Abstract
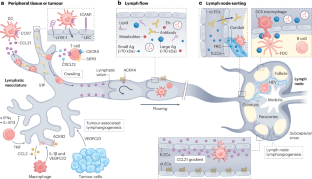
Lymphatic transport maintains homeostatic health and is necessary for immune surveillance, and yet lymphatic growth is often associated with solid tumour development and dissemination. Although tumour-associated lymphatic remodelling and growth were initially presumed to simply expand a passive route for regional metastasis, emerging research puts lymphatic vessels and their active transport at the interface of metastasis, tumour-associated inflammation and systemic immune surveillance. Here, we discuss active mechanisms through which lymphatic vessels shape their transport function to influence peripheral tissue immunity and the current understanding of how tumour-associated lymphatic vessels may both augment and disrupt antitumour immune surveillance. We end by looking forward to emerging areas of interest in the field of cancer immunotherapy in which lymphatic vessels and their transport function are likely key players: the formation of tertiary lymphoid structures, immune surveillance in the central nervous system, the microbiome, obesity and ageing. The lessons learnt support a working framework that defines the lymphatic system as a key determinant of both local and systemic inflammatory networks and thereby a crucial player in the response to cancer immunotherapy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Morton, D. L. et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N. Engl. J. Med. 370, 599–609 (2014).
Zahoor, S. et al. Sentinel lymph node biopsy in breast cancer: a clinical review and update. J. Breast Cancer 20, 217 (2017).
Stacker, S. A. et al. Lymphangiogenesis and lymphatic vessel remodelling in cancer. Nat. Rev. Cancer 14, 159–172 (2014).
Leiter, U. et al. Final analysis of DeCOG-SLT trial: no survival benefit for complete lymph node dissection in patients with melanoma with positive sentinel node. J. Clin. Oncol. 37, 3000–3008 (2019).
Faries, M. B. et al. Completion dissection or observation for sentinel-node metastasis in melanoma. N. Engl. J. Med. 376, 2211–2222 (2017).
Patel, S. P. et al. Neoadjuvant–adjuvant or adjuvant-only pembrolizumab in advanced melanoma. N. Engl. J. Med. 388, 813–823 (2023).
Rozeman, E. A. et al. Survival and biomarker analyses from the OpACIN-neo and OpACIN neoadjuvant immunotherapy trials in stage III melanoma. Nat. Med. 27, 256–263 (2021).
Provencio, M. et al. Perioperative nivolumab and chemotherapy in stage III non-small-cell lung cancer. N. Engl. J. Med. 389, 504–513 (2023).
Delclaux, I., Ventre, K. S., Jones, D. & Lund, A. W. The tumor-draining lymph node as a reservoir for systemic immune surveillance. Trends Cancer 10, 28–37 (2023).
Reticker-Flynn, N. E. et al. Lymph node colonization induces tumor-immune tolerance to promote distant metastasis. Cell 185, 1924–1942.e23 (2022). First preclinical demonstration that LN metastasis suppresses systemic immune surveillance through the local induction of Treg cells and thereby indirectly enables distant tumour progression.
Lei, P.-J. et al. Cancer cell plasticity and MHC-II-mediated immune tolerance promote breast cancer metastasis to lymph nodes. J. Exp. Med. 220, e20221847 (2023).
Petrova, T. V. & Koh, G. Y. Biological functions of lymphatic vessels. Science 369, eaax4063 (2020).
Chary, S. R. & Jain, R. K. Direct measurement of interstitial convection and diffusion of albumin in normal and neoplastic tissues by fluorescence photobleaching. Proc. Natl Acad. Sci. USA 86, 5385–5389 (1989).
Fleury, M. E., Boardman, K. C. & Swartz, M. A. Autologous morphogen gradients by subtle interstitial flow and matrix interactions. Biophys. J. 91, 113–121 (2006).
Charman, S. A., McLennan, D. N., Edwards, G. A. & Porter, C. J. H. Lymphatic absorption is a significant contributor to the subcutaneous bioavailability of insulin in a sheep model. Pharm. Res. 18, 1620–1626 (2001).
Martel, C. et al. Lymphatic vasculature mediates macrophage reverse cholesterol transport in mice. J. Clin. Invest. 123, 1571–1579 (2013).
Shields, J. D. et al. Autologous chemotaxis as a mechanism of tumor cell homing to lymphatics via interstitial flow and autocrine CCR7 signaling. Cancer Cell 11, 526–538 (2007).
Hansen, K. C., D’Alessandro, A., Clement, C. C. & Santambrogio, L. Lymph formation, composition and circulation: a proteomics perspective. Int. Immunol. 27, 219–227 (2015).
Clement, C. C. & Santambrogio, L. The lymph self-antigen repertoire. Front. Immunol. 4, 424 (2013).
Yao, L.-C., Baluk, P., Srinivasan, R. S., Oliver, G. & McDonald, D. M. Plasticity of button-like junctions in the endothelium of airway lymphatics in development and inflammation. Am. J. Pathol. 180, 2561–2575 (2012).
Zhang, F. et al. Lacteal junction zippering protects against diet-induced obesity. Science 361, 599–603 (2018).
Churchill, M. J. et al. Infection-induced lymphatic zippering restricts fluid transport and viral dissemination from skin. J. Exp. Med. 219, e20211830 (2022).
Jannaway, M. et al. VEGFR3 is required for button junction formation in lymphatic vessels. Cell Rep. 42, 112777 (2023).
Triacca, V., Güç, E., Kilarski, W. W., Pisano, M. & Swartz, M. A. Transcellular pathways in lymphatic endothelial cells regulate changes in solute transport by fluid stress. Circ. Res. 120, 1440–1452 (2017).
Prevo, R., Banerji, S., Ferguson, D. J. P., Clasper, S. & Jackson, D. G. Mouse LYVE-1 is an endocytic receptor for hyaluronan in lymphatic endothelium. J. Biol. Chem. 276, 19420–19430 (2001).
Proulx, S. T. et al. Quantitative imaging of lymphatic function with liposomal indocyanine green. Cancer Res. 70, 7053–7062 (2010).
Harrell, M. I., Iritani, B. M. & Ruddell, A. Tumor-induced sentinel lymph node lymphangiogenesis and increased lymph flow precede melanoma metastasis. Am. J. Pathol. 170, 774–786 (2007).
Gogineni, A. et al. Inhibition of VEGF-C modulates distal lymphatic remodeling and secondary metastasis. PLoS ONE 8, e68755 (2013).
Broggi, M. A. S. et al. Tumor-associated factors are enriched in lymphatic exudate compared to plasma in metastatic melanoma patients. J. Exp. Med. 216, 1091–1107 (2019).
García-Silva, S. et al. Use of extracellular vesicles from lymphatic drainage as surrogate markers of melanoma progression and BRAF V600E mutation. J. Exp. Med. 216, 1061–1070 (2019).
Sixt, M. et al. The conduit system transports soluble antigens from the afferent lymph to resident dendritic cells in the T cell area of the lymph node. Immunity 22, 19–29 (2005).
Rantakari, P. et al. The endothelial protein PLVAP in lymphatics controls the entry of lymphocytes and antigens into lymph nodes. Nat. Immunol. 16, 386–396 (2015).
Roozendaal, R. et al. Conduits mediate transport of low-molecular-weight antigen to lymph node follicles. Immunity 30, 264–276 (2009).
Gretz, J. E., Norbury, C. C., Anderson, A. O., Proudfoot, A. E. I. & Shaw, S. Lymph-borne chemokines and other low molecular weight molecules reach high endothelial venules via specialized conduits while a functional barrier limits access to the lymphocyte microenvironments in lymph node. Cortex. J. Exp. Med. 192, 1425–1440 (2000).
Carrasco, Y. R. & Batista, F. D. B cells acquire particulate antigen in a macrophage-rich area at the boundary between the follicle and the subcapsular sinus of the lymph node. Immunity 27, 160–171 (2007).
Pape, K. A., Catron, D. M., Itano, A. A. & Jenkins, M. K. The humoral immune response is initiated in lymph nodes by B cells that acquire soluble antigen directly in the follicles. Immunity 26, 491–502 (2007).
Steele, M. M. & Lund, A. W. Afferent lymphatic transport and peripheral tissue immunity. J. Immunol. 206, 264–272 (2021).
Loo, C. P. et al. Lymphatic vessels balance viral dissemination and immune activation following cutaneous viral infection. Cell Rep. 20, 3176–3187 (2017).
Lund, A. W. et al. Lymphatic vessels regulate immune microenvironments in human and murine melanoma. J. Clin. Invest. 126, 3389–3402 (2016).
Ferris, S. T. et al. cDC1 prime and are licensed by CD4+ T cells to induce anti-tumour immunity. Nature 584, 624–629 (2020).
Hildner, K. et al. Batf3 deficiency reveals a critical role for CD8α+ dendritic cells in cytotoxic T cell immunity. Science 322, 1097–1100 (2008).
Roberts, E. W. et al. Critical role for CD103+/CD141+ dendritic cells bearing CCR7 for tumor antigen trafficking and priming of T cell immunity in melanoma. Cancer Cell 30, 324–336 (2016).
Salmon, H. et al. Expansion and activation of CD103+ dendritic cell progenitors at the tumor site enhances tumor responses to therapeutic PD-L1 and BRAF inhibition. Immunity 44, 924–938 (2016).
Vigl, B. et al. Tissue inflammation modulates gene expression of lymphatic endothelial cells and dendritic cell migration in a stimulus-dependent manner. Blood 118, 205–215 (2011).
Saeki, H., Moore, A. M., Brown, M. J. & Hwang, S. T. Cutting edge: secondary lymphoid-tissue chemokine (SLC) and CC chemokine receptor 7 (CCR7) participate in the emigration pathway of mature dendritic cells from the skin to regional lymph nodes. J. Immunol. 162, 2472–2475 (1999).
Förster, R. et al. CCR7 coordinates the primary immune response by establishing functional microenvironments in secondary lymphoid organs. Cell 99, 23–33 (1999).
Davalos-Misslitz, A. C. M. et al. Generalized multi-organ autoimmunity in CCR7-deficient mice. Eur. J. Immunol. 37, 613–622 (2007).
Thomas, S. N. et al. Impaired humoral immunity and tolerance in K14-VEGFR-3-Ig mice that lack dermal lymphatic drainage. J. Immunol. 189, 2181–2190 (2012).
Pflicke, H. & Sixt, M. Preformed portals facilitate dendritic cell entry into afferent lymphatic vessels. J. Exp. Med. 206, 2925–2935 (2009).
Baluk, P. et al. Functionally specialized junctions between endothelial cells of lymphatic vessels. J. Exp. Med. 204, 2349–2362 (2007).
Lämmermann, T. et al. Rapid leukocyte migration by integrin-independent flowing and squeezing. Nature 453, 51–55 (2008).
Nitschké, M. et al. Differential requirement for ROCK in dendritic cell migration within lymphatic capillaries in steady-state and inflammation. Blood 120, 2249–2258 (2012).
Miteva, D. O. et al. Transmural flow modulates cell and fluid transport functions of lymphatic endothelium. Circ. Res. 106, 920–931 (2010).
Weber, M. et al. Interstitial dendritic cell guidance by haptotactic chemokine gradients. Science 339, 328–332 (2013).
Schumann, K. et al. Immobilized chemokine fields and soluble chemokine gradients cooperatively shape migration patterns of dendritic cells. Immunity 32, 703–713 (2010).
Russo, E. et al. Intralymphatic CCL21 promotes tissue egress of dendritic cells through afferent lymphatic vessels. Cell Rep. 14, 1723–1734 (2016).
Bastow, C. R. et al. Scavenging of soluble and immobilized CCL21 by ACKR4 regulates peripheral dendritic cell emigration. Proc. Natl Acad. Sci. USA 118, e2025763118 (2021).
Friess, M. C. et al. Mechanosensitive ACKR4 scavenges CCR7 chemokines to facilitate T cell de-adhesion and passive transport by flow in inflamed afferent lymphatics. Cell Rep. 38, 110334 (2022).
Ulvmar, M. H. et al. The atypical chemokine receptor CCRL1 shapes functional CCL21 gradients in lymph nodes. Nat. Immunol. 15, 623–630 (2014).
Druzd, D. et al. Lymphocyte circadian clocks control lymph node trafficking and adaptive immune responses. Immunity 46, 120–132 (2017).
Holtkamp, S. J. et al. Circadian clocks guide dendritic cells into skin lymphatics. Nat. Immunol. 22, 1375–1381 (2021). This study enhanced our understanding of oscillatory DC migration through lymphatic vessels, demonstrating rhythmic expression of key transcripts in LECs whose protein products mediate DC migration and which are dependent on the clock gene Bmal1.
Qian, D. C. et al. Effect of immunotherapy time-of-day infusion on overall survival among patients with advanced melanoma in the USA (MEMOIR): a propensity score-matched analysis of a single-centre, longitudinal study. Lancet Oncol. 22, 1777–1786 (2021).
Johnson, L. A. et al. An inflammation-induced mechanism for leukocyte transmigration across lymphatic vessel endothelium. J. Exp. Med. 203, 2763–2777 (2006).
Johnson, L. A., Prevo, R., Clasper, S. & Jackson, D. G. Inflammation-induced uptake and degradation of the lymphatic endothelial hyaluronan receptor LYVE-1. J. Biol. Chem. 282, 33671–33680 (2007).
Johnson, L. A. et al. Dendritic cells enter lymph vessels by hyaluronan-mediated docking to the endothelial receptor LYVE-1. Nat. Immunol. 18, 762–770 (2017).
Maddaluno, L. et al. The adhesion molecule L1 regulates transendothelial migration and trafficking of dendritic cells. J. Exp. Med. 206, 623–635 (2009).
Debes, G. F. et al. Chemokine receptor CCR7 required for T lymphocyte exit from peripheral tissues. Nat. Immunol. 6, 889–894 (2005).
Bromley, S. K., Thomas, S. Y. & Luster, A. D. Chemokine receptor CCR7 guides T cell exit from peripheral tissues and entry into afferent lymphatics. Nat. Immunol. 6, 895–901 (2005).
Brown, M. N. et al. Chemoattractant receptors and lymphocyte egress from extralymphoid tissue: changing requirements during the course of inflammation. J. Immunol. 185, 4873–4882 (2010).
Torcellan, T. et al. In vivo photolabeling of tumor-infiltrating cells reveals highly regulated egress of T-cell subsets from tumors. Proc. Natl Acad. Sci. USA 114, 5677–5682 (2017).
Pham, T. H. M. et al. Lymphatic endothelial cell sphingosine kinase activity is required for lymphocyte egress and lymphatic patterning. J. Exp. Med. 207, 17–27 (2010).
Skon, C. N. et al. Transcriptional downregulation of S1pr1 is required for the establishment of resident memory CD8+ T cells. Nat. Immunol. 14, 1285–1293 (2013).
Evrard, M. et al. Sphingosine 1-phosphate receptor 5 (S1PR5) regulates the peripheral retention of tissue-resident lymphocytes. J. Exp. Med. 219, e20210116 (2022).
Mackay, L. K. et al. Cutting edge: CD69 interference with sphingosine-1-phosphate receptor function regulates peripheral T cell retention. J. Immunol. 194, 2059–2063 (2015).
Locati, M. et al. Silent chemoattractant receptors: D6 as a decoy and scavenger receptor for inflammatory CC chemokines. Cytokine Growth Factor Rev. 16, 679–686 (2005).
Weber, M. et al. The chemokine receptor D6 constitutively traffics to and from the cell surface to internalize and degrade chemokines. Mol. Biol. Cell 15, 2492–2508 (2004).
De La Torre, Y. M. et al. Increased inflammation in mice deficient for the chemokine decoy receptor D6. Eur. J. Immunol. 35, 1342–1346 (2005).
Vetrano, S. et al. The lymphatic system controls intestinal inflammation and inflammation-associated colon cancer through the chemokine decoy receptor D6. Gut 59, 197–206 (2010).
Lee, K. M. et al. D6 facilitates cellular migration and fluid flow to lymph nodes by suppressing lymphatic congestion. Blood 118, 6220–6229 (2011).
Hirakawa, S. et al. VEGF-A induces tumor and sentinel lymph node lymphangiogenesis and promotes lymphatic metastasis. J. Exp. Med. 201, 1089–1099 (2005).
Hirakawa, S. et al. VEGF-C-induced lymphangiogenesis in sentinel lymph nodes promotes tumor metastasis to distant sites. Blood 109, 1010–1017 (2007).
Angeli, V. et al. B cell-driven lymphangiogenesis in inflamed lymph nodes enhances dendritic cell mobilization. Immunity 24, 203–215 (2006).
Skobe, M. et al. Induction of tumor lymphangiogenesis by VEGF-C promotes breast cancer metastasis. Nat. Med. 7, 192–198 (2001).
Padera, T. P. et al. Lymphatic metastasis in the absence of functional intratumor lymphatics. Science 296, 1883–1886 (2002).
Stritt, S., Koltowska, K. & Mäkinen, T. Homeostatic maintenance of the lymphatic vasculature. Trends Mol. Med. 27, 955–970 (2021).
Jeltsch, M. et al. Hyperplasia of lymphatic vessels in VEGF-C transgenic mice. Science 276, 1423–1425 (1997).
Stacker, S. A. et al. VEGF-D promotes the metastatic spread of tumor cells via the lymphatics. Nat. Med. 7, 186–191 (2001).
Karnezis, T. et al. VEGF-D promotes tumor metastasis by regulating prostaglandins produced by the collecting lymphatic endothelium. Cancer Cell 21, 181–195 (2012).
Skobe, M. et al. Concurrent induction of lymphangiogenesis, angiogenesis, and macrophage recruitment by vascular endothelial growth factor-C in melanoma. Am. J. Pathol. 159, 893–903 (2001).
Schoppmann, S. F. et al. Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral lymphangiogenesis. Am. J. Pathol. 161, 947–956 (2002).
Kubota, Y. et al. M-CSF inhibition selectively targets pathological angiogenesis and lymphangiogenesis. J. Exp. Med. 206, 1089–1102 (2009).
Petkova, M. et al. Immune-interacting lymphatic endothelial subtype at capillary terminals drives lymphatic malformation. J. Exp. Med. 220, e20220741 (2023). This study defined a novel immune interacting subtype of LECs residing at the end of capillaries in oncogenic Pik3ca-dependent lymphatic malformations that activated a positive feedback loop with local macrophages to promote lymphatic growth.
Weichand, B. et al. S1PR1 on tumor-associated macrophages promotes lymphangiogenesis and metastasis via NLRP3/IL-1β. J. Exp. Med. 214, 2695–2713 (2017).
Lyons, T. R. et al. Cyclooxygenase-2-dependent lymphangiogenesis promotes nodal metastasis of postpartum breast cancer. J. Clin. Invest. 124, 3901–3912 (2014).
Farnsworth, R. H., Karnezis, T., Maciburko, S. J., Mueller, S. N. & Stacker, S. A. The interplay between lymphatic vessels and chemokines. Front. Immunol. 10, 518 (2019).
Hong, H. et al. TNF-alpha promotes lymphangiogenesis and lymphatic metastasis of gallbladder cancer through the ERK1/2/AP-1/VEGF-D pathway. BMC Cancer 16, 240 (2016).
Ji, H. et al. TNFR1 mediates TNF-α-induced tumour lymphangiogenesis and metastasis by modulating VEGF-C-VEGFR3 signalling. Nat. Commun. 5, 4944 (2014).
Zhuo, W. et al. The CXCL12–CXCR4 chemokine pathway: a novel axis regulates lymphangiogenesis. Clin. Cancer Res. 18, 5387–5398 (2012).
Savetsky, I. L. et al. Th2 cytokines inhibit lymphangiogenesis. PLoS ONE 10, e0126908 (2015).
Kataru, R. P. et al. T lymphocytes negatively regulate lymph node lymphatic vessel formation. Immunity 34, 96–107 (2011).
Garnier, L. et al. IFN-γ-dependent tumor-antigen cross-presentation by lymphatic endothelial cells promotes their killing by T cells and inhibits metastasis. Sci. Adv. 8, eabl5162 (2022). Building off previous work that demonstrated the antigen presentation capabilities of LECs, here the authors of this study demonstrate that IFNγ-induced antigen presentation in tumour-associated LECs renders them susceptible to cytotoxic T cell killing, which in turn reduces LN metastasis.
Xu, W., Harris, N. R. & Caron, K. M. Lymphatic vasculature: an emerging therapeutic target and drug delivery route. Annu. Rev. Med. 72, 167–182 (2021).
Lohela, M., Heloterä, H., Haiko, P., Dumont, D. J. & Alitalo, K. Transgenic induction of vascular endothelial growth factor-C is strongly angiogenic in mouse embryos but leads to persistent lymphatic hyperplasia in adult tissues. Am. J. Pathol. 173, 1891–1901 (2008).
Gengenbacher, N. et al. Timed Ang2-targeted therapy identifies the angiopoietin–tie pathway as key regulator of fatal lymphogenous metastasis. Cancer Discov. 11, 424–445 (2021). Using a preclinical model of grafted melanoma fragments, the authors of this study establish that targeting the lymphangiogenic molecule, angiopoietin-2, in the adjuvant setting is sufficient to reduce regional metastasis and improve survival.
Cao, R. et al. Collaborative interplay between FGF-2 and VEGF-C promotes lymphangiogenesis and metastasis. Proc. Natl Acad. Sci. USA 109, 15894–15899 (2012).
Björndahl, M. et al. Insulin-like growth factors 1 and 2 induce lymphangiogenesis in vivo. Proc. Natl Acad. Sci. USA 102, 15593–15598 (2005).
Wong, B. W. et al. The role of fatty acid β-oxidation in lymphangiogenesis. Nature 542, 49–54 (2017).
Yu, P. et al. FGF-dependent metabolic control of vascular development. Nature 545, 224–228 (2017).
Lund, A. W. et al. VEGF-C promotes immune tolerance in B16 melanomas and cross-presentation of tumor antigen by lymph node lymphatics. Cell Rep. 1, 191–199 (2012). The first study to specifically investigate the impact of VEGFC on antitumor immune surveillance, identifying a pro-inflammatory but immune suppressive effect in the melanoma TME.
Kataru, R. P. et al. Critical role of CD11b + macrophages and VEGF in inflammatory lymphangiogenesis, antigen clearance, and inflammation resolution. Blood 113, 5650–5659 (2009).
Weinkopff, T. et al. Leishmania major infection-induced VEGF-A/VEGFR-2 signaling promotes lymphangiogenesis that controls disease. J. Immunol. Baltim. MD 1950 197, 1823–1831 (2016).
D’Alessio, S. et al. VEGF-C-dependent stimulation of lymphatic function ameliorates experimental inflammatory bowel disease. J. Clin. Invest. 124, 3863–3878 (2014).
Alitalo, A. K. et al. VEGF-C and VEGF-D blockade inhibits inflammatory skin carcinogenesis. Cancer Res. 73, 4212–4221 (2013).
Lane, R. S. et al. IFNγ-activated dermal lymphatic vessels inhibit cytotoxic T cells in melanoma and inflamed skin. J. Exp. Med. 215, 3057–3074 (2018). Direct in vivo demonstration that lymphatic intrinsic sensing of IFNγ in tumours regulates the persistence of effector immune responses, establishing a mechanism of lymphatic adaptation that promotes immune suppression. Together with Garnier et al. (2022), these two studies highlight the impact of IFNγ on lymphatic remodelling and the impact of this lymphatic remodelling on both immune surveillance and metastasis.
Dieterich, L. C. et al. Tumor-associated lymphatic vessels upregulate PDL1 to inhibit T-cell activation. Front. Immunol. 8, 66 (2017).
Mueller, S. N. et al. PD-L1 has distinct functions in hematopoietic and nonhematopoietic cells in regulating T cell responses during chronic infection in mice. J. Clin. Invest. 120, 2508–2515 (2010).
Cousin, N. et al. Lymphatic PD-L1 expression restricts tumor-specific CD8+ T-cell responses. Cancer Res. 81, 4133–4144 (2021).
Gkountidi, A. O. et al. MHC class II antigen presentation by lymphatic endothelial cells in tumors promotes intratumoral regulatory T cell-suppressive functions. Cancer Immunol. Res. 9, 748–764 (2021). This study uses a genetic model to specifically delete MHCII in LECs and demonstrates a direct effect on the accumulation and suppressive function of Treg cells within the TME. These data provide the most recent evidence that LECs have antigen-presenting capabilities that functionally shape peripheral T cell responses.
Fankhauser, M. et al. Tumor lymphangiogenesis promotes T cell infiltration and potentiates immunotherapy in melanoma. Sci. Transl. Med. 9, eaal4712 (2017).
Song, E. et al. VEGF-C-driven lymphatic drainage enables immunosurveillance of brain tumours. Nature 577, 689–694 (2020). This study demonstrates that VEGFC-driven lymphangiogenesis in the meninges enhances immunosurveillance and response to immunotherapy in brain tumours.
Issa, A., Le, T. X., Shoushtari, A. N., Shields, J. D. & Swartz, M. A. Vascular endothelial growth factor-C and C-C chemokine receptor 7 in tumor cell-lymphatic cross-talk promote invasive phenotype. Cancer Res. 69, 349–357 (2009).
Sasso, M. S. et al. Lymphangiogenesis-inducing vaccines elicit potent and long-lasting T cell immunity against melanomas. Sci. Adv. 7, eabe4362 (2021). This study demonstrates that VEGFC expression in the context of topical adjuvants promotes antigen-specific T cell priming providing superior tumour protection and long-term immunological memory.
Fear, V. S. et al. Tumour draining lymph node-generated CD8 T cells play a role in controlling lung metastases after a primary tumour is removed but not when adjuvant immunotherapy is used. Cancer Immunol. Immunother. 70, 3249–3258 (2021).
Huang, Q. et al. The primordial differentiation of tumor-specific memory CD8+ T cells as bona fide responders to PD-1/PD-L1 blockade in draining lymph nodes. Cell 185, 4049–4066.e25 (2022).
Fransen, M. F. et al. Tumor-draining lymph nodes are pivotal in PD-1/PD-L1 checkpoint therapy. JCI Insight 3, e124507 (2018).
Connolly, K. A. et al. A reservoir of stem-like CD8 + T cells in the tumor-draining lymph node preserves the ongoing antitumor immune response. Sci. Immunol. 6, eabg7836 (2021).
Spitzer, M. H. et al. Systemic immunity is required for effective cancer immunotherapy. Cell 168, 487–502.e15 (2017).
Tewalt, E. F. et al. Lymphatic endothelial cells induce tolerance via PD-L1 and lack of costimulation leading to high-level PD-1 expression on CD8 T cells. Blood 120, 4772–4782 (2012).
Cohen, J. N. et al. Lymph node-resident lymphatic endothelial cells mediate peripheral tolerance via Aire-independent direct antigen presentation. J. Exp. Med. 207, 681–688 (2010).
Hirosue, S. et al. Steady-state antigen scavenging, cross-presentation, and CD8+ T cell priming: a new role for lymphatic endothelial cells. J. Immunol. 192, 5002–5011 (2014).
Vokali, E. et al. Lymphatic endothelial cells prime naïve CD8+ T cells into memory cells under steady-state conditions. Nat. Commun. 11, 538 (2020).
Tamburini, B. A., Burchill, M. A. & Kedl, R. M. Antigen capture and archiving by lymphatic endothelial cells following vaccination or viral infection. Nat. Commun. 5, 3989 (2014).
Lukacs-Kornek, V. et al. Regulated release of nitric oxide by nonhematopoietic stroma controls expansion of the activated T cell pool in lymph nodes. Nat. Immunol. 12, 1096–1104 (2011).
Dubrot, J. et al. Lymph node stromal cells acquire peptide–MHCII complexes from dendritic cells and induce antigen-specific CD4+ T cell tolerance. J. Exp. Med. 211, 1153–1166 (2014).
Baptista, A. P. et al. Lymph node stromal cells constrain immunity via MHC class II self-antigen presentation. eLife 3, e04433 (2014).
Nadafi, R. et al. Lymph node stromal cells generate antigen-specific regulatory T cells and control autoreactive T and B cell responses. Cell Rep. 30, 4110–4123.e4 (2020).
Dubrot, J. et al. Absence of MHC-II expression by lymph node stromal cells results in autoimmunity. Life Sci. Alliance 1, e201800164 (2018).
Horton, B. L. et al. Lack of CD8+ T cell effector differentiation during priming mediates checkpoint blockade resistance in non-small cell lung cancer. Sci. Immunol. 6, eabi8800 (2021).
Zagorulya, M. et al. Tissue-specific abundance of interferon-gamma drives regulatory T cells to restrain DC1-mediated priming of cytotoxic T cells against lung cancer. Immunity 56, 386–405.e10 (2023).
Esterházy, D. et al. Compartmentalized gut lymph node drainage dictates adaptive immune responses. Nature 569, 126–130 (2019).
Houston, S. A. et al. The lymph nodes draining the small intestine and colon are anatomically separate and immunologically distinct. Mucosal Immunol. 9, 468–478 (2016).
Brown, H., Komnick, M. R., Brigleb, P. H., Dermody, T. S. & Esterházy, D. Lymph node sharing between pancreas, gut, and liver leads to immune crosstalk and regulation of pancreatic autoimmunity. Immunity 56, 2070–2085.e11 (2023). This study demonstrates LN sharing among the gut, liver and pancreas where tissue-specific characteristics of migratory DC populations impact antigen presentation within the shared LNs.
Pöysti, S. et al. Infection with the enteric pathogen C. rodentium promotes islet-specific autoimmunity by activating a lymphatic route from the gut to pancreatic lymph node. Mucosal Immunol. 15, 471–479 (2022).
Laidlaw, B. J., Gray, E. E., Zhang, Y., Ramírez-Valle, F. & Cyster, J. G. Sphingosine-1-phosphate receptor 2 restrains egress of γδ T cells from the skin. J. Exp. Med. 216, 1487–1496 (2019).
Ataide, M. A. et al. Lymphatic migration of unconventional T cells promotes site-specific immunity in distinct lymph nodes. Immunity 55, 1813–1828.e9 (2022). This study importantly demonstrates that site-specific LN immunity is installed in part by the lymphatic migration of unconventional T cells.
Steele, M. M. et al. T cell egress via lymphatic vessels is tuned by antigen encounter and limits tumor control. Nat. Immunol. 24, 664–675 (2023). This study demonstrates that CD8+ T cell egress out of tumours depends on local antigen encounter and lymphatic-derived chemokines and provides proof of principle that targeting egress could shape the intratumoural T cell repertoire and response to immunotherapy.
Li, Z. et al. In vivo labeling reveals continuous trafficking of TCF-1+ T cells between tumor and lymphoid tissue. J. Exp. Med. 219, e20210749 (2022). Together with Steele et al. (2023), this paper indicates that antigen-experienced TCF1+ cells recirculate out of the TME and that at least a subset of these may have stem-like properties.
Utzschneider, D. T. et al. T cell factor 1-expressing memory-like CD8+ T cells sustain the immune response to chronic viral infections. Immunity 45, 415–427 (2016).
Gearty, S. V. et al. An autoimmune stem-like CD8 T cell population drives type 1 diabetes. Nature 602, 156–161 (2022).
Prokhnevska, N. et al. CD8+ T cell activation in cancer comprises an initial activation phase in lymph nodes followed by effector differentiation within the tumor. Immunity 56, 107–124.e5 (2023).
Salmi, M., Karikoski, M., Elima, K., Rantakari, P. & Jalkanen, S. CD44 binds to macrophage mannose receptor on lymphatic endothelium and supports lymphocyte migration via afferent lymphatics. Circ. Res. 112, 1577–1582 (2013).
Teijeira, A. et al. T cell migration from inflamed skin to draining lymph nodes requires intralymphatic crawling supported by ICAM-1/LFA-1 interactions. Cell Rep. 18, 857–865 (2017).
Karikoski, M. et al. Clever-1/stabilin-1 regulates lymphocyte migration within lymphatics and leukocyte entrance to sites of inflammation: innate immunity. Eur. J. Immunol. 39, 3477–3487 (2009).
Li, G. et al. TGF-β-dependent lymphoid tissue residency of stem-like T cells limits response to tumor vaccine. Nat. Commun. 13, 6043 (2022).
Molodtsov, A. K. et al. Resident memory CD8+ T cells in regional lymph nodes mediate immunity to metastatic melanoma. Immunity 54, 2117–2132.e7 (2021). This study establishes the presence of TRM cells in mouse and human tumour-draining LNs, indicating that tumour-draining LNs may possess mechanisms that protect from regional metastasis.
Siddiqui, I. et al. Intratumoral Tcf1+ PD-1+ CD8+ T cells with stem-like properties promote tumor control in response to vaccination and checkpoint blockade immunotherapy. Immunity 50, 195–211.e10 (2019).
Heim, T. A. et al. Lymphatic vessel transit seeds precursors to cytotoxic resident memory T cells in skin draining lymph nodes. Preprint at bioRxiv https://doi.org/10.1101/2023.08.29.555369 (2023).
Stolley, J. M. et al. Retrograde migration supplies resident memory T cells to lung-draining LN after influenza infection. J. Exp. Med. 217, e20192197 (2020).
Pai, J. A. et al. Lineage tracing reveals clonal progenitors and long-term persistence of tumor-specific T cells during immune checkpoint blockade. Cancer Cell 41, 776–790.e7 (2023).
Yost, K. E. et al. Clonal replacement of tumor-specific T cells following PD-1 blockade. Nat. Med. 25, 1251–1259 (2019).
Beura, L. K. et al. T cells in nonlymphoid tissues give rise to lymph-node-resident memory T cells. Immunity 48, 327–338.e5 (2018).
Di Pilato, M. et al. CXCR6 positions cytotoxic T cells to receive critical survival signals in the tumor microenvironment. Cell 184, 4512–4530.e22 (2021).
Lesch, S. et al. T cells armed with C-X-C chemokine receptor type 6 enhance adoptive cell therapy for pancreatic tumours. Nat. Biomed. Eng. 5, 1246–1260 (2021).
Heim, T. A., Lin, Z., Steele, M. M., Mudianto, T. & Lund, A. W. CXCR6 promotes dermal CD8+ T cell survival and transition to long-term tissue residence. Preprint at bioRxiv https://doi.org/10.1101/2023.02.14.528487 (2023).
Weber, E. W. et al. Transient rest restores functionality in exhausted CAR-T cells through epigenetic remodeling. Science 372, eaba1786 (2021).
Cloughesy, T. F. et al. Neoadjuvant anti-PD-1 immunotherapy promotes a survival benefit with intratumoral and systemic immune responses in recurrent glioblastoma. Nat. Med. 25, 477–486 (2019).
Schudel, A., Francis, D. M. & Thomas, S. N. Material design for lymph node drug delivery. Nat. Rev. Mater. 4, 415–428 (2019).
Van Pul, K. M. et al. Local delivery of low-dose anti-CTLA-4 to the melanoma lymphatic basin leads to systemic Treg reduction and effector T cell activation. Sci. Immunol. 7, eabn8097 (2022). The results of a recent phase I clinical trial leveraging lymphatic transport for local delivery of CTLA4 antibodies that led to boosted melanoma-specific T cell responses, suggesting that the tumour-draining LN may be a functional target for ICB.
Koster, B. D. et al. Local adjuvant treatment with low-dose CpG-B offers durable protection against disease recurrence in clinical stage I–II melanoma: data from two randomized phase II trials. Clin. Cancer Res. 23, 5679–5686 (2017).
Gur-Cohen, S. et al. Stem cell-driven lymphatic remodeling coordinates tissue regeneration. Science 366, 1218–1225 (2019).
Niec, R. E. et al. Lymphatics act as a signaling hub to regulate intestinal stem cell activity. Cell Stem Cell 29, 1067–1082.e18 (2022).
Palikuqi, B. et al. Lymphangiocrine signals are required for proper intestinal repair after cytotoxic injury. Cell Stem Cell 29, 1262–1272.e5 (2022).
Liu, X. et al. Lymphoangiocrine signals promote cardiac growth and repair. Nature 588, 705–711 (2020).
Cabrita, R. et al. Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature 577, 561–565 (2020).
Helmink, B. A. et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 577, 549–555 (2020).
Ruddle, N. H. Lymphatic vessels and tertiary lymphoid organs. J. Clin. Invest. 124, 953–959 (2014).
Femel, J. et al. Quantitative multiplex immunohistochemistry reveals inter-patient lymphovascular and immune heterogeneity in primary cutaneous melanoma. Front. Immunol. 15, 1328602 (2021).
Overacre-Delgoffe, A. E. et al. Microbiota-specific T follicular helper cells drive tertiary lymphoid structures and anti-tumor immunity against colorectal cancer. Immunity 54, 2812–2824.e4 (2021).
Mounzer, R. H. et al. Lymphotoxin-alpha contributes to lymphangiogenesis. Blood 116, 2173–2182 (2010).
Cao, E. et al. Mesenteric lymphatic dysfunction promotes insulin resistance and represents a potential treatment target in obesity. Nat. Metab. 3, 1175–1188 (2021).
Shields, J. D., Kourtis, I. C., Tomei, A. A., Roberts, J. M. & Swartz, M. A. Induction of lymphoidlike stroma and immune escape by tumors that express the chemokine CCL21. Science 328, 749–752 (2010).
Czepielewski, R. S. et al. Ileitis-associated tertiary lymphoid organs arise at lymphatic valves and impede mesenteric lymph flow in response to tumor necrosis factor. Immunity 54, 2795–2811.e9 (2021). This study demonstrates that TLS formation at lymphatic valves in a TNF-dependent mouse model of intestinal inflammation leads to impaired lymphatic drainage and leukocyte trafficking that may further exacerbate local inflammation.
Reed, H. O. et al. Lymphatic impairment leads to pulmonary tertiary lymphoid organ formation and alveolar damage. J. Clin. Invest. 129, 2514–2526 (2019).
Louveau, A. et al. Structural and functional features of central nervous system lymphatic vessels. Nature 523, 337–341 (2015).
Louveau, A. et al. CNS lymphatic drainage and neuroinflammation are regulated by meningeal lymphatic vasculature. Nat. Neurosci. 21, 1380–1391 (2018).
Aspelund, A. et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J. Exp. Med. 212, 991–999 (2015).
Jacob, L. et al. Conserved meningeal lymphatic drainage circuits in mice and humans. J. Exp. Med. 219, e20220035 (2022).
Ahn, J. H. et al. Meningeal lymphatic vessels at the skull base drain cerebrospinal fluid. Nature 572, 62–66 (2019).
Smyth, L. C. D. et al. Identification of direct connections between the dura and the brain. Nature https://doi.org/10.1038/s41586-023-06993-7 (2024).
Ma, Q., Ineichen, B. V., Detmar, M. & Proulx, S. T. Outflow of cerebrospinal fluid is predominantly through lymphatic vessels and is reduced in aged mice. Nat. Commun. 8, 1434 (2017).
Ma, Q., Decker, Y., Müller, A., Ineichen, B. V. & Proulx, S. T. Clearance of cerebrospinal fluid from the sacral spine through lymphatic vessels. J. Exp. Med. 216, 2492–2502 (2019).
Spera, I. et al. Open pathways for cerebrospinal fluid outflow at the cribriform plate along the olfactory nerves. eBioMedicine 91, 104558 (2023).
Iliff, J. J. et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci. Transl. Med. 4, 147ra111 (2012).
Kovacs, M. A. et al. Meningeal lymphatic drainage promotes T cell responses against Toxoplasma gondii but is dispensable for parasite control in the brain. eLife 11, e80775 (2022).
Li, X. et al. Meningeal lymphatic vessels mediate neurotropic viral drainage from the central nervous system. Nat. Neurosci. 25, 577–587 (2022).
Hsu, M. et al. Neuroinflammation-induced lymphangiogenesis near the cribriform plate contributes to drainage of CNS-derived antigens and immune cells. Nat. Commun. 10, 229 (2019).
Li, Z. et al. Blockade of VEGFR3 signaling leads to functional impairment of dural lymphatic vessels without affecting autoimmune neuroinflammation. Sci. Immunol. 8, eabq0375 (2023).
Hu, X. et al. Meningeal lymphatic vessels regulate brain tumor drainage and immunity. Cell Res. 30, 229–243 (2020).
Gopalakrishnan, V. et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 359, 97–103 (2018).
Bernier-Latmani, J. et al. DLL4 promotes continuous adult intestinal lacteal regeneration and dietary fat transport. J. Clin. Invest. 125, 4572–4586 (2015).
Suh, S. H. et al. Gut microbiota regulates lacteal integrity by inducing VEGF‐C in intestinal villus macrophages. EMBO Rep. 20, e46927 (2019).
Becker, F. et al. Dynamic gut microbiome changes following regional intestinal lymphatic obstruction in primates. Pathophysiology 26, 253–261 (2019).
Yu, Y. et al. Mesenteric lymph system constitutes the second route in gut–liver axis and transports metabolism-modulating gut microbial metabolites. J. Genet. Genomics 49, 612–623 (2022).
Choi, Y. et al. Immune checkpoint blockade induces gut microbiota translocation that augments extraintestinal antitumor immunity. Sci. Immunol. 8, eabo2003 (2023).
Eun, Y.-G. et al. Oral microbiome associated with lymph node metastasis in oral squamous cell carcinoma. Sci. Rep. 11, 23176 (2021).
Luu, K. et al. Fecal and tissue microbiota are associated with tumor T-cell infiltration and mesenteric lymph node involvement in colorectal cancer. Nutrients 15, 316 (2023).
Quail, D. F. & Dannenberg, A. J. The obese adipose tissue microenvironment in cancer development and progression. Nat. Rev. Endocrinol. 15, 139–154 (2019).
Wang, Z. et al. Paradoxical effects of obesity on T cell function during tumor progression and PD-1 checkpoint blockade. Nat. Med. 25, 141–151 (2019).
Cortellini, A. et al. A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. J. Immunother. Cancer 7, 57 (2019).
McQuade, J. L. et al. Association of body-mass index and outcomes in patients with metastatic melanoma treated with targeted therapy, immunotherapy, or chemotherapy: a retrospective, multicohort analysis. Lancet Oncol. 19, 310–322 (2018).
Harvey, N. L. et al. Lymphatic vascular defects promoted by Prox1 haploinsufficiency cause adult-onset obesity. Nat. Genet. 37, 1072–1081 (2005).
Cifarelli, V. et al. Visceral obesity and insulin resistance associate with CD36 deletion in lymphatic endothelial cells. Nat. Commun. 12, 3350 (2021).
Weitman, E. S. et al. Obesity impairs lymphatic fluid transport and dendritic cell migration to lymph nodes. PLoS ONE 8, e70703 (2013).
García Nores, G. D. et al. Obesity but not high-fat diet impairs lymphatic function. Int. J. Obes. 40, 1582–1590 (2016).
Escobedo, N. et al. Restoration of lymphatic function rescues obesity in Prox1-haploinsufficient mice. JCI Insight 1, e85096 (2016).
Sawane, M. et al. Apelin inhibits diet-induced obesity by enhancing lymphatic and blood vessel integrity. Diabetes 62, 1970–1980 (2013).
Chakraborty, A. et al. Vascular endothelial growth factor-D (VEGF-D) overexpression and lymphatic expansion in murine adipose tissue improves metabolism in obesity. Am. J. Pathol. 189, 924–939 (2019).
Karaman, S. et al. Decline of lymphatic vessel density and function in murine skin during aging. Angiogenesis 18, 489–498 (2015).
Kataru, R. P. et al. Structural and functional changes in aged skin lymphatic vessels. Front. Aging 3, 864860 (2022).
Nagai, T., Bridenbaugh, E. A. & Gashev, A. A. Aging-associated alterations in contractility of rat mesenteric lymphatic vessels: aging of mesenteric lymphatic vessels. Microcirculation 18, 463–473 (2011).
Da Mesquita, S. et al. Functional aspects of meningeal lymphatics in ageing and Alzheimer’s disease. Nature 560, 185–191 (2018).
Rustenhoven, J. et al. Age-related alterations in meningeal immunity drive impaired CNS lymphatic drainage. J. Exp. Med. 220, e20221929 (2023). This study demonstrates that ageing is associated with an increase in IFNγ in the meninges that drives age-related impairment in meningeal-lymphatic function.
Ecker, B. L. et al. Age-related changes in HAPLN1 increase lymphatic permeability and affect routes of melanoma metastasis. Cancer Discov. 9, 82–95 (2019). This study reports clinical data indicating low retention of radiotracer during SLN biopsy in patients who are aged, which is associated with reduced rates of LN metastasis but counterintuitively reduced survival, indicating that impaired lymphatic integrity with ageing may influence disease outcomes.
Xie, X. et al. Young age increases the risk for lymph node metastasis in patients with early colon cancer. BMC Cancer 19, 803 (2019).
Behring, M. et al. Age-dependent heterogeneity of lymph node metastases and survival identified by analysis of a national breast cancer registry. J. Pharm. Pharmacol. Res. 6, 147–157 (2022).
Tian, Z. et al. Young age increases the risk of lymph-node metastasis in patients with muscle-invasive bladder urothelial carcinoma. BMC Cancer 20, 851 (2020).
Jain, V. et al. Association of age with efficacy of immunotherapy in metastatic melanoma. Oncologist 25, e381–e385 (2020).
Erbe, R. et al. Evaluating the impact of age on immune checkpoint therapy biomarkers. Cell Rep. 36, 109599 (2021).
Takeda, A. et al. Single-cell survey of human lymphatics unveils marked endothelial cell heterogeneity and mechanisms of homing for neutrophils. Immunity 51, 561–572.e5 (2019).
Abe, Y. et al. A single-cell atlas of non-haematopoietic cells in human lymph nodes and lymphoma reveals a landscape of stromal remodelling. Nat. Cell Biol. 24, 565–578 (2022).
Qian, J. et al. A pan-cancer blueprint of the heterogeneous tumor microenvironment revealed by single-cell profiling. Cell Res. 30, 745–762 (2020).
Goveia, J. et al. An integrated gene expression landscape profiling approach to identify lung tumor endothelial cell heterogeneity and angiogenic candidates. Cancer Cell 37, 21–36.e13 (2020).
Geldhof, V. et al. Single cell atlas identifies lipid-processing and immunomodulatory endothelial cells in healthy and malignant breast. Nat. Commun. 13, 5511 (2022).
Xiang, M. et al. A single-cell transcriptional roadmap of the mouse and human lymph node lymphatic vasculature. Front. Cardiovasc. Med. 7, 52 (2020).
Kalucka, J. et al. Single-cell transcriptome atlas of murine endothelial cells. Cell 180, 764–779.e20 (2020).
González-Loyola, A. et al. FOXC2 controls adult lymphatic endothelial specialization, function, and gut lymphatic barrier preventing multiorgan failure. Sci. Adv. 7, eabf4335 (2021).
Fujimoto, N. et al. Single-cell mapping reveals new markers and functions of lymphatic endothelial cells in lymph nodes. PLOS Biol. 18, e3000704 (2020).
Sibler, E. et al. Immunomodulatory responses of subcapsular sinus floor lymphatic endothelial cells in tumor-draining lymph nodes. Cancers 14, 3602 (2022).
Antila, S. et al. Development and plasticity of meningeal lymphatic vessels. J. Exp. Med. 214, 3645–3667 (2017).
Nurmi, H. et al. VEGF‐C is required for intestinal lymphatic vessel maintenance and lipid absorption. EMBO Mol. Med. 7, 1418–1425 (2015).
Brouillard, P. et al. Primary lymphoedema. Nat. Rev. Dis. Prim. 7, 77 (2021).
Wigle, J. T. & Oliver, G. Prox1 function is required for the development of the murine lymphatic system. Cell 98, 769–778 (1999).
Srinivasan, R. S. et al. The Prox1–Vegfr3 feedback loop maintains the identity and the number of lymphatic endothelial cell progenitors. Genes Dev. 28, 2175–2187 (2014).
Hong, S. P. et al. Distinct fibroblast subsets regulate lacteal integrity through YAP/TAZ-induced VEGF-C in intestinal villi. Nat. Commun. 11, 4102 (2020).
Wiig, H. et al. Immune cells control skin lymphatic electrolyte homeostasis and blood pressure. J. Clin. Invest. 123, 2803–2815 (2013).
Li, J. et al. Neurotensin is an anti-thermogenic peptide produced by lymphatic endothelial cells. Cell Metab. 33, 1449–1465.e6 (2021).
Jakus, Z. et al. Lymphatic function is required prenatally for lung inflation at birth. J. Exp. Med. 211, 815–826 (2014).
Biswas, L. et al. Lymphatic vessels in bone support regeneration after injury. Cell 186, 382–397.e24 (2023).
Polomska, A. K. & Proulx, S. T. Imaging technology of the lymphatic system. Adv. Drug Deliv. Rev. 170, 294–311 (2021).
Acknowledgements
T.K. and T.M. contributed equally and are listed alphabetically. The authors thank L.H.M. Geraldo, S. Naik and C. Nowosad for critical reading of the drafted manuscript. T.K. received support from the A.G. Leventis Foundation. A.W.L. is supported by the National Institutes of Health (R01 CA238163, R01 AR080068, U54 CA263001, P50 CA225450), the Department of Defense (ME200052), the Cancer Research Institute (Lloyd J. Old STAR Award), the Mark Foundation for Cancer Research (19-047-ELA), the American Cancer Society (RSG-18-169-01-LIB) and the American Association for Cancer Research (AACR-BMS Midcareer Female Investigator Grant).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
A.W.L. reports consulting services for AGS Therapeutics. T.K. and T.M. declare no competing interests.
Peer review
Peer review information
Nature Reviews Cancer thanks Sirpa Jalkanen, Steven Stacker, who co-reviewed with Rae Farnsworth, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Chylous effusion
-
A medical condition in which lymph formed in the digestive system (chyle) leaks and accumulates into body cavities owing to a blockage in lymphatic drainage.
- Egress
-
The directional and active migration of leukocytes out of tissues, lymphoid and non-lymphoid, through the efferent lymphatic vasculature.
- Glymphatic system
-
A waste clearance system in the brain of vertebrates that uses perivascular channels formed by astroglial cells to promote the transport of macromolecules from the CNS.
- High endothelial venules
-
Specialized blood vessels found in lymphoid organs that are crucial to facilitate lymphocyte migration to lymphoid tissues.
- Interstitial flows
-
The slow movements of fluid through the extracellular matrix in connective tissues between blood and lymphatic vessels. Increases with inflammation as a function of vascular leakiness.
- Intestinal lacteal
-
Specialized lymphatic vessels found in the small intestine that are crucial in the absorption of dietary fats and fat-soluble molecules.
- LN paracortex
-
The inner area of the LN cortex between the outer cortex, which contains the B cell follicles, and the medulla. This area is rich in T lymphocytes and antigen-presenting cells (APCs).
- Lymphadenectomy
-
A surgical procedure to remove one or more lymph nodes. Often used as an important part of cancer staging and treatment.
- Lymphangiocrine factors
-
Molecules produced by lymphatic endothelial cells that can stimulate organ-specific repair activities in damaged or diseased organs.
- Lymphangiogenesis
-
A process of lymphatic growth in which new vessels form from the proliferation of pre-existing vessels.
- Lymphangiography
-
An imaging technique that leverages the uptake of interstitial dyes to image lymphatic structures and their functional transport to lymph nodes.
- Lymphatic remodelling
-
The reorganization, dilation, activation or growth of the lymphatic vasculature.
- Lymphedema
-
A chronic condition characterized by swelling and interstitial fluid accumulation owing to impaired lymphatic drainage.
- Lymph node
-
(LN). Secondary lymphoid organs that are linked by lymphatic vessels, provide an anatomical structure for the accumulation of T and B cells and perform important immune surveillance functions. Lymph node structure is maintained by a network of specialized non-haematopoietic cells, including lymphatic endothelial cells, that compartmentalize and distribute cells, antigens and activating signals for proper immune function. Lymph nodes are also often first sites of metastasis.
- Mesentery
-
In the small intestine, a fan-shaped membrane that attaches the jejunum and ileum to the posterior abdominal wall. The mesentery helps store fat and facilitates blood and lymphatic connections to the intestines.
- Neoadjuvant therapy
-
The therapeutic administration of a drug or treatment given before definitive surgical therapy.
- Sentinel lymph node
-
(SLN). A clinical term to define the first lymph node draining the tumour as determined by the accumulation of injected radiotracers at the time of surgery (sentinel lymph node biopsy).
- Shear stress
-
A mechanical force that acts in parallel with a surface, in this case referred to as the stresses formed by luminal fluid flow along an endothelial monolayer.
- Stem-like T (TSC) cells
-
Antigen-expanded, TCF1+ T cells with the capacity to maintain persistent T cell responses in the context of chronic antigen, for example, chronic infection, autoimmunity and cancer. Also known as progenitor-exhausted T cells.
- Tissue-resident memory T (TRM) cells
-
A memory T cell state that resides long term in peripheral non-lymphoid and lymphoid tissue and presumably surveys locally for re-encounter with pathogens or neoplastic cells. TRM cells do not recirculate in the absence of additional stimulation and are found in both mouse and human models.
- Tumour-draining LNs
-
A functional term to define any lymph nodes that are connected to and receive direct lymph output from the tumour.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karakousi, T., Mudianto, T. & Lund, A.W. Lymphatic vessels in the age of cancer immunotherapy. Nat Rev Cancer (2024). https://doi.org/10.1038/s41568-024-00681-y
Accepted:
Published:
DOI: https://doi.org/10.1038/s41568-024-00681-y



