Abstract
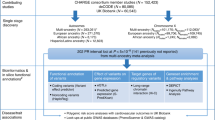
The primary electrical disorders are a group of inherited cardiac ventricular arrhythmias that are a major cause of sudden cardiac death in young individuals. Inherited ventricular arrhythmias result from mutations in genes encoding cardiac ion channels or their modulatory subunits. Advances in genetic screening in the past three decades have led to the assembly of large patient cohorts with these disorders. Studies in these patients, as well as in the general population, have striven to define the prevalence of these inherited arrhythmias and the characteristics of patients with different genetic subtypes of the disease. In this Review, we provide a comprehensive update on the epidemiology of inherited ventricular arrhythmias, focusing on natural history, prevalence and patient demographics. In addition, we summarize the various founder populations (groups of individuals with a disease that is caused by a genetic defect inherited from a common ancestor) that have been identified for some of these disorders and which lead to increased prevalence in some geographical regions. To date, although numerous studies have markedly increased our understanding of the epidemiology of these disorders, demographic data, especially from non-Western countries, remain scarce. Furthermore, defining the true prevalence of these disorders remains challenging. International collaboration will undoubtedly accelerate the collection of demographic information and improve the accuracy of prevalence data.
Key points
The primary electrical disorders, which are a common cause of sudden cardiac death in young individuals, result from mutations in genes encoding ion channels or their regulatory proteins.
Genetic testing has become an integral part of the management of patients with these disorders, although debate is ongoing about the causality of some genes that have been implicated in these disorders by candidate-gene studies.
Multiple, large cohorts of patients have facilitated studies on the natural history of these disorders and on proarrhythmic risk factors, although very few proarrhythmic risk factors have been described for short QT syndrome, idiopathic ventricular fibrillation and early repolarization syndrome.
The prevalence of these primary electrical disorders is hard to establish, given their rarity; the prevalence of long QT syndrome has been established through prospective studies whereas, for the other diseases, prevalence is based on electrocardiogram features or is merely an estimation.
In geographical regions with founder populations, the prevalence of the primary electrical disorders is likely to be much higher than currently assumed.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bagnall, R. D. et al. A prospective study of sudden cardiac death among children and young adults. N. Engl. J. Med. 374, 2441–2452 (2016).
Wang, Q. et al. Cardiac sodium channel mutations in patients with long QT syndrome, an inherited cardiac arrhythmia. Hum. Mol. Genet. 4, 1603–1607 (1995).
Curran, M. E. et al. A molecular basis for cardiac arrhythmia: HERG mutations cause long QT syndrome. Cell 80, 795–803 (1995).
Ackerman, M. J. et al. HRS/EHRA Expert Consensus Statement on the state of genetic testing for the channelopathies and cardiomyopathies. Heart Rhythm 8, 1308–1339 (2011).
Hofman, N. et al. Yield of molecular and clinical testing for arrhythmia syndromes. Circulation 128, 1513–1521 (2013).
Bezzina, C. R., Lahrouchi, N. & Priori, S. G. Genetics of sudden cardiac death. Circ. Res. 116, 1919–1936 (2015).
Tester, D. J., Will, M. L., Haglund, C. M. & Ackerman, M. J. Effect of clinical phenotype on yield of long QT syndrome genetic testing. J. Am. Coll. Cardiol. 47, 764–768 (2006).
Splawski, I. et al. Spectrum of mutations in long-QT syndrome genes: KVLQT1, HERG, SCN5A, KCNE1, and KCNE2. Circulation 102, 1178–1185 (2000).
Napolitano, C. et al. Genetic testing in the long QT syndrome. JAMA 294, 2975 (2005).
Giudicessi, J. R., Wilde, A. A. M. & Ackerman, M. J. The genetic architecture of long QT syndrome: a critical reappraisal. Trends Cardiovasc. Med. 28, 453–464 (2018).
Rohatgi, R. K. et al. Contemporary outcomes in patients with long QT syndrome. J. Am. Coll. Cardiol. 70, 453–462 (2017).
Schwartz, P. J. et al. Genotype-phenotype correlation in the long-QT syndrome: gene-specific triggers for life-threatening arrhythmias. Circulation 103, 89–95 (2001).
Wilde, A. A. M. et al. Auditory stimuli as a trigger for arrhythmic events differentiate HERG-related (LQTS2) patients from KVLQT1-related patients (LQTS1). J. Am. Coll. Cardiol. 33, 327–332 (1999).
Priori, S. G. et al. Risk stratification in the long-QT syndrome. N. Engl. J. Med. 348, 1866–1874 (2003).
Priori, S. G. et al. Association of long QT syndrome loci and cardiac events among patients treated with beta-blockers. JAMA 292, 1341–1344 (2004).
Wilde, A. A. M. et al. Clinical aspects of type 3 long-QT syndrome: an international multicenter study. Circulation 134, 872–882 (2016).
Zareba, W. et al. Influence of the genotype on the clinical course of the long-QT syndrome. N. Engl. J. Med. 339, 960–965 (1998).
Moss, A. J. et al. Clinical aspects of type-1 long-QT syndrome by location, coding type, and biophysical function of mutations involving the KCNQ1 gene. Circulation 115, 2481–2489 (2007).
Shimizu, W. et al. Genotype-phenotype aspects of type 2 long QT syndrome. J. Am. Coll. Cardiol. 54, 2052–2062 (2009).
Schwartz, P. J., Crotti, L. & George, A. L. Modifier genes for sudden cardiac death. Eur. Heart J. 39, 3925–3931 (2018).
Schwartz, P. J. et al. The Jervell and Lange-Nielsen syndrome: natural history, molecular basis, and clinical outcome. Circulation 113, 783–790 (2006).
Splawski, I. et al. CaV1.2 calcium channel dysfunction causes a multisystem disorder including arrhythmia and autism. Cell 119, 19–31 (2004).
Moss, A. J., Schwartz, P. J., Crampton, R. S., Locati, E. & Carleen, E. The long QT syndrome: a prospective international study. Circulation 71, 17–21 (1985).
Vincent, G. M. et al. High efficacy of β-blockers in long-QT syndrome type 1: contribution of noncompliance and QT-prolonging drugs to the occurrence of β-blocker treatment ‘failures’. Circulation 119, 215–221 (2009).
Hobbs, J. B. et al. Risk of aborted cardiac arrest or sudden cardiac death during adolescence in the long-QT syndrome. J. Am. Med. Assoc. 296, 1249–1254 (2006).
Mazzanti, A. et al. Interplay between genetic substrate, QTc duration, and arrhythmia risk in patients with long QT syndrome. J. Am. Coll. Cardiol. 71, 1663–1671 (2018).
Sauer, A. J. et al. Long QT syndrome in adults. J. Am. Coll. Cardiol. 49, 329–337 (2007).
Schwartz, P. J. et al. Prevalence of the congenital long-QT syndrome. Circulation 120, 1761–1767 (2009).
Yoshinaga, M. et al. Electrocardiographic screening of 1-month-old infants for identifying prolonged QT intervals. Circ. Arrhythm. Electrophysiol. 6, 932–938 (2013).
Hayashi, K. et al. Long QT syndrome and associated gene mutation carriers in Japanese children: results from ECG screening examinations. Clin. Sci. 117, 415–424 (2009).
Yoshinaga, M., Kucho, Y., Nishibatake, M., Ogata, H. & Nomura, Y. Probability of diagnosing long QT syndrome in children and adolescents according to the criteria of the HRS/EHRA/APHRS expert consensus statement. Eur. Heart J. 37, 2490–2497 (2016).
Vink, A. S. et al. Determination and interpretation of the QT interval. Circulation 138, 2345–2358 (2018).
Goldenberg, I. et al. Risk for life-threatening cardiac events in patients with genotype-confirmed long-QT syndrome and normal-range corrected QT intervals. J. Am. Coll. Cardiol. 57, 51–59 (2010).
Vink, A. S., Clur, S.-A. B., Wilde, A. A. M. & Blom, N. A. Effect of age and gender on the QTc-interval in healthy individuals and patients with long-QT syndrome. Trends Cardiovasc. Med. 28, 64–75 (2018).
Lehmann, M. H. et al. Age-gender influence on the rate-corrected QT interval and the QT-heart rate relation in families with genotypically characterized long QT syndrome. J. Am. Coll. Cardiol. 29, 93–99 (2017).
Ozawa, J. et al. Pediatric cohort with long QT syndrome — KCNH2 mutation carriers present late onset but severe symptoms. Circ. J. 80, 696–702 (2016).
Zareba, W. et al. Modulating effects of age and gender on the clinical course of long QT syndrome by genotype. J. Am. Coll. Cardiol. 42, 103–109 (2003).
Vink, A. S. et al. Effect of age and sex on the QTc interval in children and adolescents with type 1 and 2 long-QT syndrome. Circ. Arrhythm. Electrophysiol. 10, e004645 (2017).
Moss, A. J. et al. The long QT syndrome. Prospective longitudinal study of 328 families. Circulation 84, 1136–1144 (1991).
Garson, A. et al. The long QT syndrome in children: an international study of 287 patients. Circulation 87, 1866–1872 (1993).
Goldenberg, I. et al. Risk factors for aborted cardiac arrest and sudden cardiac death in children with the congenital long-QT syndrome. Circulation 117, 2184–2191 (2008).
Sedlak, T., Shufelt, C., Iribarren, C. & Merz, C. N. B. Sex hormones and the QT interval: a review. J. Womens Health 21, 933–941 (2012).
Brink, P. A. & Schwartz, P. J. Of founder populations, long QT syndrome, and destiny. Heart Rhythm 6, S25–S33 (2009).
Postema, P. G. et al. Founder mutations in the Netherlands: SCN5a 1795insD, the first described arrhythmia overlap syndrome and one of the largest and best characterised families worldwide. Neth. Heart J. 17, 422–428 (2009).
ter Bekke, R. M. A. et al. Heritability in a SCN5A-mutation founder population with increased female susceptibility to non-nocturnal ventricular tachyarrhythmia and sudden cardiac death. Heart Rhythm 14, 1873–1881 (2017).
Piippo, K. et al. A founder mutation of the potassium channel KCNQ1 in long QT syndrome. J. Am. Coll. Cardiol. 37, 562–568 (2001).
Fodstad, H. et al. Four potassium channel mutations underlying long-QT syndrome (LQTS) and provide evidence for a strong founder effect in Finland. Ann. Med. 36, 53–63 (2004).
Marjamaa, A. et al. High prevalence of four long QT syndrome founder mutations in the Finnish population. Ann. Med. 41, 234–240 (2009).
Winbo, A. et al. Origin of the Swedish long QT syndrome Y111C/KCNQ1 founder mutation. Heart Rhythm 8, 541–547 (2011).
Arbour, L. et al. A KCNQ1 V205M missense mutation causes a high rate of long QT syndrome in a First Nations community of northern British Columbia: a community-based approach to understanding the impact. Genet. Med. 10, 545–550 (2008).
Brink, P. A. et al. Phenotypic variability and unusual clinical severity of congenital long-QT syndrome in a founder population. Circulation 112, 2602–2610 (2005).
Takahashi, K. et al. High prevalence of the SCN5A E1784K mutation in school children with long QT syndrome living on the Okinawa islands. Circ. J. 78, 1974–1979 (2014).
Crotti, L. et al. NOS1AP Iis a genetic modifier of the long-QT syndrome. Circulation 120, 1657–1663 (2009).
Winbo, A. et al. Sex is a moderator of the association between NOS1AP sequence variants and QTc in two long QT syndrome founder populations: a pedigree-based measured genotype association analysis. BMC Med. Genet. 18, 74 (2017).
Lahtinen, A. M., Marjamaa, A., Swan, H. & Kontula, K. KCNE1D85N polymorphism — a sex-specific modifier in type 1 long QT syndrome? BMC Med. Genet. 12, 11 (2011).
Antzelevitch, C. et al. J-wave syndromes expert consensus conference report: emerging concepts and gaps in knowledge. Europace 19, 665–694 (2016).
Clinical Genome Resource. Explore the clinical relevance of genes & variants. ClinGen https://clinicalgenome.org/ (2015).
Hosseini, S. M. et al. Reappraisal of reported genes for sudden arrhythmic death. Circulation 138, 1195–1205 (2018).
Schulze-Bahr, E. et al. Sodium channel gene (SCN5A) mutations in 44 index patients with Brugada syndrome: different incidences in familial and sporadic disease. Hum. Mutat. 21, 651–652 (2003).
Priori, S. G. et al. Clinical and genetic heterogeneity of right bundle branch block and ST-segment elevation syndrome: a prospective evaluation of 52 families. Circulation 102, 2509–2515 (2000).
Probst, V. et al. SCN5A mutations and the role of genetic background in the pathophysiology of Brugada syndrome. Circ. Cardiovasc. Genet. 2, 552–557 (2009).
Bezzina, C. R. et al. Common variants at SCN5A-SCN10A and HEY2 are associated with Brugada syndrome, a rare disease with high risk of sudden cardiac death. Nat. Genet. 45, 1044–1049 (2013).
Rodríguez-Mañero, M. et al. Monomorphic ventricular tachycardia in patients with Brugada syndrome: a multicenter retrospective study. Heart Rhythm 13, 669–682 (2016).
Matsuo, K. et al. The circadian pattern of the development of ventricular fibrillation in patients with Brugada syndrome. Eur. Heart J. 20, 465–470 (1999).
Michowitz, Y. et al. Fever-related arrhythmic events in the multicenter survey on arrhythmic events in Brugada syndrome. Heart Rhythm 15, 1394–1401 (2018).
Giustetto, C. et al. Atrial fibrillation in a large population with Brugada electrocardiographic pattern: prevalence, management, and correlation with prognosis. Heart Rhythm 11, 259–265 (2014).
Bordachar, P. et al. Incidence, clinical implications and prognosis of atrial arrhythmias in Brugada syndrome. Eur. Heart J. 25, 879–884 (2004).
Probst, V. et al. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the finger Brugada syndrome registry. Circulation 121, 635–643 (2010).
Sieira, J. et al. Asymptomatic Brugada syndrome: clinical characterization and long-term prognosis. Circ. Arrhythm. Electrophysiol. 8, 1144–1150 (2015).
Morita, H. et al. Fragmented QRS as a marker of conduction abnormality and a predictor of prognosis of Brugada syndrome. Circulation 118, 1697–1704 (2008).
Priori, S. G. et al. Risk stratification in Brugada syndrome: results of the PRELUDE (Programmed Electrical Stimulation Predictive Value) registry. J. Am. Coll. Cardiol. 59, 37–45 (2012).
Sieira, J. et al. Prognostic value of programmed electrical stimulation in Brugada syndrome. Circ. Arrhythm. Electrophysiol. 8, 777–784 (2015).
Yamagata, K. et al. Genotype-phenotype correlation of SCN5A mutation for the clinical and electrocardiographic characteristics of probands with Brugada syndrome: a Japanese multicenter registry. Circulation 135, 2255–2270 (2017).
Meregalli, P. G. et al. Type of SCN5A mutation determines clinical severity and degree of conduction slowing in loss-of-function sodium channelopathies. Heart Rhythm 6, 341–348 (2009).
Cordeiro, J. M. et al. Compound heterozygous mutations P336L and I1660V in the human cardiac sodium channel associated with the Brugada syndrome. Circulation 114, 2026–2033 (2006).
Postema, P. G. About Brugada syndrome and its prevalence. EP Eur. 14, 925–928 (2012).
Mizusawa, Y. & Wilde, A. A. M. Brugada syndrome. Circ. Arrhythm. Electrophysiol. 5, 606–616 (2012).
Andorin, A. et al. Impact of clinical and genetic findings on the management of young patients with Brugada syndrome. Heart Rhythm 13, 1274–1282 (2016).
Gonzalez Corcia, M. C. et al. Brugada syndrome in the young: an assessment of risk factors predicting future events. Europace 19, 1864–1873 (2017).
Eckardt, L. Gender differences in Brugada syndrome. J. Cardiovasc. Electrophysiol. 18, 422–424 (2007).
Milman, A. et al. Gender differences in patients with Brugada syndrome and arrhythmic events: data from a survey on arrhythmic events in 678 patients. Heart Rhythm 15, 1457–1465 (2018).
Benito, B. et al. Gender differences in clinical manifestations of Brugada syndrome. J. Am. Coll. Cardiol. 52, 1567–1573 (2008).
Shimizu, W. et al. Sex hormone and gender difference — role of testosterone on male predominance in Brugada syndrome. J. Cardiovasc. Electrophysiol. 18, 415–421 (2007).
Probst, V. et al. Clinical aspects and prognosis of Brugada syndrome in children. Circulation 115, 2042–2048 (2007).
Gehi, A. K., Duong, T. D., Metz, L. D., Gomes, J. A. & Mehta, D. Risk stratification of individuals with the Brugada electrocardiogram: a meta-analysis. J. Cardiovasc. Electrophysiol. 17, 577–583 (2006).
Bezzina, C. R. et al. Common sodium channel promoter haplotype in Asian subjects underlies variability in cardiac conduction. Circulation 113, 338–344 (2006).
Lieve, K. V. V., van der Werf, C. & Wilde, A. A. Catecholaminergic polymorphic ventricular tachycardia. Circ. J. 80, 1 (2016).
Priori, S. G. et al. Clinical and molecular characterization of patients with catecholaminergic polymorphic ventricular tachycardia. Circulation 106, 69–74 (2002).
Roston, T. M. et al. Catecholaminergic polymorphic ventricular tachycardia in children: analysis of therapeutic strategies and outcomes from an international multicenter registry. Circ. Arrhythm. Electrophysiol. 8, 633–642 (2015).
Van Der Werf, C., Zwinderman, A. H. & Wilde, A. A. M. Therapeutic approach for patients with catecholaminergic polymorphic ventricular tachycardia: state of the art and future developments. Europace 14, 175–183 (2012).
Leenhardt, A. et al. Catecholaminergic polymorphic ventricular tachycardia in children. Circulation 91, 1512–1519 (1995).
Priori, S. G. et al. Natural history of Brugada syndrome: insights for risk stratification and management. Circulation 105, 1342–1347 (2002).
Sy, R. W. et al. Arrhythmia characterization and long-term outcomes in catecholaminergic polymorphic ventricular tachycardia. Heart Rhythm 8, 864–871 (2011).
Sumitomo, N. et al. Clinical effectiveness of pulmonary vein isolation for arrhythmic events in a patient with catecholaminergic polymorphic ventricular tachycardia. Heart Vessel 25, 448–452 (2010).
Van Der Werf, C. et al. Familial evaluation in catecholaminergic polymorphic ventricular tachycardia disease penetrance and expression in cardiac ryanodine receptor mutation-carrying relatives. Circ. Arrhythm. Electrophysiol. 5, 748–756 (2012).
Priori, S. G. & Chen, S. R. W. Inherited dysfunction of sarcoplasmic reticulum Ca2+ handling and arrhythmogenesis. Circ. Res. 108, 871–883 (2011).
Hayashi, M. et al. Incidence and risk factors of arrhythmic events in catecholaminergic polymorphic ventricular tachycardia. Circulation 119, 2426–2434 (2009).
Ostby, S. A. et al. Competitive sports participation in patients with catecholaminergic polymorphic ventricular tachycardia: a single center’s early experience. JACC Clin. Electrophysiol. 2, 253–262 (2016).
Postma, A. V. et al. Absence of calsequestrin 2 causes severe forms of catecholaminergic polymorphic ventricular tachycardia. Circ. Res. 91, e21–e26 (2002).
Leenhardt, A., Denjoy, I. & Guicheney, P. Catecholaminergic polymorphic ventricular tachycardia. Circ. Arrhythm. Electrophysiol. 5, 1044–1052 (2012).
Priori, S. G. et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Heart Rhythm 10, 1932–1963 (2013).
Lahrouchi, N. et al. Utility of post-mortem genetic testing in cases of sudden arrhythmic death syndrome. J. Am. Coll. Cardiol. 69, 2134–2145 (2017).
Jiménez-Jáimez, J. et al. Diagnostic approach to unexplained cardiac arrest (from the FIVI-Gen Study). Am. J. Cardiol. 116, 894–899 (2015).
Tester, D. J., Medeiros-Domingo, A., Will, M. L., Haglund, C. M. & Ackerman, M. J. Cardiac channel molecular autopsy: insights from 173 consecutive cases of autopsy-negative sudden unexplained death referred for postmortem genetic testing. JMCP 87, 524–539 (2012).
Postma, A. V. et al. Catecholaminergic polymorphic ventricular tachycardia: RYR2 mutations, bradycardia, and follow up of the patients. J. Med. Genet. 42, 863–870 (2005).
Lahat, H. et al. A missense mutation in a highly conserved region of CASQ2 is associated with autosomal recessive catecholamine-induced polymorphic ventricular tachycardia in Bedouin families from Israel. Am. J. Hum. Genet. 69, 1378–1384 (2001).
Wangüemert, F. et al. Clinical and molecular characterization of a cardiac ryanodine receptor founder mutation causing catecholaminergic polymorphic ventricular tachycardia. Heart Rhythm 12, 1636–1643 (2015).
Bhuiyan, Z. A. et al. Expanding spectrum of human RYR2-related disease. Circulation 116, 1569–1576 (2007).
Campbell, M. J., Czosek, R. J., Hinton, R. B. & Miller, E. M. Exon 3 deletion of ryanodine receptor causes left ventricular noncompaction, worsening catecholaminergic polymorphic ventricular tachycardia, and sudden cardiac arrest. Am. J. Med. Genet. Part A 167, 2197–2200 (2015).
Dharmawan, T. et al. Identification of a novel exon3 deletion of RYR2 in a family with catecholaminergic polymorphic ventricular tachycardia. Ann. Noninvasive Electrocardiol. 24, e12623 (2019).
Ohno, S. et al. Exon 3 deletion of RYR2 encoding cardiac ryanodine receptor is associated with left ventricular non-compaction. Europace 16, 1646–1654 (2014).
Pölönen, R. P., Penttinen, K., Swan, H. & Aalto-Setälä, K. Antiarrhythmic effects of carvedilol and flecainide in cardiomyocytes derived from catecholaminergic polymorphic ventricular tachycardia patients. Stem Cells Int. 2018, 1–11 (2018).
Patel, C., Yan, G.-X. & Antzelevitch, C. Short QT syndrome: from bench to bedside. Circ. Arrhythm. Electrophysiol. 3, 401–408 (2010).
Thorsen, K. et al. Loss-of-activity-mutation in the cardiac chloride-bicarbonate exchanger AE3 causes short QT syndrome. Nat. Commun. 8, 1696 (2017).
Mazzanti, A. et al. Novel insight into the natural history of short QT syndrome. J. Am. Coll. Cardiol. 63, 1300–1308 (2014).
Giustetto, C. et al. Long-term follow-up of patients with short QT syndrome. J. Am. Coll. Cardiol. 58, 587–595 (2011).
Villafañe, J. et al. Long-term follow-up of a pediatric cohort with short QT syndrome. J. Am. Coll. Cardiol. 61, 1183–1191 (2013).
Campuzano, O. et al. Recent advances in short QT syndrome. Front. Cardiovasc. Med. 5, 1–7 (2018).
Mazzanti, A., Underwood, K., Nevelev, D., Kofman, S. & Priori, S. G. The new kids on the block of arrhythmogenic disorders: short QT syndrome and early repolarization. J. Cardiovasc. Electrophysiol. 28, 1226–1236 (2017).
Giustetto, C. et al. Short QT syndrome and arrhythmogenic cardiac diseases in the young: the challenge of implantable cardioverter-defibrillator therapy for children. Eur. Heart J. 27, 2440–2447 (2006).
Harrell, D. T. et al. Genotype-dependent differences in age of manifestation and arrhythmia complications in short QT syndrome. Int. J. Cardiol. 190, 393–402 (2015).
Priori, S. G. et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 36, 2793–2867 (2015).
Awamleh García, P. et al. Prevalence of electrocardiographic patterns associated with sudden cardiac death in the Spanish population aged 40 years or older. Results of the OFRECE study. Rev. Española Cardiol. 70, 801–807 (2017).
Anttonen, O. et al. Prevalence and prognostic significance of Short QT interval in a middle-aged Finnish population. Circulation 116, 714–720 (2007).
Mason, J. W. et al. Electrocardiographic reference ranges derived from 79,743 ambulatory subjects. J. Electrocardiol. 40, 228–234.e8 (2007).
Dhutia, H. et al. The prevalence and significance of a short QT interval in 18,825 low-risk individuals including athletes. Br. J. Sports Med. 50, 124–129 (2016).
Kobza, R. et al. Prevalence of long and short QT in a young population of 41,767 predominantly male Swiss conscripts. Heart Rhythm 6, 652–657 (2009).
Iribarren, C. et al. Short QT in a cohort of 1.7 million persons: prevalence, correlates, and prognosis. Ann. Noninvasive Electrocardiol. 19, 490–500 (2014).
Reinig, M. G. & Engel, T. R. The shortage of short QT intervals. Chest 132, 246–249 (2007).
Funada, A. et al. Assessment of QT intervals and prevalence of short QT syndrome in Japan. Clin. Cardiol. 31, 270–274 (2008).
Guerrier, K. et al. Short QT interval prevalence and clinical outcomes in a pediatric population. Circ. Arrhythm. Electrophysiol. 8, 1460–1464 (2015).
Visser, M. et al. Idiopathic ventricular fibrillation: the struggle for definition, diagnosis, and follow-up. Circ. Arrhythm. Electrophysiol. 9, e003817 (2016).
Haïssaguerre, M. et al. Mapping and ablation of idiopathic ventricular fibrillation. Circulation 106, 962–967 (2002).
Noda, T. et al. Malignant entity of idiopathic ventricular fibrillation and polymorphic ventricular tachycardia initiated by premature extrasystoles originating from the right ventricular outflow tract. J. Am. Coll. Cardiol. 46, 1288–1294 (2005).
Marsman, R. F. et al. A mutation in CALM1 encoding calmodulin in familial idiopathic ventricular fibrillation in childhood and adolescence. J. Am. Coll. Cardiol. 63, 259–266 (2014).
Alders, M. et al. Haplotype-sharing analysis implicates chromosome 7q36 harboring DPP6 in familial idiopathic ventricular fibrillation. Am. J. Hum. Genet. 84, 468–476 (2009).
Xiao, L. et al. Unique cardiac Purkinje fiber transient outward current β-subunit composition. Circ. Res. 112, 1310–1322 (2013).
Itoh, H. et al. A type 2 ryanodine receptor variant associated with reduced Ca2+ release and short-coupled torsades de pointes ventricular arrhythmia. Heart Rhythm 14, 98–107 (2016).
Huikuri, H. V., Castellanos, A. & Myerburg, R. J. Sudden death due to cardiac arrhythmias. N. Engl. J. Med. 345, 1473–1482 (2001).
Ozaydin, M. et al. Long-term outcome of patients with idiopathic ventricular fibrillation: a meta-analysis. J. Cardiovasc. Electrophysiol. 26, 1095–1104 (2015).
Haïssaguerre, M. et al. Role of Purkinje conducting system in triggering of idiopathic ventricular fibrillation. Lancet 359, 677–678 (2002).
Visser, M. et al. Long-term outcome of patients initially diagnosed with idiopathic ventricular fibrillation. Circ. Arrhythm. Electrophysiol. 9, e004258 (2016).
Waldmann, V. et al. Characteristics and clinical assessment of unexplained sudden cardiac arrest in the real-world setting: focus on idiopathic ventricular fibrillation. Eur. Heart J. 39, 1981–1987 (2018).
Herman, A. R. M. et al. Outcome of apparently unexplained cardiac arrest: results from investigation and follow-up of the prospective cardiac arrest survivors with preserved ejection fraction registry. Circ. Arrhythm. Electrophysiol. 9, e003619 (2016).
Sande, J. N. T. et al. Detailed characterization of familial idiopathic ventricular fibrillation linked to the DPP6 locus. Heart Rhythm 13, 905–912 (2016).
Macfarlane, P. W. et al. The early repolarization pattern. J. Am. Coll. Cardiol. 66, 470–477 (2015).
Gourraud, J.-B. et al. Identification of large families in early repolarization syndrome. J. Am. Coll. Cardiol. 61, 164–172 (2013).
Sinner, M. F. et al. A meta-analysis of genome-wide association studies of the electrocardiographic early repolarization pattern. Heart Rhythm 9, 1627–1634 (2012).
Haissaguerre, M. et al. Sudden cardiac arrest associated with early repolarization. N. Engl. J. Med. 358, 2016–2023 (2008).
Rosso, R. et al. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects. J. Am. Coll. Cardiol. 52, 1231–1238 (2008).
Tikkanen, J. T. et al. Long-term outcome associated with early repolarization on electrocardiography. N. Engl. J. Med. 361, 2529–2537 (2009).
Klatsky, A. L., Oehm, R., Cooper, R. A., Udaltsova, N. & Armstrong, M. A. The early repolarization normal variant electrocardiogram: correlates and consequences. Am. J. Med. 115, 171–177 (2003).
Wasserburger, R. H. & Alt, W. J. The normal RS-T segment elevation variant. Am. J. Cardiol. 8, 184–192 (1961).
Mahida, S. et al. History and clinical significance of early repolarization syndrome. Heart Rhythm 12, 242–249 (2015).
Siebermair, J. et al. Early repolarization pattern is the strongest predictor of arrhythmia recurrence in patients with idiopathic ventricular fibrillation: results from a single centre long-term follow-up over 20 years. Europace 18, 718–725 (2016).
Aizawa, Y. et al. Dynamicity of the J-wave in idiopathic ventricular fibrillation with a special reference to pause-dependent augmentation of the J-wave. J. Am. Coll. Cardiol. 59, 1948–1953 (2012).
Amin, A. S. et al. Fever-induced QTc prolongation and ventricular arrhythmias in individuals with type 2 congenital long QT syndrome. J. Clin. Invest. 118, 2552–2561 (2008).
Bastiaenen, R., Hedley, P. L., Christiansen, M. & Behr, E. R. Therapeutic hypothermia and ventricular fibrillation storm in early repolarization syndrome. Heart Rhythm 7, 832–834 (2010).
Nakagawa, K., Nagase, S., Morita, H. & Ito, H. Left ventricular epicardial electrogram recordings in idiopathic ventricular fibrillation with inferior and lateral early repolarization. Heart Rhythm 11, 314–317 (2014).
Tikkanen, J. T. et al. Early repolarization: electrocardiographic phenotypes associated with favorable long-term outcome. Circulation 123, 2666–2673 (2011).
Patel, R. B. et al. Early repolarization associated with ventricular arrhythmias in patients with chronic coronary artery disease. Circ. Arrhythm. Electrophysiol. 3, 489–495 (2010).
Georgopoulos, S. et al. A meta-analysis on the prognostic significance of inferolateral early repolarization pattern in Brugada syndrome. Europace 20, 134–139 (2016).
Watanabe, H. et al. High prevalence of early repolarization in short QT syndrome. Heart Rhythm 7, 647–652 (2010).
Sinner, M. F. et al. Association of early repolarization pattern on ECG with risk of cardiac and all-cause mortality: a population-based prospective cohort study (MONICA/KORA). PLOS Med. 7, e1000314 (2010).
Haruta, D. et al. Incidence and prognostic value of early repolarization pattern in the 12-lead electrocardiogram. Circulation 123, 2931–2937 (2011).
Walsh, J. A. et al. Natural history of the early repolarization pattern in a biracial cohort. J. Am. Coll. Cardiol. 61, 863–869 (2013).
Rollin, A. et al. Prevalence, prognosis, and identification of the malignant form of early repolarization pattern in a population-based study. Am. J. Cardiol. 110, 1302–1308 (2012).
Wu, S.-H., Lin, X.-X., Cheng, Y.-J., Qiang, C.-C. & Zhang, J. Early repolarization pattern and risk for arrhythmia death: a meta-analysis. JACC 61, 645–650 (2013).
Watanabe, H. et al. Clinical characteristics and risk of arrhythmia recurrences in patients with idiopathic ventricular fibrillation associated with early repolarization. Int. J. Cardiol. 159, 238–240 (2012).
Jackson, H. A. et al. LQTS in northern BC: homozygosity for KCNQ1 V205M presents with a more severe cardiac phenotype but with minimal impact on auditory function. Clin. Genet. 86, 85–90 (2014).
de Jager, T., Corbett, C. H., Badenhorst, J. C., Brink, P. A. & Corfield, V. A. Evidence of a long QT founder gene with varying phenotypic expression in South African families. J. Med. Genet. 33, 567–573 (1996).
Winbo, A., Diamant, U.-B., Stattin, E.-L., Jensen, S. M. & Rydberg, A. Low incidence of sudden cardiac death in a Swedish Y111C type 1 long-QT syndrome population. Circ. Cardiovasc. Genet. 2, 558–564 (2009).
Fodstad, H. et al. Four potassium channel mutations account for 73% of the genetic spectrum underlying long-QT syndrome (LQTS) and provide evidence for a strong founder effect in Finland. Ann. Med. 36, 53–63 (2004).
Piippo, K. et al. Homozygosity for a HERG potassium channel mutation causes a severe form of long QT syndrome: identification of an apparent founder mutation in the Finns. J. Am. Coll. Cardiol. 35, 1919–1925 (2000).
Bezzina, C. et al. A single Na+ channel mutation causing both long-QT and Brugada syndromes. Circ. Res. 85, 1206–1213 (1999).
Acknowledgements
A.A.M.W. and C.R.B acknowledge the support of the Leducq Foundation (17CVD02), the Netherlands Heart Foundation (PREDICT2, CVON2018–30) and the Netherlands Organization for Scientific Research (VICI fellowship, 016.150.610, to C.R.B.).
Author information
Authors and Affiliations
Contributions
J.A.O. wrote the manuscript and researched data for the article. C.R.B and A.A.M.W. discussed the content of the manuscript, and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks S. Sanatani and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Offerhaus, J.A., Bezzina, C.R. & Wilde, A.A.M. Epidemiology of inherited arrhythmias. Nat Rev Cardiol 17, 205–215 (2020). https://doi.org/10.1038/s41569-019-0266-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-019-0266-2
This article is cited by
-
Dosage of the pseudoautosomal gene SLC25A6 is implicated in QTc interval duration
Scientific Reports (2023)
-
Gendiagnostik bei kardiovaskulären Erkrankungen
Die Kardiologie (2023)
-
Long-QT founder variant T309I-Kv7.1 with dominant negative pattern may predispose delayed afterdepolarizations under β-adrenergic stimulation
Scientific Reports (2021)
-
Reappraisal of LQTS-causing genes
Nature Reviews Cardiology (2020)
-
Cardiogenetics, 25 years a growing subspecialism
Netherlands Heart Journal (2020)