Abstract
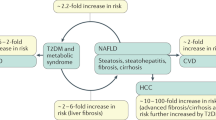
The liver is a crucial metabolic organ that has a key role in maintaining immune and endocrine homeostasis. Accumulating evidence suggests that chronic liver disease might promote the development of various cardiac disorders (such as arrhythmias and cardiomyopathy) and circulatory complications (including systemic, splanchnic and pulmonary complications), which can eventually culminate in clinical conditions ranging from portal and pulmonary hypertension to pulmonary, cardiac and renal failure, ascites and encephalopathy. Liver diseases can affect cardiovascular function during the early stages of disease progression. The development of cardiovascular diseases in patients with chronic liver failure is associated with increased morbidity and mortality, and cardiovascular complications can in turn affect liver function and liver disease progression. Furthermore, numerous infectious, inflammatory, metabolic and genetic diseases, as well as alcohol abuse can also influence both hepatic and cardiovascular outcomes. In this Review, we highlight how chronic liver diseases and associated cardiovascular effects can influence different organ pathologies. Furthermore, we explore the potential roles of inflammation, oxidative stress, vasoactive mediator imbalance, dysregulated endocannabinoid and autonomic nervous systems and endothelial dysfunction in mediating the complex interplay between the liver and the systemic vasculature that results in the development of the extrahepatic complications of chronic liver disease. The roles of ageing, sex, the gut microbiome and organ transplantation in this complex interplay are also discussed.
Key points
-
Chronic liver diseases (CLD) trigger the development of severe extrahepatic complications, including cirrhotic cardiomyopathy, hepatorenal syndrome, ascites, hepatopulmonary syndrome, portopulmonary hypertension, gastrointestinal bleeding and hepatic encephalopathy, which are associated with further increased risk of death.
-
The extrahepatic complications of CLD are often overlooked or diagnosed late into the disease process owing to the lack of specific diagnostic markers, which results in delayed treatment.
-
No definitive therapies are available for the treatment of these extrahepatic complications of CLD with the exception of liver transplantation, but the presence of these complications might preclude eligibility for liver transplantation.
-
Novel disease-modifying treatment strategies targeted at counteracting one or more of the pathophysiological mechanisms involved in the development of CLD and its extrahepatic complications are needed and their investigation is warranted.
-
Potential future research areas for the extrahepatic complications of CLD include the effects of ageing, sex and the gut microbiome on disease progression and the development of novel biomarkers for early diagnosis.
-
The identification of shared pathophysiological pathways underlying these extrahepatic complications will facilitate the development of more specific drug therapies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Schuppan, D. & Afdhal, N. H. Liver cirrhosis. Lancet 371, 838–851 (2008).
Moon, A. M., Singal, A. G. & Tapper, E. B. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin. Gastroenterol. Hepatol. https://doi.org/10.1016/j.cgh.2019.07.060 (2019).
Do, A., Kuszewski, E. J., Langberg, K. A. & Mehal, W. Z. Incorporating weight loss medications into hepatology practice for nonalcoholic steatohepatitis. Hepatology 70, 1443–1456 (2019).
Pimpin, L. et al. Burden of liver disease in Europe: epidemiology and analysis of risk factors to identify prevention policies. J. Hepatol. 69, 718–735 (2018).
Tapper, E. B. & Parikh, N. D. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ 362, k2817 (2018).
Wong, R. J. et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 148, 547–555 (2015).
Ko, J. S. New perspectives in pediatric nonalcoholic fatty liver disease: epidemiology, genetics, diagnosis, and natural history. Pediatr. Gastroenterol. Hepatol. Nutr. 22, 501–510 (2019).
World Health Organization. World health statistics 2018: monitoring health for the SDGs, sustainable development goals (WHO, 2018).
Gracia-Sancho, J., Marrone, G. & Fernandez-Iglesias, A. Hepatic microcirculation and mechanisms of portal hypertension. Nat. Rev. Gastroenterol. Hepatol. 16, 221–234 (2019).
Moller, S. & Bendtsen, F. Complications of cirrhosis. A 50 years flashback. Scand. J. Gastroenterol. 50, 763–780 (2015).
Bernardi, M., Moreau, R., Angeli, P., Schnabl, B. & Arroyo, V. Mechanisms of decompensation and organ failure in cirrhosis: from peripheral arterial vasodilation to systemic inflammation hypothesis. J. Hepatol. 63, 1272–1284 (2015).
Matyas, C. et al. Interplay of liver-heart inflammatory axis and cannabinoid 2 receptor signalling in an experimental model of hepatic cardiomyopathy. Hepatology 71, 1391–1284 (2020).
Trojnar, E. et al. Cannabinoid-2 receptor activation ameliorates hepatorenal syndrome. Free Radic. Biol. Med. 152, 540–550 (2020).
Wijdicks, E. F. Hepatic encephalopathy. N. Engl. J. Med. 375, 1660–1670 (2016).
Wiese, S., Hove, J. D. & Moller, S. Cardiac imaging in patients with chronic liver disease. Clin. Physiol. Funct. Imaging 37, 347–356 (2017).
Kowalski, H. J. & Abelmann, W. H. The cardiac output at rest in Laennec’s cirrhosis. J. Clin. Invest. 32, 1025–1033 (1953).
Izzy, M. et al. Redefining cirrhotic cardiomyopathy for the modern era. Hepatology 71, 334–345 (2020).
Moller, S., Danielsen, K. V., Wiese, S., Hove, J. D. & Bendtsen, F. An update on cirrhotic cardiomyopathy. Expert Rev. Gastroenterol. Hepatol. 13, 497–505 (2019).
Wiese, S., Hove, J. D., Bendtsen, F. & Moller, S. Cirrhotic cardiomyopathy: pathogenesis and clinical relevance. Nat. Rev. Gastroenterol. Hepatol. 11, 177–186 (2014).
Nazar, A. et al. Left ventricular function assessed by echocardiography in cirrhosis: relationship to systemic hemodynamics and renal dysfunction. J. Hepatol. 58, 51–57 (2013).
Cazzaniga, M. et al. Diastolic dysfunction is associated with poor survival in patients with cirrhosis with transjugular intrahepatic portosystemic shunt. Gut 56, 869–875 (2007).
Eyvazian, V. A. et al. Incidence, predictors, and outcomes of new-onset left ventricular systolic dysfunction after orthotopic liver transplantation. J. Card. Fail. 25, 166–172 (2019).
Shin, W. J. et al. Effect of ventriculo-arterial coupling on transplant outcomes in cirrhotics: analysis of pressure-volume curve relations. J. Hepatol. 66, 328–337 (2017).
Ruiz-del-Arbol, L. et al. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology 58, 1732–1741 (2013).
Premkumar, M. et al. Left ventricular diastolic dysfunction is associated with renal dysfunction, poor survival and low health related quality of life in cirrhosis. J. Clin. Exp. Hepatol. 9, 324–333 (2019).
Wiese, S. et al. Myocardial extracellular volume quantified by magnetic resonance is increased in cirrhosis and related to poor outcome. Liver Int. 38, 1614–1623 (2018).
Lee, S. K., Song, M. J., Kim, S. H. & Ahn, H. J. Cardiac diastolic dysfunction predicts poor prognosis in patients with decompensated liver cirrhosis. Clin. Mol. Hepatol. 24, 409–416 (2018).
Desai, M. S. et al. Bile acid excess induces cardiomyopathy and metabolic dysfunctions in the heart. Hepatology 65, 189–201 (2017).
Bortoluzzi, A. et al. Positive cardiac inotropic effect of albumin infusion in rodents with cirrhosis and ascites: molecular mechanisms. Hepatology 57, 266–276 (2013).
Jarkovska, D. et al. Expression of classical mediators in hearts of rats with hepatic dysfunction. Can. J. Physiol. Pharmacol. 95, 1351–1359 (2017).
Henriksen, J. H. et al. Increased circulating pro-brain natriuretic peptide (proBNP) and brain natriuretic peptide (BNP) in patients with cirrhosis: relation to cardiovascular dysfunction and severity of disease. Gut 52, 1511–1517 (2003).
Coss, E. et al. Predictors of cardiovascular events after liver transplantation: a role for pretransplant serum troponin levels. Liver Transpl. 17, 23–31 (2011).
Watt, K. D. et al. Pretransplant serum troponin levels are highly predictive of patient and graft survival following liver transplantation. Liver Transpl. 16, 990–998 (2010).
Wiese, S. et al. Cardiac and proinflammatory markers predict prognosis in cirrhosis. Liver Int. 34, e19–e30 (2014).
Wiese, S. et al. Cardiac dysfunction in cirrhosis: a 2-yr longitudinal follow-up study using advanced cardiac imaging. Am. J. Physiol. Gastrointest. Liver Physiol. 317, G253–G263 (2019).
Koshy, A. N. et al. Impaired cardiac reserve on dobutamine stress echocardiography predicts the development of hepatorenal syndrome. Am. J. Gastroenterol. 115, 388–397 (2020).
Moller, S. & Bernardi, M. Interactions of the heart and the liver. Eur. Heart J. 34, 2804–2811 (2013).
Henriksen, J. H., Fuglsang, S. & Bendtsen, F. Arterial pressure profile in patients with cirrhosis: Fourier analysis of arterial pulse in relation to pressure level, stroke volume, and severity of disease: on the reduction of afterload in the hyperdynamic syndrome. Scand. J. Gastroenterol. 47, 580–590 (2012).
Robotham, J. L., Takata, M., Berman, M. & Harasawa, Y. Ejection fraction revisited. Anesthesiology 74, 172–183 (1991).
Israelsen, M. et al. Dobutamine reverses the cardio-suppressive effects of terlipressin without improving renal function in cirrhosis and ascites: a randomised controlled trial. Am. J. Physiol. Gastrointest. Liver Physiol. 318, G313–G321 (2020).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 28, 1–39.e14 (2015).
Zamirian, M. et al. Reduced myocardial reserve in cirrhotic patients: an evaluation by dobutamine stress speckle tracking and tissue Doppler imaging (TDI) echocardiography. J. Cardiovasc. Thorac. Res. 11, 127–131 (2019).
Rimbas, R. C. et al. New definition criteria of myocardial dysfunction in patients with liver cirrhosis: a speckle tracking and tissue doppler imaging study. Ultrasound Med. Biol. 44, 562–574 (2018).
Moller, S., Wiese, S., Halgreen, H. & Hove, J. D. Diastolic dysfunction in cirrhosis. Heart Fail. Rev. 21, 599–610 (2016).
Dowsley, T. F. et al. Diastolic dysfunction in patients with end-stage liver disease is associated with development of heart failure early after liver transplantation. Transplantation 94, 646–651 (2012).
Tsiompanidis, E. et al. Liver cirrhosis-effect on QT interval and cardiac autonomic nervous system activity. World J. Gastrointest. Pathophysiol. 9, 28–36 (2018).
Huang, W. A., Dunipace, E. A., Sorg, J. M. & Vaseghi, M. Liver disease as a predictor of new-onset atrial fibrillation. J. Am. Heart Assoc. 7, e008703 (2018).
Adejumo, A. C. et al. Predictors, burden and impact of cardiac arrhythmias among patients hospitalized with end-stage liver disease. Heart Lung 49, 73–79 (2020).
Chokesuwattanaskul, R. et al. Liver transplantation and atrial fibrillation: a meta-analysis. World J. Hepatol. 10, 761–771 (2018).
Berzigotti, A., Seijo, S., Reverter, E. & Bosch, J. Assessing portal hypertension in liver diseases. Expert Rev. Gastroenterol. Hepatol. 7, 141–155 (2013).
Bosch, J., Groszmann, R. J. & Shah, V. H. Evolution in the understanding of the pathophysiological basis of portal hypertension: how changes in paradigm are leading to successful new treatments. J. Hepatol. 62, S121–S130 (2015).
Groszmann, R. J. et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N. Engl. J. Med. 353, 2254–2261 (2005).
Ripoll, C. et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 133, 481–488 (2007).
Ripoll, C. et al. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. J. Hepatol. 50, 923–928 (2009).
Moitinho, E. et al. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology 117, 626–631 (1999).
D’Amico, G., Garcia-Pagan, J. C., Luca, A. & Bosch, J. Hepatic vein pressure gradient reduction and prevention of variceal bleeding in cirrhosis: a systematic review. Gastroenterology 131, 1611–1624 (2006).
Moller, S. & Bendtsen, F. The pathophysiology of arterial vasodilatation and hyperdynamic circulation in cirrhosis. Liver Int. 38, 570–580 (2018).
Bolognesi, M., Di Pascoli, M., Verardo, A. & Gatta, A. Splanchnic vasodilation and hyperdynamic circulatory syndrome in cirrhosis. World J. Gastroenterol. 20, 2555–2563 (2014).
Moller, S., Kimer, N., Barlose, M. & Bendtsen, F. Pathophysiological-based treatments of complications of cirrhosis. Scand. J. Gastroenterol. 55, 383–394 (2020).
Schrier, R. W. Water and sodium retention in edematous disorders: role of vasopressin and aldosterone. Am. J. Med. 119, S47–S53 (2006).
Moller, S., Henriksen, J. H. & Bendtsen, F. Ascites: pathogenesis and therapeutic principles. Scand. J. Gastroenterol. 44, 902–911 (2009).
European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J. Hepatol. 53, 397–417 (2010).
Gines, P. et al. Hepatorenal syndrome. Nat. Rev. Dis. Primers 4, 23 (2018).
Angeli, P., Garcia-Tsao, G., Nadim, M. K. & Parikh, C. R. News in pathophysiology, definition and classification of hepatorenal syndrome: a step beyond the International Club of Ascites (ICA) consensus document. J. Hepatol. 71, 811–822 (2019).
Velez, J. C. Q., Therapondos, G. & Juncos, L. A. Reappraising the spectrum of AKI and hepatorenal syndrome in patients with cirrhosis. Nat. Rev. Nephrol. 16, 137–155 (2020).
Sole, C., Pose, E., Sola, E. & Gines, P. Hepatorenal syndrome in the era of acute kidney injury. Liver Int. 38, 1891–1901 (2018).
Puthumana, J. et al. Urine interleukin 18 and lipocalin 2 are biomarkers of acute tubular necrosis in patients with cirrhosis: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 15, 1003–1013.e3 (2017).
Best, L. M. et al. Treatment for hepatorenal syndrome in people with decompensated liver cirrhosis: a network meta-analysis. Cochrane Database Syst. Rev. 9, CD013103 (2019).
Mandorfer, M. et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology 146, 1680–1690.e1 (2014).
Krowka, M. J. et al. International Liver Transplant Society practice guidelines: diagnosis and management of hepatopulmonary syndrome and portopulmonary hypertension. Transplantation 100, 1440–1452 (2016).
Cartin-Ceba, R. & Krowka, M. J. Pulmonary complications of portal hypertension. Clin. Liver Dis. 23, 683–711 (2019).
Koch, D. G. & Fallon, M. B. Hepatopulmonary syndrome. Clin. Liver Dis. 18, 407–420 (2014).
Iqbal, S., Smith, K. A. & Khungar, V. Hepatopulmonary syndrome and portopulmonary hypertension: implications for liver transplantation. Clin. Chest Med. 38, 785–795 (2017).
Savale, L., Watherald, J. & Sitbon, O. Portopulmonary hypertension. Semin. Respir. Crit. Care Med. 38, 651–661 (2017).
Sitbon, O. et al. Macitentan for the treatment of portopulmonary hypertension (PORTICO): a multicentre, randomised, double-blind, placebo-controlled, phase 4 trial. Lancet Respir. Med. 7, 594–604 (2019).
Swanson, K. L., Wiesner, R. H., Nyberg, S. L., Rosen, C. B. & Krowka, M. J. Survival in portopulmonary hypertension: Mayo Clinic experience categorized by treatment subgroups. Am. J. Transpl. 8, 2445–2453 (2008).
Krowka, M. J., Swanson, K. L., Frantz, R. P., McGoon, M. D. & Wiesner, R. H. Portopulmonary hypertension: results from a 10-year screening algorithm. Hepatology 44, 1502–1510 (2006).
AbuHalimeh, B., Krowka, M. J. & Tonelli, A. R. Treatment barriers in portopulmonary hypertension. Hepatology 69, 431–443 (2019).
Jayakumar, A. R., Rama Rao, K. V. & Norenberg, M. D. Neuroinflammation in hepatic encephalopathy: mechanistic aspects. J. Clin. Exp. Hepatol. 5, S21–S28 (2015).
Bajaj, J. S. Hepatic encephalopathy: classification and treatment. J. Hepatol. 68, 838–839 (2018).
Cordoba, J. et al. Characteristics, risk factors, and mortality of cirrhotic patients hospitalized for hepatic encephalopathy with and without acute-on-chronic liver failure (ACLF). J. Hepatol. 60, 275–281 (2014).
Bjerring, P. N., Gluud, L. L. & Larsen, F. S. Cerebral blood flow and metabolism in hepatic encephalopathy–a meta-analysis. J. Clin. Exp. Hepatol. 8, 286–293 (2018).
Bajaj, J. S. et al. Minimal hepatic encephalopathy and mild cognitive impairment worsen quality of life in elderly patients with cirrhosis. Clin. Gastroenterol. Hepatol. https://doi.org/10.1016/j.cgh.2020.03.033 (2020).
Nardelli, S. et al. Muscle alterations are associated with minimal and overt hepatic encephalopathy in patients with liver cirrhosis. Hepatology 70, 1704–1713 (2019).
Hanai, T. et al. Sarcopenia predicts minimal hepatic encephalopathy in patients with liver cirrhosis. Hepatol. Res. 47, 1359–1367 (2017).
Vilstrup, H. et al. Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 60, 715–735 (2014).
Dirchwolf, M. & Ruf, A. E. Role of systemic inflammation in cirrhosis: from pathogenesis to prognosis. World J. Hepatol. 7, 1974–1981 (2015).
Seo, Y. S. & Shah, V. H. The role of gut-liver axis in the pathogenesis of liver cirrhosis and portal hypertension. Clin. Mol. Hepatol. 18, 337–346 (2012).
Chia, S. et al. Intra-arterial tumor necrosis factor-α impairs endothelium-dependent vasodilatation and stimulates local tissue plasminogen activator release in humans. Arterioscler. Thromb. Vasc. Biol. 23, 695–701 (2003).
Rajesh, M. et al. CB2-receptor stimulation attenuates TNF-α-induced human endothelial cell activation, transendothelial migration of monocytes, and monocyte-endothelial adhesion. Am. J. Physiol. Heart Circ. Physiol. 293, H2210–H2218 (2007).
Balasubramaniyan, V. et al. Ammonia reduction with ornithine phenylacetate restores brain eNOS activity via the DDAH-ADMA pathway in bile duct-ligated cirrhotic rats. Am. J. Physiol. Gastrointest. Liver Physiol. 302, G145–G152 (2012).
Maciejewski, J. P. et al. Nitric oxide suppression of human hematopoiesis in vitro. Contribution to inhibitory action of interferon-gamma and tumor necrosis factor-alpha. J. Clin. Invest. 96, 1085–1092 (1995).
Bulotta, S., Barsacchi, R., Rotiroti, D., Borgese, N. & Clementi, E. Activation of the endothelial nitric-oxide synthase by tumor necrosis factor-α. A novel feedback mechanism regulating cell death. J. Biol. Chem. 276, 6529–6536 (2001).
McClain, C. J., Barve, S., Deaciuc, I., Kugelmas, M. & Hill, D. Cytokines in alcoholic liver disease. Semin. Liver Dis. 19, 205–219 (1999).
Bird, G. L., Sheron, N., Goka, A. K., Alexander, G. J. & Williams, R. S. Increased plasma tumor necrosis factor in severe alcoholic hepatitis. Ann. Intern. Med. 112, 917–920 (1990).
Henao-Mejia, J. et al. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature 482, 179–185 (2012).
Nawaz, R. et al. HCV-induced regulatory alterations of IL-1β, IL-6, TNF-α, and IFN- ϒ operative, leading liver en-route to non-alcoholic steatohepatitis. Inflamm. Res. 66, 477–486 (2017).
Thenappan, T. et al. A central role for CD68(+) macrophages in hepatopulmonary syndrome. Reversal by macrophage depletion. Am. J. Respir. Crit. Care Med. 183, 1080–1091 (2011).
Zhang, J. et al. The role of CX(3)CL1/CX(3)CR1 in pulmonary angiogenesis and intravascular monocyte accumulation in rat experimental hepatopulmonary syndrome. J. Hepatol. 57, 752–758 (2012).
Sztrymf, B. et al. Cirrhotic rats with bacterial translocation have higher incidence and severity of hepatopulmonary syndrome. J. Gastroenterol. Hepatol. 20, 1538–1544 (2005).
Varga, Z. V. et al. Disruption of renal arginine metabolism promotes kidney injury in hepatorenal syndrome in mice. Hepatology 68, 1519–1533 (2018).
Shah, N. et al. Prevention of acute kidney injury in a rodent model of cirrhosis following selective gut decontamination is associated with reduced renal TLR4 expression. J. Hepatol. 56, 1047–1053 (2012).
Karagiannakis, D. S., Vlachogiannakos, J., Anastasiadis, G., Vafiadis-Zouboulis, I. & Ladas, S. D. Frequency and severity of cirrhotic cardiomyopathy and its possible relationship with bacterial endotoxemia. Dig. Dis. Sci. 58, 3029–3036 (2013).
Liu, H., Ma, Z. & Lee, S. S. Contribution of nitric oxide to the pathogenesis of cirrhotic cardiomyopathy in bile duct-ligated rats. Gastroenterology 118, 937–944 (2000).
Yang, Y. Y., Liu, H., Nam, S. W., Kunos, G. & Lee, S. S. Mechanisms of TNFα-induced cardiac dysfunction in cholestatic bile duct-ligated mice: interaction between TNFα and endocannabinoids. J. Hepatol. 53, 298–306 (2010).
Gaskari, S. A., Liu, H., D’Mello, C., Kunos, G. & Lee, S. S. Blunted cardiac response to hemorrhage in cirrhotic rats is mediated by local macrophage-released endocannabinoids. J. Hepatol. 62, 1272–1277 (2015).
Padillo, F. J. et al. Anti-TNF-α treatment and bile duct drainage restore cellular immunity and prevent tissue injury in experimental obstructive jaundice. Int. J. Immunopathol. Pharmacol. 20, 855–860 (2007).
Sheen, J. M. et al. Combined intraperitoneal and intrathecal etanercept reduce increased brain tumor necrosis factor-alpha and asymmetric dimethylarginine levels and rescues spatial deficits in young rats after bile duct ligation. Front. Cell Neurosci. 10, 167 (2016).
Shah, N. et al. Increased renal expression and urinary excretion of TLR4 in acute kidney injury associated with cirrhosis. Liver Int. 33, 398–409 (2013).
Yi, H. et al. The association of lipopolysaccharide and inflammatory factors with hepatopulmonary syndrome and their changes after orthotopic liver transplantation. J. Thorac. Dis. 6, 1469–1475 (2014).
Rodrigo, R. et al. Hyperammonemia induces neuroinflammation that contributes to cognitive impairment in rats with hepatic encephalopathy. Gastroenterology 139, 675–684 (2010).
Ochoa-Sanchez, R. & Rose, C. F. Pathogenesis of hepatic encephalopathy in chronic liver disease. J. Clin. Exp. Hepatol. 8, 262–271 (2018).
Rai, R. et al. Reversal of low-grade cerebral edema after lactulose/rifaximin therapy in patients with cirrhosis and minimal hepatic encephalopathy. Clin. Transl. Gastroenterol. 6, e111 (2015).
Jain, L. et al. Serum endotoxin, inflammatory mediators, and magnetic resonance spectroscopy before and after treatment in patients with minimal hepatic encephalopathy. J. Gastroenterol. Hepatol. 28, 1187–1193 (2013).
Fallon, M. B., Abrams, G. A., McGrath, J. W., Hou, Z. & Luo, B. Common bile duct ligation in the rat: a model of intrapulmonary vasodilatation and hepatopulmonary syndrome. Am. J. Physiol. 272, G779–G784 (1997).
Raevens, S. & Fallon, M. B. Potential clinical targets in hepatopulmonary syndrome: lessons from experimental models. Hepatology 68, 2016–2028 (2018).
Oberti, F. et al. Prevention of portal hypertension by propranolol and spironolactone in rats with bile duct ligation. J. Hepatol. 26, 167–173 (1997).
Pacher, P., Beckman, J. S. & Liaudet, L. Nitric oxide and peroxynitrite in health and disease. Physiol. Rev. 87, 315–424 (2007).
Gracia-Sancho, J. et al. Increased oxidative stress in cirrhotic rat livers: a potential mechanism contributing to reduced nitric oxide bioavailability. Hepatology 47, 1248–1256 (2008).
Vasquez-Vivar, J., Whitsett, J., Martasek, P., Hogg, N. & Kalyanaraman, B. Reaction of tetrahydrobiopterin with superoxide: EPR-kinetic analysis and characterization of the pteridine radical. Free Radic. Biol. Med. 31, 975–985 (2001).
Ungvari, Z. et al. Endothelial dysfunction and angiogenesis impairment in the ageing vasculature. Nat. Rev. Cardiol. 15, 555–565 (2018).
Szabo, C., Ischiropoulos, H. & Radi, R. Peroxynitrite: biochemistry, pathophysiology and development of therapeutics. Nat. Rev. Drug Discov. 6, 662–680 (2007).
Matei, V. et al. The eNOS cofactor tetrahydrobiopterin improves endothelial dysfunction in livers of rats with CCl4 cirrhosis. Hepatology 44, 44–52 (2006).
Morales-Ruiz, M. et al. Transduction of the liver with activated Akt normalizes portal pressure in cirrhotic rats. Gastroenterology 125, 522–531 (2003).
Shah, V. et al. Impaired endothelial nitric oxide synthase activity associated with enhanced caveolin binding in experimental cirrhosis in the rat. Gastroenterology 117, 1222–1228 (1999).
Hernandez-Guerra, M. et al. Ascorbic acid improves the intrahepatic endothelial dysfunction of patients with cirrhosis and portal hypertension. Hepatology 43, 485–491 (2006).
Nickovic, V. P. et al. Oxidative stress, NOx/l-arginine ratio and glutathione/glutathione S-transferase ratio as predictors of ‘sterile inflammation’ in patients with alcoholic cirrhosis and hepatorenal syndrome type II. Ren. Fail. 40, 340–349 (2018).
Terao, M. et al. Serum oxidative/anti-oxidative stress balance is dysregulated in potentially pulmonary hypertensive patients with liver cirrhosis: a case control study. Intern. Med. 54, 2815–2826 (2015).
Vercelino, R. et al. N-acetylcysteine effects on genotoxic and oxidative stress parameters in cirrhotic rats with hepatopulmonary syndrome. Basic Clin. Pharmacol. Toxicol. 102, 370–376 (2008).
Tieppo, J. et al. Quercetin administration ameliorates pulmonary complications of cirrhosis in rats. J. Nutr. 139, 1339–1346 (2009).
Montoliu, C. et al. 3-nitro-tyrosine as a peripheral biomarker of minimal hepatic encephalopathy in patients with liver cirrhosis. Am. J. Gastroenterol. 106, 1629–1637 (2011).
Gorg, B. et al. Oxidative stress markers in the brain of patients with cirrhosis and hepatic encephalopathy. Hepatology 52, 256–265 (2010).
Vallance, P. & Moncada, S. Hyperdynamic circulation in cirrhosis: a role for nitric oxide? Lancet 337, 776–778 (1991).
Cahill, P. A., Redmond, E. M., Hodges, R., Zhang, S. & Sitzmann, J. V. Increased endothelial nitric oxide synthase activity in the hyperemic vessels of portal hypertensive rats. J. Hepatol. 25, 370–378 (1996).
Battista, S. et al. Hyperdynamic circulation in patients with cirrhosis: direct measurement of nitric oxide levels in hepatic and portal veins. J. Hepatol. 26, 75–80 (1997).
Bolognesi, M. et al. Haeme oxygenase mediates hyporeactivity to phenylephrine in the mesenteric vessels of cirrhotic rats with ascites. Gut 54, 1630–1636 (2005).
Morales-Ruiz, M. et al. Increased nitric oxide synthase expression in arterial vessels of cirrhotic rats with ascites. Hepatology 24, 1481–1486 (1996).
Angeli, P. et al. The role of nitric oxide in the pathogenesis of systemic and splanchnic vasodilation in cirrhotic rats before and after the onset of ascites. Liver Int. 25, 429–437 (2005).
Chen, Y. C. et al. Increased vascular heme oxygenase-1 expression contributes to arterial vasodilation in experimental cirrhosis in rats. Hepatology 39, 1075–1087 (2004).
Mookerjee, R. P. et al. Increasing dimethylarginine levels are associated with adverse clinical outcome in severe alcoholic hepatitis. Hepatology 45, 62–71 (2007).
Kasumov, T. et al. Plasma levels of asymmetric dimethylarginine in patients with biopsy-proven nonalcoholic fatty liver disease. Metabolism 60, 776–781 (2011).
Vizzutti, F. et al. ADMA correlates with portal pressure in patients with compensated cirrhosis. Eur. J. Clin. Invest. 37, 509–515 (2007).
Fiorucci, S. et al. The third gas: H2S regulates perfusion pressure in both the isolated and perfused normal rat liver and in cirrhosis. Hepatology 42, 539–548 (2005).
Norris, E. J., Larion, S., Culberson, C. R. & Clemens, M. G. Hydrogen sulfide differentially affects the hepatic vasculature in response to phenylephrine and endothelin 1 during endotoxemia. Shock 39, 168–175 (2013).
Fiorucci, S., Zampella, A., Cirino, G., Bucci, M. & Distrutti, E. Decoding the vasoregulatory activities of bile acid-activated receptors in systemic and portal circulation: role of gaseous mediators. Am. J. Physiol. Heart Circ. Physiol. 312, H21–H32 (2017).
Vairappan, B. Endothelial dysfunction in cirrhosis: role of inflammation and oxidative stress. World J. Hepatol. 7, 443–459 (2015).
Xie, G. et al. Role of differentiation of liver sinusoidal endothelial cells in progression and regression of hepatic fibrosis in rats. Gastroenterology 142, 918–927.e6 (2012).
Iwakiri, Y., Shah, V. & Rockey, D. C. Vascular pathobiology in chronic liver disease and cirrhosis – current status and future directions. J. Hepatol. 61, 912–924 (2014).
Poisson, J. et al. Liver sinusoidal endothelial cells: physiology and role in liver diseases. J. Hepatol. 66, 212–227 (2017).
Horn, T., Christoffersen, P. & Henriksen, J. H. Alcoholic liver injury: defenestration in noncirrhotic livers–a scanning electron microscopic study. Hepatology 7, 77–82 (1987).
DeLeve, L. D., Wang, X., Kanel, G. C., Atkinson, R. D. & McCuskey, R. S. Prevention of hepatic fibrosis in a murine model of metabolic syndrome with nonalcoholic steatohepatitis. Am. J. Pathol. 173, 993–1001 (2008).
Deleve, L. D., Wang, X. & Guo, Y. Sinusoidal endothelial cells prevent rat stellate cell activation and promote reversion to quiescence. Hepatology 48, 920–930 (2008).
Marrone, G., Shah, V. H. & Gracia-Sancho, J. Sinusoidal communication in liver fibrosis and regeneration. J. Hepatol. 65, 608–617 (2016).
Fernandez-Iglesias, A. & Gracia-Sancho, J. How to face chronic liver disease: the sinusoidal perspective. Front. Med. 4, 7 (2017).
Yokomori, H. et al. Vascular endothelial growth factor increases fenestral permeability in hepatic sinusoidal endothelial cells. Liver Int. 23, 467–475 (2003).
Funyu, J., Mochida, S., Inao, M., Matsui, A. & Fujiwara, K. VEGF can act as vascular permeability factor in the hepatic sinusoids through upregulation of porosity of endothelial cells. Biochem. Biophys. Res. Commun. 280, 481–485 (2001).
May, D. et al. A transgenic model for conditional induction and rescue of portal hypertension reveals a role of VEGF-mediated regulation of sinusoidal fenestrations. PLoS ONE 6, e21478 (2011).
Pacher, P., Batkai, S. & Kunos, G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol. Rev. 58, 389–462 (2006).
Batkai, S. et al. Endocannabinoids acting at CB1 receptors mediate the cardiac contractile dysfunction in vivo in cirrhotic rats. Am. J. Physiol. Heart Circ. Physiol. 293, H1689–H1695 (2007).
Hegde, V. L. et al. Attenuation of experimental autoimmune hepatitis by exogenous and endogenous cannabinoids: involvement of regulatory T cells. Mol. Pharmacol. 74, 20–33 (2008).
Osei-Hyiaman, D. et al. Endocannabinoid activation at hepatic CB1 receptors stimulates fatty acid synthesis and contributes to diet-induced obesity. J. Clin. Invest. 115, 1298–1305 (2005).
Mendez-Sanchez, N. et al. Endocannabinoid receptor CB2 in nonalcoholic fatty liver disease. Liver Int. 27, 215–219 (2007).
Varga, Z. V. et al. β-Caryophyllene protects against alcoholic steatohepatitis by attenuating inflammation and metabolic dysregulation in mice. Br. J. Pharmacol. 175, 320–334 (2018).
Rajesh, M. et al. Cannabinoid-2 receptor agonist HU-308 protects against hepatic ischemia/reperfusion injury by attenuating oxidative stress, inflammatory response, and apoptosis. J. Leukoc. Biol. 82, 1382–1389 (2007).
Batkai, S. et al. Cannabinoid-2 receptor mediates protection against hepatic ischemia/reperfusion injury. FASEB J. 21, 1788–1800 (2007).
Habib, A. et al. Inhibition of monoacylglycerol lipase, an anti-inflammatory and antifibrogenic strategy in the liver. Gut 68, 522–532 (2019).
Teixeira-Clerc, F. et al. CB1 cannabinoid receptor antagonism: a new strategy for the treatment of liver fibrosis. Nat. Med. 12, 671–676 (2006).
Munoz-Luque, J. et al. Regression of fibrosis after chronic stimulation of cannabinoid CB2 receptor in cirrhotic rats. J. Pharmacol. Exp. Ther. 324, 475–483 (2008).
Julien, B. et al. Antifibrogenic role of the cannabinoid receptor CB2 in the liver. Gastroenterology 128, 742–755 (2005).
Maccarrone, M. et al. Endocannabinoid signaling at the periphery: 50 years after THC. Trends Pharmacol. Sci. 36, 277–296 (2015).
Pacher, P., Steffens, S., Hasko, G., Schindler, T. H. & Kunos, G. Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat. Rev. Cardiol. 15, 151–166 (2018).
Pacher, P. & Mechoulam, R. Is lipid signaling through cannabinoid 2 receptors part of a protective system? Prog. Lipid Res. 50, 193–211 (2011).
Batkai, S. et al. Endocannabinoids acting at vascular CB1 receptors mediate the vasodilated state in advanced liver cirrhosis. Nat. Med. 7, 827–832 (2001).
Moezi, L. et al. Anandamide mediates hyperdynamic circulation in cirrhotic rats via CB(1) and VR(1) receptors. Br. J. Pharmacol. 149, 898–908 (2006).
Simoes, E. S. A. C., Miranda, A. S., Rocha, N. P. & Teixeira, A. L. Renin angiotensin system in liver diseases: friend or foe? World J. Gastroenterol. 23, 3396–3406 (2017).
Herath, C. B. et al. Upregulation of hepatic angiotensin-converting enzyme 2 (ACE2) and angiotensin-(1-7) levels in experimental biliary fibrosis. J. Hepatol. 47, 387–395 (2007).
Vilas-Boas, W. W. et al. Relationship between angiotensin-(1-7) and angiotensin II correlates with hemodynamic changes in human liver cirrhosis. World J. Gastroenterol. 15, 2512–2519 (2009).
Grace, J. A., Herath, C. B., Mak, K. Y., Burrell, L. M. & Angus, P. W. Update on new aspects of the renin-angiotensin system in liver disease: clinical implications and new therapeutic options. Clin. Sci. 123, 225–239 (2012).
Rockey, D. C. & Weisiger, R. A. Endothelin induced contractility of stellate cells from normal and cirrhotic rat liver: implications for regulation of portal pressure and resistance. Hepatology 24, 233–240 (1996).
Schneider, A. W., Kalk, J. F. & Klein, C. P. Effect of losartan, an angiotensin II receptor antagonist, on portal pressure in cirrhosis. Hepatology 29, 334–339 (1999).
Bataller, R. et al. Activated human hepatic stellate cells express the renin-angiotensin system and synthesize angiotensin II. Gastroenterology 125, 117–125 (2003).
Paizis, G. et al. Up-regulation of components of the renin-angiotensin system in the bile duct-ligated rat liver. Gastroenterology 123, 1667–1676 (2002).
Yoshiji, H. et al. Angiotensin-II type 1 receptor interaction is a major regulator for liver fibrosis development in rats. Hepatology 34, 745–750 (2001).
Ruiz-del-Arbol, L. et al. Circulatory function and hepatorenal syndrome in cirrhosis. Hepatology 42, 439–447 (2005).
Pereira, R. M. et al. The renin-angiotensin system in a rat model of hepatic fibrosis: evidence for a protective role of angiotensin-(1-7). J. Hepatol. 46, 674–681 (2007).
Bansal, S., Lindenfeld, J. & Schrier, R. W. Sodium retention in heart failure and cirrhosis: potential role of natriuretic doses of mineralocorticoid antagonist? Circ. Heart Fail. 2, 370–376 (2009).
Hartupee, J. & Mann, D. L. Neurohormonal activation in heart failure with reduced ejection fraction. Nat. Rev. Cardiol. 14, 30–38 (2017).
Chayanupatkul, M. & Liangpunsakul, S. Cirrhotic cardiomyopathy: review of pathophysiology and treatment. Hepatol. Int. 8, 308–315 (2014).
Moller, S., Henriksen, J. H. & Bendtsen, F. Pathogenetic background for treatment of ascites and hepatorenal syndrome. Hepatol. Int. 2, 416–428 (2008).
Zablocki, D. & Sadoshima, J. Angiotensin II and oxidative stress in the failing heart. Antioxid. Redox Signal. 19, 1095–1109 (2013).
Yanagisawa, M. et al. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332, 411–415 (1988).
Moller, S., Emmeluth, C. & Henriksen, J. H. Elevated circulating plasma endothelin-1 concentrations in cirrhosis. J. Hepatol. 19, 285–290 (1993).
Pinzani, M. et al. Endothelin 1 is overexpressed in human cirrhotic liver and exerts multiple effects on activated hepatic stellate cells. Gastroenterology 110, 534–548 (1996).
Moore, K. et al. Plasma endothelin immunoreactivity in liver disease and the hepatorenal syndrome. N. Engl. J. Med. 327, 1774–1778 (1992).
Chuang, C. L. et al. Endotoxemia-enhanced renal vascular reactivity to endothelin-1 in cirrhotic rats. Am. J. Physiol. Gastrointest. Liver Physiol. 315, G752–G761 (2018).
Chuang, C. L. et al. Lipopolysaccharide enhanced renal vascular response to endothelin-1 through ETA overexpression in portal hypertensive rats. J. Gastroenterol. Hepatol. 30, 199–207 (2015).
Fritz, J. S., Fallon, M. B. & Kawut, S. M. Pulmonary vascular complications of liver disease. Am. J. Respir. Crit. Care Med. 187, 133–143 (2013).
Correale, M. et al. Endothelin-receptor antagonists in the management of pulmonary arterial hypertension: where do we stand? Vasc. Health Risk Manag. 14, 253–264 (2018).
Du, Q. H. et al. Increased endothelin receptor B and G protein coupled kinase-2 in the mesentery of portal hypertensive rats. World J. Gastroenterol. 19, 2065–2072 (2013).
Hathaway, C. K. et al. Endothelin-1 critically influences cardiac function via superoxide-MMP9 cascade. Proc. Natl Acad. Sci. USA 112, 5141–5146 (2015).
Iglarz, M. & Clozel, M. Mechanisms of ET-1-induced endothelial dysfunction. J. Cardiovasc. Pharmacol. 50, 621–628 (2007).
Zhan, S., Chan, C. C., Serdar, B. & Rockey, D. C. Fibronectin stimulates endothelin-1 synthesis in rat hepatic myofibroblasts via a Src/ERK-regulated signaling pathway. Gastroenterology 136, 2345–2355.e1-e4 (2009).
Zhan, S. & Rockey, D. C. Tumor necrosis factor α stimulates endothelin-1 synthesis in rat hepatic stellate cells in hepatic wound healing through a novel IKK/JNK pathway. Exp. Cell Res. 317, 1040–1048 (2011).
Liu, C. Q. et al. Thromboxane prostanoid receptor activation impairs endothelial nitric oxide-dependent vasorelaxations: the role of rho kinase. Biochem. Pharmacol. 78, 374–381 (2009).
Rosado, E. et al. Interaction between NO and COX pathways modulating hepatic endothelial cells from control and cirrhotic rats. J. Cell Mol. Med. 16, 2461–2470 (2012).
Graupera, M. et al. Sinusoidal endothelial COX-1-derived prostanoids modulate the hepatic vascular tone of cirrhotic rat livers. Am. J. Physiol. Gastrointest. Liver Physiol. 288, G763–G770 (2005).
Iwakiri, Y. & Groszmann, R. J. Vascular endothelial dysfunction in cirrhosis. J. Hepatol. 46, 927–934 (2007).
Graupera, M. et al. Cyclooxygenase-derived products modulate the increased intrahepatic resistance of cirrhotic rat livers. Hepatology 37, 172–181 (2003).
Laffi, G., La Villa, G., Pinzani, M., Marra, F. & Gentilini, P. Arachidonic acid derivatives and renal function in liver cirrhosis. Semin. Nephrol. 17, 530–548 (1997).
Rimola, A. et al. Urinary excretion of 6-keto-prostaglandin F1α, thromboxane B2 and prostaglandin E2 in cirrhosis with ascites. Relationship to functional renal failure (hepatorenal syndrome). J. Hepatol. 3, 111–117 (1986).
Hou, M. C. et al. Enhanced cyclooxygenase-1 expression within the superior mesenteric artery of portal hypertensive rats: role in the hyperdynamic circulation. Hepatology 27, 20–27 (1998).
Nascimento, M. et al. Hepatic injury induced by thioacetamide causes aortic endothelial dysfunction by a cyclooxygenase-dependent mechanism. Life Sci. 212, 168–175 (2018).
Lacout, A. et al. Roles of cyclooxygenase 2 and hepatic venous flow in patients with HHT or hepatopulmonary syndrome. Med. Hypotheses 83, 302–305 (2014).
Tang, X. et al. Cyclooxygenase-2 regulates HPS patient serum induced-directional collective HPMVEC migration via PKC/Rac signaling pathway. Gene 692, 176–184 (2019).
Chang, C. C. et al. Selective cyclooxygenase inhibition by SC-560 improves hepatopulmonary syndrome in cirrhotic rats. PLoS ONE 12, e0179809 (2017).
Awdish, R. L. & Cajigas, H. R. Early initiation of prostacyclin in portopulmonary hypertension: 10 years of a transplant center’s experience. Lung 191, 593–600 (2013).
Oliver, M. I. et al. Autonomic dysfunction in patients with non-alcoholic chronic liver disease. J. Hepatol. 26, 1242–1248 (1997).
Perez-Pena, J. et al. Autonomic neuropathy in end-stage cirrhotic patients and evolution after liver transplantation. Transpl. Proc. 35, 1834–1835 (2003).
Milovanovic, B. et al. Autonomic dysfunction in alcoholic cirrhosis and its relation to sudden cardiac death risk predictors. Gen. Physiol. Biophys. 28, 251–261 (2009).
Yokoyama, A. et al. Prolonged QT interval in alcoholic autonomic nervous dysfunction. Alcohol. Clin. Exp. Res. 16, 1090–1092 (1992).
Henriksen, J. H., Moller, S., Ring-Larsen, H. & Christensen, N. J. The sympathetic nervous system in liver disease. J. Hepatol. 29, 328–341 (1998).
Iga, A., Nomura, M., Sawada, Y., Ito, S. & Nakaya, Y. Autonomic nervous dysfunction in patients with liver cirrhosis using 123I-metaiodobenzylguanidine myocardial scintigraphy and spectrum analysis of heart-rate variability. J. Gastroenterol. Hepatol. 18, 651–659 (2003).
Dillon, J. F. et al. The correction of autonomic dysfunction in cirrhosis by captopril. J. Hepatol. 26, 331–335 (1997).
Hendrickse, M. T. & Triger, D. R. Vagal dysfunction and impaired urinary sodium and water excretion in cirrhosis. Am. J. Gastroenterol. 89, 750–757 (1994).
Moller, S. & Henriksen, J. H. Review article: pathogenesis and pathophysiology of hepatorenal syndrome–is there scope for prevention? Aliment. Pharmacol. Ther. 20, 31–41 (2004).
Gerbes, A. L., Remien, J., Jungst, D., Sauerbruch, T. & Paumgartner, G. Evidence for down-regulation of beta-2-adrenoceptors in cirrhotic patients with severe ascites. Lancet 1, 1409–1411 (1986).
Lee, S. S. et al. Desensitization of myocardial β-adrenergic receptors in cirrhotic rats. Hepatology 12, 481–485 (1990).
Ceolotto, G. et al. An abnormal gene expression of the β-adrenergic system contributes to the pathogenesis of cardiomyopathy in cirrhotic rats. Hepatology 48, 1913–1923 (2008).
Di Stefano, C., Milazzo, V., Milan, A., Veglio, F. & Maule, S. The role of autonomic dysfunction in cirrhotic patients before and after liver transplantation. Review of the literature. Liver Int. 36, 1081–1089 (2016).
Jaue, D. N., Ma, Z. & Lee, S. S. Cardiac muscarinic receptor function in rats with cirrhotic cardiomyopathy. Hepatology 25, 1361–1365 (1997).
Moller, S. & Henriksen, J. H. Cirrhotic cardiomyopathy. J. Hepatol. 53, 179–190 (2010).
Alvarado Tapias, E. et al. Short-term hemodynamic effects of β-blockers influence survival of patients with decompensated cirrhosis. J. Hepatol. https://doi.org/10.1016/j.jhep.2020.03.048 (2020).
Provencher, S. et al. Deleterious effects of β-blockers on exercise capacity and hemodynamics in patients with portopulmonary hypertension. Gastroenterology 130, 120–126 (2006).
Brito-Azevedo, A. et al. Propranolol improves endothelial dysfunction in advanced cirrhosis: the ‘endothelial exhaustion’ hypothesis. Gut 65, 1391–1392 (2016).
Leithead, J. A. et al. Non-selective β-blockers are associated with improved survival in patients with ascites listed for liver transplantation. Gut 64, 1111–1119 (2015).
Morsiani, C. et al. The peculiar aging of human liver: a geroscience perspective within transplant context. Ageing Res. Rev. 51, 24–34 (2019).
Yusuf, S., Reddy, S., Ounpuu, S. & Anand, S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 104, 2746–2753 (2001).
Papatheodoridi, A. M., Chrysavgis, L., Koutsilieris, M. & Chatzigeorgiou, A. The role of senescence in the development of nonalcoholic fatty liver disease and progression to nonalcoholic steatohepatitis. Hepatology 71, 363–374 (2020).
Ramirez, T. et al. Aging aggravates alcoholic liver injury and fibrosis in mice by downregulating sirtuin 1 expression. J. Hepatol. 66, 601–609 (2017).
Sheedfar, F., Di Biase, S., Koonen, D. & Vinciguerra, M. Liver diseases and aging: friends or foes? Aging Cell 12, 950–954 (2013).
Lenti, M. V. et al. Mortality rate and risk factors for gastrointestinal bleeding in elderly patients. Eur. J. Intern. Med. 61, 54–61 (2019).
Heidemann, J., Bartels, C., Berssenbrugge, C., Schmidt, H. & Meister, T. Hepatorenal syndrome: outcome of response to therapy and predictors of survival. Gastroenterol. Res. Pract. 2015, 457613 (2015).
Raevens, S. et al. Prevalence and outcome of diastolic dysfunction in liver transplantation recipients. Acta Cardiol. 69, 273–280 (2014).
Wolff, J. L., Starfield, B. & Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 162, 2269–2276 (2002).
Anstee, Q. M., Mantovani, A., Tilg, H. & Targher, G. Risk of cardiomyopathy and cardiac arrhythmias in patients with nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 15, 425–439 (2018).
Mantovani, A. et al. Nonalcoholic fatty liver disease is associated with ventricular arrhythmias in patients with type 2 diabetes referred for clinically indicated 24-hour Holter monitoring. Diabetes Care 39, 1416–1423 (2016).
Ling, L. H., Kistler, P. M., Kalman, J. M., Schilling, R. J. & Hunter, R. J. Comorbidity of atrial fibrillation and heart failure. Nat. Rev. Cardiol. 13, 131–147 (2016).
Watt, K. D., Pedersen, R. A., Kremers, W. K., Heimbach, J. K. & Charlton, M. R. Evolution of causes and risk factors for mortality post-liver transplant: results of the NIDDK long-term follow-up study. Am. J. Transpl. 10, 1420–1427 (2010).
Ruggieri, A., Gagliardi, M. C. & Anticoli, S. Sex-dependent outcome of hepatitis B and C viruses infections: synergy of sex hormones and immune responses? Front. Immunol. 9, 2302 (2018).
Zhang, B. & Wu, Z. Y. Estrogen derivatives: novel therapeutic agents for liver cirrhosis and portal hypertension. Eur. J. Gastroenterol. Hepatol. 25, 263–270 (2013).
Shimizu, I. Impact of oestrogens on the progression of liver disease. Liver Int. 23, 63–69 (2003).
Lu, G. et al. Antioxidant and antiapoptotic activities of idoxifene and estradiol in hepatic fibrosis in rats. Life Sci. 74, 897–907 (2004).
Lu, P. et al. Gender differences in hepatic ischemic reperfusion injury in rats are associated with endothelial cell nitric oxide synthase-derived nitric oxide. World J. Gastroenterol. 11, 3441–3445 (2005).
Sakamoto, M. et al. Estrogen upregulates nitric oxide synthase expression in cultured rat hepatic sinusoidal endothelial cells. J. Hepatol. 34, 858–864 (2001).
Stanhewicz, A. E., Wenner, M. M. & Stachenfeld, N. S. Sex differences in endothelial function important to vascular health and overall cardiovascular disease risk across the lifespan. Am. J. Physiol. Heart Circ. Physiol. 315, H1569–H1588 (2018).
Engelmann, C. et al. Loss of paraspinal muscle mass is a gender-specific consequence of cirrhosis that predicts complications and death. Aliment. Pharmacol. Ther. 48, 1271–1281 (2018).
Kim, S. M. et al. QT prolongation is associated with increased mortality in end stage liver disease. World J. Cardiol. 9, 347–354 (2017).
Kawut, S. M. et al. Clinical risk factors for portopulmonary hypertension. Hepatology 48, 196–203 (2008).
Rao, R. Endotoxemia and gut barrier dysfunction in alcoholic liver disease. Hepatology 50, 638–644 (2009).
Miele, L. et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology 49, 1877–1887 (2009).
Bigatello, L. M. et al. Endotoxemia, encephalopathy, and mortality in cirrhotic patients. Am. J. Gastroenterol. 82, 11–15 (1987).
Lin, R. S. et al. Endotoxemia in patients with chronic liver diseases: relationship to severity of liver diseases, presence of esophageal varices, and hyperdynamic circulation. J. Hepatol. 22, 165–172 (1995).
Fouts, D. E., Torralba, M., Nelson, K. E., Brenner, D. A. & Schnabl, B. Bacterial translocation and changes in the intestinal microbiome in mouse models of liver disease. J. Hepatol. 56, 1283–1292 (2012).
Seki, E. et al. TLR4 enhances TGF-β signaling and hepatic fibrosis. Nat. Med. 13, 1324–1332 (2007).
Bernardi, M. et al. Q-T interval prolongation in cirrhosis: prevalence, relationship with severity, and etiology of the disease and possible pathogenetic factors. Hepatology 27, 28–34 (1998).
Xiang, X. et al. Interleukin-22 ameliorates acute-on-chronic liver failure by reprogramming of impaired regeneration pathways in mice. J. Hepatol. 72, 736–745 (2020).
Swanson, K. L., Wiesner, R. H. & Krowka, M. J. Natural history of hepatopulmonary syndrome: impact of liver transplantation. Hepatology 41, 1122–1129 (2005).
Krowka, M. J., Wiseman, G. A., Steers, J. L. & Wiesner, R. H. Late recurrence and rapid evolution of severe hepatopulmonary syndrome after liver transplantation. Liver Transpl. Surg. 5, 451–453 (1999).
Casey, S., Schelleman, A. & Angus, P. Recurrence of hepatopulmonary syndrome post-orthotopic liver transplantation in a patient with noncirrhotic portal hypertension. Hepatology 58, 2205–2206 (2013).
Krowka, M. J. et al. Pulmonary hemodynamics and perioperative cardiopulmonary-related mortality in patients with portopulmonary hypertension undergoing liver transplantation. Liver Transpl. 6, 443–450 (2000).
Izzy, M., Oh, J. & Watt, K. D. Cirrhotic cardiomyopathy after transplantation: neither the transient nor innocent bystander. Hepatology 68, 2008–2015 (2018).
Mittal, C., Qureshi, W., Singla, S., Ahmad, U. & Huang, M. A. Pre-transplant left ventricular diastolic dysfunction is associated with post transplant acute graft rejection and graft failure. Dig. Dis. Sci. 59, 674–680 (2014).
Bargehr, J. et al. Preexisting atrial fibrillation and cardiac complications after liver transplantation. Liver Transpl. 21, 314–320 (2015).
Zardi, E. M. et al. Cirrhotic cardiomyopathy in the pre- and post-liver transplantation phase. J. Cardiol. 67, 125–130 (2016).
Wong, F., Leung, W., Al Beshir, M., Marquez, M. & Renner, E. L. Outcomes of patients with cirrhosis and hepatorenal syndrome type 1 treated with liver transplantation. Liver Transpl. 21, 300–307 (2015).
Carrier, P., Debette-Gratien, M., Jacques, J. & Loustaud-Ratti, V. Cirrhotic patients and older people. World J. Hepatol. 11, 663–677 (2019).
Sharpton, S. R., Feng, S., Hameed, B., Yao, F. & Lai, J. C. Combined effects of recipient age and model for end-stage liver disease score on liver transplantation outcomes. Transplantation 98, 557–562 (2014).
Wong, V. W., Adams, L. A., de Ledinghen, V., Wong, G. L. & Sookoian, S. Noninvasive biomarkers in NAFLD and NASH – current progress and future promise. Nat. Rev. Gastroenterol. Hepatol. 15, 461–478 (2018).
Acknowledgements
P.P. receives support from the Intramural Research Program of NIAAA/NIH (1ZIAAA000375-13).
Author information
Authors and Affiliations
Contributions
C.M., L.L. and P.P. researched data for the article. All authors discussed the content of the manuscript. C.M., L.L., E.T. and P.P. wrote the article, and all authors reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Additional information
Peer review information
Nature Reviews Cardiology thanks F. Triposkiadis, M. Klapholz and M. Bernardi for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Nonalcoholic fatty liver disease
-
Excessive accumulation of fat in the liver that is not related to alcohol consumption.
- Nonalcoholic steatohepatitis
-
A subtype of nonalcoholic fatty liver disease characterized by liver inflammation and liver cell damage.
- Alcoholic liver disease
-
Liver damage caused by alcohol consumption.
- Transjugular intrahepatic portosystemic shunt
-
An artificial passage connecting the portal and hepatic veins.
- Acute-on-chronic liver failure
-
A syndrome affecting patients with chronic liver disease that is characterized by systemic inflammation, organ failure and poor prognosis.
Rights and permissions
About this article
Cite this article
Matyas, C., Haskó, G., Liaudet, L. et al. Interplay of cardiovascular mediators, oxidative stress and inflammation in liver disease and its complications. Nat Rev Cardiol 18, 117–135 (2021). https://doi.org/10.1038/s41569-020-0433-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-020-0433-5
This article is cited by
-
The regional disparities in liver disease comorbidity among elderly Chinese based on a health ecological model: the China Health and Retirement Longitudinal Study
BMC Public Health (2024)
-
Sulforaphane prevents LPS-induced inflammation by regulating the Nrf2-mediated autophagy pathway in goat mammary epithelial cells and a mouse model of mastitis
Journal of Animal Science and Biotechnology (2023)
-
PCSK9: an emerging player in cardiometabolic aging and its potential as a therapeutic target and biomarker
GeroScience (2023)
-
Data-driven transcriptomics analysis identifies PCSK9 as a novel key regulator in liver aging
GeroScience (2023)
-
Revealing potential anti-fibrotic mechanism of Ganxianfang formula based on RNA sequence
Chinese Medicine (2022)