LIM protein: master regulator of cardiac and skeletal muscle functions. Gene 566, 1–7 (2015).
Walsh, R. et al. Defining the genetic architecture of hypertrophic cardiomyopathy: re-evaluating the role of non-sarcomeric genes. Eur. Heart J. 38, 3461–3468 (2017).
Geier, C. et al. Beyond the sarcomere: CSRP3 mutations cause hypertrophic cardiomyopathy. Hum. Mol. Genet. 17, 2753–2765 (2008).
Salazar-Mendiguchía, J. et al. The p.(Cys150Tyr) variant in CSRP3 is associated with late-onset hypertrophic cardiomyopathy in heterozygous individuals. Eur. J. Med. Genet. 63, 104079 (2020).
Janin, A., Bessière, F., Chauveau, S., Chevalier, P. & Millat, G. First identification of homozygous truncating CSRP3 variants in two unrelated cases with hypertrophic cardiomyopathy. Gene 676, 110–116 (2018).
Lipari, M. et al. Identification of a variant hotspot in MYBPC3 and of a novel CSRP3 autosomal recessive alteration in a cohort of Polish patients with hypertrophic cardiomyopathy. Pol. Arch. Intern. Med. 130, 89–99 (2020).
Arber, S. et al. MLP-deficient mice exhibit a disruption of cardiac cytoarchitectural organization, dilated cardiomyopathy, and heart failure. Cell 88, 393–403 (1997).
Knöll, R. et al. A common MLP (muscle LIM protein) variant is associated with cardiomyopathy. Circ. Res. 106, 695–704 (2010).
Taniguchi, K. et al. Mammalian formin Fhod3 regulates actin assembly and sarcomere organization in striated muscles. J. Biol. Chem. 284, 29873–29881 (2009).
Wooten, E. C. et al. Formin homology 2 domain containing 3 variants associated with hypertrophic cardiomyopathy. Circ. Cardiovasc. Genet. 6, 10–18 (2013).
Esslinger, U. et al. Exome-wide association study reveals novel susceptibility genes to sporadic dilated cardiomyopathy. PLoS One 12, e0172995 (2017).
Ochoa, J. P. et al. Formin homology 2 domain containing 3 (FHOD3) is a genetic basis for hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 72, 2457–2467 (2018).
Ochoa, J. P. et al. Deletions of specific exons of FHOD3 detected by next-generation sequencing are associated with hypertrophic cardiomyopathy. Clin. Genet. 98, 86–90 (2020).
Semsarian, C., Ingles, J. & Bagnall, R. D. Revisiting genome sequencing data in light of novel disease gene associations. J. Am. Coll. Cardiol. 73, 1365–1366 (2019).
Lesurf, R. et al. Whole genome sequencing delineates regulatory and novel genic variants in childhood cardiomyopathy. medRxiv https://doi.org/10.1101/2020.10.12.20211474 (2020).
Wu, G. et al. Variant spectrum of formin homology 2 domain-containing 3 gene in Chinese patients with hypertrophic cardiomyopathy. J. Am. Heart Assoc. 10, e018236 (2021).
Matsuyama, S. et al. Interaction between cardiac myosin-binding protein C and formin Fhod3. Proc. Natl Acad. Sci. USA 115, E4386–E4395 (2018).
Arimura, T. et al. Dilated cardiomyopathy-associated FHOD3 variant impairs the ability to induce activation of transcription factor serum response factor. Circ. J. 77, 2990–2996 (2013).
Kan-O, M. et al. Mammalian formin Fhod3 plays an essential role in cardiogenesis by organizing myofibrillogenesis. Biol. Open 1, 889–896 (2012).
Vorgerd, M. et al. A mutation in the dimerization domain of filamin c causes a novel type of autosomal dominant myofibrillar myopathy. Am. J. Hum. Genet. 77, 297–304 (2005).
Valdés-Mas, R. et al. Mutations in filamin C cause a new form of familial hypertrophic cardiomyopathy. Nat. Commun. 5, 5326 (2014).
Verdonschot, J. A. J. et al. A mutation update for the FLNC gene in myopathies and cardiomyopathies. Hum. Mutat. 41, 1091–1111 (2020).
Whiffin, N. et al. Using high-resolution variant frequencies to empower clinical genome interpretation. Genet. Med. 19, 1151–1158 (2017).
Gómez, J. et al. Screening of the Filamin C gene in a large cohort of hypertrophic cardiomyopathy patients. Circ. Cardiovasc. Genet. 10, e001584 (2017).
Cui, H. et al. Mutation profile of FLNC gene and its prognostic relevance in patients with hypertrophic cardiomyopathy. Mol. Genet. Genomic Med. 6, 1104–1113 (2018).
Thomson, K. L. et al. Analysis of 51 proposed hypertrophic cardiomyopathy genes from genome sequencing data in sarcomere negative cases has negligible diagnostic yield. Genet. Med. 21, 1576–1584 (2019).
Ortiz-Genga, M. F. et al. Truncating FLNC mutations are associated with high-risk dilated and arrhythmogenic cardiomyopathies. J. Am. Coll. Cardiol. 68, 2440–2451 (2016).
Begay, R. L. et al. Filamin C truncation mutations are associated with arrhythmogenic dilated cardiomyopathy and changes in the cell-cell adhesion structures. JACC Clin. Electrophysiol. 4, 504–514 (2018).
Ader, F. et al. FLNC pathogenic variants in patients with cardiomyopathies: prevalence and genotype-phenotype correlations. Clin. Genet. 96, 317–329 (2019).
Janin, A. et al. Truncating mutations on myofibrillar myopathies causing genes as prevalent molecular explanations on patients with dilated cardiomyopathy. Clin. Genet. 92, 616–623 (2017).
Hall, C. L. et al. Filamin C variants are associated with a distinctive clinical and immunohistochemical arrhythmogenic cardiomyopathy phenotype. Int. J. Cardiol. 307, 101–108 (2020).
Goli, R. et al. Genetic and phenotypic landscape of peripartum cardiomyopathy. Circulation 143, 1852–1862 (2021).
Dalkilic, I., Schienda, J., Thompson, T. G. & Kunkel, L. M. Loss of FilaminC (FLNc) results in severe defects in myogenesis and myotube structure. Mol. Cell. Biol. 26, 6522–6534 (2006).
van der Zwaag, P. A. et al. Phospholamban R14del mutation in patients diagnosed with dilated cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy: evidence supporting the concept of arrhythmogenic cardiomyopathy. Eur. J. Heart Fail. 14, 1199–1207 (2012).
Schmitt, J. P. et al. Dilated cardiomyopathy and heart failure caused by a mutation in phospholamban. Science 299, 1410–1413 (2003).
Haghighi, K. et al. Human phospholamban null results in lethal dilated cardiomyopathy revealing a critical difference between mouse and human. J. Clin. Invest. 111, 869–876 (2003).
Li, Z. et al. A PLN nonsense variant causes severe dilated cardiomyopathy in a novel autosomal recessive inheritance mode. Int. J. Cardiol. 279, 122–125 (2019).
Mademont-Soler, I. et al. Additional value of screening for minor genes and copy number variants in hypertrophic cardiomyopathy. PLoS One 12, e0181465 (2017).
Vanninen, S. U. M. et al. Heterozygous junctophilin-2 (JPH2) p.(Thr161Lys) is a monogenic cause for HCM with heart failure. PLoS One 13, e0203422 (2018).
Sabater-Molina, M. et al. Mutation in JPH2 cause dilated cardiomyopathy. Clin. Genet. 90, 468–469 (2016).
Vasilescu, C. et al. Genetic basis of severe childhood-onset cardiomyopathies. J. Am. Coll. Cardiol. 72, 2324–2338 (2018).
Jones, E. G. et al. Analysis of enriched rare variants in JPH2-encoded junctophilin-2 among greater middle eastern individuals reveals a novel homozygous variant associated with neonatal dilated cardiomyopathy. Sci. Rep. 9, 9038 (2019).
Takeshima, H., Komazaki, S., Nishi, M., Iino, M. & Kangawa, K. Junctophilins: a novel family of junctional membrane complex proteins. Mol. Cell 6, 11–22 (2000).
Salazar-Mendiguchía, J. et al. Mutations in TRIM63 cause an autosomal-recessive form of hypertrophic cardiomyopathy. Heart 106, 1342–1348 (2020).
Su, M. et al. Rare variants in genes encoding MuRF1 and MuRF2 are modifiers of hypertrophic cardiomyopathy. Int. J. Mol. Sci. 15, 9302–9313 (2014).
Witt, C. C. et al. Cooperative control of striated muscle mass and metabolism by MuRF1 and MuRF2. EMBO J. 27, 350–360 (2008).
Willis, M. S. et al. Muscle ring finger 1, but not muscle ring finger 2, regulates cardiac hypertrophy in vivo. Circ. Res. 100, 456–459 (2007).
Hedberg-Oldfors, C. et al. Cardiomyopathy with lethal arrhythmias associated with inactivation of KLHL24. Hum. Mol. Genet. 28, 1919–1929 (2019).
Lin, Z. et al. Stabilizing mutations of KLHL24 ubiquitin ligase cause loss of keratin 14 and human skin fragility. Nat. Genet. 48, 1508–1516 (2016).
Schwieger-Briel, A. et al. Epidermolysis bullosa simplex with KLHL24 mutations is associated with dilated cardiomyopathy. J. Invest. Dermatol. 139, 244–249 (2019).
Vermeer, M. C. S. C. et al. Gain-of-function mutation in ubiquitin-ligase KLHL24 causes desmin degradation and dilatation in hiPSC-derived engineered heart tissues. J. Clin. Invest. https://doi.org/10.1172/JCI140615 (2021).
Domínguez, F. et al. Dilated cardiomyopathy due to BLC2-associated athanogene 3 (BAG3) mutations. J. Am. Coll. Cardiol. 72, 2471–2481 (2018).
Alfares, A. A. et al. Results of clinical genetic testing of 2,912 probands with hypertrophic cardiomyopathy: expanded panels offer limited additional sensitivity. Genet. Med. 17, 880–888 (2015).
Kelly, M. A. et al. Adaptation and validation of the ACMG/AMP variant classification framework for MYH7-associated inherited cardiomyopathies: recommendations by ClinGen’s inherited cardiomyopathy expert panel. Genet. Med. 20, 351–359 (2018).
Walsh, R. et al. Quantitative approaches to variant classification increase the yield and precision of genetic testing in Mendelian diseases: the case of hypertrophic cardiomyopathy. Genome Med. 11, 5 (2019).
Olivotto, I. et al. Obesity and its association to phenotype and clinical course in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 62, 449–457 (2013).
Castel, S. E. et al. Modified penetrance of coding variants by cis-regulatory variation contributes to disease risk. Nat. Genet. 50, 1327–1334 (2018).
Neubauer, S. et al. Distinct subgroups in hypertrophic cardiomyopathy in the NHLBI HCM registry. J. Am. Coll. Cardiol. 74, 2333–2345 (2019).
Montefiori, L. E. et al. A promoter interaction map for cardiovascular disease genetics. eLife 7, e35788 (2018).
Acknowledgements
The authors are supported by an Amsterdam Cardiovascular Sciences fellowship, Amsterdam UMC’s PhD scholarship, the Canadian Heart Rhythm Society (George Mines Award), the ESC (Research fellowship grant), the Canadian Institutes of Health Research (reference 169063), the Fonds de Recherche du Québec—Santé (reference 135055 [R.T.]), the Dutch Heart Foundation Netherlands Cardiovascular Research Initiative (CVON; PREDICT2 2018-30), the Netherlands Organization for Scientific Research (VICI fellowship, 016.150.610), the Leducq Foundation (project 17CVD02) and the Horstingstuit Foundation.
Author information
Authors and Affiliations
Contributions
R.W. and J.A.O. researched data for the article and wrote the manuscript. All the authors made substantial contributions to discussions of the content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks D. Jacoby, J. Seidman and G. Sinagra for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinGen: https://clinicalgenome.org/
Supplementary information
Glossary
- Genetic pleiotropy
-
Variants in a gene can lead to two or more unrelated phenotypes or related conditions in which the direction of effect might differ.
- Protein-truncating variants
-
Variants that disrupt the open reading frame of a transcript, often (but not always) leading to the degradation of the disrupted mRNA through nonsense-mediated decay, which causes haploinsufficiency.
- Case–control association testing
-
Demonstration of a significant aggregated enrichment of rare variants in a gene in case cohorts compared with controls can establish a Mendelian gene–disease association.
- ClinGen
-
ClinGen, the Clinical Genome Resource, is an NIH-funded resource that aims to define the clinical relevance of genes implicated in inherited genetic diseases through structured curation and evaluation of published evidence.
- Incomplete penetrance
-
Only a subset of individuals with a particular pathogenic variant have the clinical phenotype, highlighting the role of other genetic and non-genetic factors.
- Biallelic variants
-
Biallelic loss-of-function variants are homozygous or compound heterozygous variants associated with recessive disease, usually truncating variants but can also be function-altering missense variants, equivalent to ‘human knockouts’.
- Haplotypes
-
A group of alleles that are inherited together; genome-wide association study signals usually comprise haplotypes of numerous common variants in linkage disequilibrium, any of which might be the functional variant.
- Expression quantitative trait locus
-
(eQTL). Shows that genetic variants or loci are associated with changes in gene expression in particular tissues.
Rights and permissions
About this article
Cite this article
Walsh, R., Offerhaus, J.A., Tadros, R. et al. Minor hypertrophic cardiomyopathy genes, major insights into the genetics of cardiomyopathies. Nat Rev Cardiol 19, 151–167 (2022). https://doi.org/10.1038/s41569-021-00608-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-021-00608-2
This article is cited by
-
Heptagonal Reinforcement Learning (HRL): a novel algorithm for early prevention of non-sinus cardiac arrhythmia
Journal of Ambient Intelligence and Humanized Computing (2024)
-
The China Hypertrophic Cardiomyopathy Project (CHCMP): The Rationale and Design of a Multicenter, Prospective, Registry Cohort Study
Journal of Cardiovascular Translational Research (2024)
-
Mechano-energetic efficiency in patients with hypertrophic cardiomyopathy with and without sarcomeric mutations
Journal of Cardiovascular Translational Research (2024)
-
Safety and efficacy of mavacamten for treatment of hypertrophic cardiomyopathy: a systematic review and meta-analysis of randomized clinical trials
The Egyptian Heart Journal (2023)
-
Exploring the complex spectrum of dominance and recessiveness in genetic cardiomyopathies
Nature Cardiovascular Research (2023)